Bachelor of Nursing
advertisement

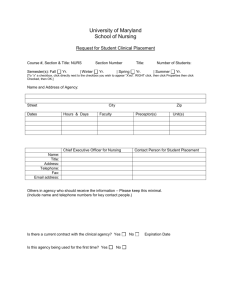
Bachelor of Nursing HANDBOOK for CLINICAL EDUCATORS & MENTORS This handbook reviewed by: Lynne Slater Director of Clinical Education Callaghan Gwyneth Harbrow Clinical Liaison Nurse School of Nursing & Midwifery Faculty of Health University of Newcastle 2012 Copyright 2012 School of Nursing & Midwifery Faculty of Health The University of Newcastle Contents Introduction ............................................................................................................................................... 3 Who do I communicate with about students and matters related to clinical learning? ............................ 3 What is the management structure of the School in relation to clinical placement? ................................ 4 What does the University expect of me? .................................................................................................. 5 Who is responsible for the client when a student is providing care? ....................................................... 6 Are students insured? .............................................................................................................................. 6 Overview of Undergraduate Clinical Skills .............................................. Error! Bookmark not defined. What can students actually do on clinical placement? ............................................................................. 7 What do I do if I have concerns about a student’s attendance or performance? ..................................... 7 What do I do if the student’s practice is unsatisfactory? .......................................................................... 8 What happens if a student is injured or involved in an incident on placement? ...................................... 8 What are the assessment requirements on a clinical placement? ........................................................... 8 Clinical Summary Forms ..................................................................................................................... 9 Clinical Performance Reports.............................................................................................................. 9 Skills Checklists ................................................................................................................................. 11 Nursing Narratives ............................................................................... Error! Bookmark not defined. What should I do if students don’t want to be on the placement? .......................................................... 12 What support is there for me as a Clinical Educator/Mentor? ................................................................ 12 What feedback and acknowledgement do I receive as a Clinical Educator/Mentor? ............................ 12 Do students need to attend orientation to the placement? .................................................................... 12 I have a student/group of students for whom English is a second language – what support is there for them? ............................................................................................................................................... 13 I have told the School about my concerns with a particular student’s performance and now I see they are back on another clinical. Why is this? ....................................................................................... 13 I was expecting a student to arrive at the clinical venue and he/she hasn’t arrived - what should I do?14 What do I do if a student arrives to attend placement and says he/she can’t undertake the usual activity because of a previous injury or condition? .......................................................................... 14 What do I do if I am sick or unable to attend laboratories or placement? .............................................. 14 Introduction The information in this handbook is specific to the School of Nursing and Midwifery. Clinical Nurse Educators, Mentors and Preceptors should also be familiar with information contained in the Faculty of Health Placement Handbook. Clinical Nurse Educators, Mentors and Preceptors often have a lot of questions related to School procedures in association with clinical courses and clinical placement. The format of this handbook is based on Frequently Asked Questions. Who do I communicate with about students and matters related to clinical learning? The Director of Clinical Education or representative will always be available on the mobile phone number/s below: Director of Clinical Education Lynne Slater (Callaghan) T: 02 49217707 M: 0429 313711 E: Lynne.Slater@newcastle.edu.au Assistant Director of Clinical Education Sarah Jeong (Ourimbah) T: 02 4921 6043 M: E: Sarah.Jeong@newcastle.edu.au Assistant Director of Clinical Education Raelene Kenny (Port Macquarie) T: 02 6581 6297 M: E: Raelene.Kenny@newcastle.edu.au Clinical Placement Liaison Nurse Gwyneth Harbrow (Callaghan and Port Macquarie) T: 02 49215820 M: 0407623114 E: Gwyneth.Harbrow@newcastle.edu.au Clinical Placement Liaison Nurse Sharon Hilgendorf (Ourimbah) T: M: E sharon.hilgendorf@newcastle.edu.au Clinical Placement Unit T: 02 49216321 (Callaghan) E: nursing-clinical-query@newcastle.edu.au Clinical Placement Unit 02 49216336 (Ourimbah) Please note nursing-clinical-query@newcastle.edu.au is the generic email address for the Clinical Placement Unit. It is checked constantly by staff in the unit. 3 Course Coordinators - as advised prior to the commencement of each semester. Course Coordinators should contact you once they have been advised of your