Enteral Nutrition
advertisement

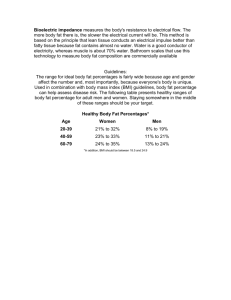
Nutrition I. Essential Nutrients Most essential = water, then energy Macronutrients: Needed in large amounts (hundreds of grams) for energy Micronutrients: vitamins, minerals required in small amounts to metabolize the macronutrients a. Carbohydrates o CHO must be ingested, digested, and metabolized o Simple (Sugars)- monosaccharide, disaccharide (glucose most abundant) o Complex (Starches, fiber)- polysaccharides o Processed foods = “empty calories” lack protein, vitamins, minerals o Types of Carbs 1. Sugars- water soluble, plants & animals, lactose (glu+ galactose) 2. Starches- Insoluble, non-sweet. [grains, bread, legumes, potatoes, pudding] 3. Fiber- plants & fruit; supply bulk to sastisfy appetite and eliminate waste. Present in outer layer of grains, bran o Carb Digestion 1. Enzymes speed up reactions to desired monossacharides in S.intestine 2. Ptyalin (salivary amliase) 3. Pancreatic amylase 4. Disaccharidase (maltase, sucrase, and lactase) o Carb Metabolism 1. Some glucose continues to circulate for readily available source of energy 2. Remainder used as energy or stored 3. Insulin enhance transport glucose into cells o Storage and conversion 1. Stored as glycogen or fat. 2. Glycogen: large polymer of glucose; most stored in liver and skeletal muscles, capable of conversion back into glucose. b. Proteins o Amino acids (C, H, O, N) – ¾ of body solids; tissue growth and immune fn. o Essential AA: can’t manufacture in body o Nonessential AA: can manufacture; also derive from diet and reconstruct new from basic elements. o Complete proteins: all essential + some many nonessential. Most animal proteins (meat, poultry, fish, dairy, eggs) o Incomplete proteins: lack one or more essential, usually from vegetables; (complementary- Combinations of vegetables with diff. essentials or w/ animal protein can be complete; Ex. Noodles w/ tuna, cereal w/ milk) o Protein digestion 1. Mouth: Pepsin breaks down protein into smaller units 2. Pancreas secrete proteolytic enzymes: trypsin, chymotrypsin, and caroxypeptidase II. 3. Intestinal wall glands: aminopeptidase and dipeptidase; breakdown protein into AA o Storage 1. AA absorbed by active transport from S.intestine to circulation 2. Liver uses AA to synthesize plasma proteins (albumin, globulin, fibrinogen) 3. Protein is stored as body tissue, body can’t store excess o Protein balance 1. Anabolism (building tissues) 2. Catabolism (breaking down tissue); excess AA to fat, degradation in liver 3. Nitrogen balance: status of protein nutrition in body c. Lipids o Organic, greasy, insoluble (Water), soluble (alcohol) o Glycerides (simple lipids, most common) o Triglycerides – 90% of lipids in food and body o Saturated triglycerides found in animal products (butter) o Unsatured triglycerides: plant products (olive, corn oil) o Cholesterol: synthesized in liver and diet; create bile acids & steroid hormones. Present in cell membranes and cell structures o Digestion 1. Begins in stomach, mainly in S.intestine (by bile, lipase) 2. To be used, S.intestine and liver convert into soluble lipoproteins o Metabolism 1. Breaks down trig. Into glycerol and fatty acids 2. 1 lb.= 3,500 kcal. 3. Calories from fat, but RBCs need glucose d. Micronutrients o Vitamins: body can’t manufacture; catalyze metabolic processes o Water soluble: C, B-complex, pantothenic acid, biotin o Fat soluble: A, D, E, K. can store; highest in fresh foods o Minerals: organic compounds; Ca & phosphorus (80%) o Macro: over 100 mg, (Ca, phosphorus, Na, K, Mg, Cl, S) o Micro: less than 100 mg (Fe, Zinc, Manganese, I, Fluoride, Co, Cu, chromium, selenium) o Anemia, Osteoporosis Energy Balance a. Energy Intake o Calorie: unit of heat energy b. Energy Output o Metabolism: process by which the body grows and maintains itself; rate of eat liberated during chemical reactions o Basal metabolic rate (BMR): rate at which the body metabolizes food to maintain energy requirements of a person awake and at rest. Activity; Calculated by measuring REE in morning, 12 hrs after eating III. IV. o Resting energy expenditure (REE): energy to maintain basic body fns. (maintain life). Body weight and Body Mass Standards a. Balance b/w expenditure of energy and intake of nutrients b. Ideal body weight (IBW): Optimal weight for optimal health. Rule of 5 F, 6 M c. Body mass index (BMI): changes in body fat stores, weight appropriate to height. Use w/ caution for fluid retentive, athletes, or older adults. (kg/(hgt. in m.)2 Factors affecting nutrition