Antibiotics
advertisement

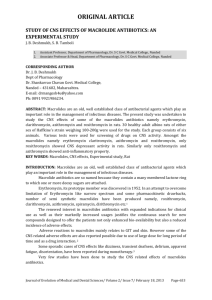
Seven lecture 7- Antibiotics Antibiotics Drugs: any compound taken with the intent to alter some forms or function of the body or treat disease. Antibiotics: a natural substance produced by a micro-organismto kill another Antimicrobial : any agent that kills or inhibits growth of a susceptible Organism Chemotherapy : treatment of a disease by a chemical compound selectively directed against invading microbes or abnormal cells • “-static” = agents which inhibit growth (e.g., bacteriostatic, fungistatic, and sporistatic) • “-cidal” = agents which kill the target organism (e.g., sporicidal, virucidal, and bactericidal). Adverse effect: An unwanted or dangerous reactions to a drug. Therapeutic effect: The positive or desirable effect expected to occur when a drug is administered. History • 1928: Alexander Fleming, a Scottish biologist, descovered the antibiotic effect of Penicillum. He observed that Penicillium notatum, a common mold, had destroyed staphylococcus bacteria in culture . Fleming received Nobel price • S. A. Waksman (1941): an antibiotic is a substance produced by a micro-organisme and has the capacity to inhibit the development of other microorganismes and even to destroy them. • 1946: started the industrial production of antibiotics. CLASSIFICATION OF ANTIBIOTICS CAN IN SEVERAL WAYS: • Depending on their mechanism of action against the infecting organism (the most common criteria). Some antibiotics attack the cell wall, some disrupt the cell membrane, the majority inhibit the synthesis of nucleic acids and proteins, etc. 1. Inhibitors of bacterial cell wall synthesis 2. Inhibitors of the function of the bacterial cell membrane. 3. Inhibitors of bacterial protein synthesis 4. Inhibitors of nucleic acid synthesis 5. Inhibitors of the synthesis of other structures bactérienes (interference with metabolic processes). • According to which bacterial strains they affect: staphylococcus, streptococcus, E. coli, etc. • Based on the chemical structure: penicillins, cephalosporins, aminoglycosides, tetracyclines, macrolides, sulfonamides, etc Prokaryotes vs. Eukaryotes We've talked about how Eubacteria and Eukaryotes differ. e.g. the cell wall, ribosomes, some enzymes may differ. Domain ribosomes Eubacteria 70S cell wall complex peptidoglycan RNA polymerase present one kind formylmethionine inhibited start codon antibiotics* Eukaryotes 80S if present, simple animals w/o cell wall absent several kinds methionine uninhibited *a number of antibiotics i.e. penicillin. The goal of an antimicrobial drug is to harm the pathogen and not harm the host. This is called selective toxicity. Spectrum of Antimicrobial Activity Broad Spectrum: Effective against many different types of bacteria (e.g.: both gram positive and negative). Examples: Tetracyclin Narrow Spectrum Antibiotics: Effective against a subset of bacteria (either gram positive and negative).Examples: Penicillin, Isoniazid (Mycobacteria only} Steps Involved in Pharmacokinetics Study: 1. Adsorption: Absorption is the process whereby a substance entering the body is assimilated by it. For proper pharmacokinetics study, it is necessary to know both the rate and the extent to which the active substance or therapeutic moiety are absorbed. They include substances intended to produce / not produce systematic effects. 2. Distribution: Distribution is the dispersion or dissemination of substances throughout the fluids and tissues of the body. 3. Metabolism: Metabolism is the process whereby a substance is irreversibly transformed into metabolites. 4. Excretion: Excretion is the elimination of the substance from the body. In rare cases, not all substances are eliminated; some drugs irreversibly accumulate in a tissue in the body. Pharmacokinetics is often studied in conjunction with pharmacodynamics. While pharmacodynamics explores what a drug does to the body, pharmacokinetics studies what the body does to the drug. Pharmacodynamics is the study of the biochemical and physiological effects of drugs and the mechanisms of drug action and the relationship between drug concentration and effect. II. Mechanisms of Resistance A. Mutations have provided for the following mechanisms of bacterial drug resistance 1. Inactivation of Drug by Enzymes 2. Prevent Drug from Entering Cell 3. Ejection of Drug 4. Alter Target Site of Drug B. Inactivation