access here - University of Alaska Anchorage
advertisement

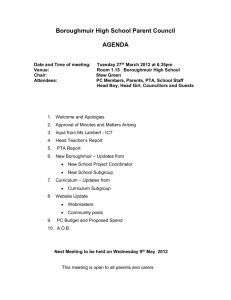
NEEDS ASSESSMENT AND ANALYSIS OF POTENTIAL STRATEGIES FOR A PHYSICAL THERAPY ASSISTANT PROGRAM FOR ALASKA Zuzana Rogers, PT, COMT Consultant Advanced Physical Therapy Abbott Rd Ste 200 Anchorage, AK 99507 January 2011 TABLE OF CONTENTS 1. Introduction ……………………………………………………………………………..3 2. PTA profession background…………………………………………………………...4 What can’t a PTA do?.................................................................................6 Practice settings………………………………………………………………...6 Direct access issues…..……………………………………………...………..7 3. Practice requirements………………………………………………………………….7 4. Career outlook for physical therapist assistants…………………………………….8 Supply and demand for physical therapist assistants in Alaska ……………..11 The need for physical therapist assistant program in Alaska…………………11 Rural areas…………………………………………………………………………13 5. Physical therapist assistant education………………………………………………14 Pre-physical therapist assistant education requirements……………………..14 Physical therapist assistant program overview…………………………………15 Clinical experience………………………………………………………………..16 Supervision of student physical therapy assistants……………………….......16 Graduation requirement…………………………………………………………..17 Continuing education and advancement……………………………………….19 6. Accreditation process………………………………………………………………...22 7. Steps towards Candidacy for Accreditation Status ……………………………….23 Program development…………………………………………………………….24 Submission of Application for Candidacy………………………………………24 Application for Candidacy review/ Visit to the Program/ Candidacy Visit Report………………………………………………………………………………25 Respond to Visit…………………………………………………………………..26 CAPTE makes a candidacy decision…………………………………………...26 8. Accreditation requirements…………………………………………………….........26 9. Recommendations for a physical therapy assistant program at the University of Alaska………………………………………………………………………………….26 Recommended program specifics………………………………………………27 Degree offered………………………………………………………………..27 Program length……………………………………………………………….27 Program delivery……………………………………………………………..28 Students enrolled…………………………………………………………….28 Resources and facilities……………………………………………………..29 Faculty…………………………………………………………………………30 Clinical education…………………………………………………………….30 Prerequisite coursework……………………………………………………..32 Cost…………………………………………………………………………….33 10. Other avenues to explore…………………………………………………………..33 11. Recommendations…………………………………………………………………..34 12. Additional resources…………………………………………………………………35 13. Attachments…………………………………………………………………………..37 2 The University of Alaska is considering the establishment of its own accredited physical therapist assistant program, whose outcome would be Associate degree, which is recognized state and nationwide. This report attempts to assess the need for physical therapist assistant education in Alaska and necessary steps to implement it. The information presented in this document was collected from, and it is based on a variety of sources including American Physical Therapy Association, the Commission on Accreditation of Educational Programs (CAPTE), Alaska State Chapter of APTA, survey of physical therapists and physical therapist assistants in Alaska, personal communications, and meetings. The University of Alaska has already committed itself to growth in the future as described in the Strategic Plan. The proposed physical therapy program was seen as a potential means to achieve this growth. Introduction When assessing the future need for a particular health profession in any given geographical region, it is important to consider five distinct and variable elements: 1. Is there currently a shortage of practitioners within the region? If so, what steps may be required to balance the market? 2. What is the region’s anticipated future growth and how many practitioners will be required to meet this anticipated growth? 3 3. What are some of the anticipated changes in the profession’s scope of practice and new career options and how will these changes increase or decrease the future demand for practitioner services within the region being evaluated? Will future practitioners require new or different skill-sets than those of current practitioners, and if so, how will these requirements affect the available workforce within the region? 4. What changes in technology will likely influence the productivity of physical therapy practitioners? 5. Will the anticipated growth in the net number of practitioners keep pace with future needs for practitioners when one considers other growth variables? (e.g., future graduation, retirement, and death rates; reciprocity into and away from the state and region; and practitioners leaving the profession). PT/ PTA profession background Physical therapy is a healthcare profession dedicated to identifying the highest functional potential of the individual client and striving to reach that goal through a variety of means. Physical therapy is only provided by a licensed physical therapist (PT) or a physical therapist assistant (PTA) under the supervision of a physical therapist. The physical therapist performs a thorough interview, examination, and evaluation with the patient and combines resulting findings with other health care information, such as diagnostic test results, to determine a diagnosis and create a unique treatment plan. 4 Physical therapists utilize a variety of treatments including, but not limited to, educating the client or caregiver, therapeutic exercise, functional training in self-care, manual therapy, orthotics and prosthetics, wound care and integumentary protection, physical, mechanical, and electrical modalities, and work integration and reintegration. Physical therapy can be beneficial to a wide range of clients, from the premature infant to the aged, the well to the terminally ill. Physical therapists may choose to specialize in a specific area such as cardiopulmonary, geriatrics, sports, clinical electrophysiology, neurology, orthopaedics or pediatrics. To meet the needs of so many different types of people, PTs and PTAs practice in a variety of settings including outpatient clinics, fitness centers, hospitals, skilled nursing facilities, schools, patient homes, sports teams, and work settings. They also practice in the community at health fairs or community centers performing general fitness assessments or screening for fall