biochem 24 [4-20
advertisement

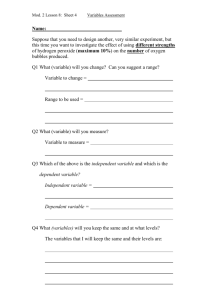
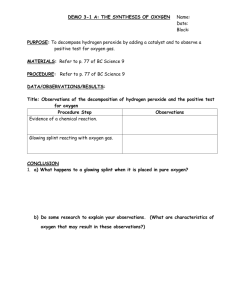
Biochem Chapter 24: Oxygen Toxicity and Free Radical Injury Generating reactive oxygen species (ROS) from oxygen in our cells is a natural everyday occurrence - ROS are formed as accidental products of both enzymatic and nonenzymatic rxns Radical – molecule that has a single unpaired electron in an orbital Free radical – radical that is capable of independent existence - Radicals formed in an enzyme active site during a rxn are not free radicals, unless they can dissociate from the protein to interact with other molecules Radicals are very reactive, and initiate chain rxns by removing an electron from a molecule to complete its own orbital Transition metals like iron, copper, and molybdenum, all have single electrons in orbitals, but they aren’t free radicals because they’re pretty stable, don’t initiate chain rxns, & are bound to proteins in the cell Oxygen is a biradical molecule, which means it has 2 single electrons in different orbitals - - - These electrons can’t both be in the same orbital, because they sp.in in the same direction (parallel spins) o Because of the parallel spins, the 2 unpaired electrons in oxygen are called antibonding electrons o Unlike oxygen, carbon-bonds with either another carbon or a hydrogen, have 2 electrons with antiparallel spins, that form a thermodynamically stable pair o So oxygen can’t oxidize a covalent bond well, because one of its electrons would need to reverse its spin to do so o The difficulty in changing spins is called spin restriction o Spin restriction makes it so that humans and other stuff with carbon in them don’t just get oxidized by oxygen in the air Oxygen is very reactive in thermodynamics, but its single electrons can’t react rapidly with the paired electrons in the covalent bonds of organic molecules So oxygen reacts slowly through the acceptance of single electrons in rxns that need a catalyst, like a metal-containing enzyme Oxygen can accept at most 4 electrons, leading to oxygen being reduced into water When oxygen accepts one electron, it forms superoxide (O2-) o Superoxide is a radical with just one unpaired electron (unlike oxygen’s 2 unpaired e-), so one of oxygen’s unpaired paired with the electron you added o The rxn to make superoxide isn’t thermodynamically favorable, and needs a strong reducing agent that can donate single electrons (like the radical form of coenzyme Q (CoQH●) in the electron transport chain) When superoxide accepts an electron, it is reduced to hydrogen peroxide (H2O2), which isn’t a radical - When hydrogen peroxide accepts an electron, it’s reduced into the hydroxyl radical (OH●) When one more electron is accepted by hydroxyl radical, you complete converting oxygen into water – page 439 steps for converting oxygenwater Reactive oxygen species – oxygen-containing stuff that are highly reactive free radicals, or things readily converted into oxygen free radicals in the cell The major oxygen metabolites made from one-electron reduction of oxygen are classified as ROS - The major oxygen metabolites into free radicals are superoxide, hydrogen peroxide, and the hydroxyl radical Reactive free radicals extract electrons, usually as hydrogen atoms, from other compounds to complete their own orbitals, which initiates free radical chain rxns Hydroxyl is the most potent ROS - Hydroxyl initiates chain rxns that form lipid peroxides and organic radicals Superoxide anion is also highly reactive, but is has limited lipid solubility, so it can’t diffuse far - Superoxide can generate the more reactive hydroxyl and hydroperoxy radicals by reacting with hydrogen peroxide in the Haber-Weiss rxn (page 440) o Superoxide + hydrogen peroxide oxygen + water + hydroxyl radical Hydrogen peroxide is not actually a radical - - - It’s a weak oxidizing agent that is classified as a ROS because it can generate the hydroxyl radical Hydrogen peroxidehydroxyl, is catalyzed by transition metals like iron or copper in the Fenton rxn (page 440) o Hydrogen peroxide –(ferrous ironferric iron) hydroxide (OH) + hydroxyl radical (OH●) o To decrease how often the fenton rxn happens in the body, a cells ability to take in iron and copper is very restricted o Events that release iron from cell storage sites, like a crushing