Trust health records policy including retention and disposal
advertisement

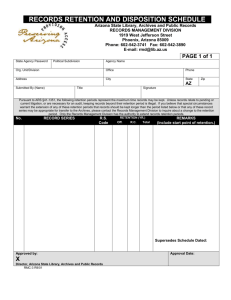
Clinical Records Management Policy Date of Implementation: December 2011 Date of Next Review: December 2014 Version No: 1.1 Approved at: IG Committee Originator: Information Governance Manager Lead Director: Senior Information Risk Owner (SIRO) Contents Page 1 Introduction ....................................................................................................... 4 2 Definitions ......................................................................................................... 4 3 Scope ................................................................................................................. 4 4 Roles and Responsibilities .............................................................................. 5 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 4.10 5 Chief Executive ...................................................................................................... 5 Caldicott Guardian ................................................................................................. 5 Medical Director ..................................................................................................... 5 Medical Records Committee .................................................................................. 5 Head of Performance & Planning ........................................................................... 6 Information Governance Manager / Information Governance Committee ............... 6 Medical Records Manager...................................................................................... 6 Executive/Clinical Directors, General Managers ..................................................... 6 Service Managers, Assistant Service Managers and Departmental Heads ............ 6 All Staff................................................................................................................... 6 Legal Obligations .............................................................................................. 6 5.1 5.2 5.3 6 Data Protection Act (DPA) 1998 ............................................................................. 6 NHS Confidentiality Code of Practice April 2007 .................................................... 7 The Caldicott Principles .......................................................................................... 7 Professional Obligations/Standards ............................................................... 7 6.1 6.2 6.3 7 Professional Obligations ......................................................................................... 7 NHSLA Risk Management Standards for Acute Trusts........................................... 8 NHS Number .......................................................................................................... 8 Unified Medical Record .................................................................................... 9 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 7.10 7.11 7.12 8 Trust Medical Record ............................................................................................. 9 Emergency Department Record ............................................................................. 9 Genito Urinary Medicine (GUM) ........................................................................... 10 Maternity Record .................................................................................................. 10 Nursing Records .................................................................................................. 11 Pathology Records ............................................................................................... 11 Private Patients .................................................................................................... 11 Radiology Records ............................................................................................... 11 Research Records ............................................................................................... 12 Therapies – Occupational Therapy....................................................................... 12 Therapies - Physiotherapy Records ..................................................................... 12 Allied Health Professional Records (AHP) ............................................................ 13 Record Information Quality Assurance ......................................................... 13 9 Record Creation .............................................................................................. 13 9.1 9.2 10 10.1 10.2 10.3 10.4 10.5 10.6 10.7 Clinical Record Creation ....................................................................................... 13 Creation of Temporary Medical Records .............................................................. 14 Record Management ................................................................................... 14 Allergy Recording ................................................................................................. 14 Use of stickers on the front of Trust Medical Records........................................... 15 Special Needs ...................................................................................................... 15 Copying Letters to Patients .................................................................................. 15 Advance Healthcare Decisions ............................................................................. 15 Medical Records Volumes .................................................................................... 15 Maintenance of Medical Records ......................................................................... 16 Clinical Records Policy Page 2 of 29 Review Date: December 2011 11 11.1 11.2 11.3 11.4 11.5 12 12.1 12.2 12.3 12.4 13 13.1 13.2 13.3 14 14.1 14.2 14.3 15 15.1 16 16.1 17 17.1 Records Storage .......................................................................................... 16 Clinical Record Storage........................................................................................ 16 Medical Records Library....................................................................................... 16 Storage of Medical Record outside of Medical Record Library ............................. 16 Storage of Medical Records on the wards ............................................................ 17 Trust Off-site Storage ........................................................................................... 17 Records Tracking / Transportation ............................................................ 17 Tracking Medical Records .................................................................................... 17 Transportation of Clinical Records within the Frimley Park Site ............................ 18 Transportation of Clinical Records off site ............................................................ 18 Removal of a clinical record from the Trust Premises ........................................... 19 Record Disclosure ....................................................................................... 19 Internal Requests for Medical Records Required for Clinical Care ....................... 19 Release of Medical Records to Other NHS Providers........................................... 19 Release of Medical Records to a Third Party........................................................ 20 Records Retention....................................................................................... 