employment. If you have not been contacted and have not been advised and do not know your Course Coordinator you may wish to contact the Clinical Coordinator (Administration) OR Director of Clinical Education as above; OR Undergraduate Program Convenor, Joy Lyneham to determine your Course Coordinator. What is the management structure of the School in relation to clinical placement? Student Clinical Educator 1st / 2nd Year Students Mentor 3rd Year or other mentored placements 3rd Year last semester = Clinical Mentor & Academic Mentor Clinical Placement Unit Course Coordinator Director of Clinical Education Undergraduate Program Convenor 4 What does the University expect of me? The School of Nursing and Midwifery expects Clinical Educators, Preceptors and Mentors to act as positive role models for students by: Demonstrating and encouraging enthusiasm for the area of nursing in which students are placed; Demonstrating knowledge, skills and behaviours that are consistent with the current role of the Registered Nurse; Practising according to the ANMC competency standards, Code of Professional Conduct and Code of Ethics for a Registered Nurse; Being cognisant and consistent with the policies of the facility in which the clinical placement is taking place; Indicating preparation for the clinical placement by ensuring that he/she is familiar with the unit prior to the placement commencement date and being familiar with the course outline and clinical placement objectives; Indicating adequate preparation for teaching/facilitating learning in the laboratory environment by preparing according to the laboratory workbook and being familiar with the course outline and clinical laboratory objectives. The School of Nursing and Midwifery expects Clinical Educators, Preceptors and Mentors to demonstrate a student centred approach to learning, evidenced by: Assisting the student to relate their clinical experience to learnt theory; Providing early, timely and constructive feedback to the student about his/her performance (that is: within a timeframe that encourages further learning within the clinical placement period); Contacting the Course Coordinator or Director of Clinical Education about any concerns to allow for student and Educator/Mentor support; Acknowledging that the student may feel out of place in a new environment and assisting others in supporting and accepting students into the new environment; Suggesting resources the student should use to support their learning; Providing direction to the student and assisting in determining learning opportunities during the placement. The School of Nursing and Midwifery expects Clinical Educators, Preceptors and Mentors to complete documentation associated with clinical placement and return to the Clinical Placement Unit as required in a timely manner: Documentation includes Clinical Summary Forms and, when required, Clinical Performance Reports; Clinical Educators, Preceptors and Mentors are to complete the Clinical Summary Forms at the end of each week the student is on a clinical placement. Unless in a preceptored placement, this responsibility lies with the University employed Educator, in a preceptored/mentored placement this responsibility lies with the Preceptor/Mentor. It is expected that if a student’s placement is facilitated, the Facilitator seek input from the student’s preceptor in the clinical area with whom the student has been working. This allows for a more accurate assessment of the students overall progression and achievement. Each day of clinical placement MUST be signed by the Educator/Preceptor/Mentor; Report any non-attendance to the Clinical Coordinator or the Clinical Placement Unit as soon as possible; All Unsatisfactory grades and/or Needs Development must be supported with a Clinical Performance Report; 5 In the event of unsatisfactory performances or awarding more than 6 “Needs Development” within one week’s Clinical Summary Report, an appropriate Clinical Performance Report needs to be completed and sent to the Course Coordinator or Clinical Placement Unit immediately; Notify the Course Coordinator of the “Unsatisfactory” or “Needs Development” reports and advise the student that they need to contact the Course Coordinator; Satisfactory Clinical Summary Forms are to be delivered (by mail or person) to the Clinical Placement Unit on the last day of the clinical placement or every two weeks, whichever is sooner; If the student is deemed unsafe – that is they have exposed patients or others to risk, harm or an adverse event; or has demonstrated unprofessional behaviour, a Clinical Challenge agreement will be discussed with the course coordinator and/or director of Clinical Education. If this agreement is not deemed to have been completed satisfactorily, the student will be given an unsatisfactory grade for that placement. Both the Clinical Summary Forms and the Clinical Performance Reports are carbonated. The original (white copy) is to be returned to the Clinical Placement Unit. The yellow copy stays in the student’s book. Please remember to press firmly with a biro pen and to place the cardboard under the yellow copy before writing; In a facilitated placement the University Educators (only) are to assess and complete the core skill assessments as set out for each course; checked off using the checklists from the text Tollefson (2010 or 2012). Only when a student is attending a preceptored or mentored placement will the nominated RN Preceptor/Mentor undertake this assessment; RN Mentors, Preceptors or Clinical Educators (other than the University Educator) are permitted to complete further assessments as required by the students. These might involve at least ONE extra