1-Normal microbial flora
advertisement
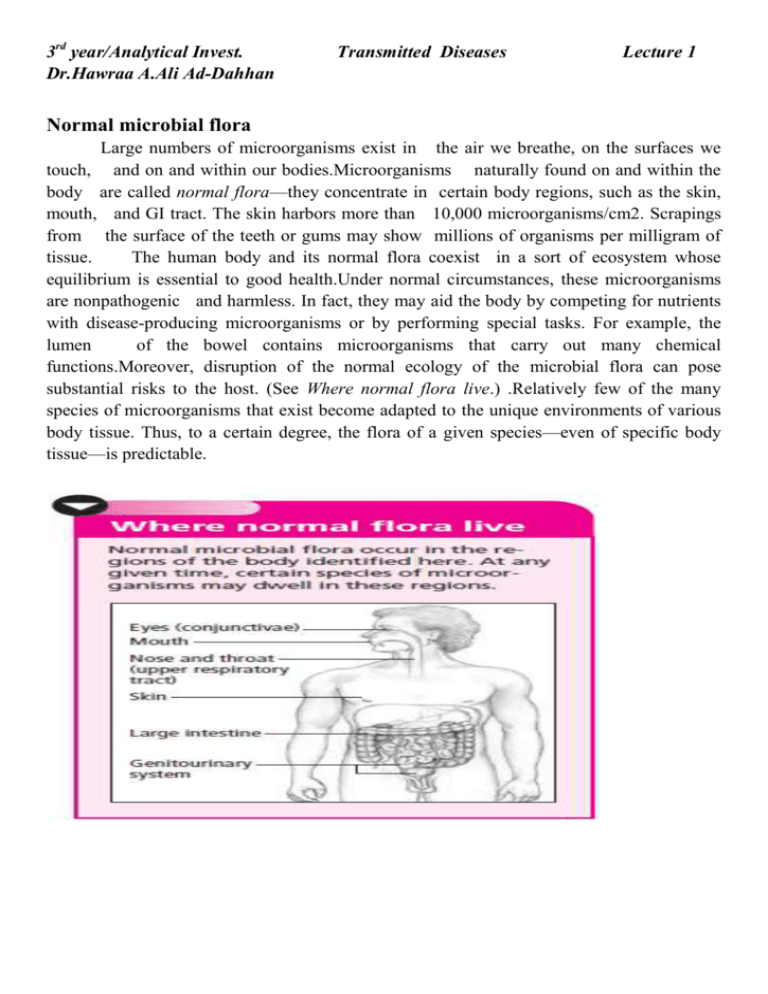
3rd year/Analytical Invest. Dr.Hawraa A.Ali Ad-Dahhan Transmitted Diseases Lecture 1 Normal microbial flora Large numbers of microorganisms exist in the air we breathe, on the surfaces we touch, and on and within our bodies.Microorganisms naturally found on and within the body are called normal flora—they concentrate in certain body regions, such as the skin, mouth, and GI tract. The skin harbors more than 10,000 microorganisms/cm2. Scrapings from the surface of the teeth or gums may show millions of organisms per milligram of tissue. The human body and its normal flora coexist in a sort of ecosystem whose equilibrium is essential to good health.Under normal circumstances, these microorganisms are nonpathogenic and harmless. In fact, they may aid the body by competing for nutrients with disease-producing microorganisms or by performing special tasks. For example, the lumen of the bowel contains microorganisms that carry out many chemical functions.Moreover, disruption of the normal ecology of the microbial flora can pose substantial risks to the host. (See Where normal flora live.) .Relatively few of the many species of microorganisms that exist become adapted to the unique environments of various body tissue. Thus, to a certain degree, the flora of a given species—even of specific body tissue—is predictable. ●What is infection? Infection is the invasion and multiplication in or on body tissue of microorganisms that produce signs and symptoms along with an immune response. Such reproduction injures the host either by causing cellular damage from microorganism-produced toxins or intracellular multiplication or by competing with host metabolism. The host’s own immune response may increase tissue damage, which may be localized (as in infected pressure ulcers) or systemic. The very young and the very old are most susceptible to infections. Microorganisms that cause infectious diseases are difficult to overcome for many reasons: ☐ Some bacteria develop a resistance to antibiotics. ☐ Some microorganisms, such as human immunodeficiency virus (HIV), include many different strains, and a single vaccine can’t provide protection against them all. ◗ Most viruses resist antiviral drugs. ◗ Some microorganisms localize in areas that make treatment difficult, such as the central nervous system and bone. ◗ New infectious agents, such as HIV and severe acute respiratory syndrome–coronavirus, occasionally arise. ◗ Opportunistic microorganisms can cause infections in immunocompromised patients. ◗ Much of the world’s ever-growing population has not received immunizations. ◗ Increased air travel by the world’s population can speed a virulent microorganism to a heavily populated urban area within hours. ◗ Biological warfare and bioterrorism with organisms such as anthrax, plague, and smallpox are an increasing threat to public health and safety throughout the world. ◗ Invasive procedures and the expanded use of immunosuppressive drugs increase the risk of infection for many. (See When microorganisms grow resistant). Also, certain factors that normally contribute to improved health, such as good nutrition, clean living conditions, and advanced medical care, can actually lead to increased risk for infection. For example, travel can expose people to diseases against which they have little natural immunity. The increased use of immunosuppressants, as well as surgery and other invasive procedures, also heighten the risk for infection. TYPES OF INFECTION Microorganisms responsible for infectious diseases include bacteria, viruses, fungi (yeasts and molds), and parasites. Bacteria are single-cell microorganisms with well-defined cell walls that can grow independently on artificial media without the need for other cells. Bacteria inhabit the intestines of humans and other animals as normal flora used in the digestion of food.Also found in soil, bacteria are vital to soil fertility. These microorganisms break down dead tissue, which allows the tissue to be used by other organisms. Despite the many types of known bacteria, only a small number are harmful to humans. In developing countries, where poor sanitation increases the risk of infection, bacterial diseases commonly cause death and disability. In industrialized countries, bacterial infections are the most common fatal infectious diseases. Bacteria are classified by shape. Spherical bacterial cells are called cocci; rod-shaped bacteria, bacilli; and spiral-shaped bacteria, spirilla. Bacteria are also classified according to their response to staining (grampositive, gram-negative, or