Dissociative Disorders
advertisement
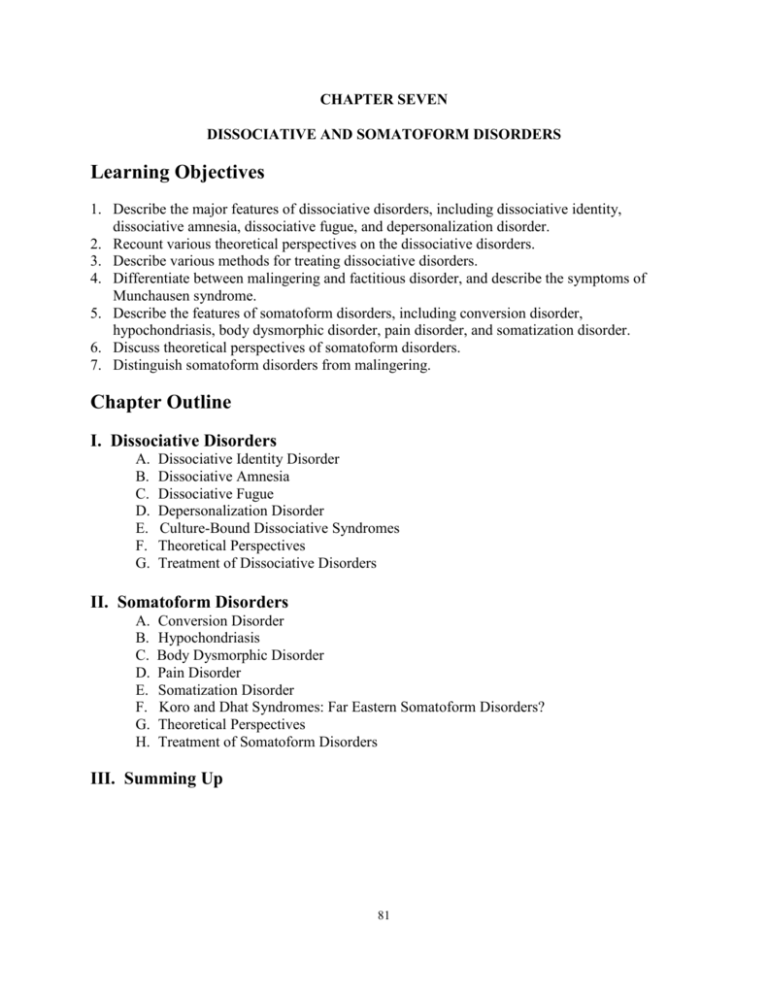
CHAPTER SEVEN DISSOCIATIVE AND SOMATOFORM DISORDERS Learning Objectives 1. Describe the major features of dissociative disorders, including dissociative identity, dissociative amnesia, dissociative fugue, and depersonalization disorder. 2. Recount various theoretical perspectives on the dissociative disorders. 3. Describe various methods for treating dissociative disorders. 4. Differentiate between malingering and factitious disorder, and describe the symptoms of Munchausen syndrome. 5. Describe the features of somatoform disorders, including conversion disorder, hypochondriasis, body dysmorphic disorder, pain disorder, and somatization disorder. 6. Discuss theoretical perspectives of somatoform disorders. 7. Distinguish somatoform disorders from malingering. Chapter Outline I. Dissociative Disorders A. B. C. D. E. F. G. Dissociative Identity Disorder Dissociative Amnesia Dissociative Fugue Depersonalization Disorder Culture-Bound Dissociative Syndromes Theoretical Perspectives Treatment of Dissociative Disorders II. Somatoform Disorders A. B. C. D. E. F. G. H. Conversion Disorder Hypochondriasis Body Dysmorphic Disorder Pain Disorder Somatization Disorder Koro and Dhat Syndromes: Far Eastern Somatoform Disorders? Theoretical Perspectives Treatment of Somatoform Disorders III. Summing Up 81 Chapter Overview Dissociative Disorders Dissociative disorders involve changes or disturbances in identity, memory, or consciousness that affect the ability to maintain an integrated sense of self. Dissociative disorders include dissociative identity disorder, dissociative amnesia, dissociative fugue, and depersonalization disorder. In dissociative identity disorder, two or more distinct personalities, each possessing well-defined traits and memories, exist within the person and repeatedly take control of the person's behavior. Dissociative amnesia involves loss of memory for personal information. There are five types of dissociative amnesia: localized, selective, generalized, continuous, and systematized. In dissociative fugue, the person travels suddenly away from home or place of work, shows a loss of memory for his other personal past and experiences identity confusion or takes on a new identity. Depersonalization disorders involve persistent or recurrent episodes of depersonalization that are of sufficient severity to cause significant distress or impairment in functioning. Psychodynamic theorists view dissociative experiences as a form of psychological defense by which the ego defends itself against troubling memories and unacceptable impulses by blotting them out of consciousness. There is increasing documentation of a link between dissociative disorders and early childhood trauma, which lends support to the view that dissociation may serve to protect the self from troubling memories. To learning and cognitive theorists, dissociative experiences involve ways of learning not to think about certain troubling behaviors or thoughts that might lead to feelings of guilt or shame. Relief from anxiety negatively reinforces this pattern of dissociation. Within the diathesis-stress model, dissociative identity disorder may be explained in terms of a diathesis consisting of psychological traits, such as a rich inner fantasy life and high levels of hypnotizability interacting with traumatic stress in the form of severe childhood abuse. Treatment of dissociative disorders from the biological approach focuses on the use of drugs to treat the anxiety and depression often associated with the disorder; but drugs have not been able to bring about reintegration of the personality. Learning perspectives focus on the use of behavioral methods of reinforcement of the most well-adjusted personality. Somatoform Disorders In somatoform disorders, there are physical complaints that cannot be accounted for by organic causes. Thus, the symptoms are theorized to reflect psychological rather than organic factors. Four types of somatoform disorders are considered: conversion disorder, hypochondriasis, body dysmorphic disorder, and somatization disorder. 