a. Development o Periods of growth (increased needs) o CHD, osteoporosis, HTN= dietary changes b. Sex o Larger muscle mass, pregnant, lactating = greater need of calories and proteins, fluid o Women prior to menopause- more Fe c. Ethnicity and culture o Just follow “universally” accepted guidelines: eat variety for adequate nutrients and moderately o Af.americans: many lactose intolerant, high in fat & Na, curvy ok o Arab: Spices, bread every meal, muslims no pork, Ramadan, feed w/ R.hand o Chinese: served in specific order, lactose int., balance yin/yang avoid indigestion o Jewish: pork forbidden, meat&milk not together o Mexican: hot&cold theory, sweet drinks popular o Navajo: herbs, sheep major, squash&corn major, lactose int. d. Beliefs about food o Fads/myths: support and suggest more nutritious diets e. Personal preferences o Taste, smells, flavor, temp, color, shape, size f. Religious Practices o Orthodox Judaism/islam: prohibit pork o Orthodox jew: kosher (inspected by rabbi) g. Lifestyle o Cooking skill, concern about health, work schedules o Muscular activity- the more strenuous, the greater the metabolism stimulation h. Economics o Higher income: more protein, fat, fewer complex carbs i. Meds and Therapy o Alter appetite, drug utilization, old people o Ca hinder antibiotic o Tetracycline enhance absorption of erythromycin o Antineoplastic agents (oral ulcers, GI bleeding, diarrhea) = diminish nutritional status o Radiotherapy- depending on locaton; swallowing difficultire, n&v, fatigue j. Health V. o Missing teeth, ill fitting dentures, sore mouth o Dysphagia: inflamed throat or stricture of esophagus cause inadequate nourishment o GI surgery (digestion, absorption, metabolism, excretion) o Gallstones (impaired lipid digestion), o Liver disease (impair metabolic processes), o Pancreas (impair glucose metabolism, fat digestion) k. Alcohol consumption o Lead to weight gain (small amount converted directly to fat) o Remainder converted to acetate by liver (released for energy) o Depress appetite, affect intestinal mucosa, increased need for vit.B (alcohol metabolism), impair nutrient storage and excretion l. Advertising o Influence choices and eating patterns o Convenience foods, take out, kids (sweets), elders (supplements) m. Psychological o Anorexia nervosa, bulimia o Overeat when stressed, depressed, or lonely Nutritional Variations throughout the life cycle a. Neonate to 1 year o Higher metabolic rate, immature kidneys, greater h2o loss = greater fluid needs o 80-100 mL breast milk/formula, Q2.5h-Q4h, then solids o slowing of sucking or fall asleep when satisfied o Reduce SIDS by placing in supine for first 6 months o Require Fe supplements prevent anemia (6-18 m) o Bottle mouth syndrome: teeth decay by constant contact with sweet b. Toddler o 33 lbs.= 1250 mL per 24 hrs. o solid food, 3x/day c. Preschooler o Very active; rush through meals. Require snacks o 45 lbs.= 1500 mL d. School age o Protein-rich for physical and mental effort at school o 66 lbs.=1750 mL o Eating habits and regular exercise e. Adolescent o Protein, Ca, vit.D, B o Obesity, depression, anorexia nervosa, bulimiat f. Young adult o Be aware of serving o Fe intake (18mg for menstruating)- organ meats, eggs, fish, poultry, leafy veggies, dried fruit o Folic acid for child-bearing (prevent birth defect) o Prevention of CV, obesity VI. VII. g. Middle-aged adult o Protein, Ca, limit cholesterol and calories o 2-3 L of fluid o Postmenopausal: Ca, Vit.D reduce osteoporosis, antioxidants= CV o late middle age: decreased gastric juice secretions and free acid “heartburn” h. Older adults o Fewer calories (lower metabolic rate and activity) o Decreased saliva, gastric juice secretions o Difficulty sleeping at night (major meal at noon) o Lowered glucose tolerance (complex carbs, fiber rather than sugar-rich) o Neuromuscular/dysphagia: chin-tuck method, thicker consistency Standards for a healthy diet a. Dietary Guidelines o Daily totally fat intake 20-35% of total calories o Less than 1,500 mg of sodium /day o Alcohol (1-women, 2-women/day) b. Recommended Dietary Intake o Estimated avg. requirements (EARs), recommended dietary allowances (RDAs), adequate intakes (AIs), tolerable upper intake levels (ULs) c. Vegetarian Diets o Need complementary protein diet & Fe (leafy greens, whole grains, raisins, molasses) & Ca (soymilk, tofu) o Animal origin (vit.B12), vegans need brewer’s yeast Altered Nutrition a. BMI (25-29.9): overweight (greater than 30): obese b. Increase stress on organs and cause malnourishment c. Improper digestion: inadequate hormones/enzymes, inflammation/obstruction of GI tract d. When undernourished, carb reserves (stored as liver &muscle glycogens) used for 24 hrs., then protein mobilized e. Protein-calorie malnutrition (PCM): starving children & chronic/cancer, depressed visceral proteins, visible muscle and fat wasting f. Somatic proteins (skeletal muscle mass) g. Visceral proteins (plasma proteins, hemoglobin, hormones, antibodies) Nursing Management Assessing a. ABCD (anthropometric, biochemical, clinical, dietary) i. Anthropometric height, weight, BMI ii. Biochemical: lymph, H&H, serum albumin iii. Clinical: Skin, hair, nails, mucous membranes iv. Dietary: 24 hr food recall, food frequency II. Nutritional Screening a. Identify risks for malnutrition or those who are b. Based on dietary hx & physical, use Patient-generated Subjective Global Assessment (well, moderately, severely) III. IV. V. VI. c. Nutrition Screening Initiative (NSI): improved nutritional care for older adults, 9 warning signs Nursing Hx a. Difficulty eating b. Conditions of mouth, teeth, dentures c. Living arrangement, economic status d. Med hx e. Cultural, religious beliefs f. General health status, medical condition Anthropometric measurements a. Non-invasive to quantify body comp. (chronic- progress of months to yrs) b. Skinfold measurement: determine fat stores; usually triceps in mm c. Mid-arm circumference (MAC): measure of fat, muscle, and skeleton. Circumference at midpt. Of arm d. Mid-arm muscle area (MAMA): formula that incorporates TSF and MAC; lean body mass or skeletal muscle reserves Biochemical (Lab) Data a. Serum proteins: visceral protein stores; i. albumin (indicator or prolonged protein depletion)- altered liver fn., hydration status, blood loss ii. Transferrin (binds & carries Fe from intestine through blood): Dec.protein loss, Fe deficient anemia, pregnancy, liver dysfunction iii. Prealbumin (thyroxine-binding or transthyretin): most responsive to rapid changes; 15-35 normal. Intervene @ 11 b. Urinary tests i. Urea: intake & breakdown of protein, rate of urea production in liver, removal in kidneys ii. Nitrogen balance: Protein intake must be recorded, kidney fn. Intact iii. Urinary creatine: reflects total muscle mass; chief end product of creatine produced when energy released during muscle metabolism. Greater the muscle mass, the greater the excretion. iv. Total lymph count: protein depletion cause certain deficiencies and forms of PCM Clinical Data a. Weight changes b. General: easily fatigued c. Skin: Dry, flaky, bruises, lack of fat, edema d. Nails: brittle, pale, spoon shaped e. Hair: dry, loss of color, brittle, dull f. Eyes: pale or red conjunctive, dryness, night blindness (vit.A) g. Lips: swollen, red cracks, vertical fissures h. Tongue: Swollen, beefy red or smooth (B vit. Def.), size diff. i. Gums: Swollen, bleed easily, spongy (vit.C def) j. Muscles: soft, wasted k. GI: anorexia, indigestion, protruding, diarrhea, constipation l. Nervous: decreased reflexes, sensory loss, tingling of hands & feet (vit.B), confusion m. Substantiate with lab tests and dietary data Calculating percentage of weight loss a. Height, current body weight (CBW), usual body weight (UBW) Dietary Data a. Factors that affect nutrition b. 24-hr food recall, food diary (portion), diet hx, food freq. record (types of food) VII. VIII. Diagnosing Imbalanced nutrion Readiness for enhanced nutrition Risk for imbalanced nutrition Activity intolerance R/t inadequate intake of Fe Constipation r/t inadequate fluid and fiber intake Low self-esteem r/t obesity Risk for infection r/t immunosuppression secondary to insufficient protein intake Planning Incorporate ability for self-care, financial resources Implementing I. Clear liquid diet a. Water, tea, coffee, clear broths, soda, plain gelatin. b. Fluid and carbs (24-36 hrs.) post-op, or acute stages of infection (GI) c. Relieve thirst, prevent dehydration, min. stimulation of GI tract II. Full Liquid a. Turn to liquid at body tem, such as ice cream b. GI disturbances c. Low in Fe, protein, and calories. High in cholesterol (amount of milk) d. Ensure or Sustacal (oral supplement) III. Soft/Pureed Diet a. Easily chewed and digested b. Difficulty chewing and swallowing c. Low-fiber IV. Diet as tolerated a. Appetite or ability to eat may change b. Changes according to situation V. Modification for disease a. DM: calorie-restricted b. Cardiac: low sodium, cholesterol VI. Dysphagia a. May aspirate food or fluids into lungs- causing pneumonia b. Stroke, cranial nerve dysfunction, radiotherapy