Results interpretation
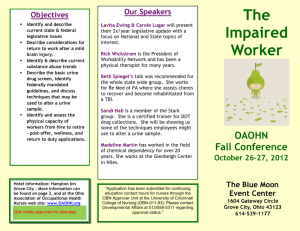
advertisement

Results interpretation Full Blood Count (FBC) Full blood count looks at the number of cells in the blood , their size and each specific type. The common measurements and values of an FBC are below… 9 White blood cells Haemoglobin (Hb) Men Women Mean cell volume (MCV) Haematocrit 4-11 x 10 /L Platelets 150 -300 x 10 /L 13-18g/dl 11.5- 16g/dl 80-100 fL 9 Red blood cells and anaemia Red blood cells carry oxygen around the body in haemoglobin (Hb). A low haemoglobin is termed anaemia. Anaemia is classified on the size of the red blood cells (MCV). Microcytic- small red blood cells MCV <80 Normocytic- normal sized cells MCV (80-100) Macrocytic- large red blood cells MCV > 100 Microcytic anaemia Often termed iron deficiency anaemia, the bone marrow doesn’t have enough iron to produce normal sized red blood cells. This is through… Iron loss: Bleeding (worm infection STH, Schistosomiasis) Menstruation Peptic ulcer disease Inadequate dietary intake of iron: Diet deficient in red meat and legumes Extra requirements Pregnancy/ Lactation Growth (puberty) Provided by T. Whitfield 2012 Treating Iron deficiency anaemia Ferrous sulphate tablets 200mg od to tds will replace iron stores but cause indigestion and black stools. Look to treat any cause praziquantel and albendazole are often given without diagnosis as hookworms and schistosomiasis are so common. Peptic ulcers should be treated with protein pump inhibitors (eg omeprazole), if severe surgical opinion should be sought. Transfusion is appropriate if the anaemia is severe, world wide a Hb less than 8g/dl would be a candidate for transfusion, in Malawi it usually considered at less than 6g/dl, unless the patient is having palpitations and feeling weak. Normocytic anaemia This is usually due to chronic disease as the bone marrow becomes tired and produces less red blood cells, in acute bleed normocytic anaemia is also seen. Common causes of normocytic anaemia Renal Failure (decreased erthropoetin production) Chronic disease: HIV, TB any other long term condition. (This can also be microcytic) Acute blood loss Treatment Treating normocytic anaemia relies on treating the cause, transfusion and iron may be appropriate. Macrocytic anaemia Large cells are formed by the bone marrow due to absence of vitamins. Causes Folate deficiency** Vitamin B12 deficiency ** Alcohol Hypothyroidism **These tend to have an MCV> 120 fL Provided by T. Whitfield 2012 Notes on B12 and folate deficiency Vitamin B12 is absorbed in the jejunum using intrinsic factor released from the stomach. B12 anaemia is rarely due to poor dietary intake. Usually there is a problem with this pathway… Gastrectomy (no stomach to produce intrinsic factor) Pernicious anaemia (antibodies against intrinsic factor, autoimmune disease) Malabsorption of intrinsic factor in jejunum (patient has diarrhoea, takes months) Folate deficiency usually results from a diet absent in green vegetables and fruits deficiency it can develop within weeks. Treating Macrocytic anaemia Folate and B12 anaemia can be diagnosed by testing their levels in the blood. This is not commonly done in Malawi. Vitamin B12 is replaced with intramuscular injections 1mg 6 times spaced over 2 weeks followed by every 6 months afterwards. This avoids needing intrinsic factor. Folate is replaced with a 5mg od tablet. Haematocrit notes Haematocrit looks at the concentration of the blood. A low Hct may indicate dilution of the blood, if the Hct is low then has the sample come from a drip arm? Has the patient been onn a large amount of IV fluids? White cell Count White cells are used for fighting infections, during an infection they are usually raised. Different subsets of white cell are raised in different infections… Neutrophils These tend to be raised in bacterial infections, but also in burns, pancreatitis and other physiological stresses. Lymphocytes These cells tend to be raised in viral infections, they can also be raised