of Drug by Enzymes 1. Destruction or inactivation of drug by enzymes produced by bacteria 2. Ex) Penicillinase (ß-lactamase) breaks ß-lactam ring of penicillins & cephalosporins a. Not just in S. Aureus b. Also, Penicillinase-producing Neisseria gonorrhoeae (PPNG) 3. Penicillin was modified to beat this resistance (methicillin) a. Methicillin resistance soon appeared 4. Over 200 variations of B-lactamase enzymes are now known a. Each effective against minor variations of ß-lactam ring b. We alter the drug, and bacteria acquire new resistance 1) “Battle of Our Technology vs. Evolution” 5. Methicillin-Resistant Staphylococcus aureus (MRSA pronounced “mersa”) a. Resistant to most antibiotics (Superbug) b. In hospitals, invasive infections have 20% mortality rate c. Some strains resistant to vancomycin d. Nosocomial (hospital) – health care-associated MRSA e. Community-associated MRSA 1) Affects healthy people in the general public 2) Virulent, produce leukocidin that kills neutrophils B. Block Entry of Drug into Cell 1. Gram- bacteria can have modified porins which restrict entry of drug 2. Porins – proteins in outer membrane of Gram- cell walls; selectively permeability C. Ejection of Drug 1. Pumps in plasma membrane pump drug out of cell D. Alter Target Site of Drug 1. If the binding site of the drug is altered, the drug cannot bind 2. Ex) In order for drugs that affect translation at ribosomes to be effective they must bind to ribosome or another structure. If the binding site is altered, the drug cannot bind and therefore not affect translation. Mechanisms of Action of Antimicrobial Drugs: Introduction Antimicrobial drugs act in one of several ways: by selective toxicity , by inhibition of cell membrane synthesis and function, by inhibition of protein synthesis, or by inhibition of nucleic acid synthesis. Selective Toxicity An ideal antimicrobial agent exhibits selective toxicity , which means that the drug is harmful to a pathogen without being harmful to the host. Often, selective toxicity is relative rather than absolute; this implies that a drug in a concentration tolerated by the host may damage an infecting microorganism. Selective toxicity may be a function of a specific receptor required for drug attachment, or it may depend on the inhibition of biochemical events essential to the pathogen but not to the host. The mechanisms of action of antimicrobial drugs can be discussed under four headings: 1. Inhibition of cell wall synthesis. 2. Inhibition of cell membrane function. 3. Inhibition of protein synthesis (ie, inhibition of translation and transcription of genetic material). 4. Inhibition of nucleic acid synthesis. Eight lecture 8- Macrolides: 1. The investigators study intensely the antibacterial products of metabolism of various streptomycetes a high molecular weight, Woodward (1957) gave the name of macrolides to these compounds, also as the product of metabolism of Str. erythreus. Macrolide antibiotics are characterized by the presence in their molecules of the macrocyclic lactone ring connected with one or several carbohydrate residues, these are usually amino sugars. Chemistry: Macrolides contain a lacton ring and one or more deoxy sugars. The most important members of the group are erythromycin, clarithromycin, and azithromycin . 3. Mechanism of action of Macrolides: Macrolides inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit. Binding inhibits elongation of the protein by peptidyl transferase or prevents translocation of the ribosome or both. Macrolides are bacteriostatic for most bacteria but are cidal for a few Gram-positive bacteria. 4. Pharmacokinetics: a. All forms of erythromycin are absorbed following oral administration and diffuse in to most body tissues and fluids except CSF fluid. b. Macrolides are concentrated in the liver and is excreted primarily in bile and feces. 5. Preparations and administration: a. Oral macrolides base is supplied as enteric coated tablets. b. Macrolides ethylsuccinate, is available as granules or powder for oral suspension, other available oral salts are stearate, and estolate. c. Sterile macrolides gluceptate is available for parenteral administration. d. Macrolides base is available in topical formulations. 