skill per placement in first and second semester of second year and first semester of third year. No assessment can be undertaken by an Enrolled Nurse Please note: Although students are preceptored and supported in their learning by nurses employed by our clinical partners, the School of Nursing and Midwifery expects facilitators to employ a model of facilitation where they are clinically active in the demonstration and guidance of clinical skill development as taught by the School of Nursing and Midwifery. This should be accomplished in negotiation with allocated preceptors, by dividing your ward time amongst students to allow for time working alongside with them. This not only provides additional support with clinical skills but also to enable adequate and fair assessment of student development as per the clinical summary guidelines". It is expected that facilitators seek input from student preceptors when completing their assessment of students within these guidelines. Who is responsible for the client when a student is providing care? Essentially, the Registered Nurse supervising the patient and the student is responsible for the client at all times. Are students insured? The School has agreements with all clinical placements that cover insurance of students. Students are covered for personal accident insurance and public liability insurance. They are not eligible for workers’ compensation. Students are only insured for periods of formal 6 learning. Additional clinical experience outside of placement and ‘work experience’ is not covered by insurance. Clinical Educators and Mentors need to know if the student is present and when they leave the facility. Some venues may ask staff and students to “sign in”. Please ensure that these policies are adhered to. As well, at the beginning of each day, ensure that all students are present in their allocated area. What can students actually do on clinical placement? The Clinical Educator/Preceptors and Mentors are responsible for the activity in which the student engages. One of the most challenging aspects of these roles can be determining the student’s readiness for tasks and capitalising on the opportunistic teaching that occurs in clinical environments. Each student is bound by a Scope of Practice which is determined by the skills demonstrated and practised in the laboratories prior to placement, as well as the associated theoretical level. However, each student should also be assessed to ensure that they are at the level commensurate with undertaking those skills. If they are not competent at that level, you are expected to provide assistance with their learning. If, following this assistance the student does not progress this needs to be documented. Students should always work within their Scope of Practice for their specified year. These are available on Blackboard and are also emailed to the venue on commencement of each semester. Students are expected to practice within the principles developed as shown in the Scopes of Practice as these are the skills that they have had demonstrated and practiced, and also have had some theoretical grounding. However, higher level skills that have not been practiced in the laboratories should not be encouraged. Examples of these are invasive procedures such as catheterisation and central line care, in first or second year . There are also variations depending on a number of factors such as student confidence, past experience and comfort in the unit, as well as the unit policy and expectations. Each student should be encouraged to practice all established skills under the supervision of a RN or yourself so that the student becomes comfortable and proficient in the core needs of patient care. Students are provided with a list of clinical objectives for each course. As well they are requested to develop a short list of personal objectives prior to commencing the clinical placement (these can be as few as three or four appropriate and achievable objectives and can be extended throughout the placement). If the student is attending your area as a member of a group of students with an Educator, facility employees can always seek advice from the Educator about the expectations of the student. What do I do if I have concerns about a student’s attendance or performance? In the first instance, you should provide immediate feedback to the student in a private area about your concerns. If you feel that the activity/behaviour is unsatisfactory or indicates poor development, this should be identified to the student and referred to in the Clinical Summary book. If the student has not demonstrated unsafe or unprofessional behaviour which might lead to the student leaving the placement, you should discuss and set learning objectives for the student to guide the student’s improvement. A Clinical Performance Report should be completed, recording the situation and reasons for the concerns (at the back of the Clinical 7 summary Book). Then, in discussion with the student (and Course Coordinator if required) set specific pathways and goals for the student that if achieved indicate a satisfactory standard in these areas. If necessary, you can add extra documents to support your information. Students should be encouraged to realise that as students it is reasonable that they have areas that need developing, however, the University also needs these concerns to be documented to ensure student support in the future. If you are unsure of your assessment or remain concerned, you should contact the Course Coordinator or the Director of Clinical Education. The Clinical Placement Unit may also be able to assist in contacting the appropriate staff. Your concerns will always