Adult_Intake
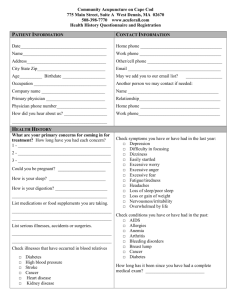
advertisement
~DISCOVERIES, LLP~ 600 S. Denton Tap Road, Suite 145, Coppell, TX 75019 (972) 473-0500 FAX: (972) 745-4542 ADULT INTAKE AND QUESTIONNAIRES PATIENT INFORMATION Patient’s Name: _____________________________________________________________________ SS# - - _____ Date of Birth: Age: Sex: Male Female Marital Status: Single Married Separated Divorced Home Address: City/State/Zip________________________________________________________________________ Phone: (home) (cell)_________________________________________ Occupation: Employer (School, if student): ___________________________________________ Work Phone: (________) Employer/Address: Your E-mail Address: ____________________________________ Pharmacy Phone #:_____________________________________________________________________ SPOUSE’S INFORMATION(if applicable) Spouse’s Name: Date of Birth: Spouse’s Employer: Occupation:___________________________ Employer’s Address: _____________________________________ Adult Intake Form _ Page 1 Adult Intake Questionnaires In order for us to be able to fully evaluate you, please fill out the following intake form and questionnaires to the best of your ability. We realize there is a lot of information and you may not remember or have access to all of it; do the best you can. If there is information you do not want in your medical chart it is ok to refrain from putting it in this information. Thank you! PATIENT IDENTIFICATION Name _______________________________ First Appointment Date _________________________________ REFERRAL SOURCE ______________________ MAIN REASON FOR SEEKING COUNSELING (Please give a brief summary of the main problems) __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ WHY DID YOU SEEK COUNSELING AT THIS TIME? What are your goals in being here? __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ _________________________________________________________________________________________ Adult Intake Form Page 2 PSYCHIATRIC MEDICATIONS/SUPPLEMENTS (Please list all current and past psychiatric medications/supplements you’ve taken; please include dosages, effectiveness and any side-effects.) If you need more room please attach a separate sheet. Date Taken Ex: 2/20005/2004 Medication Individual or Combinations Dosage(s) and time(s) taken per day Example Ritalin 5 mg BID Prozac 10mg QAM Effectiveness Example Improved concentration in morning, still moody Side-Effects/Problems Example Felt very unfocused in evening; hyperactive in evenings; dry mouth PSYCHIATRIC HISTORY Please list any psychiatrists/psychologists/therapists that you have seen previously: Name: Dates Seen: __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ MEDICAL HISTORY Current medical problems:____________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ Current non-psychiatric medications/supplements:_________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ Past medical problems: ______________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ Other doctors/clinics seen regularly: ____________________________________________________________ Adult Intake Form Page 3 Any history of head trauma? (describe): _________________________________________________________ __________________________________________________________________________________________ Prior hospitalizations (place, cause, date, outcome): ________________________________________________ Prior abnormal lab tests, X-rays, EEG, etc: _______________________________________________________ Present Height _______ Present Weight _______ CURRENT LIFE STRESSES (include anything that is currently stressful for you, examples include relationships, job, school, finances, children)______________________________________________________ __________________________________________________________________________________________ Sleep behavior: sleepwalking, nightmares, recurrent dreams, current problems (getting up, going to bed) _________________________________________________________________________________________ _________________________________________________________________________________________ School History: Last grade completed ____________ Last school attended ___________________________ Average grades received ______________ Specific learning disabilities _______________________________ Learning strengths __________________________________________________________________________ Employment History: (summarize jobs you've had, list most favorite and least favorite) Current job________________________________________________________________________________ _________________________________________________________________________________________ _________________________________________________________________________________________ _________________________________________________________________________________________ What would your employers or supervisors say about you? __________________________________________ _________________________________________________________________________________________ Religious Preference:_______________________________________________________________________ Ethnicity:_________________________________________________________________________________ Ever Any Legal Problems? _________________________________________________________________ Current Drug and Alcohol Use: (type of drug—frequency—amount used) __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ Alcohol and Drug History: (Please list age started and types of substances used through the years. Also, describe how each of these substances made you feel; what benefit you got from them.). These include alcohol, marijuana, prescription tranquilizers or sleeping pills, inhalants, cocaine or crack, amphetamines, steroids, opiates (heroin, codeine, morphine or other pain killers), hallucinating drugs (LSD, mushrooms), PCP. __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ Do you or have you ever experience withdrawal symptoms from alcohol or drugs? _______________________ Has anyone told you they thought you had a problem with drugs or alcohol? ____________________________ Caffeine use per day (caffeine is in coffee, tea, sodas, chocolate) _____________________________________ Nicotine use per day, past and present, (nicotine is in cigarettes, cigars, tobacco chew) ____________________ __________________________________________________________________________________________ Adult Intake Form Page 4 Sexual history: (answer only as much as you feel comfortable) Age at the time of first sexual experience: _______ Number of sexual partners: _________ Any history of sexually transmitted disease? _________ History of abortion? ___________________________ History of sexual abuse, molestation or rape? _____________________________________________________ Current sexual problems?_____________________________________________________________________ Any history of being physically abused: _________________________________________________________ FAMILY HISTORY Family Structure (who lives in your current household, please give relationship to each): __________________________________________________________________________________________ __________________________________________________________________________________________ Current Marital or Relationship Satisfaction___________________________________________________ __________________________________________________________________________________________ Significant Developmental Events (include marriages, separations, divorces, deaths, traumatic events, losses, abuse, etc.)________________________________________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ History of Past Marriages ___________________________________________________________________ Natural Mother's History: age_____ occupation _______________________________________________ Marriages _________________________________________________________________________________ Medical Problems __________________________________________________________________________ Childhood atmosphere (family position, abuse, illnesses, etc)_________________________________________ __________________________________________________________________________________________ Has mother ever sought psychiatric treatment? Yes ___ No ___ If yes, for what purpose? _________________ __________________________________________________________________________________________ Have any of your mother's blood relatives ever had any learning problems or psychiatric problems including such things as alcohol/drug abuse, depression, anxiety, suicide attempts, psychiatric hospitalizations? (specify) _________________________________________________________________________________________ _________________________________________________________________________________________ Natural Father's History: age_____ occupation ________________________________________________ Marriages _________________________________________________________________________________ Medical Problems __________________________________________________________________________ Childhood atmosphere (family