and/or injury risk. Additionally, PTs and PTAs may teach at universities or do research. Physical therapy is a dynamic profession and an integral part of healthcare services in the 21st century. Physical therapist assistants (PTAs) provide physical therapy services under the direction and supervision of a physical therapist. PTAs help people of all ages who have medical problems, or other health-related conditions that limit their ability to move and perform functional activities in their daily lives. PTAs work in a variety of settings including hospitals, private practices, outpatient clinics, home health, nursing homes, schools, and sports facilities. PTAs must complete a 2-year associate's degree and are licensed, certified, or registered in most states. Care provided by a PTA may include teaching patients/clients exercise for mobility, strength and coordination, training for 5 activities such as walking with crutches, canes, or walkers, massage, and the use of physical agents and electrotherapy such as ultrasound and electrical stimulation.1 What can’t a PTA do? Primarily, physical therapy assistants cannot, under any circumstances, work privately on their own. They must work with a physical therapist and assist with patient care, not dictate it. There are also guidelines that vary from state-to-state regarding the responsibilities of a PTA. The responsibilities and expectations of a PTA may also be governed by their place of employment. Practice settings Physical therapists and physical therapist assistants practice in various facilities. The 2006 APTA Practice Profile survey instrument asked a series of questions that described how respondents provided care (Table 1)2. Facility Acute care hospital Subacute rehab hospital Hospital based outpatient facility Private practice SNF Home care Musculoskeletal 44.0 Neuromuscular 26.4 Intergumentary 10.4 Cardiopulmonary 19.2 30.4 56.7 3.2 9.7 73.4 20.9 3.4 2.2 82.6 14.8 1.4 1.2 44.8 47.1 30.9 35.8 6.3 2.9 18.0 14.1 Guide to Development of Educational Programs for Physical Therapists and Physical Therapist Assistants. www.apta.org Accessed 12/01/2010. 1 2 www.apta.org/research. Accessed 11/23/10 6 Table 1. Mean percentage of patient care time spent per week in each system Direct access issues At present, there are 46 states (including Alaska) that provide patients direct access to physical therapy services. This allows the physical therapist to evaluate and treat patients without physician’s referral. Direct access laws vary from state to state, with some states having more limitations than others. Full list of states that allow direct access can be found on the American Physical Therapy Association website 3. The Alaska Physical Therapy Practice Act from 1986 uses following language when summarizing direct access: “No Restrictions to Access. License revocation or suspension when failure to refer a patient to another qualified professional when the patient’s condition is beyond PT training”. This Practice Act is due for revision in 2014, and serious effort is exerted to maintain and further define direct access. Any changes to the Practice Act might influence Physical Therapist or Physical Therapist Assistant education. Practice requirements Requirement for physical therapist assistants to practice vary from state to state. In order to provide physical therapy services, a physical therapist assistant in the State of Alaska needs to meet following requirements: 1. All 50 states and three additional jurisdictions require that physical therapist 3 www.apta.org/research. Accessed 11/23/10 7 assistants pass an accredited PTA education program consisting of classroom instruction and hands-on clinical experience. Alaska allows the use of online schools for students training to become a Physical Therapy Assistant. 2. Passing of the National Physical Therapy Exam is a prerequisite for obtaining a license in all states as well. The Federation of State Boards of Physical Therapy (FSBPT) coordinates and administers all licensure examinations for potential PTAs. Proof that the exam has been passed will be required when applying for a physical therapy assistant license. 3. Some states also require PTAs to pass a state jurisprudence exam covering laws and regulations in the state in which you are becoming licensed. These are primarily multiple choice exams administered by the state. In many cases, they are open-book or can be completed at home or online. 4. Many states also require that physical therapy assistants complete training in CPR and First-Aid. A minimum number of clinical hours are also required in all states. Additionally, it is possible that background checks will be administered to PTA license applicants. Career outlook for physical therapist assistants The nation’s aging population and expanded health care coverage will increase the demand for physical therapist (PT) and physical therapist assistant (PTA). It is projected that healthcare will add the most jobs during the 2008-2016 time period. The 8 increased demand in this area stems largely from an aging population that will require care at home, in nursing care facilities, and in inpatient and outpatient settings. The large baby-boom generation is entering the prime age for heart attacks and strokes, further increasing the demand for cardiac and physical rehabilitation. In addition, future medical developments should permit an increased percentage of trauma victims to survive, creating added demand for therapy services. Occupations that will "likely grow in importance" include physical therapists and physical therapist assistants. In addition, the expected expansion of health care coverage through reform measures could lead to increased demand for health care professionals. Physical therapy assistants are among the highest paid individuals with just an associate’s degree. After only two years of education, PTAs can enter the job field and at entry level, depending on their geographic location and place of employment, earn as much as $50,000. The median physical therapy assistant salary in the United States is $46,140. Annual physical therapy assistant pay, according to the U.S. Bureau of Labor Statistics, ranges from the lowest ten percent earning $28,580 or less to the highest earning PTAs in the country earning over $63,830. Hourly pay can vary from $13 an hour all the way up to $31 an hour. As with any job, the geographic location and the