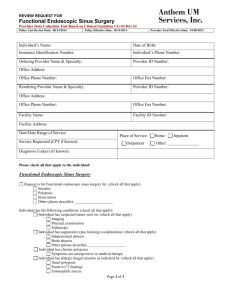
Sinusitis
advertisement

Sinusitis Author: Rochita V Ramanan, MD, Consultant in charge, Department of Radiology, The Apollo Heart Centre, Chennai, India Coauthor(s): Ali Nawaz Khan, MBBS, FRCS, FRCP, FRCR, LRCP, Chairman of Medical Imaging, Professor of Radiology, NGHA, King Fahad National Guard Hospital, King Abdulaziz Medical City, Riyadh, Saudi Arabia; Durre Sabih, MBBS, MSc, Visiting Faculty, Department of Nuclear Medicine, Pakistan Institute Applied Sciences and Nishtar Medical College, Director, Multan Institute of Nuclear Medicine and Radiotherapy Contributor Information and Disclosures Updated: Feb 20, 2007 Introduction Background Sinusitis is an inflammation of the mucosal lining of the paranasal sinuses. As the mucosa of the sinuses is continuous with that of the nose, rhinosinusitis is a more suitable term. Functional endoscopic sinus surgery (FESS) has revolutionized the treatment of sinusitis in recent years. The therapeutic benefits of FESS have helped a large number of patients with chronic sinus disease. Obstruction of the draining pathways of the sinuses is now thought to be the main cause of sinusitis. Examples of these pathways include the ostia of the maxillary sinuses and the hiatus semilunaris, where the anterior group of paranasal sinuses drains. Clearance of this obstruction is the aim of endoscopic surgery. Imaging has also progressed with FESS, and CT scanning can now demonstrate the sinus anatomy and patterns of sinusitis in exquisite detail before surgery. Pathophysiology Sinusitis is an inflammation of the mucosal lining of the paranasal sinuses usually related to viral, bacterial or fungal infections. Allergic sinusitis is also common. Inflammatory response to allergens results in edema and thickening of the mucous membrane. Usually the margins of the edematous mucosa have a scalloped appearance, but in severe cases, mucous may completely fill a sinus, making it difficult to distinguish an allergic process from infectious sinusitis. Characteristically, all of the paranasal sinuses are affected and the adjacent nasal turbinates are swollen. Air-fluid levels and bone erosion are not features of uncomplicated allergic sinusitis; however, swollen mucosa in a poorly draining sinus is more susceptible to secondary bacterial infection. The sinuses are lined by respiratory epithelium. The mucosal coat lining the sinuses can be subdivided into a superficial viscous layer and a deeper serous layer. Mucous secreted by the sinus mucosa traps bacteria. The mucous is naturally extruded through the normal ostia and expectorated or swallowed. The cilia expel the sinus secretions towards the natural ostia by beating in the serous layer. Normal sinus function is maintained as long as the ostia remain patent and the cilia function normal. Another ingredient of normal function is the quality of the mucous secreted. The most important factor in the pathogenesis of sinus disease is ostial obstruction, which leads to hypo-oxygenation, which in turn results in poor ciliary function and secretion of suboptimal quality of the mucous. Ciliary dysfunction leads to retention of the mucous within the sinuses. Several other factors that can lead to impaired ciliary function. Cold air is said to stun the ciliary epithelium, leading to impaired ciliary movement and retention of secretions in the sinus cavities. On the contrary, inhaling dry air desiccates the sinus mucous coat, leading to reduced secretions. Any mass lesion with the nasal air passages and sinuses, such as polyps, foreign bodies, tumors, and mucosal swelling from rhinitis, may block the ostia and predispose to retained secretions and subsequent infection. Drinking alcohol can also cause nasal and sinus mucosa to swell and cause impairment of mucous drainage. Kartagener syndrome is associated with immobile cilia and hence the retention of secretions and predisposition to sinus infection. Sinusitis can be subdivided into acute, subacute, and chronic disease. Acute sinusitis is defined as disease lasting less than 1 month, subacute disease lasts 1-3 months, and chronic sinusitis lasts longer than 3 months and generally related to suboptimally treated acute or subacute disease. Acute and subacute sinusitis is treated medically, whereas chronic sinusitis may require surgical intervention. Frequency United States Sinusitis is one of the most common diseases in the United States, affecting an estimated 15% of the population. The incidence of sinusitis has increased dramatically with the increasing incidence of asthma, allergies, and other upper respiratory tract infections. Each year, an estimated 50 million people in the United States have sinusitis, but the incidence of clinical frontal sinusitis specifically is lower. CT scans depict sinus abnormalities in 31-45% of the asymptomatic pediatric population. International Acute sinusitis affects 3 in 1000 people in the United Kingdom. Chronic sinusitis affects 1 in 1000 people. Sinusitis is more common in winter than in summer. Rhinoviral infections are prevalent in autumn and spring. Coronaviral infection occurs mostly from December to March. Mortality/Morbidity Sinusitis does not cause any significant mortality by itself. However, complicated sinusitis may lead to morbidity and, in rare cases, mortality. Complications of sinusitis include acute and chronic sequelae. The incidence of intracranial complications in all patients hospitalized with sinusitis has been reported as 3.7%. Sinusitis is implicated as a source of subdural abscess in 35-65% of cases. Acute distant effects include toxic shock syndrome. Acute local effects can also occur. Acute orbital complications include the following: cellulitis, proptosis, chemosis, ophthalmoplegia, orbital cellulitis, subperiosteal abscess, and orbital abscess. Other acute complications include intracranial sequelae such as meningitis; encephalitis; cavernous or sagittal sinus thrombosis; and extradural, subdural, or intracerebral abscesses. Bony complications include dental involvement and osteitis or osteomyelitis. Potts puffy tumor refers to swelling of the scalp, caused by an underlying osteitis of the skull or extradural abscess. A classical cause of such a swelling is complicated frontal sinusitis. Chronic complications of sinusitis include mucocele and pyocele. Race No significant race preponderance exists. Sex Women have more episodes of infective sinusitis than men because they tend to have more close contact with young children. The rate in women is 20.3%, compared with 11.5% in men. Age Sinusitis is more common in children and young adults, who are particularly susceptible to rhinovirus infections, than in others. Anatomy The paranasal sinuses are hollow cavities within the bones of the face and base of skull. The sinuses are lined by mucous membrane that is continuous with that of the nasal cavity. In addition, the sinuses are all paired. The frontal sinuses are posterior to the superciliary arch between the outer and inner tables of the frontal bone. The ethmoidal sinuses consist of thin-walled cavities in the ethmoid labyrinth. They vary in number and size from 3 large to 18 small sinuses. Their openings into the nasal cavity are highly variable. The 2 sphenoid sinuses are sited posterior to the upper part of the nasal cavity contained within the body of the sphenoid bone. The posterior ethmoid and sphenoid sinuses are in close relation to the optic nerve and the nerve may even be enclosed within the sphenoid sinus at times. The 2 maxillary sinuses are pyramidal cavities in the bodies of the maxillae. Their ostia are positioned nearer the roof than the floor. The anatomy of the sinuses on CT scans is described under CT Scan. Presentation Clinical findings may include the following: (1) pain over cheek and radiating to frontal region or teeth, increasing with straining or bending down; (2) redness of nose, cheeks, or eyelids; (3) tenderness to pressure over the floor of the frontal sinus immediately above the inner canthus; (4) referred pain to the vertex, temple, or occiput; (5) postnasal discharge; (6) a blocked nose; (7) persistent coughing or pharyngeal irritation; (8) facial pain; and (9) hyposmia. Preferred Examination Radiography Plain radiography is generally obsolete, but exceptions include its use in confirming airfluid levels in acute sinusitis and evaluating size and integrity of the paranasal sinuses. Radiographs may still provide a useful adjunct to diagnosis in parts of the world, where sophisticated imaging is not yet available. Whether the Waters view is sufficient for evaluating suspected acute bacterial sinusitis is debated. In general, Waters, Caldwell, and lateral views are obtained. Magnetic resonance imaging MRI is generally reserved for the evaluation of any complications of local sinus infections, particularly suspected intracranial extension. T1-weighted images and fat-suppressed T2-weighted images effectively depict the paranasal sinuses and adjacent facial compartments. Fat-suppressed gadoliniumenhanced T1-weighted images are helpful for assessing extension to the skull base and intracranial cavity. MRI is useful in differentiating sinusitis from neoplasia and in imaging patients with dental fillings that cause artifacts on CT scans and patients who cannot lie prone because of kyphoscoliosis. MRI clearly depicts tumor from surrounding inflammatory tissue and secretions within the sinuses. Typically, edema of inflamed tissue and retained secretions have low intensity on T1-weighted images and high intensity on T2-weighted images because of their increased water content. However, because of the often chronic nature of these secretions at diagnosis, a certain amount of free water will have been absorbed, and a variable pattern of intensity may be seen. On the contrary, 95% of sinus tumors are highly cellular with decreased water content, resulting in low-to-intermediate signal intensity on both T1- and T2-weighted imaging. Gadolinium enhancement provides additional information. Most sinus tumors show diffuse enhancement, whereas inflamed mucosa enhances more intensely and peripherally. Perineural spread to tumor can also be shown on MRI; this is most important in the context of adenoid cystic carcinoma. The correlation of MRI and histologic findings at surgery is as high as 94% with improvement to 98% with gadolinium enhancement. Some of the advantages of MRI are now being eroded by modern multisection CT with its capability for instant axial and coronal reformatting, which avoids dental artifact. In fact, MRI may now be limited by dental amalgams. Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have recently been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Fibrosing Dermopathy. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. As of late December 2006, the FDA had received reports of 90 such cases. Worldwide, over 200 cases have been reported, according to the FDA. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with troublemoving orstraightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape. CT scanning CT is the examination of choice in the evaluation of sinusitis, particularly chronic sinus disease providing excellent detail of sinus anatomy. However, CT is usually not useful in acute sinusitis, as diagnosis is primarily based on clinical findings. Good anatomic definition is desirable before surgical intervention. CT scans are more sensitive than plain radiography for depicting sinus pathology, especially in the sphenoid and ethmoid sinuses. However, CT findings can also be nonspecific and many centers do not use it routinely in the diagnosis of acute sinusitis. Coronal CT imaging is the preferred initial procedure. Bone-window views provide excellent resolution and a good definition of the complete osteomeatal complex and other anatomic details that play a role in sinusitis. In addition, the coronal view is best correlated with findings from sinus surgery. In general, nonenhanced CT scans suffice in cases of uncomplicated sinusitis. Multisection CT seems to have the potential to replace primary coronal CT of the paranasal sinuses without any loss of image quality, and it may even improve the overall diagnostic value. However, the doses of radiation may still have to be reduced. Limitations of Techniques On plain radiographs, other bony structures overlap the sinuses, and the rate of falsenegative results is high. The posterior ethmoids are poorly visualized. The osteomeatal complex cannot be adequately assessed. The superiority of CT over other methods of imaging the sinuses can be summarized as follows: First, coronal CT is ideal for evaluating sinusitis because the anatomy and pathology visualized in a plane almost identical to that seen by the endoscopist, and this imaging plane displays the osteomeatal unit. Second, the bony walls of the sinuses are better demonstrated with CT in the high-resolution mode than with other modalities. Third, CT provides an excellent anatomic display of soft tissue attenuation. This depiction includes fluid levels and polypoid masses within the normally air-filled cavities of the sinuses, nasal cavity, and postnasal space. Most important, disease extending beyond the bony perimeters of the sinuses into the adjacent soft tissue of the orbit, brain, and infratemporal fossa can be imaged. These applications of CT have disappointed in only one way. Although it provides an excellent anatomic display, CT generally does not help in predicting the histologic nature of the pathologic process. A major milestone in radiology occurred with the introduction of MRI. This modality provides greater soft-tissue contrast, tissue differentiation, and marginal lesion definition than those achieved with other studies. However, the bony margins of the sinuses are imaged as a plane of absent signal intensity on MRIs. Moreover, the signal intensity from the high fat content of bone narrow, as in the basisphenoid and petrous apices and around the frontal sinuses, can be confusing, particularly because fluid retained in the sinuses has signal intensity similar to that of the high water content. On CT scans, it is difficult or impossible to differentiate tumor tissue from retained fluid in sinuses, where the drainage of a sinus is blocked by obstruction from the tumor. Extension of disease into the cranial cavity is shown well on MRIs, and the ability to image in any plane is a considerable advantage. Differential Diagnoses Other Problems to Be Considered Wegener granulomatosis: This involves angiitis associated with focal necrosis and granulomatous reaction, which initially affects the respiratory tract but which may progress to involve other organs. Ataxia-telangiectasia: This autosomal recessive