82 In conversion disorder, symptoms or deficits in voluntary motor or sensory functions occur which suggest an underlying physical disorder but no apparent medical basis for the condition can be found. Hypochondriasis is a preoccupation with the fear of having, or the belief that one has, serious medical illness, but no medical basis for the complaints can be found and fears of illness persist despite medical reassurances. People with body dysmorphic disorder are preoccupied with an imagined or exaggerated physical defect in their appearance. Somatization disorder, formerly known as Briquet's syndrome, involves multiple and recurrent complaints of physical symptoms that have persisted for many years and began prior to the age of 30, but most typically during adolescence. The psychodynamic view holds that conversion disorders represent the conversion into physical symptoms of the leftover emotion or energy that is cut off from unacceptable or threatening impulses that the ego has prevented from reaching awareness. The symptom is functional, allowing the person to achieve both primary and secondary gains. Learning theorists focus on the reinforcements that are associated with conversion disorders, such as the reinforcing effects of adopting a "sick role." A learning theory view likens hypochondriasis to obsessive-compulsive behavior. Cognitive factors in hypochondriasis include self-handicapping strategies and cognitive distortions. Psychoanalysis seeks to uncover and bring to the level of awareness the unconscious conflicts, originating in childhood, that are believed to be at the root of the problem. Once the conflict is uncovered and worked through, the hysterical symptom should disappear because it is no longer needed as a partial solution to the underlying conflict. Behavioral approaches focus on removing sources of reinforcement that may be maintaining the abnormal behavior pattern. Behavior therapists may also work more directly to help people with somatoform disorders learn to handle stressful or anxiety-arousing situations more effectively. Cognitive techniques such as cognitive restructuring have been very helpful in treating hypochondrias and body dysmorphic disorder. Lecture and Discussion Suggestions 1. Differentiating dissociative identity disorder and schizophrenia. People easily confuse these two disorders, yet they are very different disorders. The term schizophrenia comes from two Greek words meaning "to split" "the mind." However, Bleuler, who proposed the term schizophrenia, was not referring to a splitting of the person into different personalities, as occurs in dissociative identity disorder. Instead, the split in schizophrenia occurs at the core of the person, loosening the connections between the various psychic functions. Thus, in the mind of the person with schizophrenia, ideas, perceptions, emotions, and behavior don't operate as an integral whole; rather he or she may think and act inappropriately in a given situation. Consequently, schizophrenia is a psychotic disorder that usually requires periods of hospitalization and medication as well as a prolonged time for recovery. People who have recovered from an acute episode of schizophrenia often remain loners or underemployed in the workplace. In contrast, many people with dissociative identity disorder may go unrecognized or be alternatively diagnosed for years after the initial evaluation. Some of them lead accomplished lives. Well-functioning people with multiple personalities may elude diagnosis because 83 clinicians are not likely to probe for evidence among those who function so well. Also, such people may have developed elaborate strategies for concealing their alternate personalities, aided by the stabilizing influences of their careers. An analogy I have used in my classes to help students visualize the differences between the two disorders is that dissociative identity disorder is somewhat like taking a large mirror and neatly cutting it into several small mirrors. They are smaller but they are still clearly mirrors. Schizophrenia, however, is like taking that same large mirror and shattering it with repeated hammer blows. What you have left is a collection of glass fragments, none of them comprising a recognizable mirror. While this analogy is not perfect, students typically find it helpful. 2. Child sexual abuse and the dissociative and somatoform disorders. Freud first identified childhood experiences of sexual abuse as a significant factor in the psychoneuroses, though he eventually dismissed them as fantasies. Today, however, there is increasing documentation of childhood sexual abuse in the lives of those who develop dissociative identity and somatization disorder. For instance, it has been estimated that as many as one out of four or five girls and one out of nine or ten boys are sexually abused before they reach 18. Certainly, only a few of these children who suffer such childhood traumas develop multiple personalities. Yet, recent recognition that this disorder is not as rare as once thought suggests that we not overlook the link between child sexual abuse and dissociative identity disorder. Similarly, one study of women with somatization disorder, compared to those who suffered from a mood disorder, showed significant differences. Although women in both groups reported similar childhood sexual experiences, such as masturbating and kissing games, women with somatization disorder were more likely to report experiences of childhood sexual abuse. More than one out of two women with somatization disorder had been sexually abused, compared to only one out of six of those with a mood disorder (Morrison, American Journal of Psychiatry, 1989, 146, 239-241). 