20 Clinical Record Retention ..................................................................................... 20 Microfilmed Records............................................................................................. 21 Scanned Records................................................................................................. 21 Records Destruction ................................................................................... 21 Clinical Record Destruction .................................................................................. 21 Record Disposal .......................................................................................... 22 Clinical Record Disposal ...................................................................................... 22 Monitoring of Policy .................................................................................... 22 Medical Records Availability ................................................................................. 22 18 Breaches of policy....................................................................................... 22 19 Training ........................................................................................................ 22 20 Review .......................................................................................................... 23 21 Equality Impact Assessment ...................................................................... 23 Appendix 1 - Clinical Records Retention Schedule ............................................ 23 Clinical Records Retention Schedule .............................................................................. 25 Pharmacy Retention Schedule ........................................................................................ 28 X-Ray Retention Schedule .............................................................................................. 28 Appendix 2 – Trust Clinical Electronic Systems ................................................. 29 Clinical Records Policy Page 3 of 29 Review Date: December 2011 1 Introduction 1.1.1 Records Management is the process by which an organisation manages all the aspects of records whether internally or externally generated and in any format or media type, from their creation, all the way through their lifecycle to their eventual disposal. 1.1.2 The Records Management: NHS Code of Practice has been published by the Department of Health as a guide to the required standards of practice in the management of records for those who work within or under contract to NHS organisations in England. It is based on current legal requirements and professional best practice. 1.1.3 The Trust’s records are its clinical memory, providing evidence of actions and decisions relating to patient care and representing a vital asset to support the treatment of patients. Clinical records support and protect the interests of the Trust and the rights of patients, staff and members of the public. 1.1.4 This policy determines the standards which must be followed when handling and dealing with any Trust Clinical record. 1.1.5 This Clinical Records policy should be read in conjunction with the Trust’s Records Management Strategy and the Trust’s Non-Clinical Records Policy. 2 Definitions 2.1.1 A Record is defined as anything which contains information (in any medium) that has been created or gathered as a result of any aspect of the work of NHS employees, including (but not limited to) bank, agency and locum staff; students; voluntary staff and trainees on temporary placements. 2.1.2 A Clinical Record is defined as ‘any record which consists of information relating to the physical or mental health or condition of an individual and has been made by or on behalf of a health professional in connection with the care of that individual’. 3 Scope 3.1.1 This policy applies to all Trust Clinical records, both manual and computerised including joint health and social care records. 3.1.2 The main principles of this policy are: it relates to all clinical records held in any format by the Trust; it applies to information in paper and other physical forms, e.g. electronic, microfilm, negatives, photographs, audio or video recordings and other assets; Clinical Records Policy Page 4 of 29 Review Date: December 2011 it relates to the 5 distinct phases in the life of information; creation, retention, maintenance, use and disposal; to set out the Trust’s commitment to create, keep and manage clinical records, including electronic records which document the treatment provided to patients. to define a structure for the Trust to ensure adequate clinical records are maintained, managed and controlled and comply with legal, operational and information needs. 3.1.3 Records can be created by anyone working within or on behalf of the Trust. This includes, but is not limited to, employees, agents, contractors and volunteers in any capacity. 3.1.4 This policy sets out a framework within which the staff responsible for managing the Trust’s clinical records can develop specific policies and procedures to ensure that all clinical records are managed and controlled effectively and at best value commensurate with legal, operational and information needs. 4 Roles and Responsibilities 4.1 Chief Executive 4.1.1 The Chief Executive has overall responsibility for records management in the Trust. As accountable officer he is responsible for the management of the Trust and for ensuring appropriate mechanisms are in place to support service delivery and continuity. Records management is key to this as it will ensure appropriate, accurate information is available as required. 4.1.2 The Chief Executive has a particular responsibility for ensuring that the Trust corporately meets its legal responsibilities and for the adoption of internal and external governance requirements. 4.2 4.2.1 4.3 4.3.1 4.4 4.4.1 Caldicott Guardian The Trust’s Caldicott Guardian has a particular responsibility for reflecting patients’ interests regarding the use of patient identifiable information. He is responsible for ensuring patient identifiable information is shared in an appropriate and secure manner. Medical Director The Medical Director has Executive responsibility for the management of Trust Clinical Records. Medical Records Committee Day to day management of the Trust’s medical records is undertaken by the Medical Records committee, which is chaired by a senior clinician. Clinical Records Policy Page 5 of 29 Review Date: December 2011 4.5 4.5.1 4.6 4.6.1 4.7 4.7.1 4.8 4.8.1 4.9 4.9.1 4.10 Head of Performance & Planning The Head of Performance & Planning has the responsibility for the dayto-day management of the Trust’s Medical Records. Information Governance Manager / Information Governance Committee The Trust’s Information Governance Manager/Committee is responsible for ensuring this policy is implemented through the implementation of a Records Management Strategy, and that the records management systems and processes are developed, co-ordinated and monitored. Medical Records Manager The Medical Records Manager is responsible for the overall development and maintenance of the Trust’s medical records management policies and their implementation throughout the Trust, in particular for drawing up guidance for good medical records management practice and promoting compliance with this policy in such a way as to ensure the easy, appropriate and timely retrieval of patient information. Executive/Clinical Directors, General Managers Executive/Clinical Directors and General Managers are responsible for ensuring that departmental policies and procedures relating to the management of their clinical records comply with this Policy and that risks associated with their clinical record usage are managed and controlled. Service Managers, Assistant Service Managers and Departmental Heads Service Managers, Assistant Service Managers and Departmental Heads are responsible for ensuring that staff within their Department receive training on this policy and their own departmental clinical records procedures to ensure clinical records management and associated risks are controlled. All Staff 4.10.1 All Trust staff, whether clinical or administrative, who create, receive and use clinical records have records management responsibilities. In particular, all staff must ensure that they maintain accurate and available clinical records for patients and ensure those records are managed in line with this policy and with any guidance subsequently produced. 