position, abuse, illnesses, etc)_________________________________________ __________________________________________________________________________________________ Has father ever sought psychiatric treatment? Yes ___ No ___ If yes, for what purpose? __________________ __________________________________________________________________________________________ Have any of your father's blood relatives ever had any learning problems or psychiatric problems including such things as alcohol/drug abuse, depression, anxiety, suicide attempts, psychiatric hospitalizations? (specify) __________________________________________________________________________________________ __________________________________________________________________________________________ Siblings (names, ages, problems, strengths, relationship to patient) ____________________________________ __________________________________________________________________________________________ Children (names, ages, problems, strengths) _____________________________________________________ __________________________________________________________________________________________ __________________________________________________________________________________________ Describe yourself __________________________________________________________________________ Describe your strengths _____________________________________________________________________ Adult Intake Form Page 5 Brain System Checklist Please rate yourself on each of the symptoms listed below using the following scale. If possible, to give us the most complete picture, have another person who knows you well rate you. List other ___________________ 0 1 2 3 4NA Never Rarely Occasionally Frequently Very Frequently Not Applicable/Not Known Other Self ____ ____ 1. Problems sustaining attention to detailed tasks ____ ____ 2. Procrastinates or turns in assignments late ____ ____ 3. Problems following through and finishing tasks ____ ____ 4. Restless and fidgety ____ ____ 5. Problems setting and attaining goals ____ ____ 6. Uses caffeine to help focus ____ ____ 7. Uses nicotine to help focus ____ ____ 8. Acts impulsively ____ ____ 9. Interrupts others ____ ____ 10. Lack of forethought (says or does things before thinking about the implications) ____ ____ 11. Shows little empathy for others ____ ____ 12. Becomes fixated on thoughts (often negative) ____ ____ 13. Worries ____ ____ 14. Has difficulty getting over things (may hold a grudge) ____ ____ 15. Becomes upset if things do not go your way ____ ____ 16. Becomes upset if things are messy or out of place ____ ____ 17. Likes to follow a certain routine ____ ____ 18. Does not like change ____ ____ 19. Experiences obsessive thoughts ____ ____ 20. Experiences compulsive behaviors ____ ____ 21. Experiences addictive behaviors ____ ____ 22. Tends to be argumentative ____ ____ 23. Trouble shifting attention ____ ____ 24. Tendency to be oppositional ____ ____ 25. Feels sad ____ ____ 26. Is pessimistic and negative ____ ____ 27. Energy level is low ____ ____ 28. Less interested in activities that are usually fun ____ ____ 29. Crying episodes ____ ____ 30. Low self-esteem ____ ____ 31. Isolates socially ____ ____ 32. The future seems hopeless ____ ____ 33. Thoughts of wishing you were dead ____ ____ 34. Feelings of guilt ____ ____ 35. Problems concentrating ____ ____ 36. Problems sleeping—too little or too much ____ ____ 37. Feeling nervous ____ ____ 38. Headaches Adult Intake Form Page 6 Other/Self ____ ____ 39. Muscle tension (sore neck, jaw, etc…) ____ ____ 40. Easily startled ____ ____ 41. Social anxiety ____ ____ 42. Hyper vigilance (feeling keyed up or on edge) ____ ____ 43. Tendency for excessive motivation ____ ____ 44. Avoids conflict ____ ____ 45. Experiences thoughts going fast ____ ____ 46. Experiences panic attacks ____ ____ 47. Tendency to predict the worst ____ ____ 48. Problems turning off brain at night to go to sleep ____ ____ 49. Periods of significant irritability ____ ____ 50.Sensitivity to slights—misinterpreting comments as negative when they are not ____ ____ 51. Experiences paranoia (feeling that others are out to get you or cause you harm) ____ ____ 52. Becomes angry quickly (short fuse) ____ ____ 53. Problems with memory ____ ____ 54. Difficulty finding the right word to say ____ ____ 55. Significant mood swings ____ ____ 56. Dark thoughts (urges to hurt self or others) ____ ____ 57. Experiences déjà vu (feeling that you been somewhere or done something before that you haven’t) ____ ____ 58. Hears audible voices that others don’t ____ ____ 59. Sees shadows or other