1. Importance of theory
advertisement

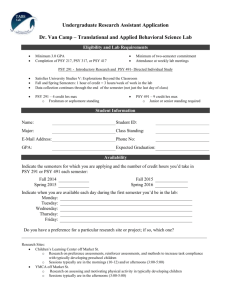
PSY 725 1 PSY 725: Cognitive Behavior Therapy for Children and Adolescents SPRING 2013 POE 724 Instructor: email: Office Hours: Scott A. Stage sastage@ncsu.edu By appointment Office: 625 Poe phone: 515-0318 Class Meeting: TH 10:15 am to 1:00 pm Purpose: PSY 724: Behavioral Interventions is a prerequisite to this course. The material covered in PSY 710.004: Multicultural Issues is also extremely relevant. In addition, this course builds upon the theoretical and procedural bases of assessment taught in PSY 723: Social and Emotional Assessment of Children and Adolescents. In PSY 725, the treatment of mental health disorders of children and adolescents discussed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR, 2000) and the NC Policies Governing Services for Children with Disabilities (2007) will be presented and discussed, with a focus on evidence-based behavior and cognitive behavior therapies. In addition, mediating and moderating influences of the treatments will also be examined. Although class sessions will include discussion of basic therapeutic tools, this course will primarily provide an overview of intervention techniques from validated programs. Implementation and skills acquisition will occur in practica placements. For school psychology students, PSY 725 will be coordinated with the Clinic-based Treatment Practicum (i.e., PSY 641.003: Academic Coaching for Educational Success) in which students will be simultaneously enrolled. Readings have been placed on e-course reserves under the NC State Libraries menu. Student Objectives: 1) To describe and evaluate evidenced-based behavior and cognitive behavior therapy interventions for students with selected DSM disorders (i.e., oppositional defiant disorder, conduct disorder, attention deficit hyperactivity disorder, autism, posttraumatic stress disorder, depression disorders, anxiety disorders, and obsessivecompulsive disorder) including selected school-wide systems for social-emotional problems. 2) To communicate, orally, via Power Point presentations, and in writing, information regarding evidenced-based behavior and/or cognitive behavior therapies to others. 3) To prepare a written treatment protocol for a student with a mental health disorder. 4) To present a review of evidenced-based behavior and/or cognitive behavior therapies for a specific mental health disorder to the class using a Power Point presentation. Course Requirements: 1. Regular class attendance and active participation in class discussions. Active participation in class discussions is essential for meeting the objectives of this course. Students are expected to participate in all phases of the class meetings. Students who are shy or appear reticent about speaking in class will need to learn how to manage this. This might require speaking to the professor. Inability to speak in class will result in an unsatisfactory evaluation. Excessive absence will result in a failing grade (i.e., 2 unexcused absences). Missing a scheduled presentation date will result in zero points unless it is excused. When students have legitimate excused absences, they are responsible for informing the instructor prior to the absence, or the excuse will not be granted. PSY 725 2 2. Students will lead a Power Point presentation and discussion on a Topic described in the Course Outline below. Students will draw numbers from a cup to determine who picks the first topic, second topic, third topic, etc. Students will retrieve the articles placed on course reserve pertaining to that topic and prepare a Power Point presentation summarizing the content of the articles and providing additional articles as seen appropriate. Each presentation should start with a complete description of the DSM-IV-TR criteria and the proposed changes for the DSM-5. The presentation is expected to be 2 to 2 1/2 hours in length. At the end of their Power Point presentation, the presenter is responsible for providing three questions to be discussed in the class between partners. The presenter should allow 20 minutes for discussion between the partners and 20 minutes for a wrap-up discussion lead by the presenter. See the grading rubric below. The Power Point presentation should be sent to the instructor and classmates prior to class. Power Point Presentation of Research Articles describing a Disorder and Treatment Description of DSM-IV-TR and DSM-5 changes. Possible points awarded = 3 What is the pertinent Sp.Ed. consideration? Description of the interventions is sufficient. Possible points awarded = 4 Statistical results and effect size of the interventions Possible points awarded = 4 discussed are provided. Discussion of the interventions in terms of whether it is Possible points awarded = 4 evidenced-based. Moderator and mediator variables are discussed. Possible points awarded = 1 Multi-cultural issues are discussed. Possible points awarded = 1 Three written questions are provided for students in the Possible points awarded = 3 class and the presenter’s facilitation of the discussion at the end of class. 