disorder is associated with recurrent sinusitis, pulmonary infections, bronchiectasis, pulmonary fibrosis, tracheomegaly, diminished lymphoid tissue, and cerebral and cerebellar atrophy. Cystic fibrosis: This autosomal recessive disorder associated with respiratory, GI, cardiovascular and sinus abnormalities, among others. Immotile cilia syndrome: This autosomal recessive disorder is associated with recurrent chest infections and/or pulmonary consolidation, sinusitis, bronchiectasis, and Kartagener syndrome. Kartagener syndrome: This autosomal recessive disease is associated with sinusitis, situs inversus, recurrent respiratory infections, and bronchiectasis, among other abnormalities. Nasal polyposis: Hyperallergic patients may have innumerable polyps filling the nasal cavity and obstructing the paranasal sinuses, giving a characteristic imaging appearance. This disease is closely associated with asthma. Wiskott-Aldrich syndrome: This X-linked, recessive, immune deficiency disease is associated with recurrent respiratory tract infections and/or pneumonia, sinusitis, and mastoiditis. Yellow-nail syndrome: The mode of inheritance is not known. This syndrome is associated with recurrent pleural effusions, pericardial effusions, chylothorax, bronchiectasis, and sinusitis. Young syndrome: The mode of inheritance is unknown. The syndrome is associated with azoospermia secondary to epididymal obstruction and recurrent respiratory infections and sinusitis. Sinusitis: Imaging Author: Rochita V Ramanan, MD, Consultant in charge, Department of Radiology, The Apollo Heart Centre, Chennai, India Coauthor(s): Ali Nawaz Khan, MBBS, FRCS, FRCP, FRCR, LRCP, Chairman of Medical Imaging, Professor of Radiology, NGHA, King Fahad National Guard Hospital, King Abdulaziz Medical City, Riyadh, Saudi Arabia; Durre Sabih, MBBS, MSc, Visiting Faculty, Department of Nuclear Medicine, Pakistan Institute Applied Sciences and Nishtar Medical College, Director, Multan Institute of Nuclear Medicine and Radiotherapy Radiography Findings Examination in the erect position is desirable to reveal fluid levels, which may be present. The following projections allow a good all round assessment of the paranasal sinuses: Occipitomental or Waters view: This view shows the maxillary antra clearly. The frontal sinus is projected obliquely. The ethmoid air cells are obscured, but a few may be seen along the medial walls of the orbit and within the nose. The sphenoid sinus is seen through the open mouth. Occipitofrontal of Caldwell view: The frontal sinuses are well seen. The floors of the maxillary sinuses are visible. The floor of the sella turcica, the crista galli, the nasal septum and the middle and inferior nasal turbinate can be seen. The anterior ethmoid air cells are also seen. However, the sphenoid sinus is obscured. Lateral view: The sphenoid sinus and frontal sinus are visualized. The rest of the sinuses are superimposed. The nasopharyngeal soft tissue and the adenoids are also well visualized. A modified basilar view (a submental vertex view) may be a useful adjunct when dealing with sphenoid sinus disease. An orthopantomographic view is not a standard view and requires different equipment. This provides a panoramic view of the floors of the maxillary sinuses and the upper and lower alveoli. Fluid levels are the most common finding in acute bacterial sinusitis and are not generally seen in other forms of sinusitis. Mucosal thickening represented by parallel soft tissue opacity along the bony walls of the sinuses may be seen. Mucous retention cysts are represented by soft tissue opacity with a surface convex towards the cavity of the sinus, along any of the walls. Hypertrophy of the turbinates may be seen. The nasal cavities may be filled in with soft tissues; this finding is suggestive of polyps. Total opacification of a sinus may also be seen. If the sinus is more opaque than its pair or the ipsilateral orbit, it is thought to be totally filled in with soft tissues or fluid. Degree of Confidence With the advent of CT, the role of conventional radiography has taken second place and presently has a limited role in the management of sinusitis. There are wide intraobserver differences in the interpretation of plain radiographs, and the rate of false-negative results is high. Possible findings in acute sinusitis include mucosal thickening, air-fluid levels, and complete opacification of the involved sinus. The role of imaging in acute sinusitis is controversial, and many regard acute sinusitis a clinical diagnosis. Mucosal thickening is seen in more than 90% of patients with sinusitis, but this finding is highly nonspecific. Air-fluid levels and complete opacification are more specific for sinusitis, but they are seen in only 60% of sinusitis cases. Air-fluid levels generally indicate bacterial sinusitis, and its presence is helpful in excluding other forms of sinusitis. In infants aged 3 years or younger, conventional sinus radiographs usually contribute little because of the sinus opacification secondary to normal nonpneumatized sinuses. Conventional radiographs allow poor visualization of ethmoid air cells. If used at all, conventional radiographs should be reserved for patients with persistent symptoms despite appropriate therapy. A single occipitomental (Waters view) suffices in this situation. Aalokken and associates evaluated plain radiography in a prospective investigation of patients with clinically suspected acute sinusitis by using standard CT as the criterion standard. They recruited 47 consecutive patients, who underwent conventional radiography and standard-dose CT on the same day. The sensitivity and specificity of the plain radiography were calculated. The specificity was high, but the sensitivity was low except for imaging of the maxillary sinus (sensitivity, 80%). Therefore, for maxillary sinusitis, plain radiography was reasonably accurate. A negative finding in the other sinuses was not reliable. The authors concluded that the sensitivity of plain radiography for detecting sinus opacifications was unacceptably low for the ethmoid, frontal, and sphenoid sinuses. The specificity was high. Garcia and associates evaluated radiography and CT for the examination of the paranasal sinuses in 91 pediatric patients with chronic upper respiratory tract symptoms for at least 3 months. When sinus radiographs were compared with CT scans, radiographs could not depict minimal disease. For clinically significant sinusitis, sinus radiographs depicted disease in 20% of frontal sinuses, 0% of sphenoidal sinuses, and 54% of ethmoidal sinuses. With the minimal criteria of 40-50% opacification or fluid-level filling of the maxillary antrum, radiographs depicted disease in 75%. The sensitivity and specificity of a Waters view to confirm clinically significant chronic sinusitis without specifying the sites and severity were acceptable at 76% and 81%, respectively. The authors concluded that a single Waters view is an acceptable part of the initial evaluation of pediatric chronic sinusitis; however, they found a limited CT scan a better alternative. False Positives/Negatives Findings on CT should be interpreted in conjunction with clinical and endoscopic findings because of high rates of false-positive findings. As many as 40% of asymptomatic adults have abnormalities on sinus CT scans, as do more than 80% of those with minor upper respiratory tract infections. The differentiation of infection, tumor, polyp, and allergic mucosal thickening may be difficult, and all of these conditions can lead to a false-positive diagnosis. Sinus mucosal thickening or opacification may also occur in hematologic disorders, fibrous dysplasia, Wegener granulomatosis, and Paget disease. Computed Tomography Findings Anatomy CT evaluation of paranasal sinuses for sinusitis should include an assessment of the pattern of disease, the extent of disease, the probable mechanical cause, and the relevant anatomic details required for planning surgery. To evaluate the pattern of sinusitis, one must understand the drainage of various sinuses. The anatomy of drainage revolves around the osteomeatal unit which is not a single morphological structure but a combination of the following structures: (1) middle turbinate, (2) ethmoid bulla, (3) uncinate process, (4) maxillary infundibulum, (5) hiatus semilunaris (ie, space beneath the middle turbinate), and (6) maxillary os. The hiatus semilunaris is a space between the uncinate process anteroinferiorly and the ethmoid bulla posterosuperiorly. The anterior group of ethmoid air cells drains into the anterior aspect of the hiatus semilunaris through the frontonasal duct. The middle group drains into the hiatus semilunaris on or above the ethmoidal bulla. The frontal sinus drains through the frontonasal duct or through the anterior ethmoidal cells into the hiatus semilunaris. The maxillary infundibulum drains into the posterior part of the hiatus semilunaris. The frontal, maxillary, anterior, and middle ethmoidal sinuses all drain into the hiatus semilunaris of the middle meatus. Any mechanical block in this region causes inflammation of the above mentioned sinuses. This is called the osteomeatal pattern or middle meatus syndrome. The sphenoid sinus drains posterior to the superior turbinate into the sphenoethmoid recess through the sphenoid ostium. The posterior ethmoid air cells also drain through the superior meatus into the sphenoethmoid recess. An obstruction in this region gives rise to the sphenoethmoid pattern of sinusitis. Normal variants Concha bullosa is an aerated middle turbinate that could compress the uncinate process and obstruct the middle meatus and the infundibulum (see Image 5). It is present in 35% of the population. The degree of pneumatization may vary from side to side. Usually, 1 cell and, occasionally, 2 or 3 cells are seen. The Haller cell, or infraorbital cell, extends inferior to the ethmoid bulla and lateral to the maxillary sinus roof and interposes itself between the lamina papyracea and the uncinate process. A large Haller cell may obstruct the middle meatus. It is usually located in the anterior ethmoid, but it may extend all the way from anterior to posterior. It is seen in 10% of the population, in whom it is unilateral in 5.4% and bilateral in 4.5%. The middle turbinates may have a paradoxical curve, causing narrowing of the middle meatus. A deviated nasal septum or a septal spur may cause compression of the middle turbinates and resultant narrowing of the middle meatus. A large ethmoid bulla can protrude into the middle meatus and cause it to become narrowed. Pathology Polypoid mucosal thickening may be seen in the affected sinuses. Polypoid soft-tissue masses may be seen to extend from the sinuses into the nasal cavities. The osteomeatal complexes may be obstructed by concha bullosa, enlarged bulla ethmoidalis, a long infundibulum or mucocele. A bony erosion may suggest the presence of a mucocele. An air-fluid level within the sinuses may be seen. Hyperattenuating soft tissue surrounded by hypoattenuating mucoperiosteum in the sinuses is suggestive of fungal infection, although it can also be seen with inspissated secretions and old polyps. Bony erosion is well demonstrated on CT scans. The following are the patterns of sinus inflammation on CT scans: (1) polyps; (2) fungal sinusitis; (3) mucocele; (4) sinusitis, which can occur as sinonasal polyposis or in an infundibular, osteomeatal unit, sphenoethmoidal recess, or sporadic or unclassifiable pattern; and (5) granulomatous sinusitis, which can be infectious (eg, due to tuberculosis, actinomycosis, rhinoscleroma, or leprosy) or noninfectious (eg, Wegener granulomatosis, sarcoid). With fungal sinusitis, the maxillary and ethmoid sinuses are most commonly involved. Allergic fungal sinusitis can involve complete opacification of multiple paranasal sinuses, unilateral or bilateral; sinus expansion and erosion of a wall of the involved sinus; or high-attenuating areas scattered amid mucosal thickening on nonenhanced scans. These areas are due to inspissated secretions or heavy metals such as iron, manganese, and calcium. Acute invasive fungal sinusitis can involve aggressive bone erosion with extension of disease into the adjacent soft tissues. Intrasinus high-attenuating areas may not be present in acute invasive fungal sinusitis. This condition may be associated with orbital, intracranial, and cheek soft-tissue invasion. Sinus mycetoma may cause a focal area of increased attenuation that is usually centered within a diseased sinus. Findings of acute sinusitis include an air-fluid level, mucosal thickening, and complete opacification of the sinus. Blood in the sinus due to recent trauma may mimic an airfluid level in the sinus, but it is easily distinguished by density measurements. In chronic sinusitis, the ethmoid sinus is commonly involved. Findings include mucosal thickening, complete opacification, bone remodeling and thickening due to osteitis, and polyposis. Mucoceles often occur in patients with chronic pansinusitis and nasal polyposis. The pathogenesis involves accumulation of mucoid secretions behind an obstructed paranasal sinus ostium with expansion of the sinus cavity and thinning of the sinus walls. The frontal sinuses account for about 60% of cases, ethmoid 30%, maxillary 10%; the sphenoid sinus is only rarely involved. Frontal sinus mucoceles may present with decreased visual acuity, visual field defect, proptosis, and intractable headaches. Conventional radiography shows a soft tissue density mass causing sinus cavity expansion, sometimes with bony erosion. Macroscopic calcification may be seen in 5% of cases, especially where there is superimposed fungal infection. Full assessment requires CT or MRI. CT techniques and indications CT techniques include thin-section, high-resolution, and coronal scanning for the evaluation of inflammatory sinonasal disease. Plain coronal scans are typically acquired with 2- to 3-mm sections and a high-frequency algorithm. Scans are obtained from the frontal sinus to the sphenoid sinus. Axial scans are not routinely necessary. Administration of antibiotics or antihistaminics may be required to permit scanning when patient has minimal symptoms. Having the patient blow his or her nose before scanning is useful for clearing mucus, and a prone position to drain fluid away from osteomeatal unit. Degree of Confidence The criterion standard imaging modality in the diagnosis of sinusitis is CT, which provides more detailed information about the anatomy and abnormalities of the sinuses than does plain radiography. The osteomeatal units are brilliantly shown on CT scans, which provide greater definition of the pathology than do other images, especially within the sphenoid and