injury, can increase free radical injury, due to the Fenton rxn Since hydrogen peroxide is lipid soluble, it can diffuse through membranes and generate hydroxyl at places with ferrous iron or copper, like at the electron transport chain in mitochondria Hydrogen peroxide is also the precursor of hypochlorous acid (HOCl), which is an oxidant made by phagocytes in the respiratory burst Organic radicals are generated when superoxide or hydroxyl radical extract electrons from organic molecules - Organic peroxy radicals are intermediates of chain rxns, like lipid peroxidation Ethoxy radical is an example of an intermediate of enzymatic rxns that escapes the rxn and goes into the body Reactive nitrogen-oxygen species (RNOS) – free radicals with nitrogen and oxygen - These come mainly from the free radical nitric oxide (NO), which is made by nitric oxide synthase (NO synthase) NO combines with oxygen or superoxide to form a RNOS Page 440 – table of the reactive oxygen species and reactive nitrogen-oxygen species ROS are constantly being formed in the cell - - About 3-5% of the oxygen we take in is converted to oxygen free radicals Some ROS are made as normal by-products that escape from the active site of metal-containing enzymes during oxidation rxns Other ROS are normal products of oxidases in peroxisomes, like hydrogen peroxide Toxic free radicals are deliberately made during the inflammatory response Drugs, radiation, air pollutants, and other things can increase making of free radicals in cells One of the major sites of superoxide making is coenzyme Q (CoQ) in the electron transport chain in mitochondria o During the electron transport chain, the reduced form of CoQ that has one electron (CoQH●) is free within the mitochondrial membrane, and can accidentally transfer an electron to oxygen, forming superoxide o When oxygen binds to cytochrome oxidase and accepts an electron though, none of the reactive oxygen species intermediates get released, so no ROS is generated Most of the oxidases, peroxidases, and oxygenases in the cell bind oxygen, and transfer single electrons to it via a metal o Free radical intermediates of these rxns can be accidentally released before the reduction is complete o Cytochrome P450 enzymes are a major source of free radicals leaked from rxns Cytochrome P450’s catalyze rxns where single electrons are transferred to oxygen and an organic substrate, so there’s a high chance of accidentally releasing a free radical before reduction is finished So inducing cytochrome P450 enzymes with alcohol, drugs, or toxins, can lead to increased cell injury Ex: carbon tetrachloride (CCl4) – used often in cleaners P450’s convert carbon tetrachloride into free radical (CCl3●) that is very reactive and can cause hepatocellular necrosis The P450 accidentally converts CCl4CCl3● + Cl, and the CCl3● can’t continue through the oxidation pathway, so it leaks out of the active - site of the P450 enzyme, and initiates chain rxns in the surrounding lipids of the ER, then the rest of the cell This leads to cell swelling, accumulation of lipids, and cell death o Monoamine oxidase (MAO) uses oxidation to degrade dopamine, producing hydrogen peroxide, in the mitochondrial membrane of some neurons o Peroxisomal fatty acid oxidase makes hydrogen peroxide during oxidation of very long chain fatty acids o Xanthine oxidase – works in purine degradation, and is a major cause of ischemiareperfusion injury, especially in the intestine mucosal or endothelial cells Xanthine oxidase can reduce oxygen to superoxide or hydrogen peroxide o Lipid peroxides can be formed as intermediates when enzymatically making eicosanoids like leukotrienes and prostaglandins Ionizing radiation has enough energy that it can split water into hydroxyl and hydrogen radicals o So it can damage the skin, and cause mutations, cancer, and cell death o Ionizing radiation includes x rays, radioactive chemicals, and cosmic rays from the sun ROS can mess up a cell by reacting with lipids, proteins, carbs, and DNA, to extract electrons - - - - Page 442 – visual of how free radicals hurt a cell Lipid & lipid peroxy radicals are formed in a cell by a free radical attacking the cell’s membrane o An initiator (ex: hydroxyl radical) starts the chain rxn by extracting a hydrogen atom, preferably from the double bond of a polyunsaturated