saq 5 - stemi
advertisement

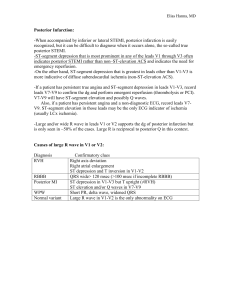
QUESTION 5 MMC Prac fellowship exam, June 2015. Papers marked by: Michaela Mee Background re: Posterior STEMI Often missed dx 15-21% of STEMis strict/ ‘true’ posterior AMI : 3-10% 22% of ‘true’ posterior STEMI have mod-severe mitral regurg often accompanied by inferior/lateral stemi Usually due to to occlusion of RCX, but may also be due to RCA occlusion In 10% of pt, RCX is the dominant vessel Classic post stemi includes ST dep in ant leads, and also prominent R waves in anterior leads (equivalent of Q ie once evolving) and prominent T waves too. However the latter ECG changes not required. Below is just a guide as to how I marked the question. I am not an examiner and I have likely been kinder than an examiner would, so beware! Look out especially for unsafe (non-judicious) use of IV fluids/ certain drugs, given patient is (1) likely APO and (2) cardiogenic shock. Examiners might give auto mark of 0 for that section if unsafe dosing. Pass rate was 81% using my marking system and assuming pass mark 17/30 Part 1 max grade 8/8 Part 2 max grade 12/12 Part 3 max grade 10/10 Part1: Best answers: (2 pt each) Best answers give info relevant to the diagnosis, or help exclude differential +: ST dep V1-4 1-2mm -: No prominent T waves -: No prominent R wave in V1-3 (equiv of Q in post leads) -: No significant inferior/lateral STE (<1mm) -: Normal SR ..other appropriate Dx: (Early) (isolated/true) Posterior STEMI Can add: possible evolving high lateral/inf stemi (not yet meeting criteria), but had to get posterior to pass question Can add: in patient with likely cardiogenic shock and APO Acceptable; (0.5-1.5) but not as useful in deciding diagnosis Eg Normal axis Use of term ‘infarct’ rather than STEMI Wrong/not good/no points: (0) Put three dx (which do I choose?) RV infarct Inferior stemi (STE is not significant in these leads, <0.5mm)) NSTEMI Incorrect ECG interpretation Unsafe answer, or missed posterior STEMI: (auto fail this part, get 4/8 max) Part 2: Best answers: (2 pt each to max 12) General: -Resus, full cardiac monitoring, defib pads, team approach A/B: -PPV/CPAP/BIPAP/NIV 100%O2, while prepare to intubate C: -IV inotropes eg adrenaline eg 5mcg/min IV infusion, eg 10mcg boluses -IV, Send bloods GpH, trop, vbg, fbe euc coag -Cautious IV fluid (eg 250ml bolus NS), careful as likely APO Rx: -Referral: cardiology interventionist, for PCI/cath lab urgent -Antiplatelet: aspirin 300mg -clopidogrel 600mg, pre cath lab, dosing included -Analgesia eg fentanyl cautious dosing eg 25mcg increments Other: -Confirm dx: posterior ECG V7-9, STE >0.5mm confirms, BUT NOTE: normal post leads doesn’t exclude posterior STEMI! Acceptable: (0.5-1.5 each) IV fluid 500ml NS, but must mention caution/titration/look for response Notify NOK Consider mitral valve rupture (TTE) +/- surgical referral GTN/frusemide if BP corrected Attach defib pads/ full cardiac monitoring Remove GTN patch ?check for signs of Aortic Dissection CXR (1) Bedside cardiac echo if available quickly (1.5) Not so great: GTN infusion given acutely in hypotension (need clarifying statement) -morphine analgesia ‘2.5-10mg’ (careful how you write drug doses, can be interpreted as 10mg stat) ?norad upper range 70 mcg/min (this upper range you wouldn’t go to with this pt) need end points/aims here atropine 150-300mcg (low dose, and why?) ‘atropine 1mg for bradycardia’ (I wouldn’t do this in STEMI with HR 60) Unsafe: (auto fail score 0 for that part) Incorrect dose inotrope eg Adrenaline 5mg/min (likely due to messy writing/rushed writing) = UNSAFE -IV fluid 20ml/kg stat (usually people who thought it was RV infarct) NB in APO? Part 3: ‘Timing’ has been interpreted in different ways. Best to think of as time in relation to induction drug or order of drugs and time between. Some people made intervals between drug x as per if you repeated same drug x (ie ‘frequency’) which doesn’t make sense for RSI 1 point for acceptable drug 1 point for appropriate dose 0.5pt for correct timing. Remember this is emergent! 