in chronic lymphocytic leukaemia. Eosinophils These cells tend to be raised in helminth infections Provided by T. Whitfield 2012 Platelets Platelets are responsible for clotting the blood, they are also often raised in infection. The platelets can also drop and cause spontaneous bleeding. Causes for spontaneous drop in platelets and bleeding include disseminated intravascular coagulation (DIC), Haemolytic Uraemic Syndrome, idiopathic thrombocytopaenic purpura and Thrombotic Thrombocytopaenia. For full assessment you would also need coagulation times which are not routinely done in Malawi. Coagulation disorders with spontaneous bleeding are best managed by giving FFP and platelets. These therapies are often blind as we cannot measure INR or APPT to see if they have been corrected. Provided by T. Whitfield 2012 Cerebro- spinal fluid (CSF) Cerebrospinal fluid is taken via a lumbar puncture; it is usually done on patients with confusion or meningism. CSF is mainly analysed to find which kind of meningitis is present. The first thing to look at is the colour and pressure of the fluid when CSF is reached in lumbar puncture (LP). Bacterial Appearance TB Viral Cloudy Clear mostly Clear WCC/mm 90-1000+ 10-1000 50-1000 Type wcc Polymorph Lymphocyte Lymphocyte Glucose <1/2 blood <1/2 blood >1/2 plasma Protein >1.5 1-5 <1 Organisms Seen Rarely seen Not seen 3 Cryptococcal Meningitis In patients with HIV another common cause for meningitis is cryptosporidium neoformans. This will give a raised pressure when inserting the needle in. Results in cryptococcal meningitis Clear/ slightly turbid fluid Raised lymphocytes Protein increased Glucose slight decrease Staining reveals yeasts India ink stain 75% effective if C.neoformans present Provided by T. Whitfield 2012 Urea and Electrolytes This measures Sodium (Na+) Pottassium (K+) Bicarbonate (HCO3-) Urea or Blood Urea Nitrogen (BUN) Creatinine (Creat) 135-145mmol/L 3.5-5mmol/L 22-28mmol/L (110-140mg/dL) 2.5-6.7mmol/L (7-21mg/dL) 70-150µmol/L (0.6-1.3mg/dL) Sodium When interpreting a sodium level you must know the fluid status of a patient. Questions to ask involve: Is the patient dehydrated? Is the patient Oedematous? Are they on any drugs? Do they have any other medical problems? Hyponatraemia Low sodium can arise in dehydrated, fluid overloaded and normally hydrated patients. Once you know the cause you can look to appropriate treatment. Common causes of low sodium in dehydrated patients Diarrhoea Burns Diuretics (frusemide, HTC) Causes of low sodium in oedematous patients Heart failure Liver failure Renal failure Nephrotic syndrome Rare causes of low sodium in euvolaemic patients Syndrome of inappropriate ADH secretion Hypothyroidism Treating Hyponatraemia If >125 mmol/L it is usually fine to just observe the patients. Provided by T. Whitfield 2012 Try to correct the underlying cause it is usually inappropriate to give salt or saline as the patient is not usually salt deplete, unless there is obvious fluid loss then normal saline may be used. However if the patient is fitting hypertonic saline can be given to correct the sodium (rarely done). The caution of giving sodium is that too fast correction of sodium can cause irreversible brain damage(by osmotic demyelination in the brain). In correcting the sodium aim for 10mmol/L per day this can be calculated as one litre of N saline will raise the concentration by 4-5 mmol/L Hypernatraemia Hypernatraemia is most commonly due to dehydration (burns, vomiting etc) Hypernatraemia can also be caused by… Excessive Normal saline Too high blood sugar After head injury - diabetes insipidus Treating hypernatraemia Usually give fluids to correct dehydration. Pottassium Hyperkalaemia There are few symptoms of hyperkalaemia itself with patients often just collapsing with arrthymias or sudden death. Symptoms may relate to the underlying cause eg. oliguria/anuria in renal failure. Hyperkalaemia is common in renal failure where K+ is usually excreted at the expense of Na+ renal failure