fatty acid in a membrane lipid o Next, oxygen adds to form lipid peroxyl radicals and lipid peroxides Eventually, lipid degradation happens, which can form: – page 443 visual o Malondialdehyde – from fatty acids with 3 or more double bonds Shows up in the urine, so it can be used to measure free radical damage o Ethane– from the ω-terminal carbons of 3 carbon fatty acids (omega 3 fats) o Pentane – from the ω-terminal carbons of 6 carbon fatty acids (omega 6 fats) Peroxidation of lipids changes or damages the lipid structure o The aldehydes formed can cross link proteins o When the lipids are part of a membrane, the membrane structure is disrupted o If the disrupted membrane is a mitochondrial membrane, it can lead to release or making of more free radicals In proteins, the amino acids most targeted by hydroxyl radical and oxidative damage are proline, histidine, arginine, cysteine, and methionine o Oxidative damage to a protein can cause the protein to fragment, or for cross-links to form o For cysteine, free radicals can cause cross-linking and form aggregates that prevent their degradation For the other amino acids though, free radicals make them more likely to be degraded o - Free radical attack and oxidation of the cysteine in glutathione will increase oxidative damage throughout the cell Glutathione is a major cell defense against free radical injury, so oxidizing it reduces its protective effects Free radicals can also attack DNA, causing strand breaks and base changes o This can be fixed by DNA repair pathways, or lead to apoptosis o Ex: hydroxyl radical can convert guanine to 8-hydroxyguanine, which can be used to measure the amount of oxidative damage in a cell Adding the hydroxyl to guanine causes it to mispair with adenine NO has a single electron, so it binds to other stuff with single electrons, like ferric iron (Fe3+) - - - NO is a gas that can diffuse through the lipid membrane and cytoplasm, into the cell NO, at low concentrations, can be a neurotransmitter, and hormone that causes vasodilation o NO synthase makes NO from arginine o NO gas, in the target cell, works by binding to iron-heme in the enzyme guanylyl cyclase Nitroglycerin is taken as a tablet for coronary artery disease with angina, because it forms NO to be a vasodilator, which increases blood flow to the heart to relieve the angina o NO though is rapidly inactivated, so cells that make NO need to be close to target cells o The body has 3 different isoforms of NO synthase, each encoded by a different gene for a specific tissue Neuronal NO synthase (nNOS, isoform 1) Inducible NO synthase (iNOS, isoform 2) Endothelial NO synthase (eNOS, isoform 3) o nNOS and eNOS are the ones that make the small amount of NO used as a neurotransmitter or hormone, and is controlled by calcium concentration At high concentrations, NO can combine with oxygen or superoxide to form reactive species that have both nitrogen and oxygen, called reactive oxygen-nitrogen species (RNOS) o iNOS is found in cells of the immune system, like macrophage or astroglia, and is controlled more by gene transcription, and not calcium o iNOS makes high toxic levels of NO, to kill invading microbes o So iNOS is the source that generates most RNOS and NO toxicity o RNOS are involved in neurodegenerative diseases, like Parkinson’s, and chronic inflammatory diseases, like rheumatoid arthritis NO can be toxic either through direct toxic effects from binding to iron containing proteins, or through indirect effects mediated by things formed when NO combines with oxygen or superoxide, to form RNOS o Direct toxic effects of NO: NO combines with iron-containing things that also have single electrons Includes Fe-S centers (ex: electron transport chain complexes 1, 2, and 3), & iron-heme proteins (Hgb & electron-transport chain cytochromes) o This only usually causes little damage, because there’s so little NO and so many of these iron compounds NO causes serious problems through direct inhibition of respiration in cells that are already compromised through oxidative phosphorylation diseases or ischemia Reactive nitrogen-oxygen species toxicity: When NO is present at very high concentrations, like during inflammation, it combines with superoxide to form peroxynitrite (ONOO -), or with oxygen to form N2O3 Peroxynitrite is not a free radical, but