ethmoid sinuses. CT also provides the relationship of the sinuses to the orbit and the brain. This is an invaluable piece of information in any patient with rhinosinusitis that is severe enough to produce complications. The primary role of CT is to aid in the diagnosis and management of recurrent and chronic sinusitis and to define the anatomy of the sinuses prior to surgery. A nonenhanced coronal CT viewed in a bone window provides excellent resolution and good definition of the complete osteomeatal complex and other soft-tissue abnormalities seen in sinusitis. The coronal view is best correlated with findings from sinus surgery. Contrast-enhanced CT may be required in cases of acute sinusitis complicated by periorbital cellulitis or abscess. False Positives/Negatives CT findings should not be interpreted in isolation, and scans should always be read in conjunction with clinical and endoscopic findings because of high rates of false-positive results. Up to 40% of asymptomatic adults have abnormalities on sinus CT scans, as do more than 80% of those with minor upper respiratory tract infections. Dhong and associates evaluated the accuracy of diagnosing sinus fungus balls with CT and compared their results with operative findings. The sensitivity of CT evaluation was 62%, and the specificity was 99%. The false-positive and false-negative rates were 22% and 2%, respectively. The authors concluded that, to diagnose fungus ball, a high index of suspicion is necessary and pathologic confirmation is mandatory. In immunocompromised patients with invasive sinusitis, CT findings may be negative in the early stages. In advanced cases, differentiating this condition from malignancy may be difficult on the basis of imaging alone. Thus, the clinician cannot rely solely on CT imaging and must maintain a high index of suspicion when evaluating immunocompromised patients to establish a prompt diagnosis. Early nasal endoscopy with biopsy and the initiation of appropriate therapy are necessary to improve the patient's prognosis. Magnetic Resonance Imaging Findings CT remains the criterion standard modality in diagnosing sinusitis, but MRI is indicated with clinically suspected complications, especially in patients with intracranial complications and an extension of infection or in those with suspected superior sagittal venous thrombosis. Both diagnostic methods have improved the care and outcomes of patients who have sinusitis with complications. T1-weighted and fat-saturated T2-weighted coronal sequences are routinely performed. Axial T1- and T2-weighted and fat-saturated T2-weighted sagittal sequences may also be performed. Fluid is hypointense on T1-weighted images and hyperintense on T2-weighted images. Mucosal swelling may be confused with fluid on T2-weighted MRIs; however, on T1weighted MRIs, it stands out as soft tissue thickening against the fluid. Tumor tissue appears hypointense, as compared with mucosal swelling on T2-weighted images. Mucocele is hyperintense with both T1- and T2-weighted sequences because of its protein content. The signal intensity on MR depends on the age and degree of inspissation of the secretions. Older mucoceles will lose their T2 signal, then their T1 signal. Degree of Confidence MRI improves the differentiation of soft tissue, but it does not help in evaluating bones. MRI clearly depicts tumor from surrounding inflammatory tissue and secretions in the sinuses (see Findings, above). CT relies on the high contrast between air, soft tissue, and bone in evaluating the paranasal sinuses. Membrane, polyps, and mucous have similar attenuation, but the polypoid appearance helps in distinguishing the inflammatory polyps. On T2-weighted MRIs, the edematous membrane and mucous are distinctly hyperintense, whereas nasal polyps have more intermediate signal intensity. MRI cannot define bony anatomy as well as CT does. Other disadvantages of MRI include a high rate of false-positive findings and its higher cost. MRIs take considerably longer to acquire than CT scans, and they may be difficult to obtain in patients who are claustrophobic. False Positives/Negatives The false-positive rate with MRI is high. Abnormal sinus MRI findings are common among otherwise healthy adults, among children attending school, and among totally asymptomatic children. Incidental MRI findings should be interpreted as normal and do not indicate a need for treatment in children imaged for purposes other than the evaluation of sinus disease. Ultrasonography Findings In general, ultrasonography has not been thought to be useful in the diagnosis of sinusitis. However, several published works (Vento, 1999; Hilbert, 2001) have shown it to be more accurate than MRI or plain radiography in the diagnosis of maxillary sinusitis. When used in combination with radiography, sonograms can depict 86% of infections. Degree of Confidence A-mode ultrasonography has been a reliable tool in the diagnosis of acute maxillary sinusitis. However, controversy still exists regarding the reliability of A-mode ultrasonography in detecting fluid retention or mucosal swelling in patients with chronic polypous rhinosinusitis or in transantrally operated-on maxillary sinuses. Ultrasonography has several limitations in the diagnosis of sinusitis. Ultrasonography can result in a positive diagnosis in the presence of antral fluid, but sonograms do not define the cause of the fluid. Sonograms cannot provide information about bony detail, and the diagnosis of frontal, ethmoidal, and sphenoidal sinusitis is difficult. False Positives/Negatives Sonographic findings cannot be used to differentiate sinus disease from bacterial, viral, fungal, and allergic causes, as with most cross-sectional imaging. Nuclear Imaging Findings Javer and associates compared scintigraphy with indium Indium-111, gallium-67, and technetium-99m to differentiate acute infection from chronic inflammation involving bone (osteitis) and/or mucosa. This information was then used to guide management. Nuclear scintigraphy results were compared with CT and surgical findings. 111 In was the best isotope for identifying pus or acute disease in the sinuses, whereas67 Ga was good for identifying both chronic mucosal disease and acute disease.99m Tc was sensitive for identifying bony remodeling and therefore not useful if the patient had undergone previous sinus surgery. The authors concluded that scintigraphy should not be considered a first-line diagnostic test. Instead, nuclear scintigraphy is useful in cases in which CT results are nondifferentiating. Goshen and associates performed bone and gallium scans of the sinus regions in 32 patients presenting with frontal sinusitis. Bone scans classified according to99 Tc methylene diphosphonate (MDP) distribution patterns indicated active and resolving sinusitis, as well as surgery-related bone trauma. However, the intensity of gallium uptake was well correlated with the final outcome. This uptake was useful for differentiating between active and resolving sinusitis, with more specifically than that of the corresponding bone scans. Thus, combined studies may have a role in the diagnosis and management of frontal sinusitis. Degree of Confidence Radionuclide studies cannot be regarded as the primary modality in the imaging of sinusitis, but they have a place when cross-sectional imaging cannot differentiate between infection and other causes of mucosal disease. Gallium and labeled WBCs are both nonspecific agents and may be taken up in infections, inflammations, and tumors. False Positives/Negatives Roccatello and associates described facial uptake of111 In-labeled granulocytes in cases of Wegener granulomatosis mimicking sinusitis. Angiography Findings Non-inflammatory lesions in the sphenoid sinus are common. Therefore, thorough preoperative evaluation is imperative. The location and character of these lesions can be defined by means of nasal endoscopy and CT, and no other investigations may be necessary. In some patients, MRI may help further define the nature and extent of a lesion. Angiography should be considered if a vascular lesion is suspected. The clinical and imaging findings should all be taken into consideration when the surgical approach is planned (Martin, 2002). Mycotic aneurysms, cerebral infarction, brain abscess, and intracranial venous thrombosis are rare but well-known complications of sinusitis. Sphenoid sinusitis may invade adjacent intracranial vessels, and angiography may be required. Degree of Confidence Angiography is an invasive procedure, though it remains the criterion standard for depicting blood-vessel pathology. Most vascular evaluations can now be performed by using magnetic resonance angiography (MRA) or CT angiography (CTA). However, angiography may still be necessary for planning surgery and radiologic interventions, such as embolization of pseudoaneurysms. False Positives/Negatives Angiography provides little if any information regarding sinusitis itself. Although vascular invasion from extension of the sinus inflammatory process or venous thrombosis can be diagnosed reliably with angiography, such pathology has many causes that cannot be differentiated with angiography. Intervention Sinus puncture may be undertaken with the patient under local anesthetic to aspirate a small amount of fluid from the sinuses. The fluid is then cultured to determine what type of bacteria is causing sinusitis. Sinus puncture is performed only if a reasonable diagnosis cannot be made by using noninvasive techniques. Medicolegal Pitfalls Invasive forms of sinusitis and malignancy must be differentiated. Infection of the ethmoid air-cells when associated with bone erosion should be regarded as an ears, nose, and throat emergency because of the risk of spreading infection to the intracranial structures and orbit. Sinus infection in an immunocompromised patient needs aggressive emergency treatment. Multimedia Media file 1: Air-fluid level (arrow) in the maxillary sinus suggests sinusitis. (Enlarge Image) [ CLOSE WINDOW ] Air-fluid level (arrow) in the maxillary sinus suggests sinusitis. Media file 2: Accessory ostia in the medial walls of both maxillary sinuses with left maxillary sinusitis. (Enlarge Image) [ CLOSE WINDOW ] Accessory ostia in the medial walls of both maxillary sinuses with left maxillary sinusitis. Media file 3: Deviated nasal septum on a coronal highresolution CT scan. (Enlarge Image) [ CLOSE WINDOW ] Deviated nasal septum on a coronal high-resolution CT scan. Media file 4: Bilateral ethmoid sinusitis on an MRI. (Enlarge Image) [ CLOSE WINDOW ] Bilateral ethmoid sinusitis on an MRI. Media file 5: Concha bullosa of the right middle turbinate. (Enlarge Image) [ CLOSE WINDOW ] Concha bullosa of the right middle turbinate. Media file 6: Ethmoid sinusitis with intracranial extension and also extension into the left orbit. (Enlarge Image) [ CLOSE WINDOW ] Ethmoid sinusitis with intracranial extension and also extension into the left orbit. Media file 7: Paradoxical curves of both middle turbinates cause narrowing of the osteomeatal units. (Enlarge Image) [ CLOSE WINDOW ] Paradoxical curves of both middle turbinates cause narrowing of the osteomeatal units. Media file 8: Sinonasal polyposis. Soft tissues completely fill the maxillary and ethmoid sinuses and extend into the nasal cavities. (Enlarge Image) [ CLOSE WINDOW ] Sinonasal polyposis. Soft tissues completely fill the maxillary and ethmoid sinuses and extend into the nasal cavities. Media file 9: CT scan obtained after functional endoscopic sinus surgery (FESS) shows surgical defects in both nasal cavities in the form of excision of the entire right osteomeatal unit and the left uncinate process with residual left ethmoid and maxillary sinusitis. (Enlarge Image) [ CLOSE WINDOW ] CT scan obtained after functional endoscopic sinus surgery (FESS) shows surgical defects in both nasal cavities in the form of excision of the entire right osteomeatal unit and the left uncinate process with residual left ethmoid and maxillary sinusitis. Media file 10: Polypoid mucosal thickening in the right maxillary sinus with a mucous retention cyst in the left on a Waters view. (Enlarge Image) [ CLOSE WINDOW ] Polypoid mucosal thickening in the right maxillary sinus with a mucous retention cyst in the left on a Waters view. Media file 11: Right-sided sphenoethmoidal pattern of sinusitis. (Enlarge Image) [ CLOSE WINDOW ] Right-sided sphenoethmoidal pattern of sinusitis. Media file 12: Mucous retention cysts along the floor of the right and the anterior wall of the left maxillary sinuses. (Enlarge Image) [ CLOSE WINDOW ] Mucous retention cysts along the floor of the right and the anterior wall of the left maxillary sinuses. Media file 13: Mucosal thickening in the left anterior ethmoid and maxillary sinuses and in the region of the infundibulum. This indicates an osteomeatal pattern of sinusitis. (Enlarge Image) [ CLOSE WINDOW ] Mucosal thickening in the left anterior ethmoid and maxillary sinuses and in the region of the infundibulum. This indicates an osteomeatal pattern of sinusitis. Media file 14: Frontal mucocele. Expansion of the left frontal sinus indicated by low-attenuating soft tissues with thinning of the walls but no erosion. (Enlarge Image) [ CLOSE WINDOW ] Frontal mucocele. Expansion of the left frontal sinus indicated by low-attenuating soft tissues with thinning of the walls but no erosion. Media file 15: Fungal sinusitis. Soft tissues occupy the right maxillary and ethmoid sinuses with central hyperattenuating areas typical of fungal sinusitis. Medial walls of the affected sinuses are eroded. (Enlarge Image) [ CLOSE WINDOW ] Fungal sinusitis. Soft tissues occupy the right maxillary and ethmoid sinuses with central hyperattenuating areas typical of fungal sinusitis. Medial walls of the affected sinuses are eroded. Media file 16: MRI shows intraorbital extension of ethmoid sinusitis on the right side. (Enlarge Image) [ CLOSE WINDOW ] MRI shows intraorbital extension of ethmoid sinusitis on the right side. Media file 17: Axial MRI in the same patient as in Image 16 shows right intraorbital extension of sinusitis with medial displacement of medial rectus muscle. (Enlarge Image) [ CLOSE WINDOW ] Axial MRI in the same patient as in Image 16 shows right intraorbital extension of sinusitis with medial displacement of medial rectus muscle. Media file 18: Expansion of the left anterior ethmoid sinuses with thinned bit intact bony walls; these findings suggest a mucocele. (Enlarge Image) [ CLOSE WINDOW ] Expansion of the left anterior ethmoid sinuses with thinned bit intact bony walls; these findings suggest a mucocele. (Enlarge Image) References 1. Aalokken TM, Hagtvedt T, Dalen I, Kolbenstvedt A. Conventional sinus radiography compared with CT in the diagnosis of acute sinusitis. Dentomaxillofac Radiol. Jan 2003;32(1):60-2. [Medline]. 