specific place of employment are key factors in figuring salary. The highest paying states for physical therapy assistants are California ($55,730), Nevada ($54,070), Texas ($53,530), Florida ($50,270), and Tennessee 9 ($49,840). The top paying metropolitan areas for this occupation are all located in California and Texas with annual mean wage topping out at $67,700 in OxnardThousand Oaks-Ventura, California. The top paying industries for this occupation are as follows, with the annual mean wage and annual hourly wage included: Home Health Care Services - $56,460, $27.14 Employment Services - $51,890, $24.95 Nursing Care Facilities - $50,070, $24.07 Individual and Family Services - $49,340, $24.72 Vocational Rehabilitation Services - $48,610, $23.37 General Medical and Surgical Hospitals - $45,190, $21.73 Health Practitioner Offices - $44,800, $21.54 Physician Offices - $43,170, $20.76 The majority of physical therapy assistants work full-time. They receive benefits comparable to other healthcare professionals including insurance, pension, vacation, disability, and retirement. Bonuses may also be included in the salary package for some PTAs. In addition, some industries of employment, such as hospitals may offer signing bonuses or incentives. Popular job listing sites, such as indeed.com and salary.com currently list jobs for physical therapy assistants with salaries that range from $34,000 to $80,000 for full-time workers. Additional costs that may be associated with physical therapy assistants primarily 10 will come from license renewal and continuing education. Most states require PTAs to renew their license biennially and complete a specific number of continuing education hours. State-to-state renewal requirements vary for physical therapy assistants. Supply and demand for physical therapy practitioners in Alaska In 2009, there were 1,008 Licensed PTs in Alaska, of which 503 resided in the state. Licensed PTs per 100,000 population was 144.31, while licensed PTs that reside in the State per 100,000 population was 72.01. National average of PTs per 100,000 population was 58.434. Currently, there are 121 licensed PTAs in the State of Alaska, of which 60 reside in the state5. Licensed PTAs per 100,000 population is 17.32, which is below nationwide average of 26.61 PTAs per 100,000 population. The need for a physical therapy assistant program in Alaska. Regarding Alaska Workforce Report from 2006, Alaska will experience a 36% growth of physical therapist positions projected to 2012. With the growth of physical therapy profession, the need for physical therapy assistants will grow as well. US Department of Labor projects 32.4% growth of Physical Therapist Assistants though 2016. The vacancy rate in private practice identified by a 2010 survey performed by the American Physical Therapy Association was found to be 14.4% among full-time PTAs, 4 5 www.apta.org, accessed 09/28/2010. www.apta.org accessed 1/12/2011 11 increase from 8.8% from 20086. Currently, there are no PTA programs in the State of Alaska. There are 6 PTA programs in the state of Washington, of which one is private. There is one PTA program in Montana, Oregon, and Idaho. Alaska students might chose one of these programs due to proximity to their state, but may also enter more distant programs. However, Alaska students often chose to enter different profession due to inability to study in-state and due to cost of out-of-state education. A survey given in 2010 assessed the need for physical therapists and physical therapist assistants in Alaska. The survey answered 67 members of the Alaska Chapter of APTA. The average distribution of physical therapists per clinic was 4.44 PTs/ clinic, with average of 1 PTA per 2 clinics. Twenty four members (36.4%) indicated vacancy for PTs/PTAs, of which 69% can be filled with PTAs. The survey also indicated that 39.7% of respondents would hire a PTA graduate from Alaska–based PTA program, 33.3% of respondents were not sure. Several respondents commented on the need for PT/ PTA program in Alaska (Table 3). Pro PT/PTA program in Alaska Support Alaska Communities Support rural areas Pro PTA Program The need for “professional extenders” in physical therapy practice Respondents had difficulty hiring a PTA Enroll Alaska Native The demand for PTAs students who will practice might increase with in rural areas increasing cost of 6 Pro PT program Limit on who PTAs can treat (Tricare insurance does not allow it) PTs might be better suited for rural areas due to supervision issues There might be limited number of clinical sites available to for PTA American Physical Therapy Association. Physical Therapy Vacancy and Turnover Rates in Outpatient Private Practice Facilities. Available at: www.apta.org/research. Accessed 07/27/2010 12 healthcare students due to supervision requirements Increase diversity for health careers in Alaska In-state tuition Table 3: AK Chapter of APTA survey results and comments, 2010 Rural areas The Alaska Center for Rural Health, in a November 2000 survey, identified shortages of nurses, social workers, dentists, dental assistants, pharmacists, opticians, speech pathologists, school psychologists, physical therapists, emergency medical technicians, mental health counselors, medical transcriptionists, radiologists, respiratory therapists, community health aides, and certified nursing assistants. Alaska Small Hospital Performance Improvement Network (ASHPIN, or Network) emerged in 2003 to form a network of the smallest, most rural hospitals. Its mission is to improve the clinical, operational, and financial performance of Alaska 's small rural hospitals to ensure patient access to appropriate healthcare services. Six (6) of the 13 Network members are healthcare providers located in medically underserved (MUS) communities serving medically underserved populations. It is important to note that of Alaska's 24 acute care hospitals, all but four of those hospitals have fewer than 100 beds , and of those 20, only two have more than 50 beds. Therefore, 75%, or 18 of Alaska 's 24 hospitals qualify as HRSA Small Hospital Improvement Project (SHIP) hospitals. The four relatively large non-military, medical/surgical hospitals in Anchorage (3) and Fairbanks (1) serve as regional referral facilities for providers from rural areas of the state, and all of Alaska's hospitals serve an 13 area larger - often much larger - than the community in which