County General Hospital 546 That Street. Some Town, YY 12347
advertisement

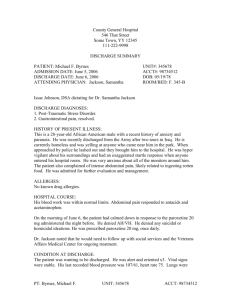
County General Hospital 546 That Street. Some Town, YY 12347 111-222-9998 DISCHARGE SUMMARY PATIENT: Collette Rose ADMISSION DATE: June 5, 1995 DISCHARGE DATE: June 13, 1995 ATTENDING PHYSICIAN: Jackson, Samantha UNIT#: 345678 ACCT#: 98734513 DOB: 12/04/78 ROOM/BED: F. 346-B Issac Johnson, DSA dictating for Dr. Samantha Jackson DISCHARGE DIAGNOSES: 1. Major Depression 2. Alcohol Abuse HISTORY OF PRESENT ILLNESS: This is an 18-year-old Caucasian female with a recent history of major depression and suicide attempt. She ingested nearly an entire bottle of acetaminophen. Her sister discovered her passed out in the bathtub and called 911. She was brought to the emergency department by ambulance. She was admitted for further evaluation, stabilization and medication management. ALLERGIES: No known drug allergies. HOSPITAL COURSE: Treatment began in the ambulance on the way to the hospital. Activated charcoal was administered. Upon admission, gastric lavage was conducted to clean out the contents of her stomach. Patient’s BAC level was 0.15. She was given fluids to rehydrate her system after respiratory stabilization. On the morning of June 13, the patient had calmed down in response to the medication and care provided the last 7 days. She denied AH/VH. She denied any suicidal or homicidal ideations. She was prescribed fluoxetine 20mg, once daily. Dr. Jackson noted that she would need to follow up with social services and XYZ Community Mental Health Center for ongoing treatment. CONDITION AT DISCHARGE: The patient was wanting to be discharged. She was alert and oriented x3. Vital signs were stable. Her last recorded blood pressure was 107/61, heart rate 75. Lungs were clear. Abdomen was soft, nontender, nondistended with positive bowel sounds. She was PT: Rose, Collette UNIT: 345678 ACCT: 98734513 discharged on June 13, 1995, with discharge instructions given and medications reconciled. LABORATORY DATA: On June 5, sodium 143, potassium 3.8, chloride 109, co2 of 28, anion gap 6.0, glucose 122, BUN 17, creatinine 1.1, total protein 6.5, albumin 3.4, globulin 3.1, calcium 8.8, phosphorus 3.7, total bilirubin 0.3, AST 14, ALT 15, alkaline phosphatase 88, magnesium 2.2, triglycerides 50, cholesterol 150, HDL cholesterol 45, and LDL 120. Hematology values on June 6, white blood count 11.6, hemoglobin and hematocrit 12.3 and 36.5 respectively, with platelet count of 282,000. DISCHARGE MEDICATIONS: 1. Fluoxetine 20 mg DISCHARGE INSTRUCTIONS: Follow up with Social Services as instructed r.e. housing. Follow-up with XYZ Community Mental Health Center for ongoing treatment. Dictated by Issac Johnson DSA DD: 06/14/1995 12:25:34 DT: 06/14/1995 13:15:25 CGHANYHSC; Job#543322 Authenticated by Samantha Jackson MD on 06/15/1995 06:45:21 PM PT: Rose, Collette UNIT: 345678 ACCT: 98734513 County General Hospital 546 That Street. Some Town, YY 12347 111-222-9998 HISTORY AND PHYSICAL REPORT PATIENT: Collette Rose ADMISSION DATE: June 5, 1995 ADMITTING PHYSICIAN: Jackson, Samantha ATTENDING PHYSICIAN: Jackson, Samantha DICTATING PHYSICIAN: Jackson, Samantha UNIT#: 345678 ACCT#: 98734513 DOB: 12/04/78 ROOM/BED: F. 346-B CHIEF COMPLAINT: The patient came in with major depression following a suicide attempt. HISTORY OF PRESENT ILLNESS: This is an 18-year-old Caucasian female with major depression. She complains of feelings of hopelessness. She has lost interest in every day activities that used to bring her joy, including caring for her son. She is sleeping 18-20 hours a day and not caring for her hygiene. She complains of little energy. She reports that she has lost 15 lbs in the last month. She appears to be underweight for her height. PAST MEDICAL HISTORY: The patient has a prior suicide attempt as a juvenile. In 1991, when the patient was 13 years old she took an entire bottle of acetaminophen “to stop the pain.” SOCIAL HISTORY: She is single, she recently had a son, is currently unemployed and homeless. She does not smoke, denies drinking or using drugs but smelled of alcohol at admittance. FAMILY HISTORY: None. MEDICATIONS: None. REVIEW OF SYSTEMS: All other systems are reviewed, otherwise negative. ALLERGIES: None. PHYSICAL EXAMINATION: GENERAL: The patient is lying in the bed, quietly crying. Occasionally sleeps. PT: Rose, Collette UNIT: 345678 ACCT: 98734513 VITAL SIGNS: Significant for patient’s temperature of 99.2, pulse of 88, respiratory rate of 18, blood pressure of 107/61, and pulse ox of 97%. HEENT: Pupils equal, round, reactive to light and accommodation. Extraocular muscles are intact. No icterus, no pallor noted. NECK: Supple, no jugular venous distention, no thyromegaly. CARDIOVASCULAR: Regular rate and rhythm, s1, s2 heard. No murmurs, gallops, or rubs. CHEST: Clear to auscultation. Abdomen: Soft, tender to the touch, nondistended. EXTREMETIES: No edema, No cyanosis. NUEROLOGIC: Alert and oriented x3 and follows all commands. LABORATORY DATA: The patient’s CBC was within normal limits. The patient’s CMP was also within normal limits. ASSESSMENT AND PLAN: Abdominal pain. The patient will be given calcium carbonate and acetaminophen. Anxiety and agitation. The patient will be given Fluoxetine 20 mg to stabilize. The patient will get social worker involved for further plan of care. We will start the patient on antidepressant medications. If this history and physical was performed prior to admission, but within the last 30 days, indicate by initialing one of the following: __I have reassessed the patient and notes that there are no significant changes to the assessment. __I have reassessed the patient and note the following significant changes occurred: DD: 06/05/1995 01:25:30 DT: 06/05/1995 03:14:09 CGHANYHSC; Job#569822 Authenticated by Samantha Jackson MD on 06/07/1995 08:49:45 AM Samantha Jackson Report ID: 0998-0098 Electronically Signed by Samantha Jackson on 06/07/1995 at 0932 PT: Rose, Collette UNIT: 345678 ACCT: 98734513