2. Bhattacharyya N, Fried MP. The accuracy of computed tomography in the diagnosis of chronic rhinosinusitis. Laryngoscope. Jan 2003;113(1):1259. [Medline]. 3. Chen MC, Davidson TM. Clinical evaluation of postoperative sinonasal surgical patients. Semin Ultrasound CT MR. Dec 2002;23(6):466-74. [Medline]. 4. Coates MH, Whyte AM, Earwaker JW. Frontal recess air cells: spectrum of CT appearances. Australas Radiol. Mar 2003;47(1):4-10. [Medline]. 5. Dhiwakar M, Thakar A, Bahadur S, et al. Preoperative diagnosis of allergic fungal sinusitis. Laryngoscope. Apr 2003;113(4):688-94. [Medline]. 6. Dhong HJ, Jung JY, Park JH. Diagnostic accuracy in sinus fungus balls: CT scan and operative findings. Am J Rhinol. Jul-Aug 2000;14(4):22731. [Medline]. 7. Dobson MJ, Fields J, Woodford T. A comparison of ultrasound and plain radiography in the diagnosis of maxillary sinusitis. Clin Radiol. Mar 1996;51(3):170-2. [Medline]. 8. El-Beltagi AH, Sobeih AA, Valvoda M, et al. Radiological appearances of sinonasal abnormalities. Clin Radiol. Aug 2002;57(8):702-18. [Medline]. 9. Eustis HS, Mafee MF, Walton C, Mondonca J. MR imaging and CT of orbital infections and complications in acute rhinosinusitis. Radiol Clin North Am. Nov 1998;36(6):1165-83, xi. [Medline]. 10. Garcia DP, Corbett ML, Eberly SM, et al. Radiographic imaging studies in pediatric chronic sinusitis. J Allergy Clin Immunol. Sep 1994;94(3 Pt 1):52330. [Medline]. 11. Ghatasheh M, Smadi A. Ultrasonography versus radiography in the diagnosis of maxillary sinusitis. East Mediterr Health J. Sep-Nov 2000;6(5-6):10836. [Medline]. 12. Goshen E, Zwas ST, Sadan M, Kronenberg J. The combined use of classified bone and gallium scans in the management of frontal sinusitis. Nucl Med Commun. May 1994;15(5):361-6. [Medline]. 13. Haapaniemi J. Comparison of ultrasound and X-ray maxillary sinus findings in school- aged children. Ear Nose Throat J. Feb 1997;76(2):102-6. [Medline]. 14. Hagtvedt T, Aalokken TM, Notthellen J, Kolbenstvedt A. A new low-dose CT examination compared with standard-dose CT in the diagnosis of acute sinusitis. Eur Radiol. May 2003;13(5):976-80. [Medline]. 15. Harrie RP. Imaging for sinusitis. JAMA. Dec 8 1993;270(22):2686-7. [Medline]. 16. Hilbert G, Vargas F, Valentino R, et al. Comparison of B-mode ultrasound and computed tomography in the diagnosis of maxillary sinusitis in mechanically ventilated patients. Crit Care Med. Jul 2001;29(7):1337-42. [Medline]. 17. Hurst RW, Judkins A, Bolger W, et al. Mycotic aneurysm and cerebral infarction resulting from fungal sinusitis: imaging and pathologic correlation. AJNR Am J Neuroradiol. May 2001;22(5):858-63. [Medline]. 18. Javer AR, Stevens HE, Stillwell M, Jafar AM. Efficacy of nuclear scintigraphy in the diagnosis and management of sinusitis. J Otolaryngol. Dec 1996;25(6):375-82. [Medline]. 19. Kristo A, Alho OP, Luotonen J, et al. Cross-sectional survey of paranasal sinus magnetic resonance imaging findings in schoolchildren. Acta Paediatr. 2003;92(1):34-6. [Medline]. 20. Laine K, Maatta T, Varonen H, Makela M. Diagnosing acute maxillary sinusitis in primary care: a comparison of ultrasound, clinical examination and radiography. Rhinology. Mar 1998;36(1):2-6. [Medline]. 21. Lee TG, Yoon HJ, Ha CK, et al. Cerebral venous thrombosis associated with maxillary and ethmoid sinusitis--a case report. J Korean Med Sci. Oct 1995;10(5):388-92. [Medline]. 22. Lichtenstein D, Biderman P, Meziere G, Gepner A. The "sinusogram", a realtime ultrasound sign of maxillary sinusitis. Intensive Care Med. Oct 1998;24(10):1057-61. [Medline]. 23. Martin TJ, Smith TL, Smith MM, Loehrl TA. Evaluation and surgical management of isolated sphenoid sinus disease. Arch Otolaryngol Head Neck Surg. Dec 2002;128(12):1413-9. [Medline]. 24. Mucha SM, Baroody FM. Sinusitis update. Curr Opin Allergy Clin Immunol. Feb 2003;3(1):33-8. [Medline]. 25. Okuyemi KS, Tsue TT. Radiologic imaging in the management of sinusitis. Am Fam Physician. Nov 15 2002;66(10):1882-6. [Medline]. 26. Ong YK, Tan HK. Suppurative intracranial complications of sinusitis in children. Int J Pediatr Otorhinolaryngol. Oct 21 2002;66(1):49. [Medline]. 27. Puhakka T, Heikkinen T, Makela MJ, et al. Validity of ultrasonography in diagnosis of acute maxillary sinusitis. Arch Otolaryngol Head Neck Surg. Dec 2000;126(12):1482-6. [Medline]. 28. Reilly JS, Hotaling AJ, Chiponis D, Wald ER. Use of ultrasound in detection of sinus disease in children. Int J Pediatr Otorhinolaryngol. Jul 1989;17(3):22530. [Medline]. 29. Revonta M, Blokmanis A. Sinusitis. Diagnostic methods. Can Fam Physician. Nov 1994;40:1969-72, 1975-6. [Medline]. 30. Roccatello D, Picciotto G, Gigliola G, et al. Indium-111-labeled granulocyte head accumulation in patients with Wegener''s granulomatosis. Am J Nephrol. 1995;15(6):500-6. [Medline]. 31. Rudralingam M, Jones K, Woolford TJ. The unilateral opaque maxillary sinus on computed tomography. Br J Oral Maxillofac Surg. Dec 2002;40(6):5047. [Medline]. 32. Shah A. Allergic bronchopulmonary and sinus aspergillosis: the roentgenologic spectrum. Front Biosci. Jan 1 2003;8:E138-46. [Medline]. 33. Skoulas IG, Helidonis E, Kountakis SE. Evaluation of sinusitis in the intensive care unit patient. Otolaryngol Head Neck Surg. Apr 2003;128(4):5039. [Medline]. 34. Varonen H, Makela M, Savolainen S, et al. Comparison of ultrasound, radiography, and clinical examination in the diagnosis of acute maxillary sinusitis: a systematic review. J Clin Epidemiol. Sep 2000;53(9):9408. [Medline]. 35. Vento SI, Ertama LO, Hytonen ML, Malmberg CH. A-mode ultrasound in the diagnosis of chronic polypous sinusitis. Acta Otolaryngol. 1999;119(8):91620. [Medline]. 36. Watkins LM, Pasternack MS, Banks M, et al. Bilateral cavernous sinus thromboses and intraorbital abscesses secondary to Streptococcus milleri. Ophthalmology. Mar 2003;110(3):569-74. [Medline]. 37. Younis RT, Lazar RH, Anand VK. Intracranial complications of sinusitis: a 15year review of 39 cases. Ear Nose Throat J. Sep 2002;81(9):636-8, 640-2, 644. [Medline]. 38. Vargas F, Boyer A, Bui HN, et al. A postural change test improves the prediction of a radiological maxillary sinusitis by ultrasonography in mechanically ventilated patients. Intensive Care Med. Jun 9 2007;[Medline]. 39. Chadha NK, Chadha R. 10-minute consultation: sinusitis. BMJ. Jun 2 2007;334(7604):1165. [Medline]. 40. Mafee MF. Imaging of paranasal sinuses and rhinosinusitis. Clin Allergy Immunol. 2007;20:185-226. [Medline]. 41. Thomas C, Aizin V. Brief report: a red streak in the lateral recess of the oropharynx predicts acute sinusitis. J Gen Intern Med. Sep 2006;21(9):9868. [Medline]. 42. Zinreich SJ. Progress in sinonasal imaging. Ann Otol Rhinol Laryngol Suppl. Sep 2006;196:61-5. [Medline]. Temporal Bone, Acquired Cholesteatoma Author: Salomon Waizel, MD, Associate Professor of Otolaryngology, Anahuac University; Consulting Surgeon, Department of Otolaryngology, Hospital De Especialidades, National Medical Center SXXI, IMSS Coauthor(s): Jose German Grandvallet, MD, Consulting Surgeon, Department of Otolaryngology, Medica Sur Medical Center, Mexico; Anil Khosla, MBBS, Assistant Professor, Department of Radiology, Section of Neuroradiology, Mallinckrodt Institute of Radiology, Washington University School of Medicine, Veterans Affairs Medical Center of St Louis Contributor Information and Disclosures Updated: May 1, 2007 Print This Email This Overview Imaging Follow-up Multimedia References Keywords Introduction Background A cholesteatoma consists of an accumulation of desquamated keratin epithelium in the middle ear cleft or any other pneumatized portion of the temporal bone. The envelope of a cholesteatoma is termed a matrix, and desquamated keratin is shed continually by the matrix and forms the central mass of the cholesteatoma, similar to the layers of an onion. The term cholesteatoma is a misnomer, since the entity does not contain cholesterol. Pathophysiology Cholesteatomas are classified as congenital or acquired, and acquired cholesteatomas are subdivided into primary (attic retraction) or secondary categories. Derlacki defines congenital cholesteatomas as an embryonic remainder of epithelial tissue in the ear, without either tympanic membrane perforation or history of infection.1 Primary acquired cholesteatomas appear as a defect of variable size adjacent to the posterosuperior portion of the tympanic membrane (pars flaccida). The center of the defect contains keratin debris. In secondary acquired cholesteatomas, the keratin epithelium has migrated through a tympanic membrane perforation. Cholesteatomas may be limited to the external auditory canal. They present as limited lesions lateral to the normal tympanic membrane; they erode the tympanic bone in older patients with otorrhea and no hearing loss. Cholesteatoma should be differentiated from keratosis obturans, which is of unknown etiology and is characterized by a large amount of cerumen and keratin filling the external ear canal; keratosis obturans produces otalgia, hearing loss, and otorrhea, usually with bilateral involvement and erosion of the external canal in younger patients. Cholesteatoma can erode bone. Multinucleated osteoclasts within the subepithelial matrix release acid phosphatase, collagenase, and other proteolytic enzymes. The osteoclast may be activated further by infection, water contamination, pressure, and Langerhans cells. Frequency United States The prevalence of acquired cholesteatoma in the United States is unknown. Congenital cholesteatoma is extremely rare. Mortality/Morbidity As cholesteatomas expand and become infected, they cause ossicular chain destruction, exposure of the membranous labyrinth, exposure of the facial nerve and dura, and infection of the mastoid and intracranial spaces. Intratemporal and intracranial infections occur in less than 1% of all cholesteatomas because of the widespread use of antibiotics and the tendency to operate earlier. Patients who develop headaches on the same side in which a cholesteatoma has developed should undergo computed tomography (CT) scanning to exclude an impending intracranial complication. Hearing loss - Ossicular chain erosion occurs in 30% of patients with cholesteatoma. Attic cholesteatomas involve the head of the malleus and body of the incus early. Labyrinthine fistula - A labyrinthine fistula may be found in as many as 10% of patients with long-standing cholesteatoma or in revision cases. A fistula is suggested in patients with chronic ear disease who have sensorineural hearing loss and/or vertigo induced by noise or pressure changes in the middle ear. Suppurative labyrinthitis with complete hearing loss and vestibular function may occur secondary to a fistula from a cholesteatoma. High-resolution thin-section CT scanning of the temporal bone may reveal a fistula of the semicircular canals or the basal turn of the cochlea. Fistulae of the horizontal semicircular canal are most common. Facial paralysis - Facial paralysis in patients with a cholesteatoma may develop acutely, secondary to infection, or slowly, as a result of chronic expansion. High-resolution thin-section CT images with both axial and coronal scanning localize the involvement. Topographic testing may confirm the site of injury. The most common site of paralysis is the geniculate ganglion. Race Racial prevalence has not been proven. Sex In congenital cholesteatoma, the male-to-female ratio is 3:1. Age Levenson et al have established an average age at presentation of 4.5 years for patients with congenital cholesteatoma.2 Anatomy Pathologic anatomy Acquired cholesteatoma appears similar to a gray or yellowish pearl and is perfectly defined in the middle-ear cavity. In almost every patient, a lesion of the ossicular chain and of the scutum (lateral wall of the attic) is noted. Surgical anatomy The middle ear is divided into 3 compartments as follows: The mesotympanum is the portion of the middle ear that is between the horizontal plane traced at the superior and inferior border of the pars tensa. It contains the stapes, the manubrium of the malleus, the long process of the incus, and the oval and round windows. The epitympanum is the portion of the middle ear that is above the level of the short process of the malleus. It contains the head of the malleus, the body of the incus, mucosal folds, and ligaments. The hypotympanum is the portion that is below the floor of the external ear canal. According to Jackler, the most common locations of origin of acquired cholesteatomas in order of descending frequency are the posterior epitympanum, posterior mesotympanum, and anterior epitympanum.3 Middle-ear pouches and spaces are related to the tympanic membrane and the cholesteatoma. The Prussak space is also termed the anterior recess of the tympanic membrane and is located between the pars flaccida and the neck of the malleus. The lateral mallear fold is the superior limit and is attached to the bony margin of the notch of Rivinus and the lateral process of the malleus as the inferior limit. The posterior von Troeltsch space is also termed the posterior recess of the tympanic membrane; it is a pouch lying between the tympanic membrane and the posterior mallear fold. The chorda tympani nerve lies in the free margin of the posterior mallear fold. The anterior pouch of von Troeltsch lies between the portion of the drumhead anterior to the malleus handle and the anterior mallear fold. Four sinuses are found at the posterior tympanic wall (ie, the sinus tympani, the lateral tympanic sinus, the posterior tympanic sinus, and the facial sinus). In chronic middleear disorders, the facial sinus always is found to contain pathologic tissue. Presentation The diagnosis of acquired cholesteatoma is made after a complete history is elicited and a physical examination is performed. Symptoms may vary. Some patients with cholesteatomas are asymptomatic, while other patients present with long-standing, malodorous otorrhea and conductive hearing loss. Some patients ignore the disease until impending complications develop, which are characterized by the onset of otalgia, vertigo, headache, facial nerve paresis, or meningitis. The treatment of acquired temporal-bone cholesteatoma is surgical. The 2 principal surgical techniques used are called canal wall up and canal wall down; the terms relate to the treatment of the posterior external auditory canal wall. The surgeon must determine the best procedure based on local factors, such as the extent of disease or the presence of complication, and on general factors, such as the medical condition of the patient and the surgeon's own skill and experience. Preferred Examination Otoscopic examination is the most important diagnostic