they are physically located. Impacting the quality of local care is the fact that many of the healthcare workers hired to work in rural settings are not of people of color, or even of Alaska Native descent. Attempts to increase the number and proportion of members of underrepresented racial and ethnic groups who are primary care providers are important, because ethnically diverse workers are more likely to provide services in a culturally appropriate manner, but these efforts have been largely unsuccessful in Alaska. For example, Alaska Natives trained in healthcare professions often do not practice in areas where health services are in short supply, or in areas with high percentages of underrepresented racial and ethnic populations7. An Allied Health Program, such as physical therapist or physical therapist assistant program that would allow Alaskans to study while living in the home state, might supply practitioners who are skilled in working with the underserved population. Physical therapist assistant education Pre-physical therapist assistant education requirements All physical therapy assistants (PTA) must complete a high school education or GED program. High school level classes that will prove helpful in the physical therapy field include Math, English, Anatomy, Physiology, and Psychology. After high school, 7 Alaska Center for Rural Health. Alaska 's Allied Health Workforce: A Statewide Assessment. University of Alaska Anchorage , March, 2001 14 potential PTAs will need to apply to an accredited physical therapy assistant education program. There are currently around 300 physical therapy assistant education programs accredited by the American Physical Therapy Association’s Commission on Accreditation in Physical Therapy Education. Physical therapist assistant program overview Physical therapy assistant degree programs typically take two years or five semesters to complete. An associate’s degree is issued upon the successful completion of a PTA education program. Most states do require that physical therapy assistants obtain an associates degree prior to filing for a PTA license. PTA education programs are available at technical or community colleges and some four-year colleges and universities. Physical Therapy Assistant Degrees are divided into academic coursework and hands-on clinical experience. Some programs may require students to get certified in CPR and complete a semester of coursework in anatomy and physiology before they can begin their clinical field experience. Other first aid certifications may also be required. Academic coursework includes instruction in the following: Algebra and Mathematics Anatomy Biology Chemistry 15 English Kinesiology Neurological Concepts Orthopedics Pathology Pediatrics Psychology Physical Therapy Techniques Physiology Clinical Experience Clinical experience is viewed as being absolutely essential to ensuring that students understand the concepts they have covered in the classroom and can properly perform their expected responsibilities. Most hand-on experience will take place in treatment centers. Supervision of student physical therapy assistants Student physical therapist assistants, when participating as part of a physical therapist assistant education curriculum, and when acting in accordance with the American Physical Therapy Association policy and applicable state laws and regulations, are qualified to perform selected physical therapy interventions under the direction and direct supervision of either the physical therapist alone or the physical 16 therapist and physical therapist assistant. The physical therapist is responsible for patient/client management. Direct supervision means the physical therapist is physically present and immediately available for direction and supervision. The physical therapist will have direct contact with the patient/client during each visit that is defined in the Guide to Physical Therapist Practice. Telecommunications does not meet the requirement of direct supervision 8 As of 10/01/10, Medicare Part A and Part B implemented new therapy student supervision guidelines in Skilled Nursing Facilities, which describes strictly 1:1, direct line of sight supervision of the PTA student by PT/ PTA (Attachment 1). Graduation requirements The completion of the degree also requires students to receive hands-on clinical experience to fulfill the degree requirements. The clinical experience gives students the first hand knowledge of the human anatomy and the basic physical therapist techniques they will need in the medical field. Employers won’t often hire graduates unless they have clinical experience. Upon completion of an accredited physical therapy assistant program, potential PTAs will need to obtain a license, certification, or register in order to practice. License, registration and certification requirements vary from state-to-state. However, most states will require the completion of an accredited PTA education program, as covered above, and the passing of the National Physical Therapy Exam. Some states also require PTA candidates to pass a state jurisprudence examination. http://www.apta.org/ Supervision of Student Physical Therapy Assistants HOD P06-00-19-31 [Amended HOD 06-96-20-35; HOD 06-95-20-11] [Position] [Document updated: 12/14/2009] 8 17 Overview of existing PTA programs which offer distance education9 Whatcom Community College, WA GateWay Community College, Phoenix, AZ San Juan College, Farmington, NM Accredited Yes, Northwest Commission on Colleges and Universities Yes, Higher learning Commission of the North Central Association of Colleges and Schools Yes, Higher learning Commission of the North Central Association of Colleges and Schools Classification Public rural, serving Medium Public Urban – serving Multicampus Public Rural serving Large Degree offered Associate in Science Associate in Applied Science Associate in Applied Science Program length 113 quarter hours 1. Full-time program Enrollment 24 students every fall/ 5,500 total 24/ year students into full-time program; 20 students every May into hybrid program, 9 2 years (6 semesters) to complete the 2. Hybrid weekend program for program distance incorporating education distance students. Format: education and on- online coursework campus weekend with on-campus courses. Can be labs completed in 21 months www.apta.org accessed 11/13/10 18 20 students every admission cycle Admission