The Unethical Tuskegee Syphilis Study
advertisement

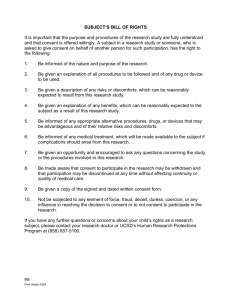
The Unethical Tuskegee Syphilis Study Dr. Joseph Costa, DHSc., PA-C Health Policy and Management MPH 525 Tracy Liichow June 2014 Table of Contents Chapter Page 1. Introduction ................................................................................................................................ 3 2. The Tuskegee Syphilis Study..................................................................................................... 5 3. Consent ...................................................................................................................................... 8 4. Summary and Recommendations ............................................................................................ 11 Summary ........................................................................................................................... 11 Recommendations ............................................................................................................. 12 References ..................................................................................................................................... 13 3 Chapter 1 Introduction The United States Public Health Service (USPHS) has some outstanding accomplishments. There have also been times of abuse of power and even hubris. The Tuskegee Syphilis Study is a black-eye on the face of public health. It was an experiment done on unknowing African American males, who had late stage syphilis over a period of 40 years. They were not informed participants. They were not given treatment for the disease. “The Tuskegee study of untreated syphilis in the Negro male is the longest nontherapeutic experiment on human beings in medical history” (S. B. Thomas & Quinn, 1991, p. 1501). According to Medical Historian, Allan M. Brandt (1978), In 1932 the U.S. Public Health Service (USPHS) initiated an experiment in Macon County, Alabama, to determine the natural course of untreated, latent syphilis in black males. The test comprised 400 syphilitic men, as well as 200 uninfected men who served as controls. . . .When penicillin became widely available by the early 1950s as the preferred treatment for syphilis, the men did not receive therapy. In fact on several occasions, the USPHS actually sought to prevent treatment. (p. 21) Initially, the USPHS thought the study would last for only six months and that it would be basically an inexpensive and simple project (Brandt, 1978). As the history of this experiment shows the idea that public health and related medical and science fields can possess misguided values is evident. Public health not only needs a code of ethics, its practitioners should adhere to it and communicate its existence to the public. American people sometimes wonder and harbor skepticism about the activities and the general field of public health. Can public health officials and agencies be trusted? In the African American community some would believe that public health authorities cannot be trusted. According to Thomas and Quinn (1991, p. 1499), “The continuing legacy of the Tuskegee Syphilis Study has contributed to Blacks’ belief that genocide is possible and that public health authorities cannot be trusted.” 4 The directive to ensure and protect the health of the public conveys with it an obligation to care for the well-being of communities. “The need to exercise power to ensure the health of populations and, at the same time, to avoid abuses of such power are at the crux of public health ethics” (J. C. Thomas, Sage, Dillenberg, & Guillory, 2002, p. 1057). Ethics in public health are essential. The Tuskegee Syphilis Study legacy of mistrust that exists in the African American community places the community at high risk for various diseases and chronic infirmities. This has affected the prevention of HIV within the African American community which has a profound effect on public HIV prevention efforts. As stated by Gamble (1997, p. 1773), “Fears that they will be used as guinea pigs like the men in the syphilis study have also led some African Americans with AIDS to refuse treatment with protease inhibitors.” Even though it is recognized that public health practitioners have faced ethical challenges for a very long time, the academic field of public health ethics has emerged and is evolving (Nixon & Forman, 2008). Nevertheless, sound and comprehensive ethical policies must be installed into the prevention efforts undertaken in public health. For instance, “Public health professionals must ensure that HIV testing and counseling are accompanied by specific informed consent, full discussion of treatment options, and appropriate referrals for primary care and clinical trials” (Thomas & Quinn, 1991, p. 1504). The value of consistent use of informed consent, full disclosure of treatment options, and appropriate primary care cannot be overstated. This paper briefly explores public health ethics and the Tuskegee Syphilis Study, a recognized symbol of unethical research on human beings. This paper discusses what went wrong and why the public health authorities along with medical care researchers pursued the study while knowingly taking advantage of disenfranchised people. 