Title: Hepatic function tests in babies with perinatal asphyxia: can it
advertisement

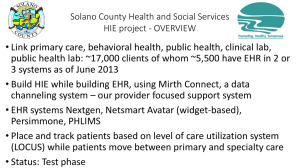
Title: Hepatic function tests in babies with perinatal asphyxia: can it predict hypoxic ischemic encephalopathy? Abstract Objective: Different organ systems of the body are affected in perinatal asphyxia. Here hepatic function was tested in full term appropriate for gestational age (AGA) newborn babies after perinatal asphyxia and its relation with severity of hypoxic ischaemic encephalopathy (HIE) was assessed. Study design: 62 full term AGA asphyxiated newborns as cases and 62 apparently healthy newborns as control group were studied. Serum glutamate pyruvate transaminase (SGPT), serum glutamate oxaloacetate transaminase (SGOT) ,alkaline phosphatase (ALP), gamma glutamyl transferase (GGT), total protein, albumin, total & direct bilirubin and prothrombin time were analyzed on 3rd day of life using validated methods and compared between two groups. Results Liver enzymes and prothrombin time is higher in cases compared to control group. SGPT,SGOT and P.time showed significant relation with severity of HIE. SGPT is most significantly related. Conclusion : Liver function tests specially SGPT can help in diagnosis of hepatic damage in perinatal asphyxia specially those having encephalopathy and also in retrospective diagnosis of perinatal asphyxia in those without availability of proper birth history. Key words: Perinatal asphyxia, Hepatic function tests, HIE (hypoxic ischemic encephalopathy). Introduction: Perinatal asphyxia (PNA) is a major cause of mortality and long term morbidity among newborn infants in developing countries like India. WHO (Organizaton, 1996) has defined perinatal asphyxia as “failure to initiate and sustain breathing at birth”. If lung expansion does not occur in the minutes after birth, a progressive cycle of hypoxia, hypercapnia and acidosis evolves. During hypoxia, series of protective mechanisms collectively called as ‘diving sea reflex’ attempt to redistribute available blood flow to some vital organs like brain, heart, and adrenals in preference to perfusion of the lungs, liver, kidneys, and intestine (Tarcan et al., 2007). Ultimately it results in serious organ damage and multiorgan failure. Central nervous system dysfunction associated with perinatal asphyxia is referred to as Hypoxic ischemic encephalopathy (HIE). HIE is of foremost concern in an asphyxiated neonate because of its potential to cause serious long-term neuromotor sequelae among survivors. The aim of our study is to determine the degree of hepatic damage in perinatal asphyxia and to relate the hepatic function changes with severity of HIE as determined by Sarnat and Sarnat staging. Materials and methods: Study Setting : A cross sectional study has been done in the Department Of Biochemistry and neonatal intensive care unit and nursery in the Department of Pediatric Medicine, R. G. Kar Medical College and Hospital, Kolkata between May 2012 to August 2013.Prior ethical permission was obtained from institutional ethical committee.A study group of 62 full term (37weeks to 42 weeks of gestational age) newborn babies having birth weight more than or equal to 2.5 kg(appropriate for gestational age) with perinatal asphyxia and another control group of 62 matched healthy newborns were studied. Their hepatic function tests were done from venous blood sample on day three of life and parameters were studied. Inclusion Criteria was any one or more than one of the following: ( 1) Apgar score less than or equal to 6 at 5 minutes after birth (2). History of delayed crying or not crying at all after birth. (3) History of failure to breathe spontaneously immediately after birth. (4) History of any resuscitation procedure needed to sustain life after birth. Exclusion Criterias were (1) newborn babies having birth weight less than 2.5kg both preterm and small for gestational age (2) Septicemia, (3) Suspected metabolic disease (4) Obvious congenital anomalies (5) History of any drug intake by mother which is known to cause hepatic function alteration. Methods of study of different parameters: SGPT estimation :(Mod.IFCC method) (Bergmeyer et al., 1986b). SGPT catalyses transfer of amino group between L-alanine and alpha-ketoglutarate to form pyruvate and