3. Hypochondriasis. Estimates of anywhere from one-fourth to three-fourths of the patients who consult physicians resemble those with hypochondriasis or some other somatoform disorder. A disproportionate number of these people are from the lower socioeconomic groups, who complain more about physical symptoms than psychological discomforts. Also, people coping with bereavement over the loss of loved ones are especially prone to symptoms that mimic signs of physical illnesses. Even though older people are susceptible to genuine age-related changes in their health, their complaints often reflect the changing health status of older people. Because people with hypochondriasis are often offended at the suggestion that their beliefs or fears may be unwarranted, they frequently become "doctor shoppers" and complain that they are not getting proper care, thereby alienating themselves from doctors. Furthermore, they frequently refuse referral for psychotherapy, and are not often seen in mental health facilities. In some instances, past experience with a true organic disease, either in one's self or family member, predisposes one to this illness. At the same time, because many complaints may be manifestations of early stages of neurological or endocrine disorders, the most important differential diagnosis is the lack of a true organic disease. However, according to the DSM-IV, even the presence of a genuine physical illness doesn't preclude the coexistence of hypochondriasis. 84 4. Differential development of dissociative disorders. Ask students why some people who are sexually abused as children develop dissociative identity disorder while most do not. Certain personality traits have been associated with the development of dissociative identity disorder, such as proneness to fantasize, increased susceptibility to hypnotic suggestion, and openness to altered states of consciousness. These factors may predispose them to dissociative responses to extreme stress. Although these factors explain why some develop dissociative identity disorder, it does not explain why females are more likely to develop it than males. 5. Multiple personalities. Pose the question, "Don't all of us have multiple personalities to some extent?" Some people question whether multiple personality disorders represent more than an extreme form of the multiple selves found in all of us. That is, our self-concept includes hundreds of self-perceptions of varying degrees of clarity and intensity, which represents various self-images, needs, interests, and social roles integrated within our personality in varying degrees. Expression of these various selves may account for much of the inconsistency in our behavior on occasions. 6. Malingering. Ask students how they can tell when someone is faking a dissociative disorder or an illness. According to the DSM-IV, the essential feature of malingering (pretending) is intentional production of false or grossly exaggerated physical or psychological symptoms, motivated largely by external incentives such as avoidance of work or military duty, or obtaining financial compensation or drugs. Also, the presenting symptoms are less likely to be symbolically related to underlying emotional conflicts, as they are in dissociative and somatoform disorders, nor relieved by hypnosis or suggestion. 7. Out of body experiences. Two of the most well-publicized types of dissociation are the socalled "out of body" experiences and "near death experiences." You might ask students to relate any knowledge they have of these experiences and then explore how various theoretical viewpoints might scientifically explain them. You might also point out that while most scientists remain skeptical about people actually leaving their bodies, many readily admit that the people claiming to have had the experiences appear to be truthful in their belief that the experience was real. What scientific evidence is there to support or refute claims that one's soul has left one's body? What alternative explanations are there and what scientific evidence is there to support them? This topic makes for an interesting discussion as it is an area that many students are keenly curious about. 