5 Chapter 2 The Tuskegee Syphilis Study Susan M. Reverby (2001, p. 22), author of Examining Tuskegee: The Infamous Syphilis Study and Its Legacy and professor of history at Wellesley College, emphatically stated the study affected, “approximately 399 African-American men with the disease and 201 controls, led to a lawsuit, Senate hearings, a federal investigation, and new rules about informed consent.” Reverby succinctly described the impact the study had upon American society. American society has had a historical indifference for the lives of African-Americans (Dalton, 1989; S. B. Thomas & Quinn, 1991). This indifference produces mistrust. Unfortunately, Harlon Dalton (1989, pp. 220–221), professor of law at Yale University and a member of the National Commission on AIDS from 1989 to 1993, believes “the government purposefully exposed Black men to syphilis so as to study the natural course of the disease.” This distortion arose out of historical mistrust and continues to live in the midst of current mistrust and festers. Why was this experiment initiated and pursued? Chief of USPHS Venereal Disease Division in 1932, Dr. Taliaferro Clark (1993, p. 91; S. B. Thomas & Quinn, 1991; Brandt, 1978), explained “the Alabama community offered an unparalleled opportunity for the study of the effect of untreated syphilis.” Clark intended to ascertain how the disease progressed and “affected the daily lives of the men” and the intent of the study was to observe the disease until death (Brandt, 1978, p. 22). This was planned as a study of late stage “untreated syphilis in the male Negro” and treatment was actually withheld and forbidden (Reverby, 2001, p. 24; Jones, 1993). According to Reverby (2001), The PHS did many things to keep the men from treatment: tracking them to other public health departments across the country, intervening with local physicians 6 and even the local draft board, perpetuating the falsification that they were being treated by providing aspirins and vitamins, and lying. (p. 24) At the time of the Tuskegee Study’s inception every major textbook of syphilis, often sexually transmitted disease, strongly supported treatment even in latent stages (Brandt, 1978). Syphilis can be acquired in a congenital manner from an infected mother to fetus, and this appears not to have been of concern to the researchers. There was a prevailing view that blacks were highly promiscuous and sexually driven. As Brandt (1978) surmises, there was a belief that conditions in Tuskegee existed “naturally” because of the inferiority of blacks. Therefore, the men would not be medical treated under the circumstances. This belief provided the experiment’s rationale. In other words, the existence of syphilis treatments did not apply to black people (Brandt, 1978). “The doctors who devised and directed the Tuskegee Study accepted the mainstream assumptions regarding blacks and venereal disease” (Brandt, 1978, p. 23). The mostly illiterate and poverty-stricken population of sharecroppers and tenant farmers was canvassed by the USPHS in search of test subjects (Brandt, 1978). Facts were withheld from the participants. The participants were uninformed, and they were not given information about syphilis (S. B. Thomas & Quinn, 1991). If a person is uninformed and ignorant about diseases, particularly communicable ones, then he or she can easily be manipulated. As stated by Thomas and Quinn (1991, p. 1501), “The PHS physicians, believing that their patients would not understand clinical terms, did not even attempt to educate them about syphilis.” Furthermore, in order to get them to participate they were lied to and told they were being treated for “bad blood” (Jones, 1993). “They were told they were ill and were promised free care” (Brandt, 1978, p. 24). According to Reverby (2009, Kindle Location 98), “The only permission asked for was the right to autopsy their bodies after the men had died in exchange for 7 payment for a decent burial.” In many cases this represented the only burial insurance many of the men could obtain (Jones, 1993). In addition, there were incentives given by USPHS, which included free physical examinations, food, and transportation (S. B. Thomas & Quinn, 1991). The study subjects were medically examined by USPHS physicians and a variety of tests were performed over the years (Jones, 1993). At the end of the study in 1972 there were 71 survivors which reflected only 18 percent of the total participants. Reverby (2001, p. 25) states “there is no reliable information on what happened to the other 328.” According to James Jones (1993, p. 6), “As the years passed the men came to understand that they were members of a social club and burial society called ‘Miss Rivers’ Lodge.’” Miss Rivers was an African American nurse employed by USPHS to act as a bridge between the health service and the men. Even with the bridge provided by USPHS and other incentives why did the men participate? It can be surmised that they did not comprehend what the experiment was about and, therefore, they did not know the dangers they were exposing themselves to (Jones, 1993). However, one of the tragedies concerning this experiment was that the project which “originally intended to meet real health needs ended in a mere attempt to salvage scientific data” (S. B. Thomas & Quinn, 1991, p. 1501). Good intentions based on misinformation can inflict harm upon unsuspecting people. People generally have tendency to trust person of authority. There are valuable lessons to be learned from this infamous study. “Today, as before, the Tuskegee Study has much to teach us about racism in the United States and the social warrant of medicine in people’s lives” (Jones, 1993, p. x). Lillie Tyson Head (2012, p. 474), a descendant of one of the participants in the study, reflects “Research is justifiable, is meaningful, and should accurately predict what is expected, but only when done ethically.” 