is a strong oxidizing agent that is stable and directly toxic Peroxynitrite can diffuse through membranes to affect methionine side chains in proteins & SH groups, like in the Fe-S centers of the electron transport chain Peroxynitrite can also break down into other RNOS, like free radical nitrogen dioxide (NO2), which can initiate lipid peroxidation Peroxynitrite can also react (called nitration) with aromatic rings N2O3 is made from either NO2 or nitrite, and is the agent of nitrosative stress N2O3 nitrosylates sulfhydryl groups in the cell Nitrosylation interferes with the proper functioning of the protein or lipid it targeted RNOS can inhibit enzymes, cause mitochondrial lipid peroxidation, inhibit the electron transport chain, and cause strand breaks in DNA Forming free radicals during phagocytosis and inflammation: - - - In response to infectious agents, phagocytes rapidly consume oxygen in the respiratory burst The respiratory burst is a major source of superoxide, hydrogen peroxide, hydroxyl radical, RNOS, and HOCl NADPH oxidase is what causes the respiratory burst, by transferring an electron from NADPH to oxygen to form superoxide o The superoxide is then converted by superoxide dismutase into hydrogen peroxide Myeloperoxidase is an enzyme found only in phagocytes that converts hydrogen peroxide into HOCl o HOCl oxidizes many iron and sulfur containing groups, oxidizes proteins, and cleaves peptide bonds o Aerobic bacteria attacked by HOCl quickly lose membrane transport The respiratory burst: o First, NADPH oxidase is activated on the outer side of the plasma membrane to initiate the respirator burst, forming superoxide o During phagocytosis, the plasma membrane invaginates, so superoxide is released into the phagolysosome o - - - Superoxide is then converted either spontaneously or with superoxide dismutase into hydrogen peroxide o Hydrogen peroxide can also be converted to hydroxyl radical by the Fenton rxn o Granules with myeloperoxidase are then secreted into the phagosome, where it generates HOCl o iNOS can be activated to make NO, which can combine with superoxide to form peroxynitrite o This together attacks the phagocytosed cell, causing it to lyse o it’s called a respiratory “burst” because it lasts only 30-60 minutes, & consumes oxygen In chronic granulomatous disease, phagocytes have a genetic defect in NADPH oxidase o The X-linked version has the defect in a transmembrane β-subunit that transfers electrons on NADPH to FAD, which then transfers them to iron-heme things o The more rare autosomal recessive version has the defect in subunits of NADPH oxidase in the cytoplasm, like p47 and p67, and the transmembrane α-subunit, which together work in assembling the enzyme and stabilizing it o People with chronic granulomatous disease are more susceptible to infections When neutrophils are activated to make NO, they also activate NADPH oxidase to make superoxide o So the NO and superoxide combine to form peroxynitrite, which can form other RNOS In rheumatoid arthritis, released free radicals from phagocytes oxidzie IgG in the synovial fluid, which makes it easier for them to bind the rheumatoid antibody, causing neutrophils to release more free radicals Cell defense against oxygen toxicity – antioxidant enzymes, antioxidants, cell compartmentation, metal sequestration, and fixing oxygen caused damage - - - - Antioxidant enzymes convert free radicals into non-toxic stuff o The highest # of these enzymes are in places where a lot of ROS are made, like the liver, adrenals, and kidney, which have lots of mitochondria & peroxisomes, & P450 enzymes Antioxidants can end free radical chain rxns o Antioxidants include dietary stuff like vitamin E and flavonoids, and endogenous stuff like urate Example of compartmentation: many enzymes that make hydrogen peroxide are localized in peroxisomes surrounded by a lot of antioxidant enzymes Metals get bound to proteins to prevent them from entering the Fenton rxn o Ex: iron binds to its storage protein ferritin, which is mobile, and excess iron is stored in nonmobile hemosiderin Antioxidant scavenging enzymes – superoxide dismutase, catalase, and glutathione peroxidase o Superoxide dismutase converts superoxide to hydrogen peroxide and oxygen (page 448) Since superoxide is such a strong initiator of chain rxns, SOD is called the