85 8. Depersonalization experiences. The text describes some of the forms depersonalization can take. Some of these forms occur from time to time in otherwise normal individuals. Because your students might read this section and wonder "Do I have depersonalization disorder?", it is useful to point out how common such episodes are. Ross, Joshi, and Currie (1990) found that these were especially reported by people age 25-44. For instance, 28 percent of those 25-34 and about 27 percent of those 35-44 indicated they had experienced depersonalization. Rates were from 8-10 percent for most other age groups. It is also important to remind students that DSM-IV considers depersonalization disorder only when it is persistent and results in significant impairment of functioning. Ross, C. A., Joshi, S., & Currie, R. (1990). “Dissociative experiences in the general population.” American Journal of Psychiatry, 147, 1547-1552. 9. Repressed memories? The topics of dissociative identity disorder and amnesia discussed in this chapter lead well into one of the major controversies of the day – repressed memory therapy. The roots of this issue go back at least to Sigmund Freud, who originally felt that many of the problems reported to him by female patients were due to childhood experiences of incest. These women were telling Freud, often while under hypnosis, that they had begun to remember these acts. Freud believed this for awhile, but gradually became convinced most of these incestual experiences were fantasized. This was a widely held opinion until about 1980, when it became clear that incestuous child abuse was much more common than thought. Then, as writer Martin Gardner tells it, "In the latter 1980s a bizarre therapeutic fad began to emerge in the United States. Hundreds of poorly trained therapists, calling themselves "traumatists" began to practice the very techniques Freud discarded." What began was a wave of incidents in which patients, generally women 25-45 years old, began to recall childhood sexual traumas that had allegedly lain buried in the unconscious, often for decades. In 1990, the first conviction based on repressed memories was handed down to a man for murdering a young girl in 1969. Observers of the trial felt that the conviction was obtained almost entirely on the basis of his daughter's memories that had lain buried until a sudden awakening of them. Gardner summarizes the thoughts of psychologists and others who are quite concerned about what they feel is false memory syndrome. These critics allege that wellmeaning and sincere therapists begin treating patients with the assumption that a sexual or other trauma had occurred early in the patients' early life, and then these therapists use leading questions to slowly implant memories of events that never really happened. There are, of course, therapists who argue that such repressed memories are real. This is an interesting topic to discuss with students. Ask students to collect examples and also to search for empirical evidence to support repressed memories. Many psychologists doubt that such repression as takes place in these cases is possible. Gardner, M. (1993). “The false memory syndrome.” Skeptical Inquirer, Summer. 86 10. Women and somatization. Women, in general, use health services more than men, even after use related to pregnancy and childbirth is accounted for. Most somatization disorder patients are women. Discuss with the class what they think explains these facts. It may be that traditional sex roles have made it more acceptable for women to admit problems and seek treatment, while for men, being sick violates the strong, sometimes "macho" image assigned to their gender. If so, though, why are there at least as many males as females with hypochondriasis? This topic can provoke a lively class discussion. 11. Reporting bodily symptoms. Ask students whether they feel that they tend to overreport bodily aches and pains as symptoms of illness, often seeking out medical assistance, or tend to underreport them, shrugging them off and going about business as usual. Then, have them relate their tendencies to the following finding. According to Paul Costal and Robert McGraw (American Psychologist, 40, 1985, 19-28), each of us differs in the tendency to label our bodily aches and pains as a symptom of illness. People who habitually complain of unfounded ailments exhibit a cluster of personality traits labeled neuroticism. Those high in neuroticism tend to be anxious, overly self-conscious, hostile, depressed, impulsive, and usually have low self-esteem. In contrast, people who underreport their bodily aches and pains exhibit another cluster of traits labeled extroversion and tend to be warm and outgoing and sufficiently involved in life that they don't have time to complain of their ailments. After you have presented these descriptions, ask students which tendency is dominant in their particular personality and the degree to which it is manifested in under- or overreporting bodily aches and pains. Think About It What is the hypothesized role of anxiety in the dissociative and somatoform disorders? In