acid-fast bacteria); their motility (motile or nonmotile bacteria); their tendency toward encapsulation (encapsulated or non encapsulated bacteria); and their capacity to form spores (sporulating or nonsporulating bacteria). Viruses are subcellular organisms made up only of a ribonucleic acid or a deoxyribonucleic acid nucleus covered with proteins. They’re the smallest known organisms, so tiny they’re visible only through an electron microscope.Viruses can’t replicate independent of host cells. Rather, they invade a host cell and stimulate it to participate in the formation of additional virus particles. The estimated 400 viruses that infect humans are classified according to their size, shape (spherical, rod-shaped, or cubic), or means of transmission (respiratory, fecal, oral, or sexual). Fungi are single-cell organisms whose nuclei are enveloped by nuclear membranes. They have rigid cell walls like plant cells but lack chlorophyll, the green matter necessary for photosynthesis. They also show relatively little cellular specialization. Fungi occur as yeasts (single-cell, oval-shaped organisms) or molds (organisms with hyphae, or branching filaments). Depending on the environment, some fungi may occur in both forms. Fungal diseases in humans are called mycoses. Parasites are unicellular or multicellular organisms that live in or on their hosts and are dependent on the host for nourishment. They usually only take the nutrients they need and rarely kill their hosts, although they can cause harm. Parasites are divided into two types, depending on their relationshipwith the host: Endoparasites live inside the host (for example, protozoans, worms, flukes,and amoebae), while ectoparasites live on the host’s skin (such as fleas, ticks, and lice). HOW INFECTION OCCURS Whether or not an infection develops hinges on variables relating to three crucial factors: ◗ An infectious organism (pathogen) ◗ A host (any organism that can support the nutritional and physical growth of another organism) ◗ A favorable environment As long as one of these factors is missing, infection does not occur.However, if an imbalance develops—for example, if a patient’s immune system is suppressed and can’t fight off pathogens—the potential for infection increases. Infection starts when a microorganism invades body tissue. Once the microorganism breaches the patient’s immune defenses and enters the body, it multiplies and causes harmful effects. The severity of the infection depends on such factors as microbial characteristics, the number of microorganisms present, and the way in which the microorganisms enter the body and spread THE INFLAMMATORY RESPONSE The body reacts to microbial invasion by producing an inflammatory response. The five classic signs and symptoms of inflammation are as follows: ◗ Redness—Caused by dilation of arterioles and increased circulation to the site; a localized blush caused by filling of previously empty or partially distended capillaries ◗ Pain—Results from stimulation of pain receptors by swollen tissue, local pH changes, and chemicals excreted during the inflammatory process ◗ Heat—Caused by local vasodilation, fluid leakage into the interstitial spaces, and increased blood flow to the area ◗ Swelling—Caused by local vasodilation, eakage of fluid into interstitial spaces, and blockage of lymphatic drainage ◗ Loss of function—Results primarily from pain and edema Other manifestations of the inflammatory response include fever, malaise, nausea, vomiting, and purulent discharge from wounds. Not all infections are apparent or symptomatic.With subclinical, or asymptomatic, infection, the infectious microorganism is present and an immune system response is initiated, but the person shows no signs or symptoms of the disease. ENDOGENOUS AND EXOGENOUS MICROORGANISMS Microorganisms may be endogenous or exogenous. Endogenous microorganisms are those found on the skin and in such body substances as saliva, feces, and sputum. They can cause disease in a susceptible individual. xogenous microorganisms originate from sources outside the body.Humans and exogenous microorganisms usually live together in harmony.However, if something disrupts this harmonious relationship, the microorganisms may cause infection. INVASION AND COLONIZATION The presence of microorganisms in or on an individual is called colonization. Colonized microorganisms grow and multiply but may not invade tissue and thus don’t produce cellular injury. In cases of colonization, tissue culture results are positive but the patient lacks evidence of infection. However, some people who are colonized with bacteria do develop localized signs and symptoms