5 5.1 5.1.1 Legal Obligations Data Protection Act (DPA) 1998 The Data Protection Act regulates the processing of personal data, held manually and on computer. It applies to all personal information; not Clinical Records Policy Page 6 of 29 Review Date: December 2011 just health records. Personal data is defined as data relating to a living individual that enables him/her to be identified either from that data alone or in conjunction with other information in the data controller’s possession. It therefore includes such items as an individual’s name, address, age, race, religion, gender and physical, mental or sexual health. 5.1.2 The Act contains 3 key strands: 5.1.3 Notification by a data controller to the Information Commissioner Compliance with the 8 data protection principles Observing the rights of data subjects Clinical Records management staff have a key role to play in ensuring that records can be located, retrieved and supplied in a timely manner. 5.2 NHS Confidentiality Code of Practice April 2007 5.2.1 This Code of Practice provides guidance to the NHS and related organisations on the handling of confidential patient information across the NHS. Patient information is held under legal and ethical obligations of confidentiality. Information provided in confidence must not be used or disclosed in a form that might identify a patient without his or her consent. 5.2.2 The Confidentiality Code of Practice describes a Confidentiality Model which has 4 key requirements: 5.3 5.3.1 The Caldicott Principles The 6 Caldicott Principles must be observed when disclosing confidential patient information to any other person either working for the Trust or for another healthcare provider: 6 Justify the purpose Do not use patient identifiable information unless absolutely necessary Use the minimum necessary patient identifiable information Access to patient identifiable information must be on a strict need to know basis Everyone must be aware of their responsibilities Everyone must understand and comply with the law. Professional Obligations/Standards 6.1 6.1.1 Protect – look after the patient’s information Inform – ensure patients are aware of how their information is used Provide Choice – allow patients to decide whether their information can be disclosed or used in particular ways Improve – always look for better ways to protect, inform and provide Choice Professional Obligations All Trust Clinical Records must be a legible record which: Enables the patient to receive effective continuing care Enables the healthcare team to communicate effectively Enables the patient to be identified without risk of error Clinical Records Policy Page 7 of 29 Review Date: December 2011 Facilitates the collection of data for research, education and audit Can be used in legal proceedings 6.1.2 The Trust has comprehensive systems in place for the access, storage, retrieval, usage, retention and destruction of all Trust Clinical records. 6.1.3 Clinical Record keeping standards are monitored through the clinical audit process. 6.2 NHSLA Risk Management Standards for Acute Trusts 6.2.1 This policy must ensure compliance with the NHSLA Risk Management Standards for Acute Trusts. 6.2.2 The original standards of the Clinical Negligence Scheme for Trusts continue to be applied to clinical records management, namely: 6.3 6.3.1 There is a unified medical record which all specialties use Records are bound and stored so that loss of documents and traces are minimised for inpatients and outpatients There are clear instructions in the medical record regarding the filing of documents Operation notes, care pathways and other key procedures are readily identifiable Machine produced medical records are securely stored and use a method that minimises deterioration to ensure availability during the entire retention period Storage arrangements allow retrieval on a 24 hour/7 day basis There is continuous multi-professional clinical audit of record keeping standards, including high risk services There is a mechanism for retaining certain records which must not be destroyed The medical record contains a designated place for the recording of hypersensitivity reactions and other information (e.g. Special Needs) relevant to all healthcare professionals A&E records are contained within the main record for patients who are subsequently admitted There is a system for ensuring that the GP is sent a copy of the A&E record Nursing, medical and other records (e.g. physiotherapy notes, obstetric notes), are filed together or referenced when the patient is discharged There is a system for measuring efficiency in the recovery of records for inpatients and outpatients An author of an entry in a medical record is clearly and easily identifiable NHS Number The NHS number is the unique identifier for all patient records and is a component of NHS CFH. Use of the NHS number will allow linkage of patient records across systems and organisations. It is envisaged that record linkage will improve effectiveness and efficiency of clinical care to patients and support the concept of a lifelong record. The Trust is required to ensure all clinical systems contain the NHS number and each system fully adopts the NHS Number in order to be compliant with the National NHS Number Information Standard. Clinical Records Policy Page 8 of 29 Review Date: December 2011 7 Unified Medical Record 7.1 7.1.1 Trust Medical Record A Trust medical record is created to ensure clinical information relating to a patient is available at the point of need within the Trust. The purpose of a medical record is: 7.1.2 Whilst the Trust aims to operate a unified medical record for patient care, with all specialty records held in a single Trust record, some departments within the Trust create and manage their own clinical record. The clinical records in use across the Trust are: 7.1.3 7.2.1 Medical Emergency Department GUM Maternity Nursing Records Pathology Private Patients Radiology Therapies - Occupational & Physiotherapy The Trust has one medical record which contains the following clinical information: 7.2 To support the care process and continuity of care. To support day-to-day business that underpins delivery of care. To support evidence based practice. To support sound administrative and managerial decision-making. To meet legal requirements, including requests from service users To assist clinical and other audits. To support improvements in clinical effectiveness through research and also to support archival functions by taking account of the historical importance of material and the needs of future research. Admission forms Correspondence Consent forms/ Anaesthetics & Recovery Investigation results ECG Cardiac Ophthalmology Charts- drug sheets – nursing records Therapies – inpatient Physiotherapy – OT Care Pathways CPA/Supervision Register (Psychiatric) Clinic Notes Emergency Department Record When a patient attends the Trust’s Emergency Department a record will be created on the department’s computer system (Symphony) detailing the care and treatment provided to the patient. Clinical Records Policy Page 9 of 29 Review Date: December 2011 7.2.2 On admission of a patient via the Emergency Department a copy of the Emergency Record is filed in the clinical note section of the Trust Medical Record for continuity of care and accompanies the patient to the admitting ward. 7.2.3 Where a patient is not admitted into hospital, a separate emergency record is held by the Trust. 