EFFECT OF THREE DIFFERENT DIRECT COMPRESSION
advertisement

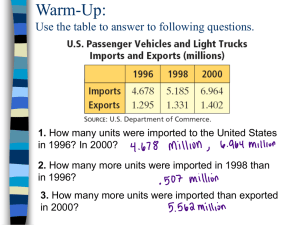
EFFECT OF THREE DIFFERENT DIRECT COMPRESSION FILLERS ON THE RELEASE KINETICS OF DILTIAZEM HYDROCHLORIDE FROM HYDROPHILIC SWELLABLE MATRICES CONTAINING XANTHAN GUM Zaw Min Soe1,*, Satit Puttipipatkhachorn2, Somboon Jateleela2, # 1 Master of Science in Pharmacy Program, Department of Manufacturing Pharmacy, Faculty of Pharmacy, Mahidol University, 447Sri-Ayudhya Road, Bangkok 10400, Thailand 2 Department of Manufacturing Pharmacy, Faculty of Pharmacy, Mahidol University, 447SriAyudhya Road, Bangkok 10400, Thailand *e-mail: zawminsoe01@gmail.com, #e-mail: somboon.jat@mahidol.ac.th Abstract One of the most interesting drug delivery systems is hydrophilic swellable matrix system which is controlled by polymer swelling, polymer erosion, drug dissolution and/or drug diffusion. In this study, the effect of three different direct compression fillers on the release kinetics of diltiazem hydrochloride (DAH) in pH 6.8 phosphate buffer from hydrophilic matrices containing various mass fractions (mf) of xanthan gum (XG) was investigated using USP dissolution apparatus 2. Each formulation of 360 mg matrix tablet contained 120 mg DAH at MF of 0.33; a natural polymer namely XG was used at the mf of 0.15, 0.30, 0.45 or 0.6; and an insoluble filler namely microcrystalline cellulose (MCC) or dibasic calcium phosphate dihydrate (DCPD or soluble filler namely spray dried lactose (SDL) was used for the left mf. From analysis of variance (ANOVA, p < 0.01) and multiple comparison test using least significant difference procedure (LSD, p < 0.01, 2-tailed) for comparing release rates of DAH from matrices containing each filler, the release rates might be ranked as (1) MCC: 0.15 XG > 0.30 XG ≈ 0.45 XG ≈ 0.60 XG, (2) DCPD: 0.15 XG > 0.30 XG > 0.45 XG > 0.60 XG, and (3) SDL: 0.15 XG ≈ 0.30 XG > 0.45 XG > 0.60 XG whereas the sustaining efficacy of fillers for drug release might be ranked as MCC > DCPD > SDL at XG mf of 0.15 – 0.45. Various drug release models were applied to drug release data in order to explain release mechanisms and kinetics. Keywords: dibasic calcium phosphate dihydrate, diltiazem hydrochloride, microcrystalline cellulose, spray dried lactose, hydrophilic swellable matrix Introduction DAH is a calcium channel blocker widely used for the treatment of angina pectoris and the management of hypertension. Its short biological half-life of 3.5 h, high aqueous solubility, and frequent administration make it a potential candidate for sustained release preparations. To control the release of the drugs, which are having different solubility properties, the drug is dispersed in hydrophilic swellable matrix or hydrophobic nonswellable matrix (1-3). Matrix is the release system which prolongs and controls the release of the drug. Various factors such as the type of polymer, drug: polymer ratio, solubility of drug and fillers, and compression force relate to the release of drug from hydrophilic swellable matrices. Husen et al. investigated influence of fillers and natural gums on the controlled release of metochlopramide hydrochloride from direct compressible tablets. Fastest release from tablet with 45% guar gum was observed in the case of MCC, followed by lactose and DCPD. The difference in the filler solubility explains the slower drug release from matrix with DCPD as compared to lactose (4-7). The objective of this study was to investigate the effect of MCC, DCPD and SDL on the release rates and kinetics of DAH from matrices containing xanthan gum. Because of its very high solubility in water and short elimination half-life of 3.5 h, DAH is a suitable model candidate selected to study the release kinetics(10). Methodology Twelve formulations were prepared with batch size of 20 tablets. Each formulation