primary defense against oxidative stress There’s 3 forms of superoxide dismutase: - A copper-zinc form in the cytoplasm A manganese form in the mitochondria A copper-zinc form gotten extracellularly Mutations to the intracellular form of copper-zinc SOD is found in familial amyotrophic lateral sclerosis (ALS, Lou Gehrig disease) Only up to 10% of cases of ALS are familial Superoxide dismutase is increased by things that make superoxide Mitochondria need lots of superoxide dismutase, because they are major sites of generating superoxide from interaction between CoQ and oxygen o Catalase reduces hydrogen peroxide into water (page 448) If hydrogen peroxide isn’t reduced, it can form hydroxyl radical Catalase is found mainly in peroxisomes, and somewhat in the cytoplasm The highest amount of catalase is found in the kidney and liver Catalase also works in phagocytes to protect from the respiratory burst o Glutathione (γ-glutamylcysteinylglycine) is one of the body’s main ways to protect from oxidative damage Glutathione is a tripeptide made of glutamate, cysteine, and glycine, with a cysteine attached to the γ-carboxyl group In glutathione peroxidases, it’s reactive sulfhydryl groups reduce hydrogen peroxide to water, and lipid peroxides to nontoxic alcohols These rxns oxidize 2 glutathiones into a single glutathione disulfide Glutathione are selenium enzymes found mainly in the mitochondria or cytoplasm, and they’re a big reason we need selenium in our diet Once oxidized glutathione is formed, it needs reduced back to the sulfhydryl form by glutathione reductase in a redox cycle (page 448 bottom pic) Glutathione reductase has FAD, and catalyzes transfer of electrons from NADPH to the disulfide bond of oxidized glutathione (GSSG) This makes NADPH essential for protecting against free radicals The major source of NADPH for this rxn is the pentose phosphate pathway Nonenzymatic antioxidants (free radical scavengers) – convert free radicals to a nonradical, nontoxic form without using enzymes o Antioxidants neutralize free radicals by donating a H+ & its electron to the radical o This oxidizes the antioxidant o Dietary antioxidants – vitamin E, vitamin C, carotenoids, flavonoids o Endogenously made antioxidants – urate, melatonin o All antioxidants have a conjugated double bond system o Vitamin E (α-tocopherol) – lipid soluble antioxidant vitamin that works mainly to protect against lipid peroxidation in membranes When vitamin E donates an electron to a lipid peroxy radical, it’s converted to a free radical form that is stabilized by resonance (page 450) o o o o Vitamin E’s makeup makes it so that it’s more likely to donate a second electron and get fully oxidized, than stay a free radical Vitamin E is gotten in the diet from vegetable oils, egg yolks, and cereals It’s absorbed with lipids (fat soluble), so problems absorbing fat cause vitamin E deficiencies Vitamin E circulates in the blood bound to lipoproteins Vitamin E deficiency causes neuro problems, because the lipids in myelin are sensitive to free radical injury Vitamin C (ascorbic acid) – reduced vitamin C can regenerate the reduced form of vitamin E by donating electrons in a redox cycle Vitamin C is water soluble and circulates unbound in blood and ECF Vitamin C is also a redox coenzyme in making collagen Carotenoids – term for βcarotene (precursor to vitamin A) and other stuff with oxygen containing stuff on its rings, like zeaxanthin and lutein These things can exert antioxidant effects, and quench singlet oxygen Singlet oxygen is a very ROS where there’s no unpaired electrons, but instead there is an entirely empty orbital Carotenoids from fruits and veggies can slow progression of cancer and atherosclerosis by acting as chain-breaking antioxidants Clinical tests with β-carotene supplements though have shown no effect or bad effects from it acting as a pro-oxidant in the free radical form Intake of lutein and zeaxanthin decreases the chances of macular degeneration Lutein and zeaxanthin are concentrated in the macula (central part of the retina), so they’re called macular carotenoids Age-related macular degeneration (AMD) is the leading cause of blindness in the US AMD is vision loss from oxidative damage to the retinal pigment epithelium (RPE) and choriocapillaris epithelium The photoreceptor/retinal pigment complex