7.2.4 The Emergency Department sends a Discharge Summary of the patient’s attendance to the patient’s General Practitioner (GP) within 24 hours. The Discharge Summary details: attendance date presenting complaint investigations diagnosis treatment and follow-up 7.2.5 Following the implementation of the Symphony system in 2011 the Trust ceased creating manual casualty cards. Old casualty cards are stored at the Trust’s off-site storage facility – CDC - for their defined retention period. 7.2.6 Symphony is fed from the Trust’s Patient Administration System (PAS) – thereby sharing the Trust PMI (Patient Master Index). 7.3 Genito Urinary Medicine (GUM) 7.3.1 When a patient attends the Trust’s GUM clinic a separate record will be created for the patient detailing the treatment provided. 7.3.2 A copy of the record is held in the GUM department and is not merged into the Trust’s Medical Record. A unique number is allocated to patients which is not obtained from the Trust’s PAS. 7.3.3 The GUM Records are stored within the GUM department for their defined retention period. 7.4 Maternity Record 7.4.1 Maternity patients have hand-held ante-natal records for the duration of their pregnancy. Maternity records are contained in a single booklet comprising ante-natal, labour and post-natal records. Investigation results will be filed onto the maternity mount sheet in the handheld record. 7.4.2 During the patient’s pregnancy the Trust’s medical record is held in the Ante-natal Department and is available at all consultations. Cardiotocograph (CTG) results are filed into the standard brown re- Clinical Records Policy Page 10 of 29 Review Date: December 2011 sealable envelope available in the Obstetric Department. At the end of the Patient’s pregnancy their ante-natal records will be amalgamated into the main medical record. 7.5 Nursing Records 7.5.1 Nursing records form part of the main medical record and are filed within the main medical record. Whilst a patient is an in-patient, nursing records will be held at the bedside for reference and recording purposes. On patient transfer, nursing records will be securely transported together with the main medical record so that these are easily re-utilised by the receiving ward. 7.5.2 When a patient transfer is planned, observation charts, fluid balance charts (not currently required as part of on-going clinical management) and investigation results will be secured within the main medical record. 7.6 7.6.1 7.7 7.7.1 7.8 Pathology Records Request forms for patients are held in the pathology department detailing the tests requested for each patient. Private Patients When a patient attends the Trust’s private patient suite the main medical record will be used to record a summary of treatment provided to the patient. More detailed information relating to the patient’s care and treatment is held by the consultant in his private patient records/files. Radiology Records 7.8.1 Radiology records are managed and stored by the Trust’s radiology department. 7.8.2 The Trust implemented Agfa Picture Archiving Computer System (PACS) in 2004. PACS is linked to the Radiology Information System (RIS) which is fed from the Trust’s Patient Administration System (PAS) – thereby sharing the Trust PMI. 7.8.3 PACS images are distributed across the Trust wide network and displayed using a web browser. 7.8.4 Radiology Reports are stored on RIS and are also available as additional information in PACS. Information from RIS such as requests, appointments and verified Radiology reports are sent to PAS. Radiology reports appear on the web browser once they are validated (checked) by the author. 7.8.5 Radiology reports are also distributed in paper copy to all referrers including GP’s. Clinical Records Policy Page 11 of 29 Review Date: December 2011 7.8.6 Following the implementation of the PACS system in 2004 the Trust ceased creating manual x-ray films. There are no manual x-rays films stored in the Trust. Old X-ray films are stored at the Trust’s off-site storage facility – Overs - for their defined retention period - 3yrs plus current year except paediatric images that are kept until the patient is 21. Images that have 'do not destroy' stickers that are kept indefinitely. 7.8.7 Following the implementation of electronic mammograms images in August 2007, the Trust ceased creating manual mammograms. There are no manual mammograms stored in the Trust. Old mammogram films are stored at the Trust’s off-site storage facility – Overs - for their defined retention period. Mammograms are stored for five years and when the patient re-attends the 5 year clock begins again. 7.9 Research Records Where a patient has consented to participate in a clinical trial/research project, a separate file for the patient will be created and stored by the Principal investigator. 7.9.2 A note is placed in the patient’s medical record indicating the patient is part of a research project. All medical records belonging to patients enrolled into clinical trials prospectively will be labelled and contain a section for the storage of clinical information relevant to patient’s trial involvement. 7.9.1 7.10 Therapies – Occupational Therapy 7.10.1 When a patient is treated by Occupational Therapy staff a separate electronic clinical record is created for them. Following the implementation of the Tiara system in 2009 the Trust ceased creating manual Occupational Therapy records. Only child Occupational Therapy records are stored on site. Adult Occupational Therapy Records are stored at the Trust’s off-site storage facility – CDC - for their defined retention period. 7.10.2 Tiara is fed from the Trust’s Patient Administration System (PAS) – thereby sharing the Trust PMI. 7.11 Therapies - Physiotherapy Records 7.11.1 When a patient is treated by the Physiotherapy department, an outpatient physiotherapy referral card is created for them. Clinical information relating to their outpatient treatment is recorded on the physiotherapy card. Physiotherapy treatment provided to an inpatient is recorded in the patient’s medical record. 7.11.2 Once the patient has been discharged from the department, the outpatient physiotherapy card is stored for a short period of time within the Physiotherapy department before being transferred off site to the Trust’s off-site storage facility – CDC - for their defined retention period. Clinical Records Policy Page 12 of 29 Review Date: December 2011 7.11.3 Tiara is fed from the Trust’s Patient Administration System (PAS) – thereby sharing the Trust PMI – patient master index. 7.12 Allied Health Professional Records (AHP) 7.12.1 Allied Health Professionals write directly into the main medical record for inpatient and some Outpatient consultations. Any other documentation is filed within the Medical Record on discharge. 