requirements -Experience in the field -2 quarters of labbased courses in Anatomy and Physiology -lab-based chemistry, biology, or physics -English 101 (Composition I) -college level math -general psychology (GERs are automatically met if completed bachelor’s degree) -min GPA of 2.5 -high school diploma or GED -40 hours of experience in the field -college level English -college-level anatomy and physiology -min GPA 2.4 -at least 5 hours of experience in the field -Human Body Structure and Function course (4 cr) -Musculoskeletal Focus for PTAs (3cr) -higher-level math -English composition -min 2.5 GPA Average tuition cost In state: $1,920/ year Out-of-state: $6,750/ year with possibility of a waiver Two part time, Two 7-week full time Resident: $71/ credit hour Resident: $43/credit hour; Non-resident: not known Non-resident: $97/credit hour Three full-time 6 week experiences One 4-week externship, Two 7week externships, One full-time, 4 part-time. Faculty to student ratio 1:24 Three full-time, several adjunct faculty. Faculty to student ratio 1;12 in labs, 1;2 in lecture classes Five full-time, 2 adjunct faculty. Faculty to student ratio 1:10 Clinical experience Faculty Continuing education and advancement The license of a physical therapy assistant will need to be renewed on a regular basis. Most states issue a two-year license. Certifications and registrations may also 19 need to be renewed. In addition, continuing education might be required in order for physical therapist assistants to maintain licensure. Continuing education most often takes the form of online courses, college courses, seminars and conferences. The American Physical Therapy Association is a great resource for exploring continuing education options. Physical therapy assistants who wish to gain further knowledge in their field can obtain additional skills in geriatric, pediatric, musculoskeletal, neuromuscular, integumentary, and cardiopulmonary physical therapy. The American Physical Therapy Associations gives recognition to such PTAs. There is minimal room for advancement as a physical therapy assistant. One option might be advanced training and certification in geriatrics, pediatrics, musculoskeletal, neuromuscular, integumentary, and cardiopulmonary physical therapy. Other PTA’s, with years of experience, may advance into non-clinical areas like administrative or academic teaching positions. Becoming a physical therapy assistant is not a stepping stone to becoming a physical therapist. While there are a few “bridge” programs that allow PTAs to work while going to school on weekends to become a physical therapist, they are rare. Such programs will award a Master’s degree in Physical Therapy upon completion. However, courses completed in a PT program are on the graduate level, while PTA courses are on the undergraduate level, so they don’t meet the graduate degree requirements of most physical therapy courses. Due to the intense study of physical therapy assistant programs in such a short time frame, there simply is just not enough time for the 20 prerequisites to be met that allows PTAs to go directly on to PT educational programs. Through campus based and online programs, aspiring Physical Therapy Assistants in Anchorage, Fairbanks, Juneau and Sitka, Alaska may be able to prepare themselves for the possibility of employment in some of the largest hospitals and healthcare facilities in the state including Providence Alaska Medical Center, Fairbanks Memorial Hospital, Alaska Regional Hospital, and Central Peninsula Regional Hospital. Current situation regarding physical therapist and physical therapist assistant education nationwide PT: US Programs PT: Non-US Program PTA: US Programs PTA: Non-US Programs Accredited 200 institutions supporting 213 programs Developing 15 institutions developing 15 programs MS/ MPT: 7 programs MS/ MPT: 0 programs Totals 215 institutions supporting/ developing 228 programs MS/ MPT: 7 programs DPT: 206 programs 3 institutions supporting 3 programs DPT: 15 programs DPT: 221 programs N/A 3 institutions supporting 3 programs Canada: 2 International: 1 244 Institutions supporting 263 programs 52 institutions developing 52 programs 479 accredited programs 67 developing programs Canada: 2 International: 1 296 institutions supporting/ developing 315 programs 546 accredited/developing programs Table 3: Number of PT and PTA programs as of December 13, 201010 10 http://www.apta.org/AM/Template.cfm?Section=PT_Programs3&TEMPLATE=/CM/Conte ntDisplay.cfm&CONTENTID=45221 21 Accreditation process through CAPTE The Commission on Accreditation in Physical Therapy Education (CAPTE) is the only recognized agency in the United States for accrediting education programs for the preparation of physical therapists and physical therapist assistants. CAPTE grants specialized accreditation status to qualified entry-level education programs for physical therapists and physical therapist assistants. Accreditation is a process used in the US to assure the quality of the education that students receive. It is a voluntary, nongovernmental, peer-review process that occurs on a regular basis. CAPTE is appointed by the Board of Directors of the American Physical Therapy Association; however, it makes autonomous decisions concerning the Evaluative Criteria, its Rules and Procedures, and the accreditation status of education programs for the preparation of physical therapists and physical therapist assistants. The 30 members of the Commission represent the communities of interest, including physical therapy and physical therapist assistant educators, clinicians, consumers, employers, representatives of institutions of higher education, and the public. 11 Robin Wahto attended CAPTE accreditation workshop in San Antonio, TX (Sept 2010). Please see lecture notes for complete detail. A summary of the accreditation process is provided below. 11 Guide to Development of Educational Programs for Physical Therapists and Physical Therapist Assistants. www.apta.org Accessed 12/01/2010. 22 The accreditation process through CAPTE consists of two steps: 1. Application for Candidacy and achievement of Candidacy status The granting of Candidate for Accreditation status must occur prior to enrollment of students in the professional/technical phase of the physical therapist assistant program. 