is exposed to sunlight, and gets almost as much oxygen as the arteries, and also has membranes with lots of lipids Lipofuscin granules accumulate in the RPE throughout life, and can serve as photosensitizers, causing damage by absorbing blue light to make singlet oxygen, leading to other radicals Lutein and zeaxanthin accumulate in the macula and absorb the blue light, and quench singlet oxygen Studies show that people who eat more foods with vitamin E, β-carotene, and vitamin C, have a lower risk of cancer and other ROS caused diseases Studies also show that supplements of these vitamins either had no effect or harmful effects compared to eating foods with this stuff o - Flavonoids – group of things with 2 aromatic rings found in red wine, green tea, chocolate, and other plant foods Some flavonoids inhibit enzymes that make superoxide, like xanthine oxidase Other flavonoids chelate iron and copper, so they can’t enter the Fenton rxn Flavonoids can also act as antioxidants by donating electrons to radicals to stabilize them, or by just complexing with them Ex: quercetin – found mainly in fruit and vegetable skins Endogenous antioxidants – uric acid and melatonin o Uric acid is made from the breakdown of purines, and is released into the blood, saliva, and lung fluid Uric acid together with protein thiols are the major free-radical trapping method of the plasma Uric acid is especially important in the upper airways, where there aren’t many antioxidants Uric acid can scavenge hydroxyl radicals, peroxy radicals, and radicals made from Hgb when it reacts with a peroxy radical (oxyheme oxidants) o Melatonin is secreted by the pineal gland, and is a neurohormone that works in circadian rhythm, light-dark signaling, and inducing sleep Melatonin also donates an electron as a hydrogen to neutralize free radicals Parkinson disease – when the neurons of the substantia nigra, which have melanin and dopamine, degenerate - - The basal ganglia is the part of the of brain that regulates flow of info from the cerebral cortex to the motor neurons of the spinal cord The neostriatum is the major thing carrying input from the cerebral cortex The substantia nigra has neurons that provide input to the striatum using dopamine as the neurotransmitter (called the nigrastriatal pathway) This info feeds back to the basal ganglia and cerebral cortex to control voluntary movement So the major problem in Parkinson’s is decreased dopamine in the neostriatum, from degeneration of dopaminergic neurons whose cell bodies are in the substantia nigra It’s thought free radicals from mitochondria dysfunction, and problems with the ubiquitinproteosome pathway of protein breakdown initiate Parkinson’s o In neurons with these problems, less dopamine is made, glutathione is decreased, and lipofuscin Lewy bodies are increased, iron levels are higher and ferritin levels are lower o Also, 1-methyl-4-phenylpyridinium (MPP+) increases superoxide making in these neurons and decreases ATP making, by inhibiting NADH:CoQ oxidoreductose, decreasing complex 1 activity o The decreased ATP decrease protein degradation by the ubiquitin-proteosome pathway In Parkinson’s, dopamine levels are decreased by monamine oxidase, which generates hydrogen peroxide o Superoxide dismutase can also convert superoxide into hydrogen peroxide o o o - - - Iron levels increase, which allows the Fenton rxn to make hydroxyl radicals iNOS also makes NO to react with superoxide and form RNOS RNOS and hydroxyl radical lead to chain rxns that cause lipid peroxidation, protein oxidation, lipofuscin making, and neuron degeneration o This all leads to less making and release of dopamine In Parkinson disease, decreased dopamine reaching the basal ganglia causes problems moving Symptoms of Parkinson’s include a resting tremor, stiff muscles that slow movements (called bradykinesia), a characteristic gait with short shuffling steps and leaning forward (postural imbalance), blank stare, and personality changes You treat early stages of Parkinson’s with a monoamine oxidase B inhibitor o Monoamine oxidase is a enzyme that inactivates dopamine in neurons, making hydrogen peroxide o So MAO-B inhibitors inhibit dopamine breakdown, and ↓ hydrogen peroxide making You treat later stages of Parkinson’s with levodopa (L-dopa), a precursor of dopamine Parkinson’s can also