be taken seriously and you will be supported in your decisions about a student. However, please be aware that in order for university staff to process and act upon unsatisfactory student performances you must be prepared to provide feedback to a student in a timely manner and complete this relevant documentation. It is important that all information in the assessment and feedback process including the setting of clear goals is documented on the Clinical Summary sheets and Clinical Performance reports. What do I do if the student’s practice is unsatisfactory? Contact the School of Nursing and Midwifery staff immediately if you have any concerns at all about a student’s performance. The first point of contact is the Course Coordinator or the Director of Clinical Education. A Clinical Performance Report is to be completed and forwarded to the Clinical Unit immediately. If you have strong concerns about the student’s actions, you may ask them to leave the clinical area until you contact a university representative, and a consultative decision made about the student’s clinical placement. What happens if a student is injured or involved in an incident on placement? An incident is something that results (or potentially results) in harm to the student or others. It can include physical injury or psychological assault. Students have been told to notify the Clinical Educator/Preceptor/Mentor if they are involved in a matter of concern and that the Clinical Educator will support them in notifying the facility and University of the incident and completing relevant documentation found in Blackboard through Clinical Resources / Prep for Placement / Policies and Associated Forms (also contained in the Faculty of Health Placement Handbook). When notifying the School of Nursing and Midwifery about the incident you should contact the Clinical Placement Unit on (02) 4921 6326. The documentation for both the facility and the University should be completed within 24 hours and returned to the Clinical Placement Unit. Students should keep a copy of the form for their own records. What are the assessment requirements on a clinical placement? All students are to attend in full the hours required for their placement. This includes 8 hours of placement and does not include meal breaks. Briefing and debriefing are counted in these hours. Students ARE NOT to leave early as the hours of placement are counted towards the total clinical hours required by the Nurses and Midwives Board (NSW). 8 If you are an Educator with a group of students it may be advisable to negotiate time with each student to facilitate their assessments and to provide learning and assistance when required. If the activity/ behaviour continues once identified, and set learning objectives are not achieved a Clinical Challenge Contract can be set with consultation with the Course coordinator. Students may request to be assessed in other skills (as covered by their Scopes of Practice). These may be assessed by supportive staff in the venue. ALL assessments MUST be undertaken by an RN. Clinical Summary Forms The student details information should be completed by the student, including their personal information and course code. Clinical Educators should collect the books at the beginning of the placement to ensure completion even if a student does not attend all days. These can then be returned to the students at the end of the clinical placement. It is the student’s responsibility to ensure these forms are completed. The Clinical Summary provides a record of the student’s hours of attendance and performance. It is to be completed by the Clinical Educator/Mentor at the end of each week and sent to the Clinical Placement Unit at the end of the placement, or at the end of each 2 week block. Each page should ONLY be for ONE WEEK and only for one course. For example, a two week placement requires one separate page for each week. Clinical Performance Reports If a student has an unsatisfactory Clinical Summary, a Clinical Performance Report is to be completed by the Clinical Educator or Mentor and the matter is to be discussed with the student. The Clinical Summary and the Clinical Performance Report are to be returned to the Clinical Placement Unit immediately. The Course Coordinator will review the documentation and an academic decision will be made about the students’ continuation. This may require the student to repeat either part of, or the entire clinical placement. Clinical Educators/Mentors should be aware that unless the student’s performance has been documented as unsatisfactory and the student has been given early feedback and an opportunity to improve, it is difficult to support an unsatisfactory grade. If a Clinical Educator/Mentor has any concerns at all about a student at any time, the Clinical Educator should speak with the student, document that feedback has been given on the Clinical Performance Report, and notify the Course Coordinator. Sometimes, providing feedback about poor performance is challenging. Support in providing this type of feedback to students will be provided by the Course Coordinator or the Director of Clinical Education when needed. Students are required to complete 100% of clinical hours in each placement as part of the assessment. Hence the importance of the Clinical Educator/Mentor accurately documenting the hours attended. 