technique. In primary acquired cholesteatoma, a retraction pouch is seen in the attic and contains keratin debris. In secondary acquired cholesteatoma, a tympanic membrane perforation is seen in which the epithelium has migrated through the borders and already has reached the middle-ear space. In an infected cholesteatoma, moderate fetid secretions with osteitis and granulation tissue are seen; these can be in the form of inflammatory aural polyps. Conventional temporal-bone projections and special imaging procedures, such as highresolution CT scanning and magnetic resonance imaging (MRI), are employed to complement physical examination and to determine the extent of the disease process, being utilized preoperatively to plan surgical treatment. CT scanning and MRI are useful when revision surgery is performed. High-resolution CT scanning in the axial and coronal planes is the imaging procedure of choice in the diagnosis of temporal-bone cholesteatomas. Limitations of Techniques Basically, conventional radiographic studies exhibit great limitations because of the complex anatomy of the temporal bone and the subtle changes induced by small cholesteatomas. CT scans also have limitations. With CT, it is difficult to differentiate a cholesteatoma from granulation tissue, pus, and fluid, which are present in chronic otitis media without the presence of a cholesteatoma. The principal limitation of MRI is the lack of bone conspicuity and detail due to the lack of mobile protons in dense cortical bone and signal void experienced when a radiofrequency pulse is applied. Because the major changes induced by a cholesteatoma in the temporal bone are produced within the bony framework, MRI has only a supportive role in the evaluation of subjacent extension of disease outside the confines of the temporal bone, intracranial extension, or rare vascular insult that may occur in large, chronic, or relapsing cases. The high cost of advanced technology imaging presents a major limitation in public institutions and developing countries. Differential Diagnoses Glomus Tumor (Head and Neck) Temporal Bone, Fractures Other Problems to Be Considered Middle ear - Tympanic membrane perforation and benign tumor Inner ear - Presbycusis and evaluation for dizziness Aural atresia Otitis media - Pediatric cases and complications Kartagener syndrome Patulous eustachian tube Mastoiditis Skull base - Petrous apex infection Residual and relapsing cholesteatomas must be differentiated following surgery. Relapsing cholesteatoma is defined as a pathologic mass that reappears from the keratin epithelium that was not removed during surgery. Recurrent cholesteatoma appears because of the incapacity of the eustachian tube to ventilate the temporal bone. Austin (personal communication) has proposed that the term relapsing cholesteatoma be used for both forms because of the difficulty in differentiating the 2 cholesteatomas based on clinical examination. This would allow uniform use of the term in the literature. CT scanning is one of the best tools for making the diagnosis of relapsing cholesteatoma. CT imaging is convenient 18-24 months after a canal-wall-up procedure (conservative) is performed. CT scanning uses axial and coronal views without the intravenous administration of contrast material. Radiography Findings Conventional temporal-bone projections remain in use in many parts of the world where CT scanning and MRI are not available. Standard projections for the temporal bone include the Law, Schuller, Mayer, Owen, Chausse III, transorbital, Stenvers, submentovertical, and Towne views. Schuller, Stenvers, Towne, and submentovertical projections are the most useful in the diagnosis of acquired cholesteatoma of the temporal bone. The Schuller view is a lateral view of the mastoid, obtained with the sagittal plane of the skull parallel to the film and with 30º-cephalocaudal angulation on the radiographic beam. This view shows the degree and extent of mastoid pneumatization, the status of the trabecular pattern, and the position of the lateral sinus. The Stenvers view is obtained with the patient facing the film and the head slightly flexed and rotated 45º toward the side opposite the examination. The radiographic beam is angulated 14º caudad. The long axis of the petrous pyramid is parallel to the plane of the film, and the entire pyramid, including its apex, is well visualized. This view shows the entire pyramid, arcuate eminence, internal auditory canal, porus acusticus, horizontal and vertical semicircular canals, vestibule, cochlea, mastoid antrum, and mastoid tip. The submentovertical view (also termed axial or basal) is obtained from under the chin and has the advantage of showing both temporal bones on the same image. In this view, the external auditory canal, eustachian tube, middle ear (including the incus and the head of the malleus), mastoid air cells, styloid process, internal auditory canal, and petrous apex are visualized. This view also demonstrates the foramen ovale, foramen spinosum, and jugular foramen from the base of the skull. The Towne view is an anteroposterior projection with a 30º tilt. As in the submentovertical view, it allows comparison of both petrous pyramids and mastoids in the same image. The petrous apex, internal auditory canals, arcuate eminence, mastoid antrum, and mastoid process can be identified clearly. High-technology imaging modalities have become the radiologic methods of choice in the study of acquired temporal-bone cholesteatoma. Degree of Confidence Degree of confidence in radiography is low because of the complex anatomy of the temporal bone and the small radiologic changes induced by pathologic conditions. Interpretation of findings always depends on the experience of the physician. False Positives/Negatives The false-negative rate with plain radiographs is high. Computed Tomography Findings CT-scanning technique Direct thin-section CT scanning in axial and coronal planes is a must for optimal evaluation of temporal-bone anatomy and pathology. Axial images are obtained parallel to the infraorbitomeatal line to reduce the radiation dose to the lens of the eye. Direct coronal images can be obtained in supine hanging-head position or prone with the neck extended. Axial images should include the top of the petrous apex to the inferior tip of the mastoid, and coronal images should be obtained from the anterior margin of the petrous apex to the posterior margin of the mastoid. Contiguous 1- to 1.5-mm-thick sections should be obtained by using conventional sequential acquisition. A spiral technique may be used if a pitch of 1:1 also is used. A small (12-cm) field of view can be applied with scans for each ear, reconstructed separately by using a bone algorithm. Intravenous contrast enhancement is usually not required. High-resolution CT scanning is ideal for the evaluation of middle-ear pathology. Contrast-enhanced CT scanning also is useful, if an intracranial complication is suspected and/or if a brain hernia (encephalocele) is present in the bed of the revision surgery. Recent advanced technology, such as multidetector-row scanning with submillimeter (0.5-mm) section thickness and high-speed rotation (0.5 second per rotation), has reinforced the benefits of CT scanning in assessing temporal-bone cholesteatomas. Applications of CT scanning CT scanning offers high-resolution images with a section thickness of approximately 1 mm, which allows for good visualization of the bony, ossicular, and innerear anatomies. On CT scans, good contrast is demonstrated for bone, soft tissue, and air. CT scanning is the preferred method for evaluating chronic middle-ear disease, including acquired cholesteatoma, because of its ability to demonstrate bony destruction. CT scanning is used to establish the surgical procedure needed in each patient. CT scanning helps to determine the extent of the cholesteatoma; the location and size of the sac; the status of the ossicular chain; the integrity of the facial canal, tegmen, and sinus plate; and the position of the dura, sigmoid sinus, and jugular bulb. CT-scan findings CT-scan findings in acquired temporal-bone cholesteatoma are characterized by a softtissue homogeneous mass with focal bone destruction. Cholesteatoma almost always presents as a complication of chronic otitis media; therefore, the middle-ear space appears cloudy as a result of granulation tissue, pus, and fluid. Liu and Bergeron have proposed the following CT-scan findings in cholesteatoma:4 Erosion and destruction of the lateral wall of the attic (scutum) Widening of the aditus ad antrum Displacement of the ossicular chain Destruction of the ossicles Labyrinthine fistula Erosion of the facial canal Dehiscence of the tympanic roof (tegmen tympani) Destruction of the mastoid (automastoidectomy cavity) Dehiscence of the sigmoid plate Erosion of the roof of the external auditory canal (posterosuperior wall) Degree of Confidence CT scanning is considerably more sensitive than conventional radiography for detecting cholesteatomas. False Positives/Negatives Granulation tissue and a chronically infected middle-ear mucosa are almost impossible to differentiate from a cholesteatoma. Magnetic Resonance Imaging Findings MRI technique Optimal MRI technique depends on the clinical situation and age of the patient. High field-strength, contrast-enhanced imaging in the axial and coronal plane has been considered the criterion standard for evaluation of the internal auditory canal (IAC) and inner-ear structures. Nonenhanced and gadolinium-contrast-enhanced T1-weighted images are compared in order to differentiate bright lesions (fat and blood products) from enhancing lesions visualized after contrast infusion. Three-dimensional (3D) fast spin-echo T2-weighted images allow high-resolution imaging of the IAC and labyrinth. A variety of 3D gradient-echo techniques with thin sections also are available. Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have been linked to the development of nephrogenic systemic fibrosis (NSF), also known as nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Fibrosing Dermopathy. The disease has occurred in patients with moderate to end-stage renal disease after they were given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography scans. As of late December 2006, the FDA had received reports of 90 such cases. Worldwide, over 200 cases have been reported, according to the FDA. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of theeyes;jointstiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape. Applications of MRI The role of MRI in the evaluation of middle-ear pathology is limited. The most important contributions of MRI to the study of acquired temporal-bone cholesteatoma are the following: MRI can precisely define the borders of large lesions. MRI can depict the relationship of the lesion to intracranial structures. MRI helps in evaluating intratemporal and extratemporal complications. Follow-up of patients who have undergone middle-ear surgery for a cholesteatoma MRI defines the integrity of the dura, which is best appreciated with T2-weighted sequences, without the need for contrast material. However, in cases of dural infection, subtle contrast enhancement may be the only clue that dural involvement is present. MRI delineates intracranial extension of the cholesteatoma or protrusion of the intracranial contents into the middle ear, when defects of the tegmen tympani or sinus plate are visualized on the CT scan. MRI is also indicated when the facial nerve is involved. MRI findings Acquired cholesteatomas generally produce low signal intensity on T1-weighted images, with no change after contrast administration, and high signal intensity on T2weighted images. MRI is also used to differentiate cholesteatomas from other temporal-bone lesions, such as cholesterol granulomas, granulation tissue, inflammatory mucosa, and scar tissue. Cholesterol granulomas produce high signal intensity on both sequences, with no contrast enhancement. Granulation tissue and inflammatory mucosa generally produce a hypointense or intermediate signal on T1-weighted images and a hyperintense signal on T2-weighted images with contrast enhancement. Because of its fibrous nature and, possibly, the microvascular thrombosis phenomenon, it is necessary to obtain delayed contrast-enhanced images with a delay of 30–45 minutes after contrast-material administration. Organized scar tissue produces a hypointense intermediate signal on T1- and T2weighted images with no contrast enhancement. A study by Frederique Dubrulle shows the reliability of diffusion-weighted fast spinecho MR imaging in the detection of recurrent cholesteatoma in patients who have undergone middle-ear surgery.5 Recurrent cholesteatoma was diagnosed if the lesion had low signal intensity on unenhanced T1-weighted images, showed no change in signal intensity on delayed contrast-enhanced T1-weighted images, and had high signal intensity on diffusion-weighted images obtained with a b factor of 800 sec/mm2. The negative predictive value was 100%, which means that patients who show no signs of recurrent cholesteatoma on diffusion-weighted fast spin-echo images may not need second-look surgery Degree of Confidence MRI is considerably more sensitive than conventional radiography, but it is less sensitive than high-resolution CT scanning, because of the lack of bone delineation on MRI. Intervention The treatment of temporal-bone acquired cholesteatomas is surgical. Two principal techniques are used, depending on the decision regarding how to manage the posterior external auditory canal wall. The canal-wall-up procedure involves preserving the posterior canal wall with or without a posterior tympanotomy. The posterior tympanotomy is performed through a triangle bounded by the fossa incudis, facial nerve, and chorda tympani nerve. The canal-wall-down procedure involves taking down the posterior canal wall to the vertical facial nerve and marsupializing the mastoid into the external ear canal. Canal-wall-down procedures can be divided into those in which the middle-ear space is preserved (modified radical mastoidectomy) and those in which the middle-ear space is eliminated and the eustachian tube plugged (radical mastoidectomy). Medicolegal Pitfalls Failure to diagnose a cholesteatoma is a pitfall. Patients often believe that the diagnosis should have been made earlier and specific treatment should have been initiated. Misdiagnosis or delay in diagnosis results in a higher morbidity rate. Documenting cholesteatoma complications is important during the first patient visit because the complications of tympanomastoid surgery are similar to those produced by the cholesteatoma (eg, facial palsy, hearing loss) an Multimedia Media file 1: Coronal high-resolution computed tomography scan shows a cholesteatoma in the posterior epitympanum (blue arrow), erosion of the scutum (white arrow), and rectification of the cochlea (red arrow). (Enlarge Image) [ CLOSE WINDOW ] Coronal high-resolution computed tomography scan shows a cholesteatoma in the posterior epitympanum (blue arrow), erosion of the scutum (white arrow), and rectification of the cochlea (red arrow). Media file 2: Temporal bone, acquired cholesteatoma. Epitympanic cholesteatoma. Coronal high-resolution CT scan of the right ear shows an eroded scutum and a softtissue mass between the ossicular chains. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Epitympanic cholesteatoma. Coronal high-resolution CT scan of the right ear shows an eroded scutum and a soft-tissue mass between the ossicular chains. Media file 3: Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows a right epitympanic cholesteatoma, with erosion of the tegmen, ossicular chain (1), and facial nerve (2). (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows a right epitympanic cholesteatoma, with erosion of the tegmen, ossicular chain (1), and facial nerve (2). Media file 4: Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows a soft-tissue mass in the epitympanum and over the oval window, an eroded scutum (red arrow), and an atelectatic tympanic membrane. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows a soft-tissue mass in the epitympanum and over the oval window, an eroded scutum (red arrow), and an atelectatic tympanic membrane. Media file 5: Temporal bone, acquired cholesteatoma. Multiple coronal CT scans show a soft-tissue mass (cholesteatoma) extending into the mastoid pneumatic system. The mastoid portion of the facial nerve (blue arrow) is seen. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Multiple coronal CT scans show a soft-tissue mass (cholesteatoma) extending into the mastoid pneumatic system. The mastoid portion of the facial nerve (blue arrow) is seen. Media file 6: Temporal bone, acquired cholesteatoma. Keratosis obturans. Coronal high-resolution CT scan shows destruction of the external auditory canal, lateral to the tympanic membrane (blue arrows), and accumulation of epithelium in the canal (red arrow). (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Keratosis obturans. Coronal highresolution CT scan shows destruction of the external auditory canal, lateral to the tympanic membrane (blue arrows), and accumulation of epithelium in the canal (red arrow). Media file 7: Temporal bone, acquired cholesteatoma. Keratosis obturans. Coronal CT scan shows a soft-tissue mass (epithelium) obstructing the external auditory canal (blue arrow). (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Keratosis obturans. Coronal CT scan shows a soft-tissue mass (epithelium) obstructing the external auditory canal (blue arrow). Media file 8: Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows a mastoid cavity (canal-wall-down mastoidectomy) in the left ear. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows a mastoid cavity (canal-wall-down mastoidectomy) in the left ear. Media file 9: Temporal bone, acquired cholesteatoma. Coronal CT of right cholesteatoma. A large soft-tissue mass in the right middle ear extending medial to the ossicles. The scutum is eroded and tympanic membrane is retracted. Note associated erosion of tegmen tympani. The normal left ear is shown for comparison. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal CT of right cholesteatoma. A large soft-tissue mass in the right middle ear extending medial to the ossicles. The scutum is eroded and tympanic membrane is retracted. Note associated erosion of tegmen tympani. The normal left ear is shown for comparison. Media file 10: Temporal bone, acquired cholesteatoma. Axial CT scan of left cholesteatoma. A soft-tissue mass in the middle ear with destruction of ossicles and erosion of the walls of middle ear cavity. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Axial CT scan of left cholesteatoma. A soft-tissue mass in the middle ear with destruction of ossicles and erosion of the walls of middle ear cavity. Media file 11: Temporal bone, acquired cholesteatoma. Axial CT scan of right cholesteatoma shows a large cavity in the right mastoid air cells; this is consistent with an automastoidectomy. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Axial CT scan of right cholesteatoma shows a large cavity in the right mastoid air cells; this is consistent with an automastoidectomy. Media file 12: Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows an epitympanic cholesteatoma with erosion of the tegmen tympani and probable herniation of brain tissue into the middle ear. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan shows an epitympanic cholesteatoma with erosion of the tegmen tympani and probable herniation of brain tissue into the middle ear. Media file 13: Temporal bone, acquired cholesteatoma. CT scan in the same patient as in Image 12. This more posterior image shows the integrity of the mastoid tegmen. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. CT scan in the same patient as in Image 12. This more posterior image shows the integrity of the mastoid tegmen. Media file 14: Temporal bone, acquired cholesteatoma. Axial MRI of the same patient as in Images 12-13 was used to identify the integrity of the brain tissue and a small right temporal-bone cholesteatoma. This produces a low signal intensity on T1-weighted images and high signal intensity on T2-weighted images and, sometimes, peripheral contrast enhancement. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Axial MRI of the same patient as in Images 12-13 was used to identify the integrity of the brain tissue and a small right temporal-bone cholesteatoma. This produces a low signal intensity on T1-weighted images and high signal intensity on T2-weighted images and, sometimes, peripheral contrast enhancement. Media file 15: Temporal bone, acquired cholesteatoma. Coronal MRI in the same patient as in Images 12-14. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal MRI in the same patient as in Images 12-14. Media file 16: Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan in a patient who underwent 3 previous otologic surgeries in the right ear. Image shows tegmen dehiscence and a mastoid cavity filled with soft-tissue attenuation of uncertain origin, which is probably brain-tissue herniation, residual cholesteatoma, or fibrosis. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal high-resolution CT scan in a patient who underwent 3 previous otologic surgeries in the right ear. Image shows tegmen dehiscence and a mastoid cavity filled with soft-tissue attenuation of uncertain origin, which is probably brain-tissue herniation, residual cholesteatoma, or fibrosis. Media file 17: Temporal bone, acquired cholesteatoma. Coronal T1-weighted MRI shows evident integrity of the dura without herniation of brain tissue (in the same patient as in Image 16). Gadolinium enhancement of the mastoid is seen; this corresponds with fibrosis seen at surgery. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal T1-weighted MRI shows evident integrity of the dura without herniation of brain tissue (in the same patient as in Image 16). Gadolinium enhancement of the mastoid is seen; this corresponds with fibrosis seen at surgery. Media file 18: Temporal bone, acquired cholesteatoma. Coronal CT scan in a 70-year-old patient with rightsided, long-standing, temporal-bone cholesteatoma. Image shows extensive erosion. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Coronal CT scan in a 70-year-old patient with right-sided, long-standing, temporal-bone cholesteatoma. Image shows extensive erosion. Media file 19: Temporal bone, acquired cholesteatoma. Contrast-enhanced coronal CT scan (in the same patient as in Image 18) was obtained to rule out intracranial complications. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Contrast-enhanced coronal CT scan (in the same patient as in Image 18) was obtained to rule out intracranial complications. Media file 20: Temporal bone, acquired cholesteatoma. Contrast-enhanced coronal CT scan (in the same patient as in Image 18) shows destruction of right tegmen tympani and dural enhancement. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Contrast-enhanced coronal CT scan (in the same patient as in Image 18) shows destruction of right tegmen tympani and dural enhancement. Media file 21: Temporal bone, acquired cholesteatoma. Contrast enhanced T1-weighted axial MRI in the same patient as in Image 20 shows an enhancing soft-tissue mass in the region of the right tegmen tympani. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. Contrast enhanced T1-weighted axial MRI in the same patient as in Image 20 shows an enhancing soft-tissue mass in the region of the right tegmen tympani. Media file 22: Temporal bone, acquired cholesteatoma. T1-weighted axial MRI in the same patient as in Image 18. Hypointense soft-tissue mass in the region of right tegmen tympani extends intracranially. (Enlarge Image) [ CLOSE WINDOW ] Temporal bone, acquired cholesteatoma. T1-weighted axial MRI in the same patient as in Image 18. Hypointense soft-tissue mass in the region of right tegmen tympani extends intracranially. Media file 23: Temporal bone, acquired cholesteatoma. T2-weighted axial MRI in the same patient as in Image 18. MRI shows a hyperintense mass in the region of right tegmen tympani with intracranial extension. (Enlarge Image) References 1. Derlacki EL, Clemis JD. Congenital cholesteatoma of the middle ear and mastoid. Ann Otol Rhinol Laryngol. Sep 1965;74(3):706-27. [Medline]. 2. Levenson MJ, Parisier SC, Chute P, et al. A review of twenty congenital cholesteatomas of the middle ear in children. Otolaryngol Head Neck Surg. Jun 1986;94(5):560-7. [Medline]. 3. Jackler RK. The surgical anatomy of cholesteatoma. Otolaryngol Clin North Am. Oct 1989;22(5):883-96. [Medline]. 4. Liu DP, Bergeron RT. Contemporary radiologic imaging in the evaluation of middle ear-attic-antral complex cholesteatomas. Otolaryngol Clin North Am. Oct 1989;22(5):897-909. [Medline]. 5. Dubrulle F, Souillard R, Chechin D, et al. Diffusion-weighted MR imaging sequence in the detection of postoperative recurrent cholesteatoma. Radiology. Feb 2006;238(2):604-10. [Medline]. [Full Text]. 6. Bowes AK, Wiet RJ, Monsell EM, et al. Brain herniation and space-occupying lesions eroding the tegmen tympani. Laryngoscope. Oct 1987;97(10):11725. [Medline]. 7. Daniels DL, Czervionke LF, Pojunas KW, et al. Facial nerve enhancement in MR imaging. AJNR Am J Neuroradiol. Jul-Aug 1987;8(4):605-7. [Medline]. 8. De Foer B, Vercruysse JP, Pilet B, et al. Single-shot, turbo spin-echo, diffusionweighted imaging versus spin-echo-planar, diffusion-weighted imaging in the detection of acquired middle ear cholesteatoma. AJNR Am J Neuroradiol. Aug 2006;27(7):1480-2. [Medline]. 9. Edelstein DR, Parisier SC. Surgical techniques and recidivism in cholesteatoma. Otolaryngol Clin North Am. Oct 1989;22(5):1029-40. [Medline]. 10. Farrior JB. Surgery for Cholesteatoma: Complications in Head and Neck Surgery. Toronto: BC Decker; 1986. 11. Gahbauer HW, Yanagisawa K, Yanagisawa E. Head and neck radiology. In: Lee KJ, ed. Essential Otolaryngology: Head and Neck Surgery. 7th ed. Norwalk, CT: Appleton & Lange; 1998. 12. Kodama T. [Temporal bone imaging]. Nippon Igaku Hoshasen Gakkai Zasshi. Sep 2000;60(11):549-59. [Medline]. 13. Levenson MJ, Michaels L, Parisier SC, et al. Congenital cholesteatomas in children: an embryologic correlation. Laryngoscope. Sep 1988;98(9):94955. [Medline]. 14. Michaels L. Biology of cholesteatoma. Otolaryngol Clin North Am. Oct 1989;22(5):869-81. [Medline]. 15. Proctor B. Cavities of the temporal bone. In: Surgical Anatomy of the Ear and the Temporal Bone. vol 1. New York, NY: Thieme Medical Publishers; 1989:39-85. 16. Ruben RJ. The disease in society: evaluation of chronic otitis media in general and cholesteatoma in particular. In: Sade J, ed. Cholesteatoma and Mastoid Surgery. Amsterdam: Kugler Publications; 1982. 17. Strunk CL. Cholesteatoma. In: Bailey BJ, Johnson JT, Newlands, SD, eds. Head and Neck Surgery--Otolaryngology. vol 2. Philadelphia, Pa: Lippincott Williams & Wilkins; 1993:1635-1646. 18. Swartz JD, Harnsberger HR. The middle ear and mastoid. In: Imaging of the Temporal Bone. 3rd ed. New York, NY: Thieme; 1998:47-169. 19. Williams MT, Ayache D, Alberti C, et al. Detection of postoperative residual cholesteatoma with delayed contrast-enhanced MR imaging: initial Le Fort Fractures Author: Anil R Shah, MD, Plastic Surgeon, Private Practice Coauthor(s): Galdino E Valvassori, MD, Professor of Radiology and Otolaryngology, University of Illinois at Chicago; Rita M Roure, MD, Staff Physician, Department of Otolaryngology-Head and Neck Surgery, New York University Medical Center Contributor Information and Disclosures Updated: Nov 10, 2008 Print This Email This Overview Imaging Multimedia References Keywords Introduction Le Fort fractures. [ CLOSE WINDOW ] Le Fort fractures. Coronal CT of a patient with right Le Fort III fracture and left Le Fort II fracture. [ CLOSE WINDOW ] Coronal CT of a patient with right Le Fort III fracture and left Le Fort II fracture. Bilateral pterygoid fractures. [ CLOSE WINDOW ] Bilateral pterygoid fractures. Axial picture. Note bilateral pterygoid plate fractures. [ CLOSE WINDOW ] Axial picture. Note bilateral pterygoid plate fractures. Three-dimensional reconstruction of a patient with right Le Fort I fracture and a left Le Fort II fracture. [ CLOSE WINDOW ] Three-dimensional reconstruction of a patient with right Le Fort I fracture and a left Le Fort II fracture. Coronal CT demonstrating a right Le Fort I fracture and a left Le Fort II fracture. [ CLOSE WINDOW ] Coronal CT demonstrating a right Le Fort I fracture and a left Le Fort II fracture. Le Fort fractures account for 10-20% of all facial fractures. They result from exposure to a considerable amount of force. Motor vehicle accidents are the predominant cause; other causes include assaults and falls. With seatbelt laws and the increased use of airbags by auto manufacturers, the overall incidence of midface fractures has decreased. Related eMedicine topics: Facial Trauma, Maxillary and Le Fort Fractures Facial Trauma, Frontal Sinus Fractures Facial Trauma, Mandibular Fractures Facial Trauma, Maxillary and Le Fort Fractures Related Medscape topics: Specialty Site Radiology Radiology CME and News Radiology Conferences Specialty Site General Surgery Resource Center Aesthetic Medicine Resource Center Resource Center Trauma Frequency United States Presentation Demographics Globally, the epidemiologies of