of infection—tenderness, swelling, redness, and pus—because the bacteria has invaded the tissue, producing cellular injury.A culture of the pus typically elicits the microorganism. Colonized bacteria may also cause systemic infection, producing fever, an elevated white blood cell count, and possibly shock. PATHOGENICITY Pathogenicity refers to a microorganism’s ability to cause pathogenic changes, or disease. An example of a highly pathogenic microorganism is the rabies virus, which always causes clinical disease in the host. In contrast, alpha-hemolytic streptococci have low pathogenicity; although they commonly colonize humans, they rarely produce clinical disease. Factors affecting pathogenicity include the microorganism’s mode of action, virulence, dose, invasiveness, toxigenicity, specificity, viability, and antigenicity. MODE OF ACTION. The means by which a microorganism produces disease is called its mode of action.Viruses, for example, cause infection by invading host cells and interfering with cell metabolism. Other modes of microbial action include: ◗ Evasion or destruction of host defenses by preventing host phagocytes (scavenger cells) from engulfing and digesting them (used by Klebsiella pneumoniae) ◗ Secretion of enzymes or toxins, which allows the microorganism to penetrate and spread through host tissue (used by the measles virus) ◗ Production of toxins that interfere with intercellular responses (used by tetanus bacilli) ◗ Stimulation of a pathologic immune response (used by group A beta-hemolytic streptococci) ◗ Destruction of T-helper lymphocytes (used by HIV). VIRULENCE. Virulence refers to the degree of a microorganism’s pathogenicity.Virulence can vary with the condition of the body’s defenses.For instance,Mycobacterium aviumintracellulare, bacteria commonly found in water and soil, can cause severe pulmonary and systemic disease in patients with acquired immunodeficiency syndrome but typically do not cause illness in those with a normal immune system.Virulence can be enhanced by several factors: ◗ Toxins produced by bacteria such as Streptococcus and Clostridium ◗ The ability of microorganisms to elude host defenses (such as Pneumococcus with its polysaccharide capsule) ◗ Persistence in the environment (spores and cysts) ◗ Genetic variation (influenza) DOSE. A microorganism must be present in a sufficient dose to cause human disease. The ize of the pathogenic dose varies from one microorganism to the next and from person to person and may be affected by the mode of transmission. The patient’s immune system also plays an important role in the pathogenic dose requirement. In order to cause diarrhea, the infective dose of Shigella is approximately 10 microorganisms, whereas the infective dose of Salmonella required to cause typhoid fever is 1,000 microorganisms. A lower infective dose does not necessarily imply that the organism causes more severe immediate disease. INVASIVENESS. Invasiveness (sometimes called infectivity) refers to the ability of a microorganism to invade tissue. Some microorganisms can enter the human body through intact skin; others can penetrate only through a break in the skin or mucous membranes. Leptospira interrogans usually enters the body through a minor skin abrasion; Clostridium tetani, through a deep puncture wound. The invasiveness of some microorganisms is increased by the enzymes they produce. TOXIGENICITY. Toxigenicity, which is related to virulence, refers to a microorganism’s potential to damage host tissue by producing and releasing toxins. Some bacteria, such as diphtheria and tetanus, release exotoxins that are quickly disseminated in the blood, causing systemic and neurologic manifestations.Other bacteria, such as Shigella, release endotoxins that can cause diarrhea and shock. SPECIFICITY. Specificity refers to the attraction of a microorganism to a specific host or range of hosts. For example, the flavivirus that causes St. Louis encephalitis has a number of hosts, including birds and humans; whereas rubeola, the virus that causes measles, is carried only by humans. VIABILITY. Viability refers to the ability of a microorganism to survive outside the host. Microorganisms can live and multiply in a reservoir, which provides what the microorganisms need to survive. The microorganisms can then be transmitted from the reservoir to another person. ANTIGENICITY. Antigenicity, the degree to which a microorganism can induce a specific immune response, varies among microorganisms. Those that invade and localize in tissue initially stimulate a cellular response, whereas those that disseminate more quickly generate an antibody response.