9 Overview of Undergraduate Clinical Core Skills NB. Assessment, documentation and client education is a component of all skills. First year, first semester First year, second semester Second year, first semester Second year, second semester Therapeutic communication Accurate taking, recording and interpreting patient temperature, pulse and respiration. Fluid status assessment and documentation Management of oxygen therapy and oxygen delivery devices. Safe client moving. Accurate taking, recording and interpreting patient blood pressure. Wound assessment. Oxygen saturation monitoring. Hand hygiene and hand washing. Meeting client hygiene needs – showering, bed bath, oral care, mouth and eye care Pain assessment. IV medication administration via bolus and burette. Assisting safe client ambulation. Blood glucose monitoring. Comprehensive mental health assessment and history taking. Drug dosages – principles and calculations. (on campus assessment) Falls risk assessment. Safe administration of parenteral medication (subcutaneous). MMSE Comp. Third year, first semester Aseptic technique. (on campus assessment) 10 Skills Checklists Clinical Educators/Mentors are also required to complete skills checklists from the text Tollefson, (2010, 2012). Students are required to achieve mastery in all identified core skills as well as attempt a range of context specific skills throughout the BN program (see the core skills listed on Clinical Skills table above). When assessing core skills the Clinical Educator or Mentor is to ask the student 3 - 5 questions from the relevant pages in Tollefson (2010, 2012). Students are expected to provide relevant answers that indicate an understanding of the theory that supports the skill they are undertaking. This is then documented in the section on the check list termed: ‘Relates Theory to Practice’. The Gibbs Reflection Cycle This is the model that our students are guided to use for reflection. This guides the students to ask: What happened? How did it affect me? What have I learned from this episode & experience? How this incident and these experiences might change my future behaviour if ever faced with similar incidents? 11 What should I do if students don’t want to be on the placement? From time to time, students can appear unmotivated, disinterested or even hostile to the placement. This can be demoralising for staff. Some suggestions include: 1. Indicate to the student that they are perceived as not wanting to be on the placement, explore what’s going from the students’ perspective and outline your expectations of behaviour in the placement; 2. Document the discussion; and 3. Advise the Course Coordinator of your concerns; 4. Allocate a needs development as an initial assessment if required. If the behaviour does not improve, an unsatisfactory may be allocated. Students may appear disinterested because they are shy, aware they are “guests-in-thehouse”, concerned about what is expected of them and overwhelmed by the clinical experience. In some cases, clinical staff are passionate about their area of practice and students may not share that degree of passion. However, students are always expected to indicate a willingness to learn and to participate in the work within the ward/venue. In a very few cases students indicate a negative attitude to completing the placement and are unable to perform in a way that reflects positively on them or the University. In those cases, if the student behaviour does not improve and clinical expectations are not unreasonable, you should contact the Course Coordinator and the student will be removed from the placement. A Clinical Performance Report should be completed. What support is there for me as a Clinical Educator/Mentor? You should feel free to discuss matters about clinical facilitation with staff of the School at any time. If you have any concerns about students, facility staff or the facility, please feel free to contact the university staff. If you would like additional support at any time contact the Course Coordinator or Director of Clinical Education. What feedback and acknowledgement do I receive as a Clinical Educator/Mentor? The School asks students to complete an evaluation of their placement, which includes feedback about their clinical educator/mentor. Feedback is then provided to the clinical educator/mentor. The School also uses an evaluation tool based on the Australian Nurse Teacher’s Society (ANTS) nurse teacher competencies. This tool encourages self evaluation by you and also for discussions with the Director of Clinical Education about areas that might require improvement. Do students need to attend orientation to the placement? Each venue has specific requirements about students needs relating to orientation procedures and introductions to the venue. These will also be part of the information sent to you. As part of the needs for placement students are required to attend yearly updates on campus in relation to infection control, manual handling, emergency response and CPR. Most facilities have indicated that students do not need to attend these when they arrive at the clinical venue. However, some venues request an orientation so that students can be familiar with the environment in which they work and much of this can be undertaken as a directed activity in the unit. 12 As well, students are required to complete an Orientation Checklist and Recognition of Scope of Practice on their first week at every clinical venue. To complete this, students MUST write down the place of the item or the answer to any questions. This is the student’s responsibility. Once complete, it is to be signed by the clinical educator or mentor and is submitted as part of the student’s portfolio. I have a student/group of students for whom English is a second language – what support is there for them? The School has organised support classes for all students who have English as a second language. Classes are provided to assist students to develop their clinical language prior to or during the