5 min wait between fentanyl and induction doesn’t make sense! Best (2.5 each max): 1. Analgesic eg Fentanyl 100mcg, given pre induction approx 1-2 min prior 2. Induction -high dose fentanyl would have been good choice (but no one did this) -Ketamine 2mg/kg approx 3. Neuromuscular blockade : -Sux 1-1.5mg/kg/150mg, -or Roc ~1.2mg/kg 4. Circulatory support: -adrenaline eg infusion 1-200 mcg/min, or 10-50mcg boluses acceptable -OR metaraminol eg 0.5-1mg boluses IV OK/acceptable 2. Induction: Propofol cautiously dosed eg 0.5mg/kg Midaz cautiously dosed eg 2mg Not good: Induction: -ketamine dose <1mg/kg (too low), or 3-5mg/kg IV (too high) -2 agents given for induction (cant give points for alternate drugs Inotrope/circ support: -metaraminol dose too high, or too low! -Norad dose too high -500ml-1L pre induction (that candidate may have thought RV infarct) -atropine 1mg as bradycardic Neuromuscular blockade: 2 RSI agents given Timing: Eg small doses of fentanyl 25-50 mcg ‘titrated every 4-5 min until total 150-200mcg’: this is not great in emergent RSI for cath lab ‘Ketamine for sedation’ (sedation is not the same as induction, induction dose given by candidate) Unsafe: -midazolam dose 0.1mg/kg (eg ?10 mg if 100kg??!!) stat 2 L NS Unsafe doses --> auto reduction in mark for that section to max 5/10 Examiners likely to be harsher APPENDIX: to Q5 Appendix 1: from Dr Smith’s ECG Blog Some ways to differentiate subendocardial ischemia from posterior STEMI First, you should know that when there is precordial ST depression due to subendocardial ischemia, it is not necessarily due to anterior wall ischemia. Data from stress testing shows that subendocardial ischemia DOES NOT LOCALIZE on the ECG, and usually is in leads II, III, aVF and V4-V6. But, again, this does not tell you which artery is involved. Second, ST depression in V1-V3, vs. V4-V6, is much more likely to be posterior than subendocardial ischemia. Third, patients at higher risk of NSTEMI (older, more risk factors, h/o angiogram with multivessel disease) are much more likely to have subendocardial disease (vs. younger smoker). Fourth, patients with reasons to have demand ischemia (tachycardia, sepsis, GI Bleed, etc.) are much more likely to have subendocardial ischemia (like in a stress test); those with posterior MI are much more likely to present with onset of chest pain and with normal vital signs. Fifth, look for tall R-waves in V1-V3 (the analog of Q-waves in other locations). Sixth, placement of posterior leads (take leads V4-V6 and place them at the level of the tip of the scapula, with V4 placed at the posterior axillary line ("V7"), V6 at paraspinal area ("V9"), and V5 ("V8") between them. At lease 0.5 mm of ST elevation in just one lead is very sensitive and specific for posterior MI. Seventh, an immediate echocardiogram can make the distinction. These are very difficult and it is very hard to detect a posterior wall motion abnormality unless you are very experienced. I recommend a formal study with Definity before concluding there is no posterior wall motion abnormality. Eighth, see above. Whether or not it is STEMI, the cath lab should be activated if the ischemia cannot be controlled medically: aspirin, nitro, beta blockers, clopidogrel, heparin/enoxaparin, GP IIb/IIIa inhibitor.