images moving out of the corners of your vision ____ ____ 60. Sloppy handwriting ____ ____ 62. Messy, disorganized ____ ____ 62. Clumsy (poor balance, coordination, or accident prone) ____ ____ 63. Sensitive to noise ____ ____ 64. Sensitive to touch or texture ____ ____ 65. Sensitive to light ____ ____ 66. Oversensitivity to environment ____ ____ 67. Problems keeping up in conversations ____ ____ 68. Slower than others in learning new tasks ____ ____ 69. Slow or slurred speech ____ ____ 70. Feel sleepy or the need to take a nap during the day ____ ____ 71. Mental sluggishness—brain fog ____ ____ 72. Difficulty losing weight (even on low calorie diet) ____ ____ 73. Irregular menstrual periods or heavy periods lasting longer than 5-7 days ____ ____ 74. Feeling fatigued even after significant sleep (8-10 hours) ____ ____ 75. Losing weight without dieting ____ ____ 76. Periods of a racing heartbeat while at rest ____ ____ 77. Crave sweets during the day ____ ____ 78. Feel shaky or jittery when hungry ____ ____ 79. Feel lightheaded and dizzy when meals are missed ____ ____ 80. Become agitated easily when hungry ____ ____ 81. Eating relieves agitation and fatigue ____ ____ 82. Decreased sex drive Adult Intake Form Page 7 Adult General Symptom Checklist Copyright 1997 Daniel G. Amen, MD Please rate yourself on each of the symptoms listed below using the following scale. If possible, to give us the most complete picture, have another person who knows you well (such as a spouse, partner or parent) rate you as well. List other person_____________________________ 0 Never Other 1 2 3 Rarely Occasionally Frequently 4NA Very Frequently Not Applicable/Not Known Self ____ ___ 1. Feeling depressed or being in a sad mood ____ ___ 2. Having a decreased interest in things that are usually fun, including sex ____ ___ 3. Experiencing a significant change in weight or appetite, increased or decreased ____ ___ 4. Having recurrent thoughts of death or suicide ____ ___ 5. Experiencing sleep changes, such as a lack of sleep or a marked increase in sleep ____ ___ 6. Feeling physically agitated or of being "slowed down" ____ ___ 7. Having feelings of low energy or tiredness ____ ___ 8. Having feelings of worthlessness, helplessness, hopelessness or guilt ____ ___ 9. Experiencing decreased concentration or memory ____ ___ 10. Having periods of an elevated, high or irritable mood ____ ___ 11. Having periods of a very high self-esteem or grandiose thinking ____ ___ 12. Having periods of decreased need for sleep without feeling tired ____ ___ 13. Being more talkative than usual or feeling pressure to keep talking ____ ___ 14. Having racing thoughts or frequently jumping from one subject to another ____ ___ 15. Being easily distracted by irrelevant things ___ ___ 16. Having a marked increase in activity level ____ ___ 17. Excessive involvement in pleasurable activities that have the potential for painful consequences (e.g., spending money, sexual indiscretions, gambling, foolish business ventures) ____ ___ 18. Experiencing panic attacks, which are periods of intense, unexpected fear or emotional discomfort (list number per month ____) ____ ___ 19. Having periods of trouble breathing of feeling smothered ____ ___ 20. Having periods of feeling dizzy, faint or unsteady on your feet ____ ___ 21. Having periods of heart pounding or rapid heart rate ____ ___ 22. Having periods of trembling or shaking ____ ___ 23. Having periods of sweating ____ ___ 24. Having periods of choking ____ ___ 25. Having periods of nausea or abdominal discomfort/trouble ____ ___ 26. Having feelings of a situation "not being real" ____ ___ 27. Experiencing numbness or tingling sensations ____ ___ 28. Experiencing hot or cold flashes ____ ___ 29. Having periods of chest pain or discomfort ____ ___ 30. Fearing death ____ ___ 31. Fearing going crazy or doing something out-of-control ____ ___ 32. Avoiding everyday places for 1) fear of having a panic attack or 2) needing to go with other people in order to feel comfortable ____ ___ 33. Excessive fearing of being judged by others, causing you to avoid or get anxious in situations ____ ___ 34. Experiencing persistent, excessive phobia (heights, closed spaces, specific animals, etc.) please list ______________________________________________________________________ ____ ___ 35. Having recurrent bothersome thoughts, ideas, or images that you try to ignore ____ ___ 36. Having trouble getting "stuck" on certain thoughts, or having the same thought over and over ____ ___ 37. Experiencing excessive or senseless worrying Adult Intake Form Page 8 Other/Self ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ___ 38. Others complaining that you worry too much or get "stuck" on the same thoughts ___ 39. Having compulsive behaviors that you must do or else you feel very anxious, such as excessive hand washing, checking locks, or counting or spelling ___ 40. Needing to have things done a certain way or else you become very upset ___ 41. Others complaining that you do the same thing over and over to an excessive degree ___ 42. Experiencing recurrent and upsetting thoughts of a past traumatic event (molestation, accident, fire, etc.), please list __________________________________________________ ___ 43. Experiencing recurrent distressing dreams of a past upsetting event ___ 44. Having a sense of reliving a past upsetting event ___ 45. Having a sense of panic or fear of events that resemble an upsetting past event ___ 46. Spending effort avoiding thoughts or feelings associated with a past trauma ___ 47. Regularly avoiding activities/situations which cause remembrance of an upsetting event ___ 48. Being unable to recall an important aspect of a past upsetting event ___ 49. Having a marked decreased interest in important activities ___ 50. Feeling detached or distant from others ___ 51. Feeling numb or restricted in your feelings ___ 52. Feeling that your future is shortened ___ 53. Being quick to startle ___ 54. Feeling like you're always watching for bad things to happen ___ 55. Experiencing a marked physical response to events that remind you of a past upsetting event ___ 56. Being markedly more irritable or experiencing anger outbursts ___ 57. Having unrealistic or excessive worry in at least a couple areas of your life ___ 58. Trembling, twitching, or feeling shaky ___ 59. Experiencing muscle tension, aches, or soreness ___ 60. Having feelings of restlessness ___ 61. Becoming easily fatigued ___ 62. Experiencing shortness of breath or feeling smothered ___ 63. Experiencing a pounding or racing heartbeat ___ 64. Sweating or having cold, clammy hands ___ 65. Experiencing dry mouth ___ 66. Experiencing dizziness or lightheadedness ___ 67. Having nausea, diarrhea or other abdominal distress ___ 68. Having hot or cold flashes ___ 69. Having to urinate frequently ___ 70. Having trouble swallowing or feeling a "lump in your throat" ___ 71. Feeling keyed up or on edge ___ 72. Being quick to startle or feeling jumpy ___ 73. Finding it difficult to concentrate, or having your "mind go blank" ___ 74. Having trouble falling or staying asleep ___ 75. Experiencing irritability ___ 76. Having trouble sustaining attention or being easily distracted ___ 77. Experiencing difficulty completing projects ___ 78. Feeling overwhelmed by the tasks of everyday living ___ 79. Having trouble maintaining an organized work or living area ___ 80. Being inconsistent in work performance ___ 81. Lacking in attention to detail ___ 82. Making decisions impulsively ___ 83. Having difficulty delaying what you want, having to have your needs met immediately ___ 84. Feeling restless and/or fidgety ___ 85. Making comments to others without considering their impact Adult Intake Form Page 9 Other/Self ___ ___ 86. Being impatient and/or easily frustrated ____ ___ 87. Experiencing frequent traffic violations or near accidents ____ ___ 88. Refusing to maintain body weight above a level that most people consider healthy ____ ___ 89. Intensely fearing gaining weight or becoming fat even though underweight ____ ___ 90. Having feelings of being fat, even though you're underweight ____ ___ 91. Experiencing recurrent episodes of binge eating large amounts of food ____ ___ 92. Feeling of lack of control over eating behavior ____ ___ 93. Engaging in regular activities to purge binges, such as self-induced vomiting, laxatives, diuretics, strict dieting, or strenuous exercise ____ ___ 94. Being over-concerned with body shape and/or weight ____ ___ 95a. Experiencing involuntary physical movements and/or motor tics (such as eye blinking, shoulder ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ shrugging, head jerking or picking). Please describe________________________________________ ____ 95b. Experiencing involuntary vocal sounds or verbal tics (such as coughing, puffing, blowing, whistling, or swearing). Please describe:________________________________________________________ ___ 96. Having delusional or bizarre thoughts (thoughts you know others would think are false) ___ 97. Seeing objects, shadows or movements that are not real ___ 98. Hearing voices or sounds that are not real ___ 99. Experiencing periods where your thoughts or speech were disjointed