Pilot Use of SystmOne STOPP Toolkit (East
advertisement

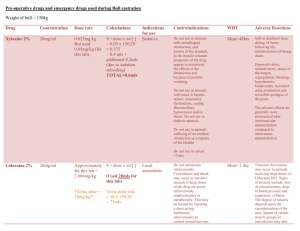
Use of STOPP Toolkit: background and review of application in practice at East Parade surgery October 2015. Background ‘STOPP’ stands for Screening Tool of Older People’s potentially inappropriate Prescriptions. This was originally devised in 2008, and has been thoroughly reviewed and updated in 2014: http://ageing.oxfordjournals.org/content/early/2014/10/16/ageing.afu145 The medications included in the STOPP criteria are significantly associated with adverse drug reactions. Applying STOPP criteria during acute hospital admission has been shown to significantly improve medication appropriateness 6 months post intervention and reduce adverse drug reactions. The tool is validated for patients over 65, but is specifically recommended in patients considered to be ‘frail’. The tool identifies markers of frailty and reviews medications, giving recommendations on reviewing these for interactions, and side effects and drugs to consider stopping or dose reduction. There is a second tool used in conjunction with ‘STOPP’ called ‘START’ which gives recommendations on suitable drugs that should be considered. This does not form part of the STOPP tool kit on System One so has not been assessed. Frailty is currently a ‘hot topic’ with the British Geriatric Society in conjunction with the RCGP having published their ‘Fit for Frailty’ Best Practice Guidance for the care of older people living with frailty in community and outpatient settings in 2014: http://www.bgs.org.uk/index.php/resources-6/bgscampaigns/fit-for-frailty Conducting a personalised, evidence based medication review is one of the key recommendations of the guidance. The STOPP/START tool is recommended as one way to assist with this. Trial of System One STOPP protocol at East Parade 22 residents of a local nursing home were chosen for the initial trial of the tool. This group was picked because they all fulfil the criteria for frailty. STOPP Alerts were generated in 15 of the 22 patients. No concerns were identified in the remaining 7 patients. Single alerts (12 patients) Alert Review use of PPI for uncomplicated peptic ulcer disease or erosive peptic oesophagitis at full therapeutic dosage for > 8 weeks (dose reduction or earlier discontinuation indicated) Number of patients 4 patients Review drugs likely to cause constipation in patients with chronic constipation. 2 patients Review hypnotics Review use of acetylcholinesterase inhibitors is a patient with known heart block OR on concurrent treatment with drugs that reduce heart rate Review antimuscarinics for OAB in patients with concurrent dementia / cognitive impairment / narrow angle glaucoma or chronic prostatism Review loop diuretic in patient without heart failure diagnosis Review loop diuretic in patient with urinary incontinence Review use of vasodilating drugs in patient with persistent postural hypotension 1 patient 1 patient Action Taken Stopped completely for one patient as no clear indication. Dose reduced to maintenance level for the 3 other patients who were all on concurrent anti-coagulation (NICE CKS recommends low dose PPI in patients at high risk of GI side effects http://cks.nice.org.uk/antiplatelettreatment#!scenariorecommendation ) No changes made as little scope to do so (one patient required current level of opiate pain relief, and the other had iron deficiency anaemia so iron therapy was appropriate) Attempt made to tackle this again Betablocker stopped as this patient had ongoing hypotension and falls. 1 patient Stopped, with review of symptoms planned. 1 patient Stopped as no obvious indication to remain on this Continued as required diuretics for symptomatic treatment for heart failure. Continued because her BP had recently been monitored on and off treatment on ongoing use considered appropriate 1 patient 1 patient Multiple alerts (3 patients) Alerts 3 Alerts: Long term use of PPI. Number of patients 1 patient Reduce lansoprazole to 15mg (on warfarin). Regular use of cyclizine reviewed, but continued as still needed and appears to be effective. Stop repeat of codeine as rarely using. Use of first generation antihistamine. Constipating agents. 5 Alerts: Action Taken 1 patient Loop diuretics and incontinence Continue furosemide 40mg as HF symptoms better with this dose. Continue prn codeine as cannot tolerate other pain relief. Try lower dose amitriptyline with a view to stopping. Reduce lansoprazole to 30 mg od initially, with a view to cutting down to 15mg. Reduce dose bisoprolol as BP tends to be low Constipating agents Tricyclics – avoid first line for depression Long term PPI Vasodilators / postural hypotension 3 Alerts: Tricyclics in patient with dementia Hypnotics Constipating agents 1 patient Reduce amitriptyline back to 25mg with a view to further reductions. Discuss lower dose zopiclone once amitriptyline tackled. Quantities of tramadol on repeat reduced. Overall 5 drugs were stopped completely and dose reductions were made for another 8 drugs, with plans to review further for 3 of these. 7 drugs were reviewed and continued use felt justified. Conclusions The STOPP protocol appears to be a useful tool in helping to identify inappropriate prescribing that might otherwise have been overlooked. In particular, avoiding long term used of treatment dose PPI has been a useful learning outcome, and there appears to be scope for wider application of this prescribing point, which was flagged up in 6 out of 22 patients. This tool is most likely to be useful when GPs are doing annual reviews or medication reviews of care home patients, care plan patients, and any other patients with identified frailty. Further Actions Follow up audit planned in 2 months time to review any adverse outcomes of cessation of medication, and any items that have been recommenced. Emma Huskins, salaried GP, October 2015