glutamate. The pyruvate formed reacts with NADH in presence of lactate dehydrogenase to form NAD. The rate of oxidation of NADH to NAD is measured as a decrease in absorbance which is proportional to the SGPT activity in serum sample. SGOT estimation (Mod IFCC method): (Bergmeyer et al., 1986a) SGOT catalyses the transfer of amino group between L-aspartate and alpha keto glutarate to form oxaloacetate and glutamate. The oxaloacetate formed reacts with NADH in presence of malate dehydrogenase to form NAD. The rate of oxidation of NADH to NAD is measured as a decrease in absorbance which is proportional to the SGOT activity in serum. Alkaline phosphatase estimation: (Pnpp kinetic method) (McComb and Bowers, 1972, 1972) ALP in an alkaline pH hydrolyses para nitrophenylphosphate to form p-nitrophenol and phosphate. The rate of formation of p- nitrophenol is measured as an increase in absorbance which is proportional to the ALP activity in serum sample. Gamma Glutamyl Transferase estimation:(Carboxy substrate method) (Bergmeyer et al., 1986a) GGT catalyses the transfer of amino group between L-γ-glutamyl-3-carboxy-4 nitroanilide and glycyglycine to form L-γ-glutamylglycyglycine and 5-amino -2nitrobenzoate.Rate of its formation is measured as an increase in absorbance which is proportional to the GGT activity in the sample. Total protein (Biuret method ) (Gornall et al., 1949, Doumas, 1975) Proteins in an alkaline medium bind with cupric ions present in the biuret reagent to form a blue violet coloured complex. The intensity of colour formed is directly proportional to the amount of protein present in the sample. Albumin estimation (BCG method):(Doumas et al., 1971) Albumin binds with the dye Bromocresol Green to form a green coloured complex. The intensity of colour is directly proportional to the amount of albumin present in the sample. Total and direct bilirubin (by Diazo method) (Pearlman and Lee, 1974, Row, 1974) Bilirubin reacts with diazotized sulphanilic acid in acidic medium to form pink coloured azobilirubin with absorbance directly proportional to bilirubin concentration. Direct bilirubin being water soluble directly reacts in acidic medium. Indirect or unconjugated bilirubin is solubilised using a surfactant and then it reacts similar to direct bilirubin. Prothrombin time: (using tissue thromboplastin) (L, 1998, CLSI, 2008) Coagulation process is triggered by incubation of plasma with the optimal amount of thromboplastin and calcium. The time to formation of fibrin clot is then measured. Method: 1 part of sodium citrate solution (0.11mol/L or 3.2%) and 9 parts of venous blood is mixed carefully avoiding formation of foam. The specimen is centrifuged at 1500g for 15 minutes at room temperature.100 µl of supernatant is taken as sample. 200µl of reagent is prewarmed at 37°C in automated coagulation analyzer. Sample is also incubated for 1 minute at 37°C. Reagent is added to the sample and time of the automated coagulation analyzer is started. After the fibrin clot is formed it showed the time which is the prothrombin time. Instrument used were Centrifuge Machine (REMI R-8C, REMI COOLING CENTRIFUGE) Semi auto-analyser( ERBA Chem 5), autoanalyser (ERBA–Mannheim XL-600) and automated coagulation analyser (Sysmex CA-50 ). Calculation was done by independent‘t’ test, analysis of variance study, post hoc test (bonferroni ), logistic regression study and ROC curve analysis with the help of spss 17 software and medcalc software. Results: It has been found that SGPT,SGOT,ALP, GGT and P.time is significantly raised in cases compared to controls (p value ˂0.001) but no significant difference was found in case of total protein, albumin, total and direct bilirubin. By analysis of variance study,it was found that SGPT,SGOT is significantly raised with stages of HIE (p value˂0.001). P.time is also raised but less significantly than SGPT and SGOT (p value = 0.018)(Table 2 ). The relation of SGPT, SGPT and P.time between different stages of HIE has been more precisely detected by bonferroni test (Table3, Table 4 & Table 5). But in logistic regression analysis, only in SGPT, p is less than conventional 0.05 (Table 6) that is SGPT contributes significantly to the prediction of the dependent variable (HIE). In ROC curve analysis for SGPT, the area under the curve is 0.841 which