semester. However, some students will still have difficulties while on placement. It might be relevant to prioritise their English communication skills as one of the main primary learning objectives in the clinical placement and this should be encouraged. If you are concerned about the student’s proficiency in English, consult with the student advising them to make this a priority for the placement. Consult with the student’s preceptor/buddy to discuss any problems and provide support for the clinician when needed. Contact the student’s Course Coordinator if there are problems that will need to be addressed. The Course Coordinator will then arrange support for you and the student in consultation with the Language Support Centre on campus. If there is ongoing concern, a “Needs Development” or “Unsatisfactory” grade in Communication should be awarded in the Clinical Summary book and a Clinical Performance report completed. The Course Coordinator and/or the Director of Clinical Education can then investigate further support for the student. If the language difficulties impact on the student’s performance of safe practice, please discuss a Clinical Assessment Procedure with the course coordinator. I have told the School about my concerns with a particular student’s performance and now I see they are back on another clinical. Why is this? The purpose of the clinical placement is to provide students with a learning experience that supports effective clinical practice. As we all know, on campus tutorials and simulated environments do not fully provide this experience. When you let the School know of your concerns, matters are discussed with the student and strategies to address these are put in place. Frequently, the concerns about student performance in the clinical setting can only be addressed through remediation and additional placement time. If a student is considered to demonstrate unsafe or unprofessional behaviours and has not responded to a Clinical Challenge Contract, their development is discussed by the Clinical Committee. Outcomes are determined by the student’s needs and the needs for safe and professional behaviour for the patient. It is vitally important that all situations are clearly documented and in a timely manner. Some students – others will be asked to leave the placement on the advice of the Director of Clinical Education, the Undergraduate Program convenor or the specific staff member in charge on the ward/venue. Students do need to be given the chance to develop their confidence and skills. However, if a makeup or remedial placement does not increase the student’s ability to complete their skills or a satisfactory placement, the student may fail the course. The student then needs to complete the whole course again. 13 I was expecting a student to arrive at the clinical venue and he/she hasn’t arrived - what should I do? Contact the Clinical Placement Unit ((02) 4921 6321) and/or the appropriate Course Coordinator so that the student’s safety can be ensured and insurance requirements followed. Students sometimes decide to withdraw from the program without notifying University staff, and this knowledge is gained only when the clinical venue contacts us to say the student has not attended. Alternatively, the student may not have completed the required clinical laboratories in the weeks prior to placement and therefore is not able to attend placement. Clinical Placement Unit staff do try to ensure all Educators/Mentors and facilities have current knowledge about student attendance. If a student is unable to attend placement for any reason (such as illness) they are advised to contact their Educator/Mentor, the facility and their Course Coordinator. The process then is for the student to submit an application for Adverse Circumstances via their myHub. What do I do if a student arrives to attend placement and says he/she can’t undertake the usual activity because of a previous injury or condition? No student is to attend placement when they have had a previous illness or injury, or are experiencing injury or ill health unless they have provided a clearance letter, document to the Director of Clinical Education. Students are not to attend placement while experiencing such infectious diseases as gastroenteritis, influenza, serious viral infection or other illnesses. If a student indicates that they have a medical condition which leads to limitation in clinical activities they should be asked to leave the placement and contact the Director of Clinical Education immediately. If in doubt please ring the relevant Director or Assist. Director of Clinical Education to discuss. Examples are students who are under a Workcover agreement, who have worked a shift directly preceding the placement “shift”, are indicating mental health issues or students who cannot complete ALL of the physical requirements of clinical placement. Where there are restrictions that would interfere with the student’s ability to demonstrate competence in clinical practice, contact the Course Coordinator. The placement may be changed or withheld until the student is able to meet the requirements of satisfactory clinical performance. If you have any concerns about a particular student contact the Clinical Coordinator or the Director of Clinical Education. What do I do if I am sick or unable to attend laboratories or placement? Make contact with: the relevant Director or Assistant Director of Clinical Education if it is outside office hours (see phone numbers or in your paperwork relevant to the clinical placement); OR the Course Coordinator; OR the Clinical Placement Unit: as soon as possible. Respective phone numbers are supplied in your paperwork. 14