8 Chapter 3 Consent The public health manager and the organization or agency he represents should be sincerely concerned about informed consent, which is an ethical issue (Burke & Friedman, 2011). Public health leadership has to set an example of public health ethics. Public health managers that promote values that highly esteem respect of persons and liberty are to be commended. Giving consent to be used as a subject or participant in a study is giving permission to be intruded upon. Personal liberty is involved. The view that liberty rights forbid any intervention unless the individual has agreed to it forms the basis of the legal dimensions of consent in health services (Burke & Friedman, 2011). The broad scope of the promotion of the population’s physical well-being includes particular kinds of individual rights, such as study participant rights and patient rights. According to Teitelbaum and Wilensky (2012, p. 111), “One of the most important healthcare rights is the right of individual patients to make informed decisions about the scope and course of their own care.” Three factors are involved for consent to be ethical, the consent should be voluntary, competently obtain, and informed (Burke & Friedman, 2011). Public health organizations must assure managerially that they have provided “adequate, understood, and communicated information as to the services that are to be rendered under their auspices” (Burke & Friedman, 2011, p. 96). Informed consent incorporates a few significant aspects. Informed consent encompasses effective communication of information and includes a discussion of alternatives and risks as well as benefits. “The usual standard is that the information must be what a reasonable physician would give a reasonable patient” (Burke & Friedman, 2011, p. 97). Informed consent is an educational endeavor and includes more than 9 just the patient and physician. Public agencies should consider using a team approach to ensure proper informed consent. Furthermore, Teitelbaum and Wilensky (2012) describe the Nuremberg Code and the contemporary ideas involving informed consent in the following manner: Modern notions of informed consent have their roots in the Nuremberg Code, which derived from the Nuremberg trials in the late 1940s of German physicians who performed horrendous experiments on prisoners in Nazi concentration camps during the Second World War. The code spells out principles of research ethics, including the need to secure in advance the voluntary consent of the research subject. These principles have been codified and expanded in American federal statutory and regulatory law concerning federally funded biomedical research. (p. 111) The code has beneficence comprised in it. Beneficence means making sure a proposed study has in mind the best interest of the participants. Contemporary public health applications of beneficence include a positive duty to the public and acting with charity and kindness (Burke & Friedman, 2011). In research studies the act of balancing benefits and harms is important and beneficence should figure prominently (Burke & Friedman, 2011). Currently regarding research designs and clinical trials there is agreement that the benefits of participation in an experimental study must outweigh any possible risks to the subject and include informed consent (Friis & Sellers, 2014). “Generally accepted international bioethics guidelines state that clinical care and research should be conducted in accordance with four ethical principles: respect for autonomy, beneficence, nonmaleficence and justice” (Elsayed, 2007, p. 146). The Tuskegee Syphilis Study was conducted outside of the realm of acceptable ethics. “In light of the deceptions and exploitations which the experiment perpetrated, it is an understatement to declare . . . that the experiment was ‘ethically unjustified,’ because it failed to obtain informed consent from the subjects” (Brandt, 1978, p. 27). 10 Waiving consent leads to taking advantage of vulnerable populations as proven by the Tuskegee Syphilis Study. It would not be recommended ever to waive consent, even though some researchers have raised the question of waiving consent in some areas of clinical investigation. This approach leaves room for unethical behavior to occur. One problem to foresee is an abuse of power like the one that occurred during the Tuskegee Syphilis Study. It is acknowledged there are circumstances under which waiving informed consent is acceptable in research, such as when researchers are unable to obtain it and when the studies involve only minimal risks. “In such circumstances, research participants generally need protection in other ways, such as through confidentiality safeguards and appropriate review by an independent research ethics committee” (Friis & Sellers, 2014, p. 717). However, minimal risk can be interpreted subjectively. Additionally, researchers should do the uttermost to obtain informed consent. Also, public health studies are required to submit study proposals for independent ethical review (Friis & Sellers, 2014). It is beneficial for the field of population health to have a document like the Belmont Report. The Belmont Report attempts to condense the basic ethical principles identified by The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (U. S. Department of Health and Human Services, 1979). The Belmont Report includes respect for autonomy, beneficence, and justice. Individual autonomy is “the right to be free from interference” (Burke & Friedman, 2011, p. 91). Nonetheless, society cannot be put at risk because of individual rights (Burke & Friedman, 2011). There are times of crisis when the