of 360 mg matrix tablet contained 120 mg DAH (B.T. Gen S.A, Lugano Branch, Switzerland) at MF of 0.33, XG (Pernofen/Wulzeshofen, Austria) was used as a natural polymer at MF of 0.15, 0.30, 0.45 or 0.6 while MCC (Avicel® PH-101) or DCPD (Emcompress®) was used as an insoluble filler or SDL (FlowLac®) was used as a soluble filler. Blending of the mixture is performed in pestle and motar for 15 min. Each matrix were manually made by direct compaction of the 360 mg mixture at a force of 1000 kg in a hydraulic press (model C, Fred S. Carver, USA) equipped with a 12.5-mm round flat-face tooling. The release of DAH from the matrices was measured in a 900 ml of pH 6.8 phosphate buffer at 37ºC ± 0.5ºC using basket apparatus (model VK 7000, Vankel, USA) at a speed of 100 rpm. Filtered samples were withdrawn and assayed at 1, 2, 3, 4, 5, 6, 12 and 24 h using the UV spectrophotometer (Shimadzu, model UV-1601, Japan) at 236.4 nm. Six replicates were tested and their mean % released and SD was calculated. Table 1. DAH Formulation prepared with insoluble and soluble fillers containing Xanthan Gum Formulation DAH XG MCC DCPD SDL I 120 54 186 - II 120 108 132 - III 120 162 78 - IV 120 216 24 - V 120 54 186 - VI 120 108 132 - VII 120 162 78 - VIII 120 216 24 - IX 120 54 - X 120 108 - XI 120 162 - XII 120 mg 216 mg - 186 132 78 24 mg Theoretical Consideration (8-10) The release of a water-soluble-drug drug by diffusion through the gel layer is approximately dependent on the square root of time and can be expressed in the following formula which conforms Higuchi’s model of drug diffusion. Q = k’√𝐷𝑎 𝑡 = k √𝑡 (1) Where Q is the amount of drug released in time, t; Da is the apparent diffusivity of drug through the rubbery region; k’ and k are kinetic constants. For Soluble Filler To predict drug release from a matrix system with various concentration of polymers, several assumptions were made (i) drug release can be approximately modeled using Eq (1), (ii) apparent diffusivity of drug in the rubbery region is related to the porosity, ε and the tortuosity, τ of the swelling layer Eq (2), (iii) for soluble filler, the porosity is directly proportional to the volume fraction of soluble solutes (drug and filler) in matrix, which are related to (1- polymer concentration) / apparent density of mixed solute compact (ρa) as in Eq (3), and (iv) Shah et al demonstrated that the tortuosity depends upon the degree of polymer hydration, which is directly proportional to the polymer concentration as in Eq (4). Da = ε/τ ε = δ (1–Cp)/ρa τ = ψCp Da = γ (1-Cp)/Cp Q= 𝜎√(1−𝐶𝑝 )𝑡 √𝐶𝑝 (2) (3) (4) (5) (6) where δ, ψ, γ and σ are kinetic constants. From Eq (6) Q is the function of Cp and can be expressed as Q = α+β √(1 − 𝐶𝑝 )/𝐶𝑝 (7) where α and β are kinetic constants. The regression equations for the amount of drug released at 1, 2, 3, ….i h (Q1, Q2, Q3, …Qi) in relation of polymer concentration are as follows: Qi = ai+bi√(1 − 𝐶𝑝 )/𝐶𝑝 (8) A plot of the amount, Q versus √(1 − 𝐶𝑝 )/𝐶𝑝 will give ai and bi. It is possible that both ai and bi are a function of the square root of time if is constant, therefore, ai = c + Ka √𝑡 (9) bi = d + Kb√𝑡 (10) where c, d, Ka, and Kb are the regression constants. Equation (8) is further derived to obtain the working equation for prediction drug release from a hydrophilic swellable matrix. Qi = (c+Ka√𝑡) + (d+Kb√𝑡) √(1 − 𝐶𝑝 )/𝐶𝑝 (11) Qi = (c+d√(1 − 𝐶𝑝 )/𝐶𝑝 ) + (Ka+Kb√(1 − 𝐶𝑝 )/𝐶𝑝 )√𝑡 (12) For Insoluble filler For insoluble filler, the porosity is only directly proportional to the volume fraction of soluble drug in matrix, which depends upon the mass fraction of drug divided by the density of solid compact and is assumed to be constant, f as in Eq (13), and (iv) Shah et al demonstrated that the tortuosity depends upon the degree of polymer hydration, which is directly proportional to the polymer