the early versions of the DSM, the dissociative and somatoform disorders were grouped with the anxiety disorders under the general category of neurosis. The common grouping was based on the psychodynamic model, which holds that various disorders involve maladaptive ways of managing anxiety. In anxiety disorders, the appearance of disturbing levels of anxiety was expressed directly, but the role of anxiety in dissociative and somatoform disorders was inferred rather than expressed in behavior. It was theorized that symptoms mask unconscious sources of anxiety. The DSM now separates the anxiety disorders from the other categories of neurosis--the dissociative and somatoform disorders-- with which they were historically linked. Why is the diagnosis of dissociative identity disorder controversial? Do you believe that people with dissociative identity disorder are merely playing a role they have learned? Why or why not? This is an opinion question. Students should be familiar with the symptoms and features of dissociative identity disorder. Encourage them to 1) maintain a skeptical attitude, 2) consider the definitions of the terms, 3) weigh the assumptions or promises on which arguments are based, 4) bear in mind that correlation is not causation, 5) consider the kinds of evidence on which conclusions are based, 6) do not oversimplify, 7) do not overgeneralize. 87 What is the difference between dissociative amnesia and ordinary forgetfulness? The definition of dissociative amnesia excludes ordinary forgetfulness. Dissociative amnesia is when a person becomes unable to recall important personal information, usually involving traumatic or stressful experiences, in a way that cannot be accounted for by simple forgetfulness. Amnesia is not ordinary forgetfulness, such as forgetting someone’s name or where you left the car keys. Memory loss in amnesia is more profound or wide-ranging. Most cases of dissociative amnesia take the form of localized amnesia in which events occurring during a specific period of time are lost to memory. What role does childhood physical and sexual abuse play in dissociative disorders? The most widely held view of dissociative identity disorders is that it represents a means of coping with and surviving severe, repetitive childhood abuse, generally beginning before the age of 5. The great majority of people with dissociative identity disorder report being physically or sexually abused as children. The severely abused child may retreat into alter personalities as a psychological defense against unbearable abuse. In the face of continued abuse, these alter personalities may become stabilized, making it difficult for the person to maintain a unified personality. What psychological formulations have been proposed to explain the development of dissociative disorders? What do they have in common? To psychodynamic theorists, dissociative disorders involve the massive use of repression, resulting in the “splitting off” from consciousness of unacceptable impulses and painful memories. Learning and cognitive theorists view dissociation as a learned response that involves not thinking about disturbing acts or thoughts in order to avoid feelings of guilt and shame evoked by such experiences. Biological theorists have found evidence that shows differences in brain metabolic activity between people with depersonalization disorder and healthy subjects. The commonality appears to be the recognition that a history of childhood abuse plays a pivotal role. Why is it so difficult to distinguish psychological pain from medical pain? What criteria would you use to determine whether someone has psychological pain associated with pain disorder or medical pain associated with a physical/biological condition? Often, the underlying cause of medical pain is difficult to determine, but this does not mean the pain is purely psychological. The pain one feels, even if physical, can be heightened or lessened by psychological factors, such as one’s style of coping, making the experience of medical pain a psychological phenomenon as well as a physical one. As a result of this diagnostic quandary, many debate whether somatoform pain disorder should be a separate diagnosable psychological condition. Why is conversion disorder considered a treasure trove in the annals of abnormal psychology? What role did the disorder play in the development of psychological models of abnormal behavior? Conversion disorder used to be called hysterical neurosis and, as such, is considered classic in the history of abnormal psychology. It played an important role in the development of Freud’s psychoanalysis. Freud presented several classic cases of conversion disorder including the famous “Anna O.” Hysterical or conversion disorders seem to have been much more