6. Side effects of Macrolides: a. Cholestatic hepatitis has occurred in adults treated for a week or longer with the estolate form. Hepatitis can also occur with the ethylsuccinate, and possibly with the stearate. The hepatitis is uncommon and is reversible. b. Epigastric distress can occur. c. A high incidence of thrombophlebitis occurs when erythromycin is administered intravenously even when the drug is dissolved in a large fluid volume. d. Superinfection can occur. e. Transient deafness has been reported, especially with higher doses. f. Erythromycin causes nausea and vomiting after oral administration in a significant number of patients. Jaundice is associated with some formulations of the drug. 7. Spectrum of activity: a. This drug is effective against G+ve organism, including some strains of S. aureus that are penicillin G resistance. b. Neisseria species, some strains of H. influenzae, and Bordetella, Legionella, Treponema, Mycoplasma species are sensitive to erythromycin. c. In general, it is not very active against most G-ve bacilli. d. Macrolide antibiotics can be administered orally, making them the choice for treating children who have streptococcal and staphylococcal infections. The most commonly used macrolide is Erythromycin, which is used to treat legionellosis, mycoplasmal pneumonia, and streptococcal and staphylococcal infections. e. Clarithromycin is also active against mycobacterium. In addition, both azithromycin and clarthromycin have demonstrated efficacy against Borrelia burgdorferi , the causal agent of lyme disease and the protozoan parasite Toxoplasma gondii, which causes toxoplasmosis. 5. Lincosamides : 1. The antibacterial products of metabolism of various streptomycetes, the product of metabolism of Str. lincolnesis . including clindomycin and lincomycin. Chemistry: Clindomycin is the 7-deoxy,7-chloro derivative of the parent drug, lincomycin, which it has essentially replaced. Pharmakinetics a. Although it is well absorbed following oral administration, clindomycin most often is administered parenterally. b. The drug is widely distributed in body fluids and tissues but does not pass readily into CSF fluid. c. Most of the drug is metabolized to the inactive sulfoxide form, which then is excreted in the bile and urine. 2. Mode of action: Lincosamides is chemically unrelated to the macrolides but has a similar mode of action and spectrum, are a miscellaneous group of protein synthesis inhibitors with activity similar to the macrolides. 3. Spectrum activity: Lincomycin has activity against Gram-positive bacteria and some Gram-negative bacteria (Neisseria, H. influenzae). Clindamycin is usually used to treat infections with anaerobic bacteria but can also be used to treat some protozoal diseases, such as malaria. It is a common topical treatment for acne, and can be useful against some methicillin-resistant Staphylococcus aureus (MRSA) infections. The most severe common adverse effect of clindamycin is Clostridium difficileassociated diarrhea (the most frequent cause of pseudomembranous colitis). Although this side-effect occurs with almost all antibiotics, including beta-lactam antibiotics, it is classically linked to clindamycin use. 4. Side effect: Pseudomembranous colitis can occur, resulting in diarrhea, abdominal pain, fever, and mucus and blood in the stools. At one time, this condition was often fatal, but now that the causative organism is known to be C. difficile, it can treated with vancomycin. 5.Resistance bacteria of Macrolides and clindamycin a. Altered accumulation (Minimal outer membrane penetration, efflux pump) b. Altered target (methylation of rRNA). c. Enzymatic inactivation (phosphotransferase, esterase). Macrolides: 1. The investigators study intensely the antibacterial products of metabolism of various streptomycetes a high molecular weight, Woodward (1957) gave the name of macrolides to these compounds, also as the product of metabolism of Str. erythreus. Macrolide antibiotics are characterized by the presence in their molecules of the macrocyclic lactone ring connected with one or several carbohydrate residues, these are usually amino sugars. Chemistry: Macrolides contain a lacton ring and one or more deoxy sugars. The most important members of the group are erythromycin, clarithromycin, and azithromycin . 3. Mechanism of action of Macrolides: Macrolides inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit. Binding inhibits elongation of the protein by peptidyl transferase or prevents translocation of the ribosome or both. Macrolides are bacteriostatic for most bacteria but are cidal for a few Gram-positive bacteria. 