2. Accreditation STEPS TOWARDS CANDIDACY FOR ACCREDITATION STATUS 1. Program director and supporting staff 1A. Employ a Program Director The program director should be employed full time 6-9 months prior to planned date for submission of AFC (Application for Candidacy), to develop the program. The program director for a PTA program should have following qualifications: PT or a PTA with minimum of Master’s degree, licensure or certificate in the state, experience in higher education (didactic/ teaching), experience in clinical practice, experience in administration, experience in curriculum design, development, implementation, and evaluation, and minimum of 5 years physical therapy experience. The program director must be working for the institution on a full-time basis to develop the program. The Program Director and at least one higher administrator from the institution must attend a workshop to learn about the candidacy process. This must be done prior to the 23 Application for Candidacy. Three workshops are conducted by the Department of Accreditation staff annually in February, June/July, and October. 1B. Notify CAPTE CAPTE needs to be notified of new program development when Program Director is hired (the notification letter should be official with PD’s CV attached). CAPTE then will add the program to the list of developing programs and will allow the PD access to electronic Portal. 1C. Employ an ACCE/ DCE Clinical education makes up approximately 1/3 of the curriculum. CAPTE does not require this step but strongly recommends it. The program director and clinical Coordinator then should work together to develop the program. 2. Program Development 2A. Selection of timing cycle. Application for Candidacy and fee due Staff determination that AFC is bona fide AFC sent to Candidacy reviewer Candidacy visits between Report of Candidacy Visit to program Response to Report of Candidacy Visit due CAPTE decision Cycle A March 1 Cycle B June 1 Cycle C Sept 1 Cycle D Dec 1 March 10 June 10 Sept 10 Dec 10 March 15 June 15 Sept 15 Dec 15 April 15-30 May 15 July 16-31 August 15 Oct 16-31 Nov 15 Jan 16-31 Feb 15 June 15 Sept 15 Dec 15 March 15 Late July Late Oct Late Jan Late April 24 It is estimated that it takes 4-5 months after AFC submission before the program can be implemented. Timing is crucial. 2B. Program development Mission, goals Expected outcomes Policies, procedures, and practices Curriculum Resources Clinical education program All other aspects of the program 2C. Write the Application for Candidacy The Application for Candidacy is a report through which institution provides information about the institution’s plans for development and implementation of the proposed program, such that it will meet the Evaluative Criteria for accreditation. 3. Submission of Application for Candidacy The AFC must be submitted on or before Mar 1, Jun 1, Sep 1, Dec 1. 4. AFC review by Candidacy Reviewer/ Visit to the program/ Candidacy Visit Report 25 When the Application for Candidacy is considered bona fide by the reviewers and is complete, the Candidacy Reviewer conducts a two-day visit to the program. 5. Respond to visit report Due 30 days after receipt of report, approximately 5 weeks prior to CAPTE review 6. CAPTE makes a candidacy decision Upon CAPTE’s determination to grant a program Candidate for Accreditation Status, students may be enrolled/ matriculated into the program’s first professional/technical courses. ACCREDITATION REQUIREMENTS 1. Full complement of core faculty 2. Complete curriculum, implemented 3. All necessary space and equipment 4. All needed clinical education placement Recommendations for a Physical Therapist Program at the University of Alaska The University of Alaska is well-suited for a physical therapist assistant program. 26 The mission of the University of Alaska Anchorage is “to discover and disseminate knowledge through teaching, research, engagement, and creative expression. Located in Anchorage and on community campuses in Southcentral Alaska, UAA is committed to serving the higher education needs of the state, its communities, and its diverse peoples. The University of Alaska Anchorage is an open access university with academic programs leading to occupational endorsements; undergraduate and graduate certificates; and associate, baccalaureate, and graduate degrees in a rich, diverse, and inclusive environment.”12 The potential PTA program should be an integral part of the University. Allied Health programs are designed to prepare graduates for work in rewarding careers in Alaska’s rapidly growing health care industry. Each program provides experiential education with students working alongside health professionals in real-work situations. The current and well-designed Allied Health Sciences Division is part of the Community and Technical College at UAA and should support a PTA program. Recommended Program Specifics Degree offered: Associate in Science or Associate in Applied Science Program length: 5 semesters (CAPTE requirements) 12 http://www.uaa.alaska.edu/chancellor/uaa-mission-statement.cfm Accessed 1/20/2010 27 Program delivery The two curricular format options that are utilized are an integrated, 2-year format or a 1+1 format, where the general education courses are taught in the first year and the technical PTA courses are offered in the second year. Admission requirements may vary depending on the format selected. A hybrid program with didactic courses in pure online delivery and procedural courses with online delivery of didactic material and face to face delivery of hands-on materials and skills seems to be the most suited for Alaska. Students would meet on regular basis for lab instructions and practice. All practical skills would be taught, practiced, and tested during these lab sessions, as well as all written exams would be completed during these lab sessions. Accreditation standards require distant delivery strategies to achieve equivalent curricular outcomes and all delivery models require students to complete the same curriculum and learning strategies - laboratories, small group discussions, and experiential education programs - regardless of their physical location. The major differences between the models are the degree to which students are required to be independent learners and the amount of direct engagement between faculty and students. Students enrolled: 8-10 students enrolled in the program (based on conversation with Jan Harris and Robin Wahto). This number of students should be able to meet