is between 0.5 (discriminating power not better than chance) to 1.0 ( perfect discriminating power (Table7). From coordinates of the curve, it is being seen that if we take serum SGPT value as 72.5 IU/L as cut off value between cases with no hypoxic ischemic encephalopathy and encephalopathy , it has sensitivity of 84 % and specificity of (1.222) x100 =78 % (Table 8 ). Discussion In the neonatal intensive care unit one of the leading causes of neonatal morbidity and death is perinatal asphyxia. It often results in multiple organ dysfunction including hypoxicischemic encephalopathy (HIE) and the infants with moderate and severe HIE have higher risk of developing cerebral palsy (CP) and other long-term neurological sequel and may even cause early death .The multiple organ dysfunction phenomenon is mechanistically related to the ‘diving reflex’ , the reflex activated by asphyxia, consists of shunting of blood from the skin and splanchnic area to the heart, adrenal glands and brain, to protect these vital organs from hypoxic ischemic injury (Bocking et al., 1988, Peeters et al., 1979, Sheldon et al., 1979, Jensen et al., 1999). Thus, due to this, it is likely that each neonate with clinically detectable heart or brain dysfunction resulting from intrapartum asphyxia would already have dysfunction of one or more organs other than heart, brain or adrenal gland, particularly kidney and liver. In our study, 62 full term appropriate for gestational age (AGA) newborn babies with perinatal asphyxia fulfilling inclusion and exclusion criteria were chosen as cases and another 62 full term AGA apparently healthy matched newborns were chosen as controls. Birth weight ± SD of the study group was 2.80±0.27 Kg and that of the reference group was 2.75± 0.28 Kg (difference not significant as p value = 0.249). Among the 62 asphyxiated patients 18 (29.03%) babies did not develop encephalopathy, 16 babies (25.80% ) were in HIE Stage-I, 17 babies ( 27.41% ) in HIE Stage- II and 11 babies (17.74%) in HIE Stage-III. Mother’s mean age in case group was 24.26 ± 3.2 years and in control group was 23.26 ± 2.89years and there was no significant difference between these two groups (p value = 0.071). In all cases and controls, liver function tests were done on day 3 of life. Beckett gj et al in a study done in Edinburgh in 1989, showed no significant change in serum SGPT level during initial 24 hours period after birth with perinatal asphyxia, but after 24 hours, SGPT increased significantly (p<0.01) reaching peak median values of 2.1 times the upper limit of reference interval by 48 hrs postpartum (Beckett et al., 1989) The plasma half life of SGPT is ~ 48 hrs. In another study done by Martín-Ancel A et al, the Apgar scores at 1 and 5 minutes were the only perinatal factors related to the number of organs involved and the severity of involvement; the Apgar score at 5 minutes had the stronger independent association (MartinAncel et al., 1995). Any score lower than 7 is a sign that the baby needs medical attention. Considering these facts , study of LFT was done on 3 rd day of life in babies with 5 minute Apgar score of 6 or less . In our study, it has been seen that mean ± standard deviation of some liver function parameters like SGPT, SGOT, ALP, GGT and prothrombin time are higher in cases compared to control group (p value of ≤0.001)(Table 1). Serum total protein and albumin level were not statistically significantly related with stages of HIE. (p=0.934 and 0.258 respectively (Table 1). The value of SGPT , SGOT and P. time also showed significant rise with increasing severity of HIE as demonstrated by analysis of variance test and post hoc test .( showed ‘t’ values of ˂0.001, ˂0.001 and ˂0.005 respectively) (Table 2, Table 3, Table 4 & Table 5). SGPT is most significantly related as seen by logistic regression analysis (table 6). Now we determined the value of serum SGPT which can be used as a cut off value with highest sensitivity and specificity. SGPT value of 72.5 IU/L can be used as a cut off value (with a sensitivity 84% and specificity 78% to differentiate between babies without encephalopathy and with encephalopathy following perinatal asphyxia (Table 8). Similar results were obtained by Godambe et al .The mean SGPT levels was noted to increase from 35.3 ± 28.8 IU/L in mild asphyxia