common in Freud’s day than they are today, when they are relatively rare. 88 Do you know anyone you would consider to be a “hypochondriac”? What is the basis of your opinion? Did reading the text change your view? This is a personal experience opinion question. Students need to know the symptoms of hypochondriasis and that the main issue in hypochondrias is fear of illness. Does koro or dhat syndrome seem strange to you? How might your feelings depend on the culture in which you were raised? How might behaviors found in your culture be viewed as strange by members of other cultures? This is a personal opinion question. Students should know the symptoms of both koro and dhat as well as the cultural factors that contribute to the manifestation of these disorders, such as the cultural belief in the life-preserving nature of semen contributing to dhat. Similarly, students should know which individual factors make it more or less likely that one will develop either disorder. For example, Guangdong residents who are less superstitious and more highly educated are significantly less likely to develop koro. Why is it so difficult to distinguish malingering from somatoform and dissociative disorders? How might secondary gain contribute to the development or maintenance of these conditions? Those with somatoform and dissociative disorders are often accused of malingering, or faking illness. To date, few methods exist to distinguish the two. Moreover, there may be unseen benefits, or secondary gains, to having such a condition. Imagine the man with pain disorder who does not have to do any housework or heavy lifting as a result – so a real experience of pain is reinforced because the person experiences some benefit from its presence. There are also numerous accounts of World War II soldiers developing “night blindness” that prevented them from going on dangerous nighttime missions. In these cases, how might you go about distinguishing these conditions? Activities/Demonstrations 1. The Dissociative Experiences Scale. Ask students to look over the Dissociative Experiences Scale presented in this chapter and to share their responses. One way to use the scale is to have students go down the list, marking the frequency with which each item occurs, such as "often," "occasionally," or "rarely." Then, determine which types of dissociative experiences occur most often or most rarely. Or you might simply go down the list getting a show of hands for each item. Either way, ask students how they feel when they become aware of such discrepancies in their experience. Do most of them accept such occasional lapses in consciousness as normal? 2. Hypnosis. Have someone skilled in hypnosis conduct a class demonstration to determine how susceptible to hypnosis your students are. You might point out that individuals with multiple personality disorder are quite susceptible to self-hypnosis and are especially likely to dissociate in coping with trauma. However, hypnotic suggestibility has many constructive uses, such as enhancing relaxation, creativity, weight loss programs, and smoking cessation. 89 3. Right-left hemisphere differences. Researchers have found that conversion symptoms are more likely to occur on the left side of the body than the right (leading to the hypothesis that they relate to the functioning of the right hemisphere and emotional arousal). A simple demonstration of the differential functioning of the hemispheres can be done by having students briefly interview one or two people outside of class. The question asked should be a problem, which most college students could accomplish with concentration. For instance: "How many letters are there in the word Washington?" or "Multiply 12 by 13." The interviewer's task is to record the direction of the subject's eye movements when he or she pauses to think about the question. It has been reported that when people concentrate on a reasoning problem, their eyes tend to shift up and to the right. 4. Multiple personality in film. Two of the most famous film examples of multiple personality (now called dissociative identity disorder in the DSM-IV) are Three Faces of Eve and Sybil. These are generally too long to show in class, but it is possible to have students rent the videos of these films and have a get-together where they can view one or the other. They can report to class on the behavior of Eve and Sybil, and how it corresponds to the text discussion. 5. Is multiple personality real? Organize a class debate. Divide the class into pro and con positions. Have your students do a bit of research before the next class. Assign students to read The Case of Billy Milligan or recall an old talk show where “multiples” appeared. Using their “evidence” allow a 20 minute mock debate, presenting and refuting findings. 