midface fractures are similar. Young males are the typical patients, with motor vehicle accidents and assaults being the most common overall causes of facial and midfacial trauma. Male patients with midface fractures outnumber female patients with midface fractures by 5 to 1. Typically, these fractures affect younger males. The incidence of midface fractures is far lower in children than in adults, owing to anatomic differences and the overall elasticity of children's tissues.1,2,3 In a study from United Arab Emirates, the average age of patients with facial fractures was 26.5 years.4 The majority of patients (83%) were males. The most common cause was motor vehicle accidents (59%), followed by falls (21%). Of all the patients with facial fractures, 33% had isolated midface fractures, and 14% had a combination of midface fracture and mandibular fracture. In a study from China, 78.6% of midface fractures occurred in males; motor vehicle accidents were the leading cause (33%), followed by assaults (25%). In a study by Motamedi from Iran, 89% of maxillofacial trauma patients were male.5 Motor vehicle accidents were the number one cause (31%), followed by assaults (10%). Le Fort II fractures were the most common (55%), followed by Le Fort I fractures (24%) and Le Fort III fractures (12%). In a Turkish study on maxillofacial trauma by Aksoy et al, 83% of fractures occurred in males.6 The most common causes of facial fracture were motor vehicle accidents (90%) and assaults (3%). Presentation Because of the degree of force required to produce midface fractures, such injuries are often associated with a high incidence of serious intracranial and ophthalmologic injury. Le Fort fractures are often comminuted and are often associated with frontal or mandible fractures. Because of the accompanying injuries to the entire body, the standard trauma protocol of ABCs must be strictly followed before any intervention. Often, the midface fracture is of less immediate concern because of the severity of intracranial injury and associated bodily injuries. Because about one half of midface fractures are associated with significant cerebral edema and a low Glasgow Coma Scale score (<5), and because such patients have a poor prognosis, it is important to understand the goals of the family and the other medical teams involved in the care of the trauma patient. First of all, it is important to evaluate the airway early to rule out intraoral hemorrhage, edema, loose teeth, and posteroinferior displacement of the maxilla. Establishment of a safe airway is a priority; a tracheostomy may be needed if intubation proves to be impossible or unsafe for the patient. Bleeding may complicate midface fractures. If the bleeding is severe enough, packing of the midface vessels and temporary reduction of the fracture may be necessary. Angiography may be necessary to locate arterial bleeding from the internal maxillary before embolization. Obvious clinical signs of facial skeleton compromise include malocclusion, subcutaneous emphysema, abnormally mobile skeletal structures, and palpable stepoffs. Crepitus may be a result of paranasal sinus air leaking into the soft tissues of the face. Palpable step-offs are seen especially with zygomatic fractures. Associated facial fractures must be evaluated and ruled out. The patient's visual status, before and after traumatic insult, is vital in the treatment algorithm of midface fracture. There is a high incidence of visual problems associated with midface fractures, including enophthalmos, diplopia, entrapment, and epiphora. Epiphora occurs in 4% of Le Fort II or III fractures. CSF leakage is also seen, especially in Le Fort III fractures. Any persistent, clear rhinorrhea should be tested appropriately for CSF fluid leak. Patients may complain of paresthesias of the upper jaw because of damage to the superior alveolar nerve. As with all facial fractures, it is important to assess malocclusion. Patients may present with trismus and mouth pain. Palatal fractures often include a lip laceration and/or lacerations of the gingival and palatal mucosa. Patients with a palatal fracture may have an anterior open-bite deformity. Facial edema may obscure the facial examination, and step-offs may not be palpable. It is important to assess fracture mobility by palpating the anterior maxilla between the thumb and forefinger. Motion at the level of the anterior nasal spine without simultaneous motion is a sign of a Le Fort I fracture. Le Fort I fractures may be associated with gingival crepitation. Le Fort II fractures result in motion of the nasal pyramid along the medial orbit rims. The patient may have midface flattening and elongation. Le Fort II fractures often are associated with infraorbital paresthesias. In Le Fort III fractures, motion is seen at the zygomaticofrontal suture (craniofacial dysjunction). The patient may have anosmia resulting from fracture at the cribriform plate, as well as severe edema, or lengthening; this is known as a dish-face deformity. This is a result of the lack of sagittal projection from the face, causing it to lose its contours and look spherical. Midface fractures are usually not confused with other phenomena. The main concern is whether associated fractures are present. Examples include nasoethmoidal and orbitozygomatic fractures. These associated fractures are typically evident on examination or CT scanning. A history of trauma to the face and proper suspicion of imaging results should lead to the proper diagnosis.7,8 Denture wearers typically have additional protection from midface fracture. However, when fractures do occur, unusual fracture patterns are common. Lack of repair of the overlying soft tissue may result in descent and diastasis of the soft tissue of the face, leaving a flat or depressed area of the face. Hypesthesia of the infraorbital nerve is a common complaint. The infraorbital nerve is entirely sensory. If a neuroma develops or if the patient's pain becomes intolerable, resection of the nerve may be required Malocclusion is a common complaint. Molar occlusion is based on the angle classification of the first maxillary molar in relationship with its corresponding mandibular molar. When malocclusion occurs, additional osteotomies or orthognathic work may be required. Infection of the bone is always a concern. Any fracture with mucosal involvement of the nose, sinus, or mouth should be considered a compound fracture. These should be treated with the appropriate antibiotic coverage to prevent further complication. Le Fort classification system Rene Le Fort described the classic patterns of fracture in his 1901 work. Le Fort's experiments consisted of dropping cadaver skulls from several stories or striking them with a wooden club. He found 3 distinct fracture patterns, which he termed the linea minoros resistentiae. Simply stated, in the Le Fort I fracture, the palate is separated from the maxilla; in the Le Fort II fracture, the maxilla separates from the face; and in the Le Fort III fracture, craniofacial dysjunction is present. Le Fort fractures. The Le Fort I fracture is a low transverse fracture that crosses the floor of the nose, pyriform aperture, canine fossa, and lateral wall from the maxilla, resulting in separation of the palate from the maxilla. The Le Fort II fracture crosses the nasal bones on the ascending process of the maxilla and lacrimal bone and crosses the orbital rim. Only the Le Fort II fracture violates the orbital rim. Because of this proximity to the infraorbital foramen, type II fractures are associated with the highest incidence of infraorbital nerve hypesthesias. The Le Fort II fracture extends posteriorly to the pterygoid plates at the base of the skull. A Le Fort I fracture is characterized by a low septal fracture, whereas a Le Fort II fracture results in a high septal fracture. Finally, the Le Fort III fracture traverses the frontal process of the maxilla, the lacrimal bone, the lamina papyracea, and the orbital floor. This fracture often involves the posterior plate of the ethmoid. Because of their location, Le Fort III fractures are associated with the highest rate of cerebrospinal fluid (CSF) leaks.9,10,11 Shortcomings of the Le Fort classification system Despite its shortcomings, the Le Fort fracture classification system is still the most accepted method of classifying fractures and the location of osteotomies of the midface. However, recent studies have demonstrated that this classification system may be imprecise. The Le Fort fracture system is deficient in addressing most midface fractures because most midface fractures do not follow the simple Le Fort pattern of fracture; rather, a combination of Le Fort fractures is usually encountered. In addition, most midface fractures have some degree of comminution and are complicated by fractures and displacement not addressed in the Le Fort system. These midface fractures include palate, medial maxillary arch, dentoalveolar, and anterior maxillary fractures. Other classification systems Sagittal fractures of the palate occur in as many as 25% of all patients with fractures of the midface. They are not classified in typical Le Fort fracture terminology. However, Rene Le Fort did describe traumatic injuries to the palate in his series of papers on maxillary fractures. Palatal fractures were classified by Hendrickson et al, who described 6 types of palatal fractures, including the following: I, anterior and posterolateral alveolar; II, sagittal; III, parasagittal; IV, para-alveolar; V, complex; and VI, transverse. Palatal fractures are associated with Le Fort I fractures 100% of the time and with either Le Fort II/III or mandible fractures 50% of the time. There are many other classification systems for describing midface fractures. In the system of Donat et al, the face is divided into a matrix of vertical and horizontal beams, creating a lattice of 11 unilateral and 22 bilateral sites; this lattice is used to describe midface fractures.12 According to their preliminary data in 87 patients with midface fractures, this scheme enabled accurate transcription and communication among physicians 98% of the time. Another classification system is the Wassmund system. This system classifies fractures into grades I-V. A Wassmund I fracture is equivalent to a Le Fort II fracture. A Wassmund IV fracture is equivalent to a Le Fort III fracture. A Wassmund III fracture is characterized as a Le Fort III fracture without inclusion of the nasal bones. Manson described a facial fracture classification system on the basis of CT findings.13 He divided fractures into low- and high-impact fractures. His schema is described further in the CT Scan section below. Anatomy and natural history The maxilla has 4 processes: zygomatic, frontal, palatine, and alveolar. The maxillary sinus is housed within the maxilla and varies in size, depending on the degree of pneumatization. The midface can be thought of as a grid of horizontal and vertical buttresses that provide support for the face. The 3 paired vertical buttresses of the midface are the nasomaxillary, zygomaticomaxillary, and pterygomaxillary structures. The nasomaxillary buttress is formed by the lower maxilla, the frontal process of the maxilla, the lacrimal bone, and the nasal process of the frontal bone. The zygomaticomaxillary buttress is formed from the lateral portion of the maxilla, zygoma, and lateral portion of the frontal bone. The final buttress extends along the pterygoid plates to the skull base. The lone unpaired, vertical support mechanism is the nasal septum/ethmoid complex. The horizontal buttresses are composed of the alveolus, the hard palate, the inferior orbital rim, and the frontal bar. Horizontal buttresses have coronal and sagittal components. The sagittal buttresses are vital for facial projection. The midface is relatively deficient in sagittal buttresses. The skull base is at a 45° angle relative to the occlusal plane of the maxilla and may act as an axial buttress as well. Nahum revealed that low forces may create a fracture in the midface. This is partly the result of the presence of the large, air-filled sinus cavities. Therefore, the midface acts as a shock absorber. The midface is relatively resistant to vertically oriented forces (anteroposterior [AP] direction). The lateral forces may fracture the obliquely directed force vectors. The fractures may be of significant functional and aesthetic importance. Functional problems may lead to disorders of occlusion, nasal obstruction, and trigeminal-nerve sensation. Aesthetic losses include decreased midface height, facial width, facial projection, and malar eminence. These losses may lead to a dish-face deformity.14 Treatment All patients with midface fractures are given antibiotics, because these fractures are considered open or compound. Violation of the paranasal sinus or alveolus and open soft tissue wounds are inevitable sequelae of midface fractures. Antibiotics have been shown to decrease the incidence of infection after midface fractures. Typically, the earlier the repair of a midface fracture, the better the surgical result. This creates a dilemma for the midface reconstructive surgeon in that most patients with a midface fracture also have serious bodily injury. On the other hand, early repair prevents soft tissue scarring and memory from insetting, as well as fibrous malunion between the bony fragments. A long surgical procedure in a terminal patient is not desirable for the patient, the patient's family, or the surgeon. Also, an additional procedure in a patient who is in unstable condition may not be in the patient's best interests. Piotrowski and Brandt have elucidated some parameters for reconstructive surgeons to allow for safe early repair. If the intracranial pressure is less than 15 mm Hg, midface repair—early, intermediate, or late—does not negatively affect the patient's recovery. The radiologist and the reconstructive surgeon must communicate about the specific location of the fracture. Exposure is crucial in repair of the midface fracture. Generally speaking, a Le Fort I fracture is approached from a sublabial exposure; a Le Fort II fracture is approached with a combination of sublabial and periorbital exposure; and a Le Fort III fracture requires a combination of sublabial and bicoronal fracture for adequate exposure. The surgical approaches to fractures of the midface have changed radically in the past 20 years. The technology has now evolved to allow for miniplate fixation to the midface instead of bulky external hardware. Complex internal wiring was the standard of care 10 years ago, but because of poor cosmetic results and extended periods of IMF, newer technologies have replaced it. Miniplate technology involves the