to 65.6 ± 33.2 IU/L in severe asphyxia (Godambe et al., 1997). Similar results were observed by other workers who noted a rise from 44 ± 61.9 IU/L in mild to 59.5 ± 108 IU/L in severe asphyxia (Saili A, 1990, Zanardo V, 1985, Beckett et al., 1989). Karlsson et al suggested that there was a correlation existing between the magnitude of elevation of SGPT, SGOT and the severity of the hypoxic event (Karlsson et al., 2006). In our study also significant rise was found in case of SGPT (p value˂0.001), SGOT (p value˂0.001) and prothrombin time (p value˂0.005) with severity of HIE (Table 2). In our study no difference was found between cases and controls in the values of serum total protein, albumin, serum total and direct bilirubin (Table 1). They also did not show statistically significant change with different stages of HIE (Table 2 ). But prothrombin time is significantly different between cases and controls (p value ˂0.001) (Table 1) and also has significant relation with stages of HIE (p value ˂0.005) (Table 2). Similarly, in one study, prothrombin index [PI =(mean p.time/patient’s prothrombin time) x 100%] was reduced in all grades of asphyxia (Godambe et al., 1997) and similar observations of altered liver dependent coagulation parameters were observed by others (Zanardo V, 1985, Bhargava et al., 1978, Dube et al., 1986). In the initial period of perinatal asphyxia, the blood flow to brain, heart and adrenal glands of the newborn is preserved at the expense of reduction of perfusion to kidneys, lungs, gastrointestinal tract, liver, spleen and skeletal muscles. In case of liver asphyxia, cell death occurs by necrosis or apoptosis. One of the earliest hepatocellular changes in hypoxia is the formation of plasma membrane protrusions called blebs. These early changes are reversible. Irreversible injury occurs when a plasma membrane bleb bursts, causing abrupt failure of the plasma membrane permeability barrier. There is collapse of all electrical and ionic gradients across the plasma membrane and release of intracellular enzymes and metabolites occur. There is leakage of cytoplasmic enzymes from cell, but minimal release of other enzymes. Thus necroinflammatory change in liver leads to release of SGOT and SGPT but not of mitochondrial isoenzyme of SGOT nor to release of ALP or GGT .This might be the cause of comparatively less increase of serum SGOT value than SGPT. In perinatal asphyxia also, rise in transaminases indicative of liver cell dysfunction is either due to hepatocyte necrosis or due to changes in cell permeability (Beckett GJ, 1986). The mechanism of release of membrane bound enzyme such as GGT and ALP into the circulation is less well understood. Serum albumin measurements are useful in assessing the chronicity and severity of liver disease. It is the most commonly used serum protein and is produced exclusively by liver .Hypoproteinemia is an imprecise index of the severity of liver damage due to the long life of serum protein (AP, 1979). In our study also, serum total protein and albumin levels were not statistically significantly related with stages of HIE. No significant difference was found in level of serum bilirubin between cases and controls and total serum bilirubin did not show statistically significant change with different stages of HIE. It is probably due to presence of physiological jaundice in newborns both in cases and controls. In our study P.time also is significantly different between cases and controls (p value ˂0.001) and also has significant relation with stages of HIE (p value ˂0.005). The prothrombin time (PT) measures of extrinsic pathway of coagulation. This test measures factors I (fibrinogen), II (prothrombin), V, VII, and X. Since all these factors are made in the liver; a prolonged PT often indicates the presence of significant liver disease. Perinatal asphyxia remains a cause of significant morbidity and mortality in newborns despite advances in knowledge of neonatal physiology and improvement in newborn rescucitation procedure. According to the literature, the incidence of HIE varies between 0.1-0.4% of births, with diagnosis being essentially clinical (Hughes and Newton, 1992). In addition to clinical features, some markers of birth asphyxia is necessary for proper monitoring and management. Radiological markers