concentration as in Eq (14). ε = δf/ρa (13) τ = ψC (14) Da = γ/Cp (15) Q= 𝜎 √𝑡 √𝐶𝑝 (16) where δ, ψ, γ and σ are kinetic constants. From Eq (16) Q is the function of Cp and can be expressed as Q = α+β√1/(𝐶𝑝 (17) where α and β are kinetic constants. The regression equations for the amount of drug released at1, 2, 3, ….i h (Q1, Q2, Q3, …Qi) in relation of polymer concentration are as follows: Qi = ai+bi√(1/𝐶𝑝 (18) A plot of the amount, Qi versus √(1/𝐶𝑝 will give ai and bi. It is possible that both ai and bi are a function of the square root of time, therefore ai = c+Ka√𝑡 (19) bi = d+Kb√𝑡 (20) where c, d, Ka and Kb are the regression constants. Equation (18) is further derived to obtain the working equation for prediction drug release from a hydrophilic swellable matrix: Qi = (c+Ka√𝑡) + (d +Kb√𝑡)√(1/𝐶𝑝 ) (21) Qi = (c+d√(1/𝐶𝑝 )+ (Ka+Kb√(1/𝐶𝑝 )√𝑡 (22) Results and Discussions High regression coefficients (R2) from linear regression analysis between % DAH released and √𝑡 indicated that the release of DAH by diffusion across swelling matrix was dependent on √𝑡 and various kinetic rate constants k were received as shown in Table 2-3. Using equation 22, the working equation to predict drug release from xanthan gum matrices containing insoluble fillers and equation 12, the working equation to predict drug release from xanthan gum matrices containing soluble filler are as follows: For insoluble fillers, Q = (-11.91+5.37x) + (14.74+1.28) √𝑡 for MCC (23) Q = (-10.27+4.52x) + (8.41+6.31x) √𝑡 for DCPD (24) where x = √(1/𝐶𝑝 ) For soluble filler, Q = (-12.50+6.40x) + (15.21+4.09x) √𝑡 for SDL (25) where x = √(1 − 𝐶𝑝 )/𝐶𝑝 ) Figure 1-3 show the theoretical DAH release profiles versus experimental data for xanthan gum matrices using MCC, DCPD and SDL, respectively. The experimental data from release testing are closely matched the theoretical release profiles. This implies that the release profiles of DAH from various matrices can be predicted mainly by the diffusion model of Shah et al for insoluble MCC or DCPD and that of Jateleela et al for soluble SDL. Table 2. Kinetic constants k, y-intercepts and R2 for formulations containing insoluble fillers. Formulation k, % h-1/2 SD of k y-intercept, % R2 I 18.97 0.75 0.02 0.9979 II 16.64 1.37 -0.58 0.9978 III 16.83 0.48 -4.50 0.9968 IV 17.51 0.92 -5.91 0.9958 V 24.69 0.43 1.77 0.9976 VI 19.71 0.37 -2.70 0.9967 VII 18.42 0.20 -4.04 0.9972 VIII 16.15 0.53 -3.60 0.9959 Table 3. Kinetic constants k, y-intercepts and R2 for formulations containing SDL. Formulation k, % h-1/2 SD of k y-intercept, % R2 IX 24.20 1.03 3.68 0.9942 X 23.55 1.23 -4.53 0.9967 XI 20.91 0.25 -7.44 0.9960 XII 16.97 0.78 -4.95 0.9900 100 % Drug Rleleased 80 60 40 20 0 0 -20 4 8 12 16 20 24 Time, h Figure 1. Theoretical predicted release profiles versus experimental data for matrices using MCC at various mf of XG. Key: Theoretical: ˗˗˗, 0.15; - - -, 0.30; ˗ ∙ ˗ ∙ ˗, 0.45; and ........., 0.60. Experimental: ●, 0.15; ■, 0.30; ▲, 0.45; and ♦, 0.60. % Drug Released 100 80 60 40 20 0 0 4 8 -20 12 16 20 24 Time, h Figure 2. Theoretical predicted release profiles versus experimental data for matrices using DCPD at various mf of XG. Key: Theoretical: ˗˗˗, 0.15; - - -, 0.30; ˗ ∙ ˗ ∙ ˗, 0.45; and ........., 0.60. Experimental: ●, 0.15; ■, 0.30; ▲, 0.45; and ♦, 0.60. % Drug Released 100 80 60 40 20 0 0 4 8 12 Time, h 16 20 24 Figure 3. Theoretical predicted release profiles versus experimental data for matrices using SDL at various mf of XG. Key: Theoretical: ˗˗˗, 0.15; - - -, 0.30; ˗ ∙ ˗ ∙ ˗, 0.45; and …., 0.60. Experimental: ●, 0.15; ■, 0.30; ▲, 0.45; and ♦, 0.60. From analysis of variance (ANOVA, p < 0.01) and multiple comparison test using least significant difference procedure (LSD, p < 0.01, 2-tailed) for comparing release rates of DAH from matrices containing each filler, the release rate of DAH was