means an excess of potassium is retained. The potassium sparing diuretic spironolactone is a common cause of hyperkalaemia. Other causes include acidosis, muscle cell destruction and burns. Artefact: high potassium can occur when red blood cells break down inside the collecting tube if it is unexpected then it should be repeated. Raised potassium above 6.5 mmol/l can cause life threatening arrthymias, it is treated … Calcium gluconate 10% 10ml given iv to prctect the heart Provided by T. Whitfield 2012 Insulin 10-20 units in 10% dextrose given over 5hours (the insulin drives the potassium into the cells Salbutamol nebulisers 5mg also drive potassium back into the cells. In severe hyperkalaemia it may be appropriate to dialyse. Then look to treat the underlying cause. Hypokalaemia If the potassium is <2.5mmol/L it can be life threatening symtpoms and complications include muscle weakness, hypotonia, cramps and arrhythmias. Common causes of hypokalaemia include vomiting, diarrhoea and other intestinal problems. The diuretic drug frusemide is also responsible for lowering potassium. Treating hypokalaemia Correct the underlying cause and replace the potassium, in severe hypokalaemia (<2.5mmol/L) replace intravenously slowly at no more than 20 mmol over an hour, any faster can lead to arrhythmia. In less severe hypokalaemia oral sando K can be given at 1-2 tablets up to three times a day. Potassium tablets should not be given for more than 5 days to avoid hyperkalaemia. Bicarbonate Bicarbonate measures the acidity of the blood it is low if the blood is acidic and raised in alkalosis. Common causes of acidic blood… Lactic acidosis (is the patient on ARVs ? metformin?) Diabetic ketoacidosis (check the blood sugar) Renal failure (urine output) Acidotic patients should be given lots of fluid to wash out and dilute the acid, the urine output and fluid status should be monitored whilst doing this to avoid fluid overload, any causative drugs should be withdrawn. Urea and Creatinine Urea and creatinine are markers of renal function. They are raised in acute kidney injury and in chronic renal failure. Provided by T. Whitfield 2012 Urea/BUN may also be raised in muscle damage and gastrointestinal bleeding as the blood/ muscle cells are digested it raises the urea levels. Liver Function Tests (LFTs) Liver function tests consist of Billirubin (bil) Alanine aminotransferase (alt) Aspartate transaminase (ast) Alkaline phosphatase (ALP) Albumin (alb) 3-17 µmol/L 3-35 iu/L (1-1.4 mg/dL) 3-35 iu/L 30-300iu/L 35-50 g/L (3.5-5.5 U/L) A raised bilirubin is seen as jaundice in the patient. Jaundice is classified as… Pre-hepatic Intra hepatic Post-hepatic Pre-hepatic jaundice Pre-hepatic jaundice in adults is usually caused by blood haemolysis and should therefore be present with anaemia. The patient should not have any disruption to their other liver enzymes. Urobiligen in the urine and increased reticulocytes on a blood film would be expected. Intra-hepatic jaundice Intra-hepatic jaundice will present with elevation of all liver enzymes, elevated bilirubin and either low or normal albumin. The ast, alt and alp all be elevated the ast and alt are usually higher than the alp. The most common causes of intra-hepatic jaundice are viruses such as Epstein Barr virus (EBV), Hepatitis A, Hepatitis B, Hepatitis C as well as alcohol, Tuberculosis medications and malignancy. Usually there is no pain associated with these conditions. Post-hepatic jaundice Post hepatic jaundice is caused by obstruction of the billary tree. This causes a back log of conjugated bilirubin from the bile ducts to the blood. The liver enzymes will all be elevated as in intra-hepatic jaundice, however in post hepatic jaundice the alp tends to be greatly elevated above the ast/alt. Common causes of post hepatic jaundice include gall stones blocking the bile duct, pancreatic tumour and billary stricture. Gall stones are very painful as opposed to tumours. Provided by T. Whitfield 2012 In Malawi abdominal ultrasound