6. Munchausen Syndrome by Proxy. M. Night Shyamalan’s 1999 film, The Sixth Sense tells the story of a boy who communicates with spirits that either do not know they are dead, or have a message to pass to the living. One of the spirits is a victim of Munchausen Syndrome by Proxy who wants to expose her mother’s abuse in order to save her younger sister. Show the segment of the movie depicting the child’s funeral and the showing of a secret video that shows the mother poisoning her daughter. Ask students to note the mother’s behaviors (such as the red dress she wore at the funeral) that may appear to be odd and/or attention-seeking. This movie also provides an opportunity to discuss important facts associated with this disorder, such as the 6 percent mortality rate for victims. Video Resources Case Study of a Multiple Personality, 30 min. (Penn State). Cleckley's "classic" case study of the three personalities of "Eve," including an interview with the patient herself. Child Abuse, 19 min. color (Films for the Humanities and Sciences). Describes the common characteristics of offenders and the effects of abuse on children. Childhood Sexual Abuse, 26 min. color (Films for the Humanities and Sciences). Shows how adult women learn to work out the problems caused by sexually abusive fathers. Experts explain how the pattern of abuse spreads and is kept secret. 90 Cyrano de Bergerac, this 1990 Metro-Goldwyn-Mayer film depicts Cyrano as a man obsessed with the size of his nose, which he believes is so deformed that it renders him unlovable. This movie can be used to discuss body dysmorphic disorder. Hypochondriasis and Health Care: A Tug of War, 38 min. color (Workshop Films). Lecture and simulated interviews with people with hypochondriasis and ways of dealing with it. Speaking Out Videos in Abnormal Psychology CD-ROM 5 - Henry: Hypochondriasis VIDEO BACKGROUND: In this interview, Henry talks about his health problems, both real and psychologically imagined. He notes that he is hyperaware of his physical health and has possibly seen over seventy doctors since his twenties to help him relieve the worries he has about getting sick and losing physical functionality. Henry discusses how his perceived diseases cause him anxiety and although he studies medical issues, contradictory information makes him confused and distressed about how to be healthy. His strongest concerns are that he is “afraid of being sick” and that his disorder prevents him from enjoying life or being able to talk about other people’s problems without internalizing them. Of particular interest in this interview are the disorders that Henry perceives he has experienced and/or worries about including: asthma, high cholesterol, respiratory problems, colon and lung cancer, heart disease, a heart attack, bloody urine/stool and malaria. DISCUSSION QUESTIONS: 1. People with Hypochondriasis: a) are preoccupied with fears of having serious diseases b) often refuse to accept a clean bill of health from a doctor c) often seek excessive reassurance from physicians d) all of the above Answer: d. Choice A is a partial definition of Hypochondriasis and choices B and C are common behaviors of people with Hypochondriasis. 2. The most important factor of Hypochondriasis that results in a fear of diseases is: a) being told that someone you know is ill b) learning about diseases from medical books c) misinterpreting bodily symptoms d) doing research about a particular disease that is popular in the media Answer: c. Although the other choices may influence Hypochondriasis, a person with Hypochondriasis misinterprets bodily symptoms and feelings, which leads her to believe she is sick. 91 3. Why do people with Hypochondriasis go to doctors frequently? Does this help them? Suggested answers: They go to doctors to relieve the fear they feel about their perceived sickness. Hypochondriasis, however, requires that their preoccupation with the disease continue despite medical evaluations and reassurance. 4. In addition to physical symptoms, what other factors do you think contribute to Hypochondriasis? Suggested answers: the media, knowledge of medicine, friends or family being diagnosed with disorders, etc. 5. How are Hypochondriasis beliefs different from psychotic delusions? Suggested answer: People with Hypochondriasis are able to acknowledge that they may be exaggerating the extent of the feared disease or that there may be no disease at all. CLASS ACTIVITY: 1. People with Hypochondriasis experience numerous problems because of their fears of disease. In addition to anxiety arising from this particular worry, what other problems might people with Hypochondriasis experience? Suggested answers: rejection or belittling by doctors, ridicule by associates, difficulty with work or relationships, etc. 92