3. Create a written treatment plan for a student with a DSM-IV-TR multiaxial diagnosis and Special Education consideration (Due April 18th or the 25th depending on your Power Point presentation date). Each graduate student will present a treatment case that describes a course of treatment for a school-aged student either in individual or group psychotherapy treatment. Within this description possible psychosocial mediating or moderating influences that affect the student’s functioning and possible eligibility within the special education nomenclature should be discussed. The written format will be as follows: Background Information: Present made-up developmental, cognitive, academic, behavioral and other psychosocial information that frames your client’s level of functioning, also include school functioning. This section should provide the necessary information to determine what the client’s probable multiaxial diagnosis is, as well as, whether the student might qualify for special education services. Close this section with your diagnosis. (Recommended length of this section is 1 to 2 pages). Treatment Plan: PSY 725 3 Treatment goals. Provide short- and long-term goals of therapy prior to describing the sessions. Short term goals describe the desired results after weeks of therapy. Long term goals should describe desired results for the client after therapy is over and one year later. The long term therapy goals should follow from the short term goals. (Recommended length ½ to 1 page). Assessment of client’s performance per session. Devise a way to assess the client and your performance over the course of treatment. For example, for client functioning: Parent/ Teacher Ratings of Behavior, Self-Report Methods, Rating of Group Experience, Self-Monitoring, Observations Outside of the Group, In-Group Observations, Role-Play Tests, and/or Goal Attainment Scaling. Therapist functioning: Supervisor Observations, Client-Rating of Experience, Narrative Notes (i.e., Subjective, Objective, Assessment, Plan), and Self-Assessment. (Recommended length ½ to 1 page). Therapy sessions. Provide a detailed session by session treatment plan. Please cite appropriate references from borrowed material. Describe in detail what each session entails and what the intended outcomes of each session are. Explain how each session will be evaluated as to its intended therapeutic agents (i.e., What is the client learning? and How do you know it is working?). For the best examples of proposed treatment plans, describe what needs to be altered in response to your client’s lack of adaptation at certain key phases along the therapeutic continuum. The treatment plan should include mock session assessments so we can determine in an objective way that the client is benefitting from your treatment (Recommended length of this section is 7 to 10 pages). Summary: Provide a summary paragraph or two of your client’s treatment outcome describing their attainment of their Short and potential to attain Long-term Goals (Recommended length 1 page). Recommendations: Provide a paragraph describing what additional psychotherapeutic interventions would be beneficial (Limit this to only 3 if necessary or not at all). 4. Give a PowerPoint Presentation of your Case Study Treatment Plan. Each student will present a “case study” of your Treatment Plan to the class using PowerPoint. A 45 minute presentation based on your treatment plan will be presented. Time this so that you know when your 45 minutes is done. Grading Rubric for both Written and Power Point Case Study Treatment Plan INGREDIENTS 1 Treatment Plan and PowerPoint contain all the items described above. 2 A copy of your treatment plan is given to your classmates. 3 The plan is coherent and well thought out with accompanying citations that indicate that it is evidenced based. 4 The plan takes into consideration DSM-IV-TR multiaxial diagnoses. 5 Special education eligibility is considered. 6 Assessment of the client’s functioning across therapy is objective and thorough. 7 Assessment of the therapist’s functioning is assessed. 8 Treatment goals are explicit and follow from the diagnoses. GRADE A+ =100 PSY 725 4 9 The Summary is well integrated in relation to the overall background information, treatment plan, and outcome. 10 Recommendations are thoughtful in relationship to other sources of help for the client. DO NOT provide over 3 recommendations, but select only the most salient and important as adjunct to the primary therapy. One of the ingredients described above is unclear or vague. Two of the ingredients above are unclear or vague. Three of the ingredients above are unclear or vague. Four of the ingredients above are unclear or vague. One ingredient is missing or multiple items presented are unclear or missing. Two ingredients are missing or many items presented are unclear Three ingredients are missing or there over six items noted that are unclear or problematic More missing ingredients than above will result in no credit for the project. A=96 A-=92 B+=89 B=86 B-=82 C+=79 C=76 F=59 4. Take-home Final Examination. The final will be composed of up to 10 questions taken from Power Point presentations and assigned readings. Expected length is to be 15-20 pages double-spaced. Course Grades. The Topic Presentation is worth 20 points, Written Treatment Plan (20 points) + Power Point Presentation (20 points) are worth 40 points of your course grade, and the Final Exam is worth 40 points of your course grade. Course letter grades are assigned as shown below and based on the weighted project totals described above. 