is used in all jaundice cases to look for correctable obstructive causes and to look at the texture of the liver. Albumin Albumin is a measure of the synthetic function of the liver. In cirrhosis the function of the liver is poor and albumin will drop. Chronic disease states such as malnutrition, HIV and TB will also lower the albumin as the liver is compromised. Provided by T. Whitfield 2012 Analysing urine This is done through analysing the urine in the lab and urine dipstick on the ward. Urine dipstick This measures: Blood: shouldn’t be present, positive in UTI, Glomerulonephritis, bladder/renal tumour, schistosomiasis, trauma (catheter), renal stones Leucocytes (White cells): present in infection mainly. Ketones: present in starvation at low levels, tends to be greater than ++ in DKA Nitrites: the break down product when bacteria digest nitrate, positive in UTI Protein: +++ protein by itself with nil else suggests nephrotic syndrome, also can be present in glomerulonephritis, UTI, exercise and pregnancy. Diabetic renopathy will have protein in the urine as the disease progresses. Bilirubin present on the dipstick indicates obstructive jaundice Urobilinogen: indicates pre-hepatic jaundice Specific gravity range 1.000- 1.030 indicates the density of the urine and indicates the degree of protein/ blood in the urine. Urine microscopy This looks at the urine under a microscope to see what is in the urine. Urinalysis measures Red cells: which occur for the same reasons as in the dipstick. >2mm3 is abnormal White cells: for the same reasons as in the dipstick, but they are counted for significance. >10/mm3 is abnormal Protein: this will state the volume being excreted. Should be <150mg/day, it can be raised for the same reasons as protein is found on the urine dipstick. Microscopy will detect lower levels of proteinuria. Casts are also seen in the urine Casts are made when the cells/ material bunch together in the glomerulus to form a lump which is then passed out in the urine. The casts have the shape of the part glomerulus where they formed. Hyaline/ granular casts: these occur commonly in individuals who exercise and those taking loop diuretics. Dense granular casts can occur in diabetic nephropathy and glomerulonephritis. Red cell casts: indicate any blood found has come from the glomerulus this happens in extreme hypertension and glomerulonephritis. White cell casts: occur in pyelonephritis and some forms of glomerulonephritis. Provided by T. Whitfield 2012 Fatty casts: in heavy proteinuria Epithelial cell casts: in acute tubular necrosis or glomerulonephritis. Pleural Fluid analysis These are classified according to their protein content as either transudates (<30g/L)or exudates (>30g/L). Transudates are commonly due to… Increased venous pressure, Hypoproteinaemia (low oncotic pressure) Cardiac failure Cirrhosis Pericarditis Nephrotic syndrome Fluid overload Malabsorption Ascitic fluid analysis Malnutrition A transudate may also be related to ovarian cancer (right sided effusion in Meigs syndrome) and in hypothyroidism. Exudates are commonly due to… Pneumonia Malignancy (lymphoma, Kaposi sarcoma, others) TB Blood in the pleural cavity suggests malignancy, trauma or TB. If lymphocytes are the dominant white cell Tb is also suggested. Provided by T. Whitfield 2012 Ascitic fluid analysis Ascitic fluid looks at white cell count greater than 200 suggests bacterial peritonitis. If these are mainly lymphocytes then it could be TB peritonitis. Culture is performed to determine the organism. Protein levels are greater than 30 g/L in the following conditions Malignancy TB Bacterial infection Pancreatitis Protein levels are less than 30g/L in the following conditions Congestive cardiac failure Nephrotic syndrome Cirrhosis Myxoedema Portal vein thrombosis Diuretic therapy can increase protein levels in the ascitic fluid in conditions where it would normally be <30g/L. Bloody ascites is usually due to malignancy and occasionally TB. Provided by T. Whitfield 2012