health and safety of the community outweigh individual rights. The study this paper has reviewed does not reflect such a time. 11 Chapter 4 Summary and Recommendations Summary There have been many great accomplishments in the field of public health over the last 100 years. There have been many lessons learned from the success and failures. This paper has discussed an example of a failure. The 40 year Syphilis Study started at Tuskegee Institute in Alabama in 1932 conducted by the USPHS on African American men was unethical. Furthermore, this study has become legendary and stands as blemish upon public health research. This failure has contributed to the development of a public health code of ethics. It is recognized that public health places values on individual informed consent and autonomy. Public health has striven to embrace the mistakes of the past and put into place a variety of rules and oversight to ensure that this kind of research experiment never happens again. The Tuskegee Syphilis Study is an example of research using human subjects who were not protected. This occurrence was allowed because the subjects were African American. Even though individual autonomy is highly valued in the United States, African Americans experience individual rights violations within the arena of population health. The Tuskegee Syphilis Study subjects trusted the public health officials and these same officials withheld treatment from them. As already been indicated above the study lasted for 40 years during a time of innovations in medical treatments for syphilis. As a result of the study mistrust has been bred and still breeds among African Americans. Trust must be earned and consistent goodwill must be demonstrated to recover from the legacy of the study. 12 Lastly, informed consent is a vital part of any public health code of ethics. Informed consent involves public health leadership, dedication, planning, and education. Beneficence and autonomy are keys to comprehensive and effective informed consent. Recommendations Public health research is foundational in the struggle to conquer infectious diseases that rampage populations. Therefore, it is essential that public health research continue, yet it must continue with an ethical basis if it is going to effective and generate trust. Placing a high value on all human life and dignity is an essential commitment that public health researcher must possess. Researchers have an obligation to design investigations that take into accountable a host of variables and to be mindful of beneficence in regards to potential participants. Another recommendation would be to not forget what occurred and the legacy that still affects the African American community. Remember that miscommunication and misunderstanding can breed mistrust in any community, and especially in a community where health disparities exist. The changes to make regarding how the Tuskegee Syphilis Study was conducted are numerous. The study designed was not well thought out. The duration was too long. The foundational basis was unstable and did not allow for future advancements in medical research. Most importantly, the truth should have been told to the participants in the beginning and throughout the course of the study. There should be been a wholehearted effort to obtain informed consent and provide full disclosure. Respect of persons should have been demonstrated especially because the USPHS represents the entire American population. 13 References Brandt, A. M. (1978). Racism and research: the case of the Tuskegee Syphilis Study. Hastings Center Report, 8(6), 21–29. Burke, R. E., & Friedman, L. H. (2011). Essentials of management and leadership in public health. Sudbury, MA: Jones and Bartlett Publishers. Dalton, H. L. (1989). AIDS in blackface. Daedalus, 205–227. Elsayed, D. E. M. (2007). Public health and ethics: An overview. Sudanese Journal of Public Health, 2(3). Retrieved from http://sjph.net.sd/files/vol2i3p146-151.pdf Friis, R. H., & Sellers, T. A. (2014). Epidemiology for Public Health Practice. Jones & Bartlett Publishers. Gamble, V. N. (1997). Under the shadow of Tuskegee: African Americans and health care. American Journal of Public Health, 87(11), 1773–1778. doi:10.2105/AJPH.87.11.1773 Head, L. T. (2012). One Voice: A Commentary on the Syphilis Study at Tuskegee by a Descendant’s Daughter. Ethics & Behavior, 22(6), 472–474. doi:10.1080/10508422.2012.730004 Jones, J. H. (1993). Bad Blood. Simon and Schuster. Nixon, S., & Forman, L. (2008). Exploring synergies between human rights and public health ethics: A whole greater than the sum of its parts. BMC International Health and Human Rights, 8(1), 2. Reverby, S. M. (2001). More than fact and fiction: Cultural memory and the Tuskegee syphilis study. Hastings Center Report, 31(5), 22–28. Reverby, S. M. (2009). Examining Tuskegee: The Infamous Syphilis Study and Its Legacy (Kindle.). The University of North Carolina Press. 14 References (Cont.) Teitelbaum, J. B., & Wilensky, S. E. (2012). Essentials of Health Policy and Law. Jones & Bartlett Learning, LLC. Thomas, J. C., Sage, M., Dillenberg, J., & Guillory, V. J. (2002). A Code of Ethics for Public Health. American Journal of Public Health, 92(7), 1057–1059. doi:10.2105/AJPH.92.7.1057 Thomas, S. B., & Quinn, S. C. (1991). The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community. American Journal of Public Health, 81(11), 1498–1505. doi:10.2105/AJPH.81.11.1498 U. S. Department of Health and Human Services. (1979, April 18). The Belmont Report. Retrieved June 22, 2014, from http://www.hhs.gov/ohrp/humansubjects/guidance/belmont.html