significantly affected by the mf of XG and might be ranked as (1) MCC: 0.15 XG > 0.30 XG ≈ 0.45 XG ≈ 0.60 XG, (2) DCPD: 0.15 XG > 0.30 XG > 0.45 XG > 0.60 XG, (3) SDL: 0.15 XG ≈ 0.30 XG > 0.45 XG > 0.60 XG The sustaining efficacy of fillers for DAH release rate might be ranked as MCC > DCPD > SDL at XG mf of 0.15 – 0.45, but at 0.60 XG, the sustaining efficacy of these fillers was not significantly different. MCC or DCPD cannot be dissolved in phosphate buffer whereas SDL can be dissolved and released very rapidly, subsequently smaller pores are produced in the insoluble matrix and DAH is then released with slower rate than from matrix using SDL. However, MCC provided slower drug release than DCPD did at 0.15 – 0.45 mf XG. This may be caused by some swelling property of MCC which result in smaller pores in matrix. From fig 2, the matrix using DCPD showed that the real % DAH release data is higher theoretical prediction. This indicated that matrix using DCPD at lowest mf of XG possessed lower structural strength and easily caused eroded particles from the surface which provide higher release rate of DAH. Conclusion The release rate of DAH was significantly affected by the mf of XG in matrix containing each direct compression filler and might be ranked as (1) MCC: 0.15 XG > 0.30 XG ≈ 0.45 XG ≈ 0.60 XG, (2) DCPD: 0.15 XG > 0.30 XG > 0.45 XG > 0.60 XG, (3) SDL: 0.15 XG ≈ 0.30 XG > 0.45 XG > 0.60 XG. MCC provided highest retarding efficacy of for DAH release from matrices containing XG mf of 0.15 – 0.45. The release profiles of DHA from XG matrices using insoluble MCC or DCPD or soluble SDL could be predicted by the three operating equations developed according to Higuchi’s diffusion model along with Shah et al equations for insoluble fillers, and Jateleela et al equations for soluble filler. This investigation showed that the drug release from matrices could be optimized to prepare an once-daily dose of DAH using a minimum of experiments. References 1. Prabu SL, Shirwaikar AA, Shirwaikar A, Ravikumar G, Kumar A, Jacob A. Formulation and evaluation of oral sustained release of diltiazem hydrochloride using rosin as matrix forming material. Ars Pharm 2009; 50(1): 32-42. 2. Nokhodchi A, Raja S, Patel P, Addo KA. The role of oral controlled release matrix tablets in drug delivery systems. BioImpacts 2012; 2(4): 175-187. 3. Patel H, Panchal DR, Patel U, Brahmbhatt T, Suthar M. Matrix type drug delivery system: a review. JPSBR 2011; 1(3): 143-151. 4. Jayanthi B, Manna PK, Madhusudhan S, Mohanta GP, Manavalan R. Per oral extended release products An overview. JAPS 2011; 1(2): 50-55. 5. Grassi M, Grassi G. Mathematical modeling and controlled drug delivery: matrix systems. Current Drug Delivery 2005; 2: 97-116. 6. Maderuelo C, Zarzuelo A, Lanao JM. Critical factors in the release of drugs from sustained release hydrophilic matrices. J Control Release 2011; 154(1): 2-19. 7. Husen PM, Kumar PA, Kulkarni SV, Someshwara. Formulation and in vitro evaluation of controlled release matrix tablets of metochlopramide hydrochloride: influence of fillers on hydrophilic natural gums. Int J Pharm Sci 2012; 4(4): 181-187. 8. Vaghani SS, Goyani M, Singh S. Matrix dosage form of diltiazem hydrochloride: development, characterization and in vitro evaluation. Acta Pharm Sci 2011; 53: 393-400. 9. Shah N, Zhang G, Apelian V, Zeng F, Infeld MH, Malick AW. Prediction of drug release from hydroxypropylmethylcellulose (HPMC) matrices: effect of polymer concentration. Pharm Res 1993; 10(11): 1963-1965. 10. Jateleela S, Mitrevej A, Sarisuta N, Kinetic release of diltiazem hydrochloride from hydrophilic swellable matrices. J Ind Pharm 2010; 13: 25-34. 11. Bolton S. Statistics: Multiple comparisons in ANOVA. In: Troy DB ed, Remington: The science and practice of pharmacy. 22nd ed, London: Pharmaceutical Press; 2012: 508-517.