the workforce need in the State of Alaska. Based on Vacancy data described earlier, the clinical community 28 will be able to absorb the number of graduates expected (8-10 graduating PTA students per 2 year period). Resources and Facilities Significant resources are needed to develop and implement a PT or PTA education program. This includes, but is not limited to: 1. Financial resources for Renovations of existing facilities or for new facilities Appropriate student services. Faculty recruitment Faculty salaries that may need to be competitive with the clinical salaries Faculty development Equipment and supplies Travel (clinical education; professional development) Library and learning resources 2. Space/Facilities Appropriate student services. Classrooms that will accommodate planned class size Laboratory space that accommodates needed treatment tables and physical therapy equipment for planned class size; laboratory space will need appropriate water and electrical access that will meet the needs of lab activities. Lab space is typically dedicated space. The students will need access to this lab outside of 29 class time for additional practice. Storage: of laboratory equipment and supplies Offices: space that ensures confidentiality Space for dressing/locker room space, computer labs, student gatherings Faculty: Recruiting a qualified director is typically a difficult task due to the ongoing shortage of qualified program directors for both PT and PTA programs. A program director with expertise in curriculum development, accreditation requirements and academic administration is vital to the success of a new program. Two full time faculty members are required, including a full-time program director (hired 6-9 months prior to application for candidacy), and adjunct faculty as needed. One of the full-time faculty must be a PT (per CAPTE). Because there is also a shortage of qualified faculty, recruiting qualified core (physical therapy educators) faculty will need to occur early during program development and could also impact the timeline for starting the program. Clinical Education Both PT and PTA programs must have sufficient numbers and varieties of clinical sites to ensure that students achieve expected program outcomes. It is important to have an abundance of available clinical education sites as staff shortages and competition from other physical therapy education programs may limit the number and 30 quality of available clinical experiences. The accreditation criteria require that the number of clinical sites be 125% of the number of students seeking those sites. That would result in the necessity of 10-13 clinical sites. Based on personal communication with practicing physical therapists and clinic owners/ directors, there seems to be sufficient number of clinics that would be available for clinical education in the Anchorage and Mat-Su area. The potential availability of physical therapy clinics in Fairbanks, Kenai Peninsula, and Southeast is unknown. Because developing the clinical education component of the curriculum is a time consuming activity, the Director of Clinical Education/Academic Coordinator of Clinical Education (DCE/ACCE) is often the second person to be hired. Curriculum development in physical therapy education requires careful coordination of the classroom/laboratory and clinical components. Clinical education sites must be recruited and developed to provide the appropriate clinical experiences for the level of student preparation. Qualified clinical instructors are essential to ensure sufficient clinical mentoring and teaching. Clinical education experiences are typically completed at clinical sites in the immediate geographic area for PTA programs. Sufficient time, personnel and budget will be needed to obtain and develop clinical education sites that will meet the needs of the program related to program and institutional mission, curricular expectations, curricular format, and planned class size. Prerequisite coursework 31 Current University of Alaska coursework that might satisfy admission requirement to a PTA program: Category UA course Written Communication Skills ENGL 111 Methods of written communication Quantitative Skills MATH 107 College Algebra MATH 108 Trigonometry Human Anatomy and Physiology with lab BIOL111 Human Anatomy and Physiology I BIOL 112 Human Anatomy and Physiology II Natural Sciences BIOL A102 Introductory Biology (Lab – based Biology, Chemistry, or Physics) Optional BIOL A103 Introductory Biology Lab CHEM A105/L General Chemistry I CHEM A106/L General Chemistry II PHYS A123/L Basic Physics I PHYS A124/L Basic Physics II Sociology SOC 101 Introduction to Sociology Psychology PSY 111 General psychology PSY 150 Lifespan Development Note: If the University of Alaska decides to address rural population, the mission of the program needs to reflect it. Also, might consider adding Alaska History / Culture to the program prerequisites or core curriculum. 32 Cost The costs for the Alaska student to complete an in-state program would be significantly less expensive as compared to relocating out-of-state to study. Other avenues to explore Partnership with already existing PTA programs The partnership model for physical therapy assistant education is one viable option for the University of Alaska; it would provide the opportunity for Alaska residents to receive a physical therapy assistant education and generate a meaningful increase in PTA manpower for the state. Although there are no sources of data to determine the number of students who studied out-of-state and then returned to practice in Alaska, the general consensus is that students tend to locate close to where they complete their education and thus don’t return to Alaska. If this tenet is true, then it is logical that conducting— at a minimum—the last semester of full-time experiential education in Alaska will increase the likelihood that Alaska residents who study physical therapy will be more likely to remain in the state to practice. If UA were to partner with an existing accredited physical therapist assistant program experienced in satellite program delivery, a satellite campus delivery model for local access to PTA education could provide Alaska residents with an opportunity to remain in Alaska to complete their entire PTA degree. 