are helpful to some extent, but not always easily possible. Single or combination of biochemical markers may be helpful in this respect. They may help in knowing multiorgan involvement. Several biomarkers of birth asphyxia have been studied. Here we have studied different liver function parameters to see if their values are altered or not in case of perinatal asphyxia. In our study, it has been seen that value of SGPT, SGOT and P.time showed significant rise with increasing severity of HIE (showed ‘t’ values of ˂0.001, ˂0.001 and ˂0.005 respectively). SGPT is most significantly related as seen by logistic regression analysis. SGPT value of 72.5 IU/L can be used as a cut off value (with a sensitivity 84% and specificity 78%) to differentiate between babies without encephalopathy and with encephalopathy following perinatal asphyxia. We can conclude that the determination of serum SGPT could offer a routine and rapid laboratory test for establishing the presence of hepatic cellular damage following perinatal asphyxia. They may help in modification of ongoing treatment. It will also help in retrospective diagnosis of perinatal asphyxia mainly those leading to encephalopathy; especially in those newborns whose birth records are not available. References 1972. Recommendations of the German Society for Clinical Chemistry. Standardisation of methods for the estimation of enzyme activities in biological fluids. Experimental basis for the optimized standard conditions. Z Klin Chem Klin Biochem, 10, 281-91. AP, M. 1979. Laboratory assessment of hepatobiliary disease. Liver Disorders in Childhood. London: Butterworths. BECKETT GJ, H. J. 1986. Plasma Glutathione Stransferase measurements and Liver disease in Man. J Clin Biochem Nutr 11, 21-24. BECKETT, G. J., HUSSEY, A. J., LAING, I., HOWIE, A. F., HAYES, J. D., STRANGE, R. C., FAULDER, C. G. & HUME, R. 1989. Measurements of glutathione S-transferase B1 in plasma after birth asphyxia: an early indication of hepatocellular damage. Clin Chem, 35, 995-9. BERGMEYER, H. U., HORDER, M. & REJ, R. 1986a. International Federation of Clinical Chemistry (IFCC) Scientific Committee, Analytical Section: approved recommendation (1985) on IFCC methods for the measurement of catalytic concentration of enzymes. Part 2. IFCC method for aspartate aminotransferase (Laspartate: 2-oxoglutarate aminotransferase, EC 2.6.1.1). J Clin Chem Clin Biochem, 24, 497-510. BERGMEYER, H. U., HORDER, M. & REJ, R. 1986b. International Federation of Clinical Chemistry (IFCC) Scientific Committee, Analytical Section: approved recommendation (1985) on IFCC methods for the measurement of catalytic concentration of enzymes. Part 3. IFCC method for alanine aminotransferase (Lalanine: 2-oxoglutarate aminotransferase, EC 2.6.1.2). J Clin Chem Clin Biochem, 24, 481-95. BHARGAVA, M., BHARGAVA, S. K. & KUMARI, S. 1978. Impairment of platelet function in birth anoxia. Indian J Med Res, 68, 976-9. BOCKING, A. D., GAGNON, R., WHITE, S. E., HOMAN, J., MILNE, K. M. & RICHARDSON, B. S. 1988. Circulatory responses to prolonged hypoxemia in fetal sheep. Am J Obstet Gynecol, 159, 1418-24. CLSI 2008. Collection,Transport and Processing of Blood Specimens for Testing PlasmaBased Coagulation Assays and Molecular Hemostais Assays ;Approved Guideline. Fifth ed. Pennsylvania. DOUMAS, B. T. 1975. Standards for total serum protein assays--a collaborative study. Clin Chem, 21, 1159-66. DOUMAS, B. T., WATSON, W. A. & BIGGS, H. G. 1971. Albumin standards and the measurement of serum albumin with bromcresol green. Clin Chim Acta, 31, 87-96. DUBE, B., BHARGAVA, V., DUBE, R. K., DAS, B. K., ABROL, P. & KOLINDEWALA, J. K. 1986. Disseminated intravascular coagulation in neonatal period. Indian Pediatr, 23, 925-31. GODAMBE, S. V., UDANI, R. H., MALIK, S. & KANDALKAR, B. M. 1997. Hepatic profile in asphyxia neonatorum. Indian Pediatr, 34, 927-30. GORNALL, A. G., BARDAWILL, C. J. & DAVID, M. M. 1949. Determination of serum proteins by means of the biuret reaction. J Biol Chem, 177, 751-66. HUGHES, I. & NEWTON, R. 1992. Genetic aspects of cerebral palsy. Dev Med Child Neurol, 34, 80-6. JENSEN, A., GARNIER, Y. & BERGER, R. 1999. Dynamics of fetal circulatory responses to hypoxia and asphyxia. Eur J Obstet Gynecol Reprod Biol, 84, 155-72. KARLSSON, M., BLENNOW, M., NEMETH, A. & WINBLADH, B. 