show lipofuscin deposits as Lewy bodies in degenerating neurons o The pigment lipofuscin is formed from peroxidatively damaged cell organelles that got autophagocytosed, but couldn’t be digested o Lipofuscin is a mix of lipids and proteins formed from lipid peroxidation o When lipofuscin deposits show up on the skin of old people, they’re called “liver spots,” which is characteristic of aging Ventricular fibrillation – rapid premature beats from an irritative focus in ventricular muscle happen in runs of varying duration - Persistent vfib decreases cardiac output, leading to death Vfib is an arrhythmia that can happen from severe ischemia in the ventricular muscle caused by clots from a ruptured atherosclerotic plaque, or from reperfusing a previously ischemic area, like when you lyse a clot (example of ischemic-reperfusion injury) o Ischemic-reperfusion injury is caused by ROS o When there isn’t enough oxygen, ischemic heart muscle mitochondria can’t maintain ATP levels, causing high sodium and calcium levels in the cell o The decreased amount of electron carriers when there’s no oxygen, and loss of the mitochondrial ion gradient or membrane integrity, leads to making of superoxide once oxygen is available again in reperfusion o Xanthine oxidase in ischemic heart endothelial cells can make ROS In normal tissue, xanthine oxidase is a dehydrogenase that uses NAD+ instead of oxygen as an electron acceptor to degrade purines into uric acid When there is low oxygen, ADPATP decreases, so xanthine oxidase converts to an oxidase to breakdown the increased ADP and adenine While oxygen levels are low, xanthine oxidase doesn’t cause damage Once oxygen is reperfused though, xanthine oxidase generates hydrogen peroxide and superoxide o o During ischemia, the heart can’t generate ATP from oxidative phosphorylation, and damage seems to accelerate once you get oxygen back During ischemia, CoQ of the electron transport chain gets saturated with electrons When oxygen is reperfused, more electrons are donated to oxygen to form superoxide, which increased making of hydrogen peroxide & hydroxyl radical Also macrophage come in to clean up the area, and release NO, which can form RNOS During ischemia the decreased oxygen means less ATP is made, and there’s less heart muscle contraction This causes cAMP to accumulate, activating anaerobic glycolysis and lactic acid making If there isn’t enough ATP to maintain sodium-potassium ATPase, sodium accumulates in the cell, causing the cell to swell, and increasing cell proton and calcium levels The decrease in ATP and increase in calcium can open the mitochondrial permeability transition pore, causing permanent inhibition of oxidative phosphorylation Calcium also activates phospholipases to damage lipid membranes Reperfusion with oxygen allows recovery of oxidative phosphorylation, as long as the mitochdonrial membrane has some integrity left and the transition pore can close Reperfusion also increases generation of free radicals Transfer of electrons from CoQ●oxygen to make superoxide increases Endothelium also makes more superoxide from xanthine oxidase Superoxide then forms hydroxyl radical, which can damage the electron-transport chain and mitochondria lipids,and activate the transition pore Macrophage then move in and release NO and superoxide This can all lead to cell death through necrosis, with surrounding slower cell death by apoptosis The lung-lining fluid extends from the nasal cavity to the alveoli, & protects epithelial cells of the airway from ozone and other air pollutants , which aren’t radicals but are toxic & can cause making of ROS - Ozone targets membrane lipids to cause lipid peroxidation Most people can protect themselves from small amounts of ozone, but even a slight increase in ozone can cause respiratory symptoms When ozone levels are low, it’s neutralized by uric acid in the fluid lining the nasal cavity Uric acid, glutathione, and vitamin C are the first line of defense, followed by a combo of vitamin E, glutathione, and superoxide dismutase Premature babies with low levels of lung surfactant need oxygen therapy - You have to closely watch the oxygen levels though to prevent ROS-induced retinopathy and blindness, as well as bronchial pulmonary dysplasia Low levels of SOD and vitamin E increases the chances these things will happen