in head and neck c. Thin, nectar-like, honey-like, spoon-thick liquids d. Semisolid/solid foods: pureed, mechanically soft, mechanically altered, regular/general Stimulating the appetite Determine reason for lack of appetite Provide familiar food, small portions, oral hygiene before, analgesics for pain Assisting clients with meals Check each tray with correlating type of diet For a blind person, identify the placement of the food as you would a clock Whenever possible, let them feed themselves Feeding aids (widened, foam, syringe, guards on plates) Enteral Nutrition (EN, Total enteral nutrition (TEN)) Through GI, when unable to ingest foods or upper GI tract is impaired and transport to S.intestine is disrupted NG, small-bore feeding tubes, gastrostomy/jejunostomy tubes I. Enteral Access Devices a. Nasogastric i. Inserted through one of the nostrils, down nasopharynx, into alimentary tract ii. Large bore (larger then 12 Fr) placed in stomach iii. Levin (plastic or rubber, single-lumen w/ holes near tip) iv. Salem sump (larger, double lumen, blue pigtail prevent vacuum if tube adheres to wall of stomach during suction) v. Larger lumen: allow delivery of liquids and suction vi. Smaller bore tubes (smaller than 12 Fr)- more flexible, soft for nutrition vii. Adequate gastric emptying, SHORT-TERM viii. Check gag/cough reflex w/ tongue depressor – prevent accidental placement into lungs ix. Alternative reasons for tubing: prevent n&v post-op, gastric analysis, gastric lavage for OD Check for nasal hx or deviated septum UAP no, can assist with oral hygiene High fowler’s (HOB>30) Hyperextend neck (reduce curvature), choose nostril with greater airflow Small-bore – ensure stylet/guidewire is secured Salem- place in warm water for more pliability Measure distance (tip of nose to earlobe to xiphoid) Lubricate w/ water-soluble (lidocaine anesthetic) If resistance met, withdraw. Relubricaate and insert through the other Once gag reflex met, tilt head forward and swallow to move epiglottis and enter through esophagus (posterior) If continues gag, withdraw slightly and check for coiling in throat II. III. IV. Check placement o Before each intermittent feeding or Q4h (flush 30 mL) o pH 1-5, (greater than 6 indicate lower intestinal tract or resp.) o gastric: Grassy-green, off-white or tan color o Can also test bilirubin (1.5 mg/dL in stomach, more than 10 in intestine) o Intestinal: stained w/ bile, golden yellow or brownish green o X-ray o Listen over epigastrium, while injecting 10-30 mL of air o Confirm length Provide daily tube care b. Nasoenteric (nasointestinal) i. Longer than NG (40 cm/16 in.) ii. Through one nostril into upper S.intestine iii. Specially trained/ primary care provider iv. Used for at risk for aspiration pt. 1. Decreased LOC 2. Poor gag/cough reflexes 3. Inability to participate in procedure 4. Restlessness/agitation c. Gastrostomy/jejunostomy i. LONG-TERM (more than 6-8 wks) ii. Placed surgically or laproscopically iii. Percutaneous endoscopic gastrostomy (PEG) or PEJ iv. Care before healing require surgical asepsis v. After about 1 month, can be removed and reinserted for each feeding Enteral Feedings a. Standard: protein, fat, carbs, minerals, vitamins b. Intermittent: 300-500 mL couple times/day over 30 min. c. Continuous: over 24-hours, infusion pump (kangaroo), essential in small bowel d. Cyclic: nocturnal feedings use higher infusion rates e. Open: flip-top cans/ powdered formula w/ sterile h2o; no more than 8-12 hrs; bag replaced every 24 hrs. f. Closed: prefilled container, can hang for 48 hrs. if sterile g. Refeeding syndrome: shift in fluids and electrolyte after length period of malnutrition/starvation h. Start post-op w/o need to wait for flatus or bm (check for bowel sounds) Managing clogged tubes a. Prevent: 30 mL before, b/w and after b. Reposition pt. to straighten kink c. Alternately flush and aspirate w/ h2o Parenteral Nutrition (TPN) a. IV infusion: dextrose, h2o, fat, proteins, electrolytes, vitamins, trace elements b. yellow c. Hypertonic- into high-flow central veins diluted by blood d. Severe malnutrition, nitrogen imbalance e. f. g. h. i. Infection, fluid/electrolyte/glucose imbalance 1 L= 1000 mL of 5% dextrose = less than 200 cal Prevent hyperglycemia/hypoglycemia – taper on/ off Dextrose bypassing the GI, so give insulin (check glucose Q6h) PPN i. Prevention deficits ii. Smaller peripheral veins- less concentrated solution iii. Can accommodate lipids iv. Phlebitis (vein inflammation) v. Short-term vi. Have separate, dedicated line diff. from med IV vii. White