97.00-100 93.00-96.99 90.00-92.99 87.00-89.99 83.00-86.99 80.00-82.99 77.00-79.99 73.00-76.99 70.00-72.99 60.00-69.99 <59.99 A+ A AB+ B BC+ C CD F Other Information: Incomplete Grades The NCSU Handbook states, “At the discretion of the instructor, students may be given an IN grade for work not completed because of a serious interruption in their work not caused by their own negligence.” IN grades require that the course be completed the following semester. Adverse Weather Policy PSY 725 5 The adverse weather policy for the course is the same as the University policy. Therefore, when in doubt about this class, please check the University web site and follow the directions as posted. Academic Integrity: Students are expected to do their own work on exams and for homework assignments. Any student caught violating this policy will receive a failing grade and be referred to the appropriate university officials. Please consult the university policy on academic integrity at: http://policies.ncsu.edu/policy/pol-11-35-1. The Code of Student Conduct identifies three areas of behavior that constitute academic misconduct: Cheating, Plagiarism, and Aiding and Abetting Others to Cheat or Plagiarize. Students with Disabilities: Accommodations will be made for students with verifiable disabilities. In order to receive accommodations, students must register with Disability Services Office http://www.ncsu.edu/dso/students/students.html Location: Student Health Center Building, 2815 Cates Avenue, Suite 2221, Campus Box 7509, Raleigh, NC 27695-7509 Office Hours: 8:00 AM to 5:00 PM Monday through Friday Phone Numbers: Main: 919.515.7653 TTY: 919.515.8830 Fax: 919.513.2840 Email: disability@ncsu.edu COURSE OUTLINE Week# Date Jan 10th Jan 17th Jan 24th Jan 31st Feb 7th Feb 14th Feb 21st Treatment Topic Review PSY 725 Syllabus What are evidencedbased interventions? Reading Assignment Chambless & Ollendick (2001); Chorpita, Bernstein, & Daleiden (2011); and, Chorpita et al. (2011). Special Education DSM-IV-TR Multiaxial eligibility categories/ vs. Assessment (pp. 27-37).NC DSM IV-TR nomenclature Policies Governing Services and Ethnic Minority Youth for Children with EBIs Disabilities (2007); and, Huey & Polo (2008). School-wide interventions Cheney et al. (2009); for students at-risk for ED. Nelson et al. (2009); Stage et al. (2012); and, Sumi et al. (2012). Disruptive Behavior Brown et al. (2008) pp. 35Disorders: ODD/CD 41; Eyberg, Nelson, & Boggs (2008); Henggeler et al. (1998); and, Kazdin (2003). Attention Deficit Brown et al. (2008) pp. 23Hyperactivity Disorder 32 Fabiano et al. (2010); and, Pelham & Fabiano (2008). Autism Rogers & Vismara (2008); and, Soorya, Carpenter, & Warren (2013). Presentation of Topic by Instructor Instructor Instructor Instructor PSY 725 6 Feb 28th Anxiety Disorders Mar 7th Mar 14th NCSU Spring Break Depression Disorders Mar 21st Post-traumatic Stress Mar 28th Apr 4th NCSU Holiday No class Apr 11th Obsessive-Compulsive Disorder Apr 18th Students case treatment presentations. Students case treatment presentations. Take home final handed-out. Apr 25th May 2nd Brown et al. (2008) pp. 6367; Kendall Coping Cat (1994); Kendall et al. (2000); and, Silverman et al. (2008). Brown et al. (2008) pp. 7685; Cuijpers et al. (2009); David-Ferdon & Kaslow (2008); and, Stark et al. (1998) Silverman et al. (2008); Trauma Focused Cognitive Behavioral Therapy Prepare Power Point Presentation and Treatment Plan Barrett et al. (2008); Brown et al. (2008) pp. 53-58; and, Lewin et al. (2005) Treatment plan due for those presenting. Treatment plan due for those presenting. Take home final due in my office mailbox at 5 pm. Required Text: American Psychological Association (2000). Diagnostic and statistical manual (4th ed – TR). Washington DC: Author. Readings: Barrett, P.M., Farrell, L., Pina, A.A., Peris, T.S., & Piacentini, J. (2008). Evidenced-based psychosocial treatments for child and adolescent obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psychology, 37, 131-156. Brown, R.T., Antonuccio, D.O., DuPaul, G.J., Fristad, M.A., King, C.A., Leslie, L.K., McCormick, G.S., Pelham, W.E., Piacentinit, J.C., & Vitiello, B. (2008). Childhood mental health disorders: Evidence base and contextual factors for psychosocial, psychopharmacological, and combined interventions. Washington, DC: APA. Chambless, D.L. & Ollendick, D.H. (2001). Empirically-supported psychological interventions: Controversies and evidence. Annual Review of Psychology, 52, 685-716. Cheney, D, Stage, S.A., Hawken, L. Lynass, L., Mielenz, C., & Waugh, M. (2009). A two-year outcome study of the Check, Connect, and Expect intervention for students at-risk of severe behavior problems. Journal of Emotional and Behavior PSY 725 7 Disorders, 17, 226-243. Chorpita, B.F., Bernstein, A., & Daleiden, E.L. (2011a). Empirically guided coordination of multiple evidence-based treatments: An illustration of relevance mapping in children’s mental health services. Journal of Consulting and Clinical Psychology, 79, 470-480. Chorpita, B.F., Daleidon et al. (2011b). Evidenced-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clinical Psychology: Science and Practice, 18, 154-172. Cuijpers, P., Munoz, R., Clarke, G.N. & Lewinsohn, P.M. (2009). Psychoeducational treatment and prevention of depression: the “coping with depression” course thirty years later. Clinical Psychology Review, 29, 449-458. David-Ferdon, C. & Kaslow, N.J. (2008). Evidenced-based psychosocial treatments for child and adolescent depression. Journal of Clinical Child and Adolescent Psychology, 37, 62-105. Eyberg, S., Nelson, M.M., & Boggs, S.R. (2008). Evidenced-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology, 37, 215-238. Fabiano, G.A., Vujunovic, R.K., Pelham, W.E., Waschbusch, D.A., Massetti, G.M., Pariseau, M.E., Naylor, J., Yu, J., Robins, M., Carnefix, T., Greiner, A.R., & Volker, M. (2010). Enhancing the effectiveness of special education programming for children with attention deficit hyperactivity disorder using a daily report card. School Psychology Review, 39, 219-239. Henggeler, S.W., Schoenwald, S.K., Borduin, C.M., Rowland, M.D., & Cunningham P.B. (1998). Clinical foundations in MST. Multisystemic treatment of antisocial behavior in children and adolescents (pp. 21-57). New York, NY: Guilford. Huey, S.J., & Polo, A.J. (2008). Evidenced-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology, 37, 262-301. Kazdin, A.E. (2003). Problem-solving skills training and parent management training for conduct disorder. In A.E. Kazdin & J.R. Weisz (Ed.s), Evidence-based psychotherapies for children and adolscents (pp.241-262). New York, NY: Guilford. Kendall, P. (1994). Coping cat program. Promising Practices Network. http://www.promisingpractices.net/program.asp?programid=156 Kendall, P., Chu, B.C., Pimental, S.S., & Choudhury, M. (2000). Treating anxiety disorders in youth. In P. Kendall (Ed.) Child & adolescent therapy: cognitive-behavioral procedures (2nd ed.)(pp. 253-287). New York, NY: Guilford. Lewin, A.B., Storch, E.A., Merlo, L.J., Adkins, J.W., Murphy, T., & Geffken, G.R. (2005). Intensive cognitive behavioral therapy for pediatric obsessive-compulsive disorder: A treatment protocol for mental health providers. Psychological Services, 2, 91-104. Nelson, J.R., Duppong Hurley, K., Synhorst, L., Epstein, M.H., Stage, S., & Buckley, J. (2009). The child outcomes of a behavior model. Exceptional Children, 76, 7-30. North Carolina Polices Governing Services for Children with Disabilities (2007). NC State Board of Education. http://www.dpi.state.nc.us/docs/ec/policy/policies/2007policies.pdf PSY 725 8 Pelham, W.E. & Fabiano, G.A. (2008). Evidenced-based psychosocial treatments for attentiondeficit/ hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology, 37, 184-215. Rogers, S.J. & Vismara, L.A. (2008). Evidenced-based comprehensive treatments for early autism. Journal of Clinical Child and Adolescent Psychology, 37, 8-39. Silverman, W.K., Ortiz, C.D., Viswescvaran, C., Burns, B.J., Kolko, D.J., Putnam, F.W., Fabiano, G.A., Amaya-Jackson, L. (2008). Evidenced-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology, 37, 156-184. Silverman, W.K., Pina, A.A., Peris, & Viswesvaran, C. (2008). Evidenced-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 37, 105-131. Soorya, L.V., Carpenter, L.A. & Warren, Z.(2013). Behavioral and psychosocial interventions for individuals with ASD. The neuroscience of autism spectrum disorders (pp. 69-84). http://dx.doi.org/10.1016/B978-0-12-391924-3.00005-3 Stage, S.A., Cheney, D., Lynass, L., Mielenz,C., & Flower, A. (2012). Three validity studies of the daily progress report in relationship to the Check, Connect, and Expect Intervention. Journal of Positive Behavior Interventions, 14, 181-191. Stark, K.D., Swearer, S., Sommer, D., Hickey B.B., Napolitano, S., Kurowski, C., & Dempsey, M. (1998). School-based group treatment for depressive disorders in children. In K.C. Stoiber & T.R. Kratochwill (Ed.s), Handbook of group intervention for children and families (pp. 68-100). Needham Hts., MA: Allyn & Bacon. Sumi, W.C. et al. (2012). Assessing the effectiveness of First-Step to Success: Are short-term results the first step to long-term improvement? Journal of Emotional and Behavior Disorders. DOI: 10.1177/1063426611429571 Trauma-focused cognitive-behavior therapy. SAMSA: Substance Abuse and Mental Health Services Administration. http://www.modelprograms.samhsa.gov/pdfs/model/TFCBT.pdf