7.12.2 Where an AHP has undertaken an assessment in the patient’s home whilst the patient is an inpatient, this documentation is filed within the main medical record. If care continues on an outpatient basis, regular reports must be made and filed in the medical record, particularly if there is a change of treatment or on discharge. Reports are addressed to consultants (or other relevant clinical staff) and are filed in the medical record by Directorate clerical staff. 8 Record Information Quality Assurance 8.1.1 Good quality information stored in clinical records enable staff to undertake their roles and responsibilities effectively as well as provide authentication of the records so that the evidence derived from them is shown to be credible and authoritative. 8.1.2 When managing its clinical records, the Trust must ensure that the clinical record being created is of high quality. All Clinical records must: 9 9.1 9.1.1 Be factual, consistent and accurate Be written in black ink Be written as soon as possible after an event has occurred, providing current information on the care and condition of the service user Be written clearly, legibly and in such a manner that they cannot be erased Have errors corrected by a single line and any such corrections signed and dated by the person making the amendment. Erasers, liquid paper, or any other obliterating agents should not be used Be accurately dated, timed and signed with the signature being printed alongside the first entry Contain as few abbreviations or jargon as possible Be consecutive Be bound and stored in accordance with Trust’s procedures ensuring that the likelihood of loss of documentation is minimised Record Creation Clinical Record Creation Records of all clinical treatment provided to a patient must be recorded within the patient’s medical record or the applicable electronic clinical system (see appendix 2 for the list of the Trust’s Clinical systems) to enable members of staff and their successors to continue the care and treatment of a patient. Clinical Records Policy Page 13 of 29 Review Date: December 2011 9.1.2 A number of departments are able to create new Medical Records for each new patient e.g. Emergency Department, Parkside. The Trust’s medical records are pre-printed with Trust hospital numbers. Upon creation of a new patient record the hospital number is entered into the PAS. At the point of creating a medical record a year sticker is placed on the side of the medical record folder to assist with the destruction/retention of the record. 9.1.3 Where a patient record has been stored off site for longer than 5 years and the patient re-attends the Hospital, the patient’s old medical folder will be recalled from the Trust’s off-site storage and a new record created for the patient with a new hospital number. 9.1.4 Where a clinical department creates a record for a patient they must ensure this record can be linked to the patient’s main medical record. Each clinical record department must develop and maintain procedures relating to the creation of their clinical records. 9.1.5 At the point of creating a clinical record consideration must be given to the lifecycle of the record and its ultimate destruction, particularly where the record is in electronic format. 9.2 Creation of Temporary Medical Records 9.2.1 If a patient’s medical record cannot be located, a temporary record will be created for the patient. A set of temporary medical records is only created with approval from the Medical Records Manager or their deputy. 9.2.2 The temporary medical record for a patient has a red cover. The Medical Records department will monitor all temporary medical records to search and locate the original medical record. 9.2.3 Where the original medical record has not been found within 2 years of the temporary medical record being created, the temporary medical record will become the patient’s main health record. 9.2.4 The Medical Record Department manages and maintains a missing record log. 9.2.5 When temporary medical records are created this is indicated in the Loan Comment field on the Trust PAS. 10 Record Management 10.1 Allergy Recording Clinical Records Policy Page 14 of 29 Review Date: December 2011 10.1.1 Allergies & Adverse Drug Reaction form part of the inside cover in the medical records from 2006. Medical Records prior to 2006 must have the documentation placed on front inside cover in all instances. 10.1.2 Allergies must be recorded on the inside front cover sheet. This instruction is printed in the front of new medical records from 2006. Prior to 2006, details were recorded on the “Patient Alert” sheet in the front of the medical record. 10.2 Use of stickers on the front of Trust Medical Records 10.2.1 Following approval of the Trust’s Caldicott Guardian, stickers may be placed on the front of the Trust’s medical records. The following stickers have been approved to be placed on the front of a medical record: 10.3 Year sticker – indicating the year the patient was treated in the Trust to facilitate the retention of the record Butterfly sticker – indicating the patient has dementia Special needs – Identify the patient has additional care requirements Special Needs 10.3.1 Where a patient has a special need (e.g. interpreter, large print, wheelchair) this must be recorded on the front sheet of the medical records and a ‘special needs’ sticker placed on the front of the medical record. The Trust PAS maintains a Special Needs Register which staff must ensure is kept up to date. 10.4 Copying Letters to Patients 10.4.1 Patients will receive a copy of the letters sent to their GP and other consultants relating to their care. 10.4.2 If the patient does not want to receive a copy of these letters this will be recorded on the PAS in the “Medisec” section of the PAS. This allows Medical Secretaries to see whether a copy of the letter needs to be sent to the patient. 10.4.3 Results letters are generally not transmitted to patients as these may contain information not discussed at consultation. 10.5 Advance Healthcare Decisions 10.5.1 Advance Healthcare Decisions (Living Wills) must be flagged on the front sheet of the medical records from 2007. The Advance Decisions must be filed behind the Patient Administration Sheet. Advance decisions can be flagged in older records by the use of the stickers available from Medical Records. 10.6 Medical Records Volumes Clinical Records Policy Page 15 of 29 Review Date: December 2011 10.6.1 Where a medical record becomes too large for easy day to day use, a second medical record for the patient will be created. The latest volume will be used when the patient attends the hospital unless specifically requested by the treating clinician. 10.7 Maintenance of Medical Records 10.7.1 The maintenance of the Trust’s medical records is the responsibility of all staff who make use of the record. This includes the correct filing of all loose paperwork relating to the patients care and the volumising of a record should it exceed the required size of 4cm.. 11 11.1 Records Storage Clinical Record Storage 11.1.1 All systems used to store Clinical records will ensure the information is kept safe and secure from unauthorised access whilst allowing maximum accessibility to the information commensurate with its frequency of use. 11.1.2 All manual Clinical records will be kept in a secure environment and access will be restricted to authorised personnel only. 11.2 Medical Records Library 11.2.1 A Patient’s medical record contains the majority of the clinical records created by the Trust. This record is stored in the Trust’s Medical Records library. 11.2.2 The Trust operates a closed library system, operated only by designated staff, who are authorised to file and retrieve medical records. Restricted access to the library ensures confidentiality and security measures are in place and improves medical record availability. 