33 RECOMMENDATIONS 1. Organize an Advisory board consisting of: a. UAA representative (budget, timeline, organization, academic affairs, etc) b. PT/ PTA with experience in higher PT/ PTA education (prerequisites, curriculum, student selection process, student advisor) c. PT/ PTA with experience in clinical placement and equipment issues (developing clinical rotation sites, sequencing, contracts with clinical sites) d. Accreditation consultant Consultant services are strongly advised for institutions considering developing a new physical therapy education program for guidance in program planning, development, and implementation, including program assessment. Consultants that are experienced physical therapy educators can facilitate discussions about whether or not to proceed with program development. Should the decision be made to move forward, consultants may be beneficial to guide program development or to provide expertise in a specific area of program development; for example, curriculum development, faculty development or outcomes assessment. A list of educational consultants may be obtained by contacting Jody Gandy, Director, Department of Academic/Clinical Education Affairs at jodygandy@apta.org. 13 13 Guide 13 to Development of Educational Programs for Physical Therapists and Physical Therapist Assistants. www.apta.org Accessed 01/10/2011. 34 Additional Resources: Administrators of established education programs for the preparation of physical therapists and physical therapist assistants: Personnel from the institution considering the establishment of a program may find it helpful to visit other programs from similar academic institutions to gather information on space, staffing, equipment, and other resources. The director of an existing program may be willing to share information on essential resources and costs. However, since a new program may be in competition with an existing program for students, faculty and clinical education sites, program directors may be limited in the amount or type of assistance they can provide. Physical therapists and physical therapist assistants employed in varied practice settings within the community: Physical therapists in the community may be able to assist in the assessment of the availability and accessibility of local clinical education sites and the potential for positions in the local area for graduates of the proposed program. These individuals may be good sources for members of a program advisory committee. Advisory Committee: Advisory committees typically include representatives from stakeholder groups from within and outside the college. In addition to the clinicians, advisory committees often include leaders in the health care community, other health care professionals, health care administrators, future employers, and consumers. Representatives from within the college may include faculty and administrators of the 35 basic sciences and other health care professions, admissions officials, student services personnel, and the deans of appropriate colleges. 36 ATTACHEMENTS Implementing MDS 3.0: Use of Therapy Students As facilities continue to change their current practices to implement the Minimum Data Set Version 3.0 (better known as MDS 3.0), one of the emerging issues is the manner in which they document and utilize therapy students. Under the new rules, in order to record the minutes as individual therapy when a therapy student is involved in the treatment of a resident, only one resident can be treated by the therapy student and the supervising therapist or assistant (for Medicare Part A and Part B). In addition, the supervising therapist or assistant cannot engage in any other activity or treatment when the resident is receiving treatment under Medicare Part B. However, for those residents whose stay is covered under Medicare Part A, the supervising therapist or assistant cannot be treating or supervising other individuals and the therapist or assistant must be able to immediately intervene or assist the student as needed while the student and resident are both within line of sight supervision. For example under Part A, the therapist or assistant could be attending to paperwork while supervising the student and resident. Under Medicare Part A, when a therapy student is involved with the treatment, and one of the following occurs, the minutes may be coded as concurrent therapy: • The therapy student is treating one resident and the supervising therapist or assistant is treating another resident and the therapy student and the resident the student is treating are in line of sight of the supervising therapist or assistant; or • The therapy student is treating two residents, both of whom are in line of sight of the therapy student and the supervising therapist or assistant, and the therapist is not treating any residents and not supervising other individuals; or • The therapy student is not treating any residents and the supervising therapist or assistant is treating two residents at the same time, regardless of payer source, both of whom are in line of sight. The student would be precluded from treating the resident and recording the minutes as concurrent therapy under Medicare Part B. Under Medicare Part A, when a therapy student is involved with group therapy treatment, and one of the following occurs, the minutes may be coded as group therapy: • The therapy student is providing the group treatment and all the residents participating in the group and the therapy student are in line of sight of the supervising therapist or assistant who is not treating any residents and is not supervising other individuals (students or residents); or • The supervising therapist/assistant is providing the group treatment and the therapy student is not providing treatment to any resident. 37 Under Medicare Part B, when a therapy student is involved with group therapy treatment, and one of the following occurs, the minutes may be coded as group therapy: • The therapy student is providing group treatment and the supervising therapist or assistant is present and in the room and is not engaged in any other activity or treatment; or • The supervising therapist or assistant is providing group treatment and the therapy student is not providing treatment to any resident. These changes as well as other changes regarding MDS 3.0 took effect October 1, 2010. If you have questions regarding this provision or other provisions within MDS 3.0, please contact the APTA at advocacy@apta.org or at 888.999.2782 ext. 8533. 38