Patient positioning - Questions 24. How does the lateral decubitus
advertisement
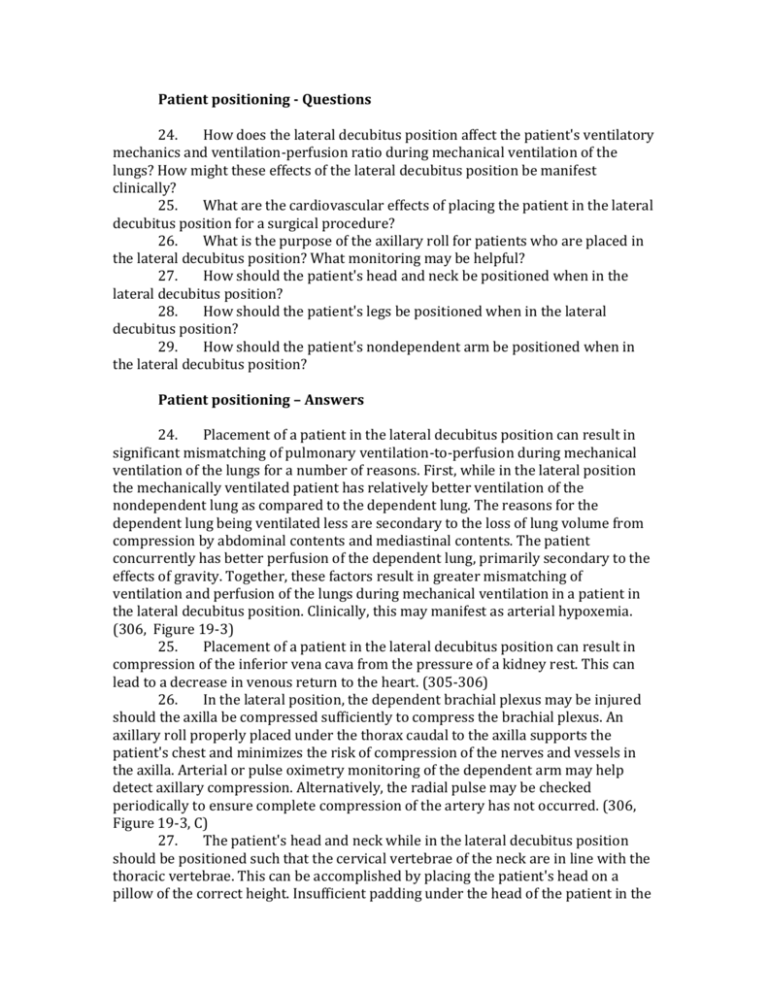
Patient positioning - Questions 24. How does the lateral decubitus position affect the patient's ventilatory mechanics and ventilation-perfusion ratio during mechanical ventilation of the lungs? How might these effects of the lateral decubitus position be manifest clinically? 25. What are the cardiovascular effects of placing the patient in the lateral decubitus position for a surgical procedure? 26. What is the purpose of the axillary roll for patients who are placed in the lateral decubitus position? What monitoring may be helpful? 27. How should the patient's head and neck be positioned when in the lateral decubitus position? 28. How should the patient's legs be positioned when in the lateral decubitus position? 29. How should the patient's nondependent arm be positioned when in the lateral decubitus position? Patient positioning – Answers 24. Placement of a patient in the lateral decubitus position can result in significant mismatching of pulmonary ventilation-to-perfusion during mechanical ventilation of the lungs for a number of reasons. First, while in the lateral position the mechanically ventilated patient has relatively better ventilation of the nondependent lung as compared to the dependent lung. The reasons for the dependent lung being ventilated less are secondary to the loss of lung volume from compression by abdominal contents and mediastinal contents. The patient concurrently has better perfusion of the dependent lung, primarily secondary to the effects of gravity. Together, these factors result in greater mismatching of ventilation and perfusion of the lungs during mechanical ventilation in a patient in the lateral decubitus position. Clinically, this may manifest as arterial hypoxemia. (306, Figure 19-3) 25. Placement of a patient in the lateral decubitus position can result in compression of the inferior vena cava from the pressure of a kidney rest. This can lead to a decrease in venous return to the heart. (305-306) 26. In the lateral position, the dependent brachial plexus may be injured should the axilla be compressed sufficiently to compress the brachial plexus. An axillary roll properly placed under the thorax caudal to the axilla supports the patient's chest and minimizes the risk of compression of the nerves and vessels in the axilla. Arterial or pulse oximetry monitoring of the dependent arm may help detect axillary compression. Alternatively, the radial pulse may be checked periodically to ensure complete compression of the artery has not occurred. (306, Figure 19-3, C) 27. The patient's head and neck while in the lateral decubitus position should be positioned such that the cervical vertebrae of the neck are in line with the thoracic vertebrae. This can be accomplished by placing the patient's head on a pillow of the correct height. Insufficient padding under the head of the patient in the lateral decubitus position can result in compression and stretching to the brachial plexus and direct compression to the dependent ear and eye. (305-306) 28. The patient's legs while in the lateral decubitus position should be positioned such that the dependent leg is flexed at the knee and there is a pillow between the two legs. This helps to minimize stretch of the nerves of the dependent leg and distributes more evenly the weight of the legs, such that discrete pressure points are avoided. Indeed, there have been case reports of arterial insufficiency of the dependent leg of patients undergoing hip arthroplasty in the lateral position. (305-306) 29. The patient's nondependent arm while in the lateral decubitus position should be supported by a holder or padding above and in front of the patient's face. Alternatively, the arm may be suspended from a support bar that is well padded. Both positions should limit the extension of the arm to less than 90 degrees at the shoulder. (305-306, Figure 19-3, B)