or didn’t make sense ___ 100. Feeling socially isolated or withdrawn ___ 101. Having a severely impaired ability to function at home or at work ___ 102. Behaving peculiarly ___ 103. Lacking personal hygiene or grooming ___ 104. Being in an inappropriate mood for a given situation (e.g., laughing at sad events) ___ 105. Having a marked lack of initiative ___ 106. Having frequent feelings that someone or something is out to hurt you or discredit you ___ 107. Snoring loudly (or others complaining about your snoring) ___ 108. Others saying that you stop breathing when you sleep ___ 109. Feeling fatigued or tired during the day ___ 110. Often feeling cold when others feel fine or they are warm ___ 111. Often feeling warm when others feel fine or they are cold ___ 112. Having problems with brittle or dry hair ___ 113. Having problems with dry skin ___ 114. Having problems with sweating ___ 115. Having problems with chronic anxiety or tension ___ 116. Having impairment in communication as manifested by at least one of the following (please circle all that apply): A delay in or total lack of the development of spoken language (not accompanied by an attempt to compensate); In individuals with adequate speech, having a marked impairment in the ability to initiate or sustain a conversation with others; The repetitive use of language, or the use of odd language; ___ 117. Having an impairment in social interaction, with at least two of the following (please circle all that apply): A marked impairment in the use of multiple nonverbal behaviors such as eye-to-eye gaze, facial expression, body postures, and gestures to regulate social interaction; A failure to develop peer relationships appropriate to developmental level; A lack of social or emotional reciprocity. Adult Intake Form Page 10 Medical Review of Systems Please place a check mark in the boxes that apply. Explain any problem areas. General Head, Eye, Ear, Nose, & Throat Genitourinary Being overweight Recent weight gain or weight loss Poor appetite Increased appetite Abnormal sensitivity to cold Cold sweats during the day Tired or worn out Hot or cold spells Abnormal sensitivity to heat Excessive sleeping Difficulty sleeping Lowered resistance to infection Flu-like or vague sick feeling Sweating excessively at night Excessive daytime sweating Excessive thirst Other_______________________ Facial pain Headache Head injury Neck pain or stiffness Frequent sore throat Blurred vision Double vision Overly sensitive to light See spots or shadows Hearing loss in both ears Ear ringing Disturbances in smell Runny nose Dry mouth Sore tongue Other________________________ Gastrointestinal and Hepatic Neurological Pacing due to muscle restlessness Forgotten periods of time Dizziness Drowsiness Muscle spasms or tremors Impaired ability to remember “Tics” Numbness Convulsions / fits Slurred speech Speech problem (other) Weakness in muscles Other_______________________ Trouble swallowing Nausea or vomiting (throwing up) Abdominal (stomach / belly) pain Anal itching Painful bowel movements Infrequent bowel movements Liquid bowel movements Loss of bowel control Frequent belching or gas Vomiting blood Rectal bleeding (red or black blood) Jaundice (yellowing of skin) Other________________________ Musculoskeletal Respiratory Asthma, wheezing Cough Coughing up blood or sputum Shortness of breath Rapid breathing Repeated nose or chest colds Other_______________________ Chest and Cardiovascular Ankle swelling Rapid / irregular pulse Breast tenderness Chest pain High blood pressure Low blood pressure Other_______________________ __ Adult Intake Form Back pain or stiffness Bone pain Joint pain or stiffness Leg pain Muscle cramps or pain Other________________________ Skin, Hair Dry hair or skin Itchy skin or scalp Easy bruising Hair loss Increased perspiration Sun sensitivity Other________________________ Itchy privates or genitals Painful urination Excessive urination Difficulty in starting urine Accidental wetting of self Pus or blood in urine Decreased sexual desire Other_______________________ Females No menses Menstrual irregularity Painful or heavy periods Premenstrual moodiness, irritability, anger, tension, bloating, breast tenderness, cramps, headache Painful menstrual periods Painful intercourse or sex Sterility infertility Abnormal vaginal discharge Other_______________________ Males Impotence (weak male erection) Inability to ejaculate or orgasm Scrotal pain Abnormal penis discharge Other_______________________ Explanation __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ __________________________ Page 11