4. Pharmacokinetics: a. All forms of erythromycin are absorbed following oral administration and diffuse in to most body tissues and fluids except CSF fluid. b. Macrolides are concentrated in the liver and is excreted primarily in bile and feces. 5. Preparations and administration: a. Oral macrolides base is supplied as enteric coated tablets. b. Macrolides ethylsuccinate, is available as granules or powder for oral suspension, other available oral salts are stearate, and estolate. c. Sterile macrolides gluceptate is available for parenteral administration. d. Macrolides base is available in topical formulations. 6. Side effects of Macrolides: a. Cholestatic hepatitis has occurred in adults treated for a week or longer with the estolate form. Hepatitis can also occur with the ethylsuccinate, and possibly with the stearate. The hepatitis is uncommon and is reversible. b. Epigastric distress can occur. c. A high incidence of thrombophlebitis occurs when erythromycin is administered intravenously even when the drug is dissolved in a large fluid volume. d. Superinfection can occur. e. Transient deafness has been reported, especially with higher doses. f. Erythromycin causes nausea and vomiting after oral administration in a significant number of patients. Jaundice is associated with some formulations of the drug. 7. Spectrum of activity: a. This drug is effective against G+ve organism, including some strains of S. aureus that are penicillin G resistance. b. Neisseria species, some strains of H. influenzae, and Bordetella, Legionella, Treponema, Mycoplasma species are sensitive to erythromycin. c. In general, it is not very active against most G-ve bacilli. d. Macrolide antibiotics can be administered orally, making them the choice for treating children who have streptococcal and staphylococcal infections. The most commonly used macrolide is Erythromycin, which is used to treat legionellosis, mycoplasmal pneumonia, and streptococcal and staphylococcal infections. e. Clarithromycin is also active against mycobacterium. In addition, both azithromycin and clarthromycin have demonstrated efficacy against Borrelia burgdorferi , the causal agent of lyme disease and the protozoan parasite Toxoplasma gondii, which causes toxoplasmosis. 5. Lincosamides : 1. The antibacterial products of metabolism of various streptomycetes, the product of metabolism of Str. lincolnesis . including clindomycin and lincomycin. Chemistry: Clindomycin is the 7-deoxy,7-chloro derivative of the parent drug, lincomycin, which it has essentially replaced. Pharmakinetics a. Although it is well absorbed following oral administration, clindomycin most often is administered parenterally. b. The drug is widely distributed in body fluids and tissues but does not pass readily into CSF fluid. c. Most of the drug is metabolized to the inactive sulfoxide form, which then is excreted in the bile and urine. 2. Mode of action: Lincosamides is chemically unrelated to the macrolides but has a similar mode of action and spectrum, are a miscellaneous group of protein synthesis inhibitors with activity similar to the macrolides. 3. Spectrum activity: Lincomycin has activity against Gram-positive bacteria and some Gram-negative bacteria (Neisseria, H. influenzae). Clindamycin is usually used to treat infections with anaerobic bacteria but can also be used to treat some protozoal diseases, such as malaria. It is a common topical treatment for acne, and can be useful against some methicillin-resistant Staphylococcus aureus (MRSA) infections. The most severe common adverse effect of clindamycin is Clostridium difficileassociated diarrhea (the most frequent cause of pseudomembranous colitis). Although this side-effect occurs with almost all antibiotics, including beta-lactam antibiotics, it is classically linked to clindamycin use. 4. Side effect: Pseudomembranous colitis can occur, resulting in diarrhea, abdominal pain, fever, and mucus and blood in the stools. At one time, this condition was often fatal, but now that the causative organism is known to be C. difficile, it can treated with vancomycin. 5.Resistance bacteria of Macrolides and clindamycin a. Altered accumulation (Minimal outer membrane penetration, efflux pump) b. Altered target (methylation of rRNA). c. Enzymatic inactivation (phosphotransferase, esterase).