11.2.3 Any member of staff requesting a medical record must be an authorised Trust employee. Records requested on an urgent or routine basis will be made available within agreed time limits, urgent requests being acted upon immediately. 11.2.4 The Medical Record Library is open 24 hours per day 7 days per week, including Bank Holidays, to support emergency retrievals, requests and returns of the Trust’s medical records. 11.2.5 The Medical Records procedure manual details the process Medical Records staff follow when retrieving Medical Records for staff from the Trust’s Medical Record’s library. 11.3 Storage of Medical Record outside of Medical Record Library Clinical Records Policy Page 16 of 29 Review Date: December 2011 11.3.1 Where a Clinical record is stored outside of the Trust’s medical record library the records must be stored in a logical order to enable quick and easy retrieval of the medical record e.g. organised by date of clinic, numerically, etc. 11.3.2 Medical Records must always be kept secure when left unattended to prevent unauthorised access to the medical record e.g. stored in a locked cupboard/room. 11.3.3 Where a medical record is not located in Trust’s medical record library, the Emergency Department are able to retrieve the medical record from the location in the hospital that they are tracked to. Master keys for offices are available via the switchboard. 11.4 Storage of Medical Records on the wards 11.4.1 Medical Records will be stored on the ward either in a medical record trolley behind the Ward desk, or for surgical patients at the end of the patient’s bed with their nursing notes. 11.5 Trust Off-site Storage 11.5.1 When discharged from the Trust the patient’s medical record will be stored in the Medical Records library for 2 years before being sent to the Trust’s off-site storage facility for their defined retention period. 11.5.2 The Trust’s off-site storage facility – CDC - is used to stored inactive clinical records (Pharmacy, Occupational Therapy, Physiotherapy, Emergency Department). Each department is responsible for ensuring clinical records are stored in line with the Trust Off Site Storage Procedures. 11.5.3 It is the responsibility of the off-site storage company to ensure that security and confidentiality of all Trust clinical records and their operational procedures are compliant with Principle 7 of the Data Protection Act 1998. 11.5.4 Access to the clinical records will be restricted to personnel employed by the off-site storage company. The clinical records will only be accessed when a request is made for the record to be returned to the Trust. This is done through either the Medical Records Department or the Information Governance Department. 11.5.5 At no time will a clinical record be opened or read by any member of staff employed by the off-site company. 12 12.1 Records Tracking / Transportation Tracking Medical Records Clinical Records Policy Page 17 of 29 Review Date: December 2011 12.1.1 The Trust’s medical records are registered on the PAS. All record transactions (i.e. movements) relating to a Trust medical records must be recorded on the PAS within the “Casenote Tracking module”. 12.1.2 When a Medical Record leaves the Trust’s medical record library it must be tracked to the location it is being moved to. Tracking the medical records electronically records the movement of the medical record. 12.1.3 All movements of a medical record must be tracked on the PAS as soon as possible and certainly within 15 minutes of the movement. The history of previous medical record movements will be kept for the last six movements. 12.1.4 When a record is moved it is the responsibility of the person in the current location to track the record to its new location. 12.2 Transportation of Clinical Records within the Frimley Park Site 12.2.1 Medical Records being transported must be placed in sealed and accurately addressed envelopes, marked Private & Confidential and stating the name of the person to whom they are being sent (i.e. it is insufficient to simply address them to a department or building). 12.2.2 When a patient is being transferred within the Hospital building from department to department by a Trust member of staff (e.g. a porter) the member of staff must carry the medical record. 12.2.3 When a patient is not escorted by a Trust member of staff the patient could be asked to carry their medical records, providing they are in a sealed envelope that is fully addressed to the department/ward the patient is due to visit/attend. 12.2.4 Medical records must not be left unattended at any time (e.g. when awaiting portering services). 12.3 Transportation of Clinical Records off site 12.3.1 Where medical records need to be transferred to another location to support the Trust services (e.g. For outpatient appointments at off-site clinics - Farnham, Fleet, Aldershot Centre For Health, Bracknell, Skipton Hill, etc.), the transportation of medical records be must be undertaken by Trust transport in sealed envelopes or, in the case of bulk returns, in sealed bags/boxes. 12.3.2 Where medical records are being transferred to the Trust’s off-site storage facility it is the responsibility of the off-site storage company to ensure all records are securely transferred in full compliance with the Data Protection Act 1998. Clinical Records Policy Page 18 of 29 Review Date: December 2011 12.3.3 Only where staff need to treat a patient outside of Trust premises (e.g. at home, nursing home, provision of community services etc.), the member of staff is permitted to transfer the patient’s medical record. 12.3.4 When staff are transporting a medical records they must ensure all records are kept secure during transit (e.g. in the boot of a car and not on a seat) and are not left in a car unattended overnight. 12.3.5 All medical records must be returned to the hospital as soon as possible. 12.4 Removal of a clinical record from the Trust Premises 12.4.1 The Trust’s Medical record must not be removed from the Trust premises by individual members of staff unless for approved business use (i.e. outpatient appointment at an off-site location, care and treatment of patient in the community, at their home). 12.4.2 Where staff have a need to take a medical record off site for a reason other than those detailed above, they must obtain approval of the Trust’s Medical records Manager or Deputy. 13 13.1 Record Disclosure Internal Requests for Medical Records Required for Clinical Care 13.1.1 Internal requests for medical records from Trust staff must only be for the purpose of clinical care. Requesters are required to state the purpose for the loan of the record and Library staff will check this on receipt. 13.1.2 Where a medical record needs to be accessed for the Trust’s healthcare purposes (i.e. research, audit, complaints, litigation) records must be requested following the appropriate Trust procedures. 13.2 Release of Medical Records to Other NHS Providers 13.2.1 On receipt of a request to release records to another hospital, patient consent must be obtained. 13.2.2 It is essential that all requests to release medical records are obtained in writing. 13.2.3 Requests from GP surgeries for results or discharge documentation must be directed to the department that initiated the requested information. 13.2.4 Only photocopies of the medical record can be released to another NHS Provider, allowing retention of the original medical record by the Trust. Clinical Records Policy Page 19 of 29 Review Date: December 2011 Any exceptions to this procedure must be agreed with the Medical Records Manager. 