2006. Dynamics of hepatic enzyme activity following birth asphyxia. Acta Paediatr, 95, 1405-11. L, P. 1998. The Prothrombine Time. WHO/LAB/98.3. MARTIN-ANCEL, A., GARCIA-ALIX, A., GAYA, F., CABANAS, F., BURGUEROS, M. & QUERO, J. 1995. Multiple organ involvement in perinatal asphyxia. J Pediatr, 127, 786-93. MCCOMB, R. B. & BOWERS, G. N., JR. 1972. Study of optimum buffer conditions for measuring alkaline phosphatase activity in human serum. Clin Chem, 18, 97-104. ORGANIZATON, W. H. 1996. Perinatal mortality: a listing of available information. Geneva. PEARLMAN, F. C. & LEE, R. T. 1974. Detection and measurement of total bilirubin in serum, with use of surfactants as solubilizing agents. Clin Chem, 20, 447-53. PEETERS, L. L., SHELDON, R. E., JONES, M. D., JR., MAKOWSKI, E. L. & MESCHIA, G. 1979. Blood flow to fetal organs as a function of arterial oxygen content. Am J Obstet Gynecol, 135, 637-46. ROW, H. A. 1974. In: HENRY, R. J. (ed.) Clinical Chemistry:Principles and Techniques 2ed. SAILI A, S. M., GATHWALA G, KUMARI S, DUTTA AK 1990. Liver dysfunction in severe birth asphyxia. Indian Pediatr, 12, 1291-4. SHELDON, R. E., PEETERS, L. L., JONES, M. D., JR., MAKOWSKI, E. L. & MESCHIA, G. 1979. Redistribution of cardiac output and oxygen delivery in the hypoxemic fetal lamb. Am J Obstet Gynecol, 135, 1071-8. TARCAN, A., TIKER, F., GUVENIR, H. & GURAKAN, B. 2007. Hepatic involvement in perinatal asphyxia. J Matern Fetal Neonatal Med, 20, 407-10. ZANARDO V, B. M., PERINI GF 1985. Serum glutamic oxaloacetic transaminase and glutamic pyruvic transaminase activity in premature and full term asphyxiated newborns. Biol Neonate, 47, 61-69. Tables Table 1: Mean of different LFT parameters in birth asphyxia cases and controls and their comparison CONTROL CASE PARAMETER t value p value (Mean±SD) (Mean±SD) SGPT 37.12±16.80 100.85±50.14 9.488 ˂0.001 SGOT 70.69±32.65 147.90±68.79 7.983 ˂0.001 134.30±60.32 239.00±113.04 6.433 ˂0.001 GGT 71.53±29.60 116.45±57.0 5.505 ˂0.001 Total protein 6.03±1.22 5.68±1.14 -1.606 0.111 Albumin 3.34±0.74 3.39±0.80 0.364 0.716 Total bilirubin 7.81±2.90 6.90±3.28 1.644 0.103 Direct bilirubin 1.38±0.45 1.33±0.62 0.478 0.634 13.12±1.92 15.37±2.90 5.086 ˂0.001 Alkaline Phosphatase Prothrombin time Table 2: Relation of different LFT parameters with stages of HIE (by analysis of variance study) LFT parameters F value Significance(p value) SGPT 18.596 ˂0.001 SGOT 14.517 ˂0.001 ALP 1.752 0.166 GGT 1.189 0.322 TP 0.453 0.716 ALB 0.371 0.774 Total bilirubin 1.884 0.142 Direct bilirubin 1.062 0.372 P.time 3.616 0.018 Comparison with other Dependent Variable Stages of HIE stages Significance SGPT HIE Stage 1 0.896 HIE Stage 2 ˂.001 HIE Stage 3 ˂.001 HIE Stage 2 0.025 HIE Stage 1 with HIE Stage 3 ˂.001 HIE Stage 2 with HIE Stage 3 0.044 No encephalopathy with Table 3: Multiple comparison of serum SGPT levels between different stages of HIE by Post Hoc Test (Bonferroni) Table 4: Multiple comparison of serum SGOT between different stages of HIE by Post Hoc Test (Bonferroni) Table 5: Multiple comparison of Prothrombin time levels between different stages of HIE by Post Hoc Test (Bonferroni) Comparison Dependent Variable with other Stages of HIE stages Significance HIE Stage 1 1 HIE Stage 2 0.02 HIE Stage 3 0.287 HIE Stage 2 0.23 HIE Stage 3 1 HIE Stage 3 1 No encephalopathy P. time Comparison Dependent Variable with with other Stages of HIE stages Significance HIE Stage 1 with HIE Stage 1 1 HIE Stage 2 No HIE Stage 2 0.001 HIE Stage 3 ˂.001 HIE Stage 2 0.004 HIE Stage 3 ˂.001 with encephalopathy SGOT with HIE Stage 1 with by Logistic regression analysis HIE Stage 2 with Variable Table 6 : Coefficients and Standard Errors HIE Stage 3 0.408 Coefficient Std. Error P SGPT 0.028854 0.012839 0.0246 SGOT 0.010464 0.0086035 0.2239 P.Time 0.14155 0.13478 0.2936 Constant (-) 4.9089 Table 7 : ROC curve analysis and Area Under the Curve Test Result Variable(s):SGPT Asymptotic 95% Confidence Interval Area 0.841 Std. Error Asymptotic Sig. 0.055 0.000 Lower Bound Upper Bound 0.733 0.949 Table 8 : Coordinates of the Curve (Test Result Variable : SGPT) Positive if Greater Than Sensitivity 1 - Specificity 60 0.864 0.389 65.5 0.841 0.333 68 0.841 0.278 72.5 0.841 0.222 76 0.727 0.167 78.5 0.705 0.167 or Equal To 81 0.659 Figure: Figure 1: Pictorial presentation of ROC curve 0.167