Wt: 3.100kg - Ohio Neonatal Nutritionists

Induced Hypothermia
Nutritional considerations for infants undergoing induced hypothermia following acute perinatal hypoxic ischemia
Trayce Gardner, MEd, RD, CSP, LD
Presented at Fall ONN Meeting 2011
Columbus, Ohio
Hypoxic Ischemic Encephalopathy
(HIE)
Linked with high-risk of morbidity
(adverse neurological and developmental outcomes) and mortality
Principal cause for many cases of cerebral palsy
Definition of HIE
Any event that leads to a decreased oxygen and blood supply to the brain can result in hypoxic ischemic encephalopathy with both clinical and laboratory findings
Selway, L. D. State of Science Hypoxic Ischemic Encephalopathy and Hypothermic Intervention for Neonates.
Advances in Neonatal Care. 2010; Vol. 10, No.2: 60-66.
Long, M. and Brandon, D. Induced Hypothermia for Neonates With Hypoxic-Ischemic Encephalopathy. JOGNN.
2007; Vol.36, 3: 293-298
Conditions that can lead to HIE
Umbilical cord prolapse
Placental abruption
Acute blood loss
Uterine rupture
Phases of HIE
Initial insult
Conversion to anaerobic metabolism in the neonatal brain
Subsequent abnormal brain function
Accumulation of sodium, calcium, and water within the cells; potassium shifts out of the cells
Cell death as a result of free radical production and cell apoptosis
Secondary injury
Occurs 6 to15 hours following the initial event
Following resuscitation of the infant, the brain attempts to regain normal function
Mitochondrial function remains impaired; inflammatory response continues to promote injury
This is the time frame in which induced hypothermia is initiated to prevent reperfusion injury
Induced Hypothermic Therapy
Has been employed in clinical practice in the NICU setting since the late 1990s
Selective head cooling or total body cooling
Deep cooling
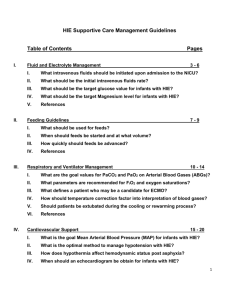
Nutritional Implications
“Optimizing nutrition is important when caring for a neonate with HIE but is complicated by compromised bowel perfusion.”
“Total parenteral nutrition is initiated and electrolytes carefully monitored.”
“Adequate protein intake is necessary for growth and repair…”
“The unit dietitian may aid the health care provider in reviewing the patient’s laboratory values and growth trends…”
Long, M. and Brandon, D. Induced Hypothermia for Neonates With Hypoxic-Ischemic Encephalopathy. JOGNN.
2007; Vol.36, 3: 293-298
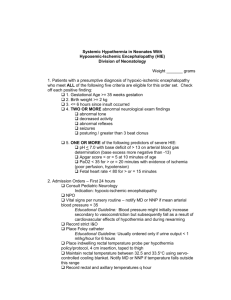
Induced hypothermia
Eligibility criteria
◦ Term or near term infant
Signs & symptoms of moderate to severe
HIE
Low 10 minute Apgar score
Low cord pH or postnatal blood pH <7.0
Severe metabolic acidosis (base deficit
>16)
HIE - Nutritional Considerations
Eligibility criteria
◦ Term or near term infant
S/S Moderate to Severe
HIE
Low 10 minute Apgar score
Low cord pH or postnatal blood pH <7.0
Severe metabolic acidosis (base deficit
>16)
Baby is term or near term
Need for close monitoring of TPN metabolic tolerance
Concern about gut perfusion
Possible low fluid/Cal needs early on – followed by high nutrition, low Cal needs later in life; need for ongoing nutrition followup
Case Study
Maternal History and Delivery
37 year old G3 P2 with history of hypertension and sleep apnea; chronic pain – on methadone.
Underwent emergency C/S due to bradycardia and NRFHT (non-reassuring fetal heart-rate tracing).
Case Study
Delivery
Infant had no heart rate initially; received chest compressions, intubation, and PPV (positive pressure ventilation) in the delivery room. No respiratory efforts until after moved to SCN (special care nursery)
Pupils dilated and nonreactive; UVC gas, pH 6.96 and base deficit of
25; UAC gas, pH 7.09 with base deficit 20
Blood glucose 119 mg/dL; Hematocrit 51%
Received NS (normal saline) bolus
Case Study
38-3/7 week infant, AGA, S/P HIE, transferred to NICU, cooling protocol initiated
BW: 3.25 kg
Length: 48 cm
Head Circumference: 34 cm
Case Study
DOL 1 – NPO (Cooling)
Fluids:
UVC: D10% with trophamine 2.5 g/kg and 1.5 mEq calcium/kg at 8.1 mL/hr
(60mL/kg/d)
UAC: ¼ Sodium Acetate at 0.5 ml/hr (3.7 mL/kg)
Initial neonatal EEG obtained pH 7.23, base deficit range 7-10
Case Study
DOL 2 (Cooling)
TPN order: 80 mL/kg/d; D10% with 3 g
Trophamine/kg/d and 1.5 g lipids/kg/d. 2 mEq Na Acetate/kg.
~51 kcal /kg/d
Base deficit 8
Case Study
DOL 3 (Cooling)
TPN order: 80 mL/kg/d; D10% with 3 g Trophamine/kg/d and 3 g lipids/kg/d.
~56 kcal /kg/d
Wt: 3.100kg (95% BW) Length 48 cm, HC 34 cm pH 7.39, base deficit 1, total protein 5.2 g/dL, albumin 2.9 g/dL, total bilirubin/direct bilirubin within normal limits
(WNL)
Case Study
DOL 4 (Rewarming)
TPN order: 80 mL/kg/d; D11% with 3 g
Trophamine/kg/d and 3 g lipids/kg/d.
~71 kcal /kg/d
Case Study
DOL 5
Ordered to PO (term infant formula) minimum of 20 mL/kg/d
Can advance to 40 mL/kg/d later in day pending readiness
TPN changed to D 9.5%, 1.5 g/kg
Trophamine; allowed lipids to run out
Case Study
Second EEG showed 20-30 second seizure activity and staring episodes
Phenobarbital started
Case Study
DOL 6
Infant continued on term infant formula; allowed to ad lib with minimum of 120 mL/kg/d
Took volumes of 30 – 58 mL per feeding during the day, then 37 – 60 mL later in evening
Met minimums and took closer to 152 mL/kg/d
Started multivitamin at 1 mL/d for 400 IU of vitamin D due to <500 mL of formula per day and initiation of Phenobarbital
Case Study
DOL 9
Continued to take 150+ mL/kg/d term infant formula
~100 kcal/kg/d, 2.1g pro/kg/d
Wt: 3.150 kg, Length 51 cm, HC 34.2
97% BW, gain of 7 g/d over past week and taking all po
Discharge
Home with mother
Follow-up with pediatrician and high-risk infant clinic