13.2.5 Any release of a medical record must be recorded within the casenote tracking module on the PAS by the person responsible for sending the medical record to the requested location/person. 13.3 Release of Medical Records to a Third Party 13.3.1 Where the Trust receives a request for patient information from a Third Party (e.g. benefits office, police, insurance company, solicitor) it will only be disclosed where the patient has consented to the release of their information. 13.3.2 The release of patient information to third parties will be managed in full compliance with the Data Protection Act 1998, Common Law Duty of Confidentiality and Access to Health Records Act 1990. 14 14.1 Records Retention Clinical Record Retention 14.1.1 All Clinical records must be retained for defined periods. This retention period is calculated from the end of the calendar year following the last entry in the record (e.g. manual file, computer record). 14.1.2 The Trust has adopted the retention periods set out in the Department of Health Records Management: NHS Code of Practice. Appendix 1 of this policy details the retention periods for all Trust clinical records. 14.1.3 Where a record type is not listed the Trust’s clinical managers will carry out a risk assessment to decide how long the record is required to be kept for. Attention will be paid to other retention periods for similar record types combined with the risks and benefits of destroying or maintaining the records for a prolonged period of time. 14.1.4 Once a retention period has been decided for a clinical record, this will be approved by the Trust’s IG committee and incorporated within the retention schedule detailed in Appendix 1 of this policy. 14.1.5 The retention schedule details the minimum retention period for each type of clinical record. Clinical records (whatever the media) may be retained for longer than the minimum period, however generally records should not be retained for more than 30 years in accordance with the Public Records Act 1958. 14.1.6 The Trust will develop procedures detailing how the Trust undertakes an appraisal of its records. The appraisal process determines whether records are worthy of permanent archival preservation. Clinical Records Policy Page 20 of 29 Review Date: December 2011 14.1.7 The Trust would undertake the appraisal process in conjunction with the local approved Place of Deposit. This normally applies to a record where a retention period in excess of 30 years is required (e.g. to be preserved for historical purposes), or for any pre-1948 records. In these cases, the National Archives will be consulted. 14.2 Microfilmed Records 14.2.1 Microfich is a permissible storage medium acceptable to the courts. Microfilming standards were quality assured to ensure reconstruction of the microfilmed record is possible. 14.2.2 The Trust’s Medical Record Department mircofiched inactive medical records from 1992/3 until 2006. A register of all microfiched records is held on a secure departmental database within the Medical Records Library. 14.3 Scanned Records 14.3.1 The GUM department has scanned their clinical records to CD to maintain the record for the required retention period, enabling the manual records to be destroyed and providing much needed physical storage for the active clinical record. 15 15.1 Records Destruction Clinical Record Destruction 15.1.1 Clinical records (including copies) not selected for archival preservation and which have reached the end of their life will be destroyed in a secure manner. This will be undertaken either on site or by the Trust’s off-site storage company. 15.1.2 In exceptional circumstances clinical records may require permanent preservation – the clinician who is seeking to retain a record must gain approval for permanent preservation from the Medical Director and, if possible, consent from the Data Subject. 15.1.3 If the Caldicott Guardian is in agreement, the clinician must document clearly the reason for permanent preservation clearly within the medical record. Medical Records required for permanent preservation must be clearly marked “FOR PERMANENT PRESERVATION” on the outside front cover. 15.1.4 The destruction of records is an irreversible act. The normal destruction method used by the Trust is shredding. 15.1.5 All removable magnetic or optical media containing clinical information must be returned to the IT department for safe disposal. In addition, Clinical Records Policy Page 21 of 29 Review Date: December 2011 any IT equipment scheduled for disposal which contains non-removable storage devices such as hard disk drives, must also be returned to the IT department. 15.1.6 The hard disk must be formatted or rendered inoperable (e.g. physically destroyed) and stored securely awaiting disposal by the same means as removable media. In order to dispose of magnetic media, a secure bonded media disposal facility must be employed and a full audit trail of tapes and disks disposed should be maintained by the Informatics Department. 16 Record Disposal 16.1 Clinical Record Disposal 16.1.1 All clinical records must be disposed of in line with the Trust’s Confidential Waste Procedures. 17 Monitoring of Policy 17.1 Medical Records Availability 17.1.1 The following standards for Medical Record Availability have been agreed: Outpatient Clinic - 98% of medical record must be available at the start of the clinic Elective Admission -100% of medical records must be available on the ward at the time of admission 17.1.2 Audits on the management of the Trust’s medical records are undertaken by medical records staff on a regular basis including: A Monthly snapshot of random areas showing compliance of tracking records. To cover a selection of areas within the Trust including inpatient, outpatient and non patient care areas. 17.1.3 Additional audits will be undertaken by the Medical Records department as and when required to demonstrate compliance with this policy and the Medical Records Procedure Manual. 17.1.4 Results of these audits will be reported to the Trust’s Medical Records Committee and to the Trust Board through the SIRO report every 6 months. 18 Breaches of policy 18.1.1 Where it is identified a member of staff is not adhering to the guidelines set out in this policy, the Trust reserves the right to take disciplinary action. 19 Training Clinical Records Policy Page 22 of 29 Review Date: December 2011 19.1.1 Staff awareness of their individual responsibilities for the maintenance and protection of the clinical records that they create, use or manage will be raised through the Trust’s induction programme, team meetings, Trust Briefings and other avenues as appropriate. 19.1.2 The training needs of staff in relation to clinical records management will be identified so that training can be updated and reinforced as necessary. 19.1.3 Managers will be responsible for ensuring that all their staff are aware of the Trust’s Clinical Records Management Policy. 19.1.4 The Trust will provide general Records Management training as part of its annual Information Governance Training. 19.1.5 All Trust staff will be made aware of their responsibilities for record- keeping and record management through generic and specific training programmes and guidance. 20 Review 20.1.1 This policy will be reviewed every three years (or sooner if new legislation, codes of practice or national standards are introduced). 21 Equality Impact Assessment 21.1.1 The users of this policy will take into account their statutory duty to promote equality and human rights and to act lawfully within current equality legislation and guidance. 