placement of strong titanium plates to bridge the fractured areas. The principle is similar to that of bridge making: Stable areas are fixed to unstable areas until the overall stability of the area has been secured. If large deficiencies are present, bone grafting may be necessary. For fractures involving large, displaced segments, the displaced segment may need to be pulled forward with a hook or index finger. If the fracture is impacted into adjacent bone and is immobile, a Rowe forceps may be useful. Nondisplaced midface fractures require little intervention. Usually, a short period of IMF is all that is needed. With any displacement, an open approach is typically required. A variety of midface fractures may be addressed effectively with a closed technique. Patients with nondisplaced, noncomminuted fractures are ideal candidates for a closed approach.15,16,17,18,19,20 Repair in pediatric patients is a controversial area. Midface fractures are relatively rare in children because of their flexible skeleton, underdeveloped sinuses, unerupted dentition, and proportionally large frontal bone and mandible. Unerupted dentition results in several challenges for the surgeon. The use of rigid fixation remains debatable. Animal experiments have shown that rigid fixation can lead to growth abnormalities. Some additional concerns are that an injury to the eyes or brain may happen due to slow movement of the plates. The counterargument is that not treating the bony injury can lead to significant permanent deformities. Differential Diagnoses Skull, Fractures Other Problems to Be Considered Associated fractures, such as nasoethmoidal and orbitozygomatic fractures Radiography Technique Plain radiographs are usually not ordered in complex trauma cases. The applicable plain images include facial bone series, which typically includes Waters, Stevens, and Townsend views. Panorex views are the best images for showing the orthognathic relationship and occlusion. Imaging pearls A Panorex view is especially helpful when associated mandible fractures are present. If there is concern with the possibility of a midface fracture, a CT scan is warranted. Plain radiographs have largely been replaced by CT scans for examining the midface. Computed Tomography Coronal CT of a patient with right Le Fort III fracture and left Le Fort II fracture. [ CLOSE WINDOW ] Coronal CT of a patient with right Le Fort III fracture and left Le Fort II fracture. Bilateral pterygoid fractures. [ CLOSE WINDOW ] Bilateral pterygoid fractures. Axial picture. Note bilateral pterygoid plate fractures. [ CLOSE WINDOW ] Axial picture. Note bilateral pterygoid plate fractures. Three-dimensional reconstruction of a patient with right Le Fort I fracture and a left Le Fort II fracture. [ CLOSE WINDOW ] Three-dimensional reconstruction of a patient with right Le Fort I fracture and a left Le Fort II fracture. Coronal CT demonstrating a right Le Fort I fracture and a left Le Fort II fracture. [ CLOSE WINDOW ] Coronal CT demonstrating a right Le Fort I fracture and a left Le Fort II fracture. Technique The preferred examination begins with a proper evaluation in the emergency department to ensure that the patient is stable and that the appropriate organ systems are treated in the necessary order. The preferred radiologic examination is CT scanning of the facial bones, with coronal and axial sections in bone windows for maximal detail. Midface fractures are best evaluated with CT imaging. Plain radiography and MRI play more limited roles in the evaluation of midfacial fractures.21 The imaging of choice for Le Fort fractures is CT scanning of the midface without contrast enhancement. It is important to analyze the whole face for fractures, including the entire mandible, because of the high rate of fracture of the upper and lower face when midface fractures occur. The CT scan is analyzed in bone windows; 2- to 3-mm sections are preferred. A singleplane CT scan does not provide as much information as a 2-plane CT scan. It is crucial to use a systematic analysis in analyzing midface fracture CT scans. Axial sections are best for analyzing the posterior wall of the antrum, the pterygoid plates, the hard palate, dentoalveolar segments, the zygomatic arch and body, and the lateral wall of the orbit. Coronal sections provide the best images for analyzing the anterior wall of the maxilla, the inferior orbital rim, the palate, and the orbital floor. Reformatted CT images are also of high quality and have been shown to be reliable and accurate in surgical reconstructive efforts. With the introduction of helical CT, which acquires data in a continuous fashion, it is now possible to produce computer-reformatted images, either coronal or sagittal, from the standard axial images. Coronal images reformatted from helically acquired thinsection axial CT data have been shown to have high sensitivity and specificity in the detection of fractures, as compared with direct coronal imaging. Three-dimensional (3D) reconstructions are usually not necessary in analyzing midface fractures. However, these reconstructions may be useful in highly complex fractures or secondary reconstructions and in facilitating communication between the radiologist and the surgeon. Cavalanti et al have shown that 3D construction is quantitatively accurate for surgical planning and evaluation. Three-dimensional reconstruction of a patient with a right Le Fort III fracture and left Le Fort II fracture. [ CLOSE WINDOW ] Three-dimensional reconstruction of a patient with a right Le Fort III fracture and left Le Fort II fracture. Interpretation Manson described a classification system in which fractures were classified as resulting from low-, middle-, or high-energy mechanisms; the determination of whether a fracture was the result of a log-, middle-, or high-energy mechanism was made on the basis of the degree of segmentation and displacement seen on CT scans.22 In Manson's system, fractures are classified according to the displacement and the degree of comminution. In type I fractures, there is minimal displacement and no comminution. In type II fractures, there is moderate displacement and a small amount of comminution. In type III fractures, there is severe displacement, with the major buttresses comminuted in multiple locations. This system may serve as a dependable guide for determining the prognosis and proper intervention. In making the radiologic report, it is important that damage to adjacent structures, such as the nasolacrimal duct, mandible, zygoma, and orbit, be commented upon. The degree of displacement and the degree of comminution may affect the surgical approach. The presence of any hardware may signify previous traumatic injury and repair.23,24,25 Accuracy CT scanning is the criterion standard for detecting facial fractures. It is superior to clinical examination, and it is more than 95% accurate. Sagittal reformatted helical CT scans are comparable in quality to direct sagittal scans. CT scanning of a facial bone results in few false-positive or false-negative results. Koltai et al (1999) applied Manson's energy classification with CT scanning in children and found that CT is an effective way of determining the severity of fracture. The more severe the fracture, the more likely a repair is necessary. Imaging Pearls CT is the criterion standard for evaluating midface trauma. CT is not as suitable as MRI for assessing soft tissue changes and acute intracranial changes. Misinterpretation of facial suture lines can cause an inexperienced examiner to diagnose facial fractures when none is present. Previous hardware and dental fillings can cause a scatter effect, making interpretation of fracture difficult in certain circumstances. Previously, an adequate examination of the cribriform plate, orbital roof, and orbital floor required images in the coronal plane, necessitating a direct coronal CT scan. However, to acquire a direct coronal CT scan, the cervical spine had to be cleared, and this wasted valuable time. Obtaining a direct coronal CT scan also increased costs, increased patient exposure to ionizing radiation, and required transport of a potentially unstable patient to the scanner itself. Magnetic Resonance Imaging Accuracy With regard to imaging the midface, the incidence of false-negative results are high with MRI, as compared with CT. Imaging pearls MRIs are typically not helpful in cases involving acute bony trauma to the face. If there is a question of soft-tissue injury to nervous structures, MRI may be helpful. MRI is typically performed 48 hours after trauma. The signal intensity of blood on T1-weighted images varies, depending on the age and location of the blood. Generally, a radiologist has a low degree of confidence in MRI findings when assessing a facial fracture. MRI plays an adjunctive role in the examination. MRI does have a role in cases involving intracranial injury or in cases in which unusual soft-tissue injury may be present. MRI is superior in the evaluation of brain and dural-space injury. Angiography Imaging pearl Angiography may be needed if there is concern about an associated injury to the carotid artery or internal maxillary artery (eg, to identify the site of arterial bleeding before embolization). Multimedia Media file 1: Le Fort fractures. (Enlarge Image) [ CLOSE WINDOW ] Le Fort fractures. Media file 2: Three-dimensional reconstruction of a patient with a right Le Fort III fracture and left Le Fort II fracture. (Enlarge Image) [ CLOSE WINDOW ] Three-dimensional reconstruction of a patient with a right Le Fort III fracture and left Le Fort II fracture. Media file 3: Coronal CT of a patient with right Le Fort III fracture and left Le Fort II fracture. (Enlarge Image) [ CLOSE WINDOW ] Coronal CT of a patient with right Le Fort III fracture and left Le Fort II fracture. Media file 4: Bilateral pterygoid fractures. (Enlarge Image) [ CLOSE WINDOW ] Bilateral pterygoid fractures. Media file 5: Axial picture. Note bilateral pterygoid plate fractures. (Enlarge Image) [ CLOSE WINDOW ] Axial picture. Note bilateral pterygoid plate fractures. Media file 6: Three-dimensional reconstruction of a patient with right Le Fort I fracture and a left Le Fort II fracture. (Enlarge Image) [ CLOSE WINDOW ] Three-dimensional reconstruction of a patient with right Le Fort I fracture and a left Le Fort II fracture. Media file 7: Coronal CT demonstrating a right Le Fort I fracture and a left Le Fort II fracture. (Enlarge Image) References 1. Iida S, Matsuya T. Paediatric maxillofacial fractures: their aetiological characters and fracture patterns. J Craniomaxillofac Surg. Aug 2002;30(4):23741. 2. Koltai PJ, Eames F, Selkin B. Midfacial Fractures in Children. Facial Plast Clinic of North Am. 1999;7:169-173. 3. Rehman K, Edmondson H. The causes and consequences of maxillofacial injuries in elderly people. Gerodontology. Jul 2002;19(1):60-4. [Medline]. 4. Klenk G, Kovacs A. Etiology and patterns of facial fractures in the United Arab Emirates. J Craniofac Surg. Jan 2003;14(1):78-84. 5. Motamedi MH. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. Jan 2003;61(1):61-4. [Medline]. 6. Aksoy E, Unlu E, Sensoz O. A retrospective study on epidemiology and treatment of maxillofacial fractures. J Craniofac Surg. Nov 2002;13(6):7725. [Medline]. 7. Rimell F, Marentette LJ. Injuries of the hard palate and the horizontal buttress of the midface. Otolaryngol Head Neck Surg. Sep 1993;109(3 Pt 1):499505. [Medline]. 8. Romano JJ, Manson PN, Mirvis SE, et al. Le Fort fractures without mobility. Plast Reconstr Surg. Mar 1990;85(3):355-62. [Medline]. 9. Gasparini G, Brunelli A, Rivaroli A, et al. Maxillofacial traumas. J Craniofac Surg. Sep 2002;13(5):645-9. [Medline]. 10. Thomas SH. Maxillofacial injuries. In: Harwood Nuss, ed. The Clinical Practice. Philadelphia: Lippincott Williams & Wilkins;. 1996: 408-18. 11. Fraioli RE, Branstetter BF 4th, Deleyiannis FW. Facial fractures: beyond Le Fort. Otolaryngol Clin North Am. Feb 2008;41(1):51-76, vi. [Medline]. 12. Donat TL, Endress C, Mathog RH. Facial fracture classification according to skeletal support mechanisms. Arch Otolaryngol Head Neck Surg. Dec 1998;124(12):1306-14. [Medline]. 13. Manson PN, Clark N, Robertson B, et al. Subunit principles in midface fractures: the importance of sagittal buttresses, soft-tissue reductions, and sequencing treatment of segmental fractures. Plast Reconstr Surg. Apr 1999;103(4):1287-306; quiz 1307. [Medline]. 14. Hoffman GR, Islam S. The difficult Le Fort I osteotomy and downfracture: a review with consideration given to an atypical maxillary morphology. J Plast Reconstr Aesthet Surg. Jun 16 2008;[Medline]. 15. Abramson DL, Vander Woude DL, Orgill DP, Pribaz JJ. Traumatic avulsion and reconstruction of the midface. J Craniomaxillofac Trauma. Spring 1996;2(1):614. [Medline]. 16. Derdyn C, Persing JA, Broaddus WC, et al. Craniofacial trauma: an assessment of risk related to timing of surgery. Plast Reconstr Surg. Aug 1990;86(2):23845; discussion 246-7. [Medline]. 17. Tian W, Li S, Pan J, et al. [Surgical reduction and rigid internal fixation of midface fractures]. Hua Xi Kou Qiang Yi Xue Za Zhi. May 1999;17(2):1369. [Medline]. 18. Dhol WS, Reyneke JP, Tompson B, Sándor GK. Comparison of titanium and resorbable copolymer fixation after Le Fort I maxillary impaction. Am J Orthod Dentofacial Orthop. Jul 2008;134(1):67-73. [Medline]. 19. Dolanmaz D, Esen A, Emlik D, Candirli C, Kalayci A, Ci¸ce¸kcibas¸i A. Comparison of two different approches to the pterygomaxillary junction in Le Fort I osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. Jul 7 2008;[Medline]. 20. Ueki K, Hashiba Y, Marukawa K, Nakagawa K, Alam S, Yamamoto E. The evaluation of surgical factors related to recovery period of upper lip hypoaesthesia after Le Fort I osteotomy. J Craniomaxillofac Surg. May 15 2008;[Medline]. 21. Laine FJ, Conway WF, Laskin DM. Radiology of maxillofacial trauma. Curr Probl Diagn Radiol. Jul-Aug 1993;22(4):145-88. [Medline]. 22. Manson PN, Glassman D, Vanderkolk C, et al. Rigid stabilization of sagittal fractures of the maxilla and palate. Plast Reconstr Surg. May 1990;85(5):7117. [Medline]. 23. Buitrago-Tellez CH, Schilli W, Bohnert M, et al. A comprehensive classification of craniofacial fractures: postmortem and clinical studies with two- and threedimensional computed tomography. Injury. Oct 2002;33(8):651-68. [Medline]. 24. Chen WJ, Yang YJ, Fang YM, et al. Identification and classification in le fort type fractures by using 2D and 3D computed tomography. Chin J Traumatol. Feb 2006;9(1):59-64. [Medline]. 25. Nan X, Fan Y, Li R, Wu Z. [Clinical application of three-dimensional spiral CT in the complexmaxillofacial fractures]. Hua Xi Kou Qiang Yi Xue Za Zhi. Dec 2001;19(6):372-4. [Medline].