21.1.2 This policy has been equality impact assessed and has been shown to have no adverse impact on any equality group. 21.1.3 The Trust will continue to monitor its effect and will assess again if negative impact is identified or at the review date. Appendix 1 - Clinical Records Retention Schedule 21.1.4 The coding within the schedules denotes the status of the type of record and its retention period: Note 1 = Where an organisation has an existing relationship with an approved Place of Deposit, it should consult the Place of Deposit in the first instance. Where there is no pre-existing relationship with a Place of Deposit, organisations should consult The National Archives. Note 2 = a previously existing record type (i.e. referenced in the previous retention schedule dated March 2006) but where there has been a change to the retention period following release of the updated Department of health Records Management Code of Practice 2008. Clinical Records Policy Page 23 of 29 Review Date: December 2011 Clinical Records Policy Page 24 of 29 Review Date: December 2011 Clinical Records Retention Schedule Minimum Retention Period Notes From date of attendance relating to the following specialities: Emergency Department Audiology Dental Endoscopy Ophthalmology Intensive Care Charts Oncology/Cancer Medical Illustrations Microfiche/Microfilm Occupational Therapy Sexual Health Records Physiotherapy Podiatry Ultrasound Final Action Adult Record 8 years Child Record Retain until the patient’s 25th birthday or 26th if young person was 17 at conclusion of treatment, or 8 years after death. Admission Books 8 years From last entry Note 1 Angiography tapes and disks 8 years From last date of treatment Destroy Audio tapes of calls 3 years All relevant clinical information has been transferred to Trust Medical Record Destroy Audit Trails (electronic records) Until further notice Birth Registers 2 years Birth Notification Retain until the patient’s 25th birthday. Blood Transfusion 30 years From date of transfusion Destroy Breast Screening (Mammography) 9 years After date of final attendance/death Destroy Mammography – Screen detected cancers, interval cancers, interesting cases Indefinitely Destroy Cervical Screening slides 10 years Destroy Chaplaincy records 2 years Note 1 Clinical Records Policy Page 25 of 29 Review Date: December 2011 Destroy Destroy Destroy Lists are sent to General Register Office. Note 1 Destroy Clinical Records Retention Schedule Minimum Retention Period Notes Final Action Clinical audit records 5 years Clinical Trials (including Pharmacy records) 5 years Clinical psychology 20 years Note 2 Contraception records 8 years (in adults) or until 25th birthday in a child (age 26 if entry made when young person was 17) Destroy Counseling Records 20 years, 8 years after patient’s death Note 2 Creutzfeldt‐Jakob Disease 30 years from date of diagnosis, including deceased patients Note 2 Death Certificates/ Registers 2 years Destroy Deceased Records 8 years Except: CJD and transfusion. Diaries 2 years After end of year to which the diary relates. Patient specific information must be transferred to medical record. Destroy Discharge Books 8 years After the last entry date Note 1 Did Not Attend 2 years After decision is made Destroy Donor Records 30 years From date of post operation Note 1 Duplicate Records 2 years After decision to merge or unmerge Destroy Electrocardiogram (ECG) Records 7 years Genetic Records 30 years From last date of attendance Note 1 GUM Adult Records 10 years From last entry Destroy GUM Child Records (under 18) 8 years (in adults) or until 25th birthday in a child (age 26 if entry made when young person was 17). Destroy Infection Control Records 6 years Destroy Joint Replacement Records 10 years Note 1 Clinical Records Policy Page 26 of 29 Review Date: December 2011 Destroy From closure of trial Destroy Note Destroy Clinical Records Retention Schedule Minimum Retention Period Notes Mental Health Record 20 years Mortuary registers 10 years Note 1 Notifiable Diseases 6 years Destroy Operating Theatre Lists 4 years Destroy Operating Theatre Registers 8 years Note 1 Oncology Records 30 years Note 1 Outpatient Lists 2 years Pathology Records 10 years Post Mortem Records 30 years Referral Letters 2 years Destroy Refrigeration and freezer charts 11 years Destroy Research Records 5 years Smoking Cessation 2 years Clinical Records Policy Page 27 of 29 Review Date: December 2011 From last contact, or 8 years after death Final Action After the year they relate Destroy Destroy Destroy Approval sought from Coroner to file in the medical records After conclusion of trial Destroy Destroy Destroy Pharmacy Retention Schedule Minimum Retention Period Requisitions 2 years Registers and CDRBs Extemporaneous preparation worksheets Aseptic worksheets (adult) 2 years Notes From last entry Final Action Destroy Destroy 13 years Destroy 13 years Destroy Aseptic worksheets (Paediatric) 26 years Destroy External orders and delivery notes 2 years Destroy Prescriptions (inpatients) 2 years Destroy Prescriptions (outpatients) 2 years Destroy Destruction of CDs 7 years Destroy Ward Pharmacy Requests/Books 1 year Destroy X-Ray Retention Schedule Minimum Retention Period Notes Final Action Adult 8 years Destroy Children 25 years Until the child’s 25th Birthday Destroy Maternity 25 years After birth of child Destroy Clinical Trials 15 years After completion of treatment Destroy Litigation 10 years After file is closed Destroy Mental Health 30 years Destroy Oncology Clinical Records Policy Retain Page 28 of 29 Review Date: December 2011 Appendix 2 – Trust Clinical Electronic Systems Daryl Gasson Information Helen Coe Medicine, Eldery, Outpatients and Ian Fry Diagnostic and Therapy Services Paul Bostock Chris Ball Surgical Services Womens & Children Information Infocom Reporting system Cardiology Prismnet Anticoagulant RAID Audiology AuditBase Childrens Centre Information Ardentia Data Warehouse Cardiology XIMS Anticoagulant Coaguchek XS plus Cancer Department Somerset Maternity Information CHKS Live (Signpost) Cardiology Medcon Microbiology Kiestra Cancer Department/Re search IBIS-II Maternity Diabetic Clinic Diabeta3 Pathology Sunquest ICE Critical Care (ICU) Ward Watcher Pathology Pathology DART MSoft Endoscopy Endoscopy Pathology Infection Control Endoscopy Mirocam Prescription Pharmacy Tracker System Pathology B-Plan Activity Based Costing Software Ophthalmology Medisoft A&E/MAU Medex Pathology Radiance Ophthalmology Point of Care A&E Sympthony Pathology QCM3 Point of Care Sterile Services (HSDU) SSDMan ?? IBS Pathology Medifact Cytology Results to PCA ENT EncorePro2 PTS Online Services Cleric Surgery Orthoview Radiology PACS Theatres CareSuite Radiology Bbrad Urology Urodynamics Radiology RIS Urology Ezzee Peezee PAS (Clinicom)/Pa Trust-wide tient Centre GP Browser 4 GUM Lilie System Pharmacy JAC Medicines Pharmacy Information Databank Clinical Novacor Investigaton RTSoft s Clinical Hypertensio Investigaton n s Clinical Multiple Investigaton Sclerosis s Clinical Breeze Investigaton Database s 15 Pathology Therapies Clinical Records Policy Winpath/ Ophthalmology Ward Enquiry Tiara Pathology TPath Radiology RIS Archive Radiology Radiology NightHawk CT Scanners 21 Page 29 of 29 Anaesethics 3di Mike McSweene Finance and Contracting IT Euroking/C TG Monitoring K2 Fetal Monitoring Training System EDTS 1 Maternity Colposcopy Unisoft Neo-Natal Trackerscope Neo-Natal Viewpoint SEND Neo-Natal Massinimo 7 Humphrey Visual Field Analyser Optos RotaTrack 17 Review Date: December 2011 Total Number of Systems 65