Formative evaluation of the Home Care Packages Programme
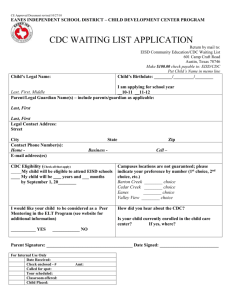
advertisement

Department of Social Services Formative evaluation of the Home Care Packages Programme Detailed findings report April 2015 Inherent Limitations This report has been prepared as outlined in the Introduction Section and Appendix A. The services provided in connection with this engagement comprise an advisory engagement, which is not subject to assurance or other standards issued by the Australian Auditing and Assurance Standards Board and, consequently no opinions or conclusions intended to convey assurance have been expressed. No warranty of completeness, accuracy or reliability is given in relation to the statements and representations made by, and the information and documentation provided by stakeholders consulted as part of the process. KPMG has indicated within this report the sources of the information provided. We have not sought to independently verify those sources unless otherwise noted within the report. KPMG is under no obligation in any circumstance to update this report, in either oral or written form, for events occurring after the report has been issued in final form. The findings in this report have been formed on the above basis. Third Party Reliance This report has been prepared at the request of the Department of Social Services in accordance with the terms of KPMG’s Official Order dated 7 April 2014 and the Deed of Variation dated 18 July 2014. Other than our responsibility to the Department of Social Services, neither KPMG nor any member or employee of KPMG undertakes responsibility arising in any way from reliance placed by a third party on this report. Any reliance placed is that party’s sole responsibility. Contents Glossary ................................................................................................................................ 6 Abbreviations ...................................................................................................................... 8 1 Introduction and purpose of this report ........................................................................... 9 1.1 Programme context and background....................................................................... 9 1.2 Evaluation framework ............................................................................................11 1. How effective has the implementation of the Home Care Packages Programme been? ......................................................................................................................................11 2. Are there any operational issues or possible adjustments needed?..........................12 1.3 Spectrum of CDC - service orientation ...................................................................12 1.4 Structure of this report...............................................................................................14 2 Implementation of the Home Care Packages Programme .............................................15 2.1 Programme implementation timing .........................................................................16 2.2 Implementation approach by the Department .........................................................16 2.3 Communication and support materials ...................................................................17 2.3.1 2.4 Effectiveness of support materials ...................................................................17 Assessment and referral processes .......................................................................21 2.5 Consumer care fees....................................................................................................23 2.6 Administration and case management fees.................................................................24 2.7 Implementing new administrative requirements ..........................................................26 Processing of subsidy claims by the Department of Human Services (Medicare) ..........26 Role of aged care advocacy services ............................................................................27 2.8 Interface with other services ...................................................................................27 2.9 Other issues relevant to the Programme implementation .......................................29 Dementia and cognition supplement .............................................................................30 2.10 3 Acceptance of programme change and commitment to CDC .................................31 Transitioning to consumer-directed care........................................................................31 Summary of key points: development of and transition to CDC .....................................32 Main considerations for providers in transition were: .....................................................32 3.1 Provider readiness for CDC....................................................................................32 3.1.1 Classifying providers’ level of CDC readiness .................................................34 3.1.2 Activities undertaken to prepare for CDC implementation ...............................35 Internally, activities included: .........................................................................................35 Strategy and approach ..................................................................................................36 Systems ........................................................................................................................37 Management and board commitment ............................................................................38 Staff commitment, skills and capabilities .......................................................................38 Culture and practice changes ........................................................................................38 3.1.3 Provider transition and readiness for CDC – key considerations .........................38 3.2 Transitioning existing consumers to CDC ...........................................................39 Process for transitioning existing consumers .................................................................41 Consumer experience of transition to CDC....................................................................42 3.3 Key transition considerations for providers .............................................................43 Transitioning ‘high cost’ consumers ...............................................................................43 Systems changes and costs ..........................................................................................44 Administrative and coordination costs ...........................................................................44 Embedding practice changes ........................................................................................46 Other considerations .....................................................................................................46 Survey results ...............................................................................................................47 4 Consumer-directed care in action ..................................................................................48 4.1 Consumer choice and control .................................................................................48 4.2 Rights .....................................................................................................................49 4.3 Respectful and balanced partnerships ...................................................................50 4.4 Participation ...........................................................................................................51 4.5 Wellness and re-enablement ..............................................................................51 4.6 Transparency .........................................................................................................53 4.7 Considerations for special needs groups ................................................................53 4.7.1 People from Aboriginal and Torres Strait Islander backgrounds ......................53 4.7.2 People from culturally and linguistically diverse backgrounds..........................54 4.7.3 People who live in rural or remote areas...............................................................55 4.7.4 People who are financially or socially disadvantaged ......................................55 4.7.5 Veterans ...............................................................................................................57 4.7.6 People who are homeless or at risk of becoming homeless..................................57 4.7.7 Care leavers .........................................................................................................57 4.7.8 Parents separated from their children by forced adoption or removal ...................58 4.7.9 Lesbian, gay, bisexual, transgender and intersex people......................................58 5 Considerations for strengthening and improving home care and CDC...........................60 5.1 Supporting providers to implement CDC ................................................................60 5.2 Strengthened focus on re-enablement and wellness ...................................................61 5.3 Clarifying the basic care interface ...............................................................................61 5.4 Increasing knowledge of CDC across key agencies and services ...............................61 5.5 Trialling new approaches for under-represented special needs groups .......................62 5.6 Improving assessment and the continuum of care ..................................................62 5.7 Increasing consumer control through self-directed funding and portability ..............63 Appendix A Evaluation methodology ..............................................................................64 Background ...................................................................................................................64 Objectives of the Home Care Packages Programme .....................................................64 Purpose of the formative evaluation ..............................................................................66 Evaluation questions .........................................................................................................66 1. How effective has the implementation of the Home Care Packages Programme (including CDC) been? ..................................................................................................66 2. Are there any operational issues or possible adjustments needed to strengthen the Home Care Packages Programme’s effectiveness in meeting its objectives? ...............66 Online survey for all Home Care Packages Programme home care providers ...............67 Review of de-identified Ministerial correspondence and Departmental communications67 Template report for Home Care Packages Programme providers delivering CDC places ......................................................................................................................................67 Evaluation governance and ethics .................................................................................72 Appendix B Provider survey – detailed tables .................................................................74 Appendix C Survey results: Implementation of the Home Care Packages Programme ........80 Appendix D Survey results: Transition to Consumer Directed Care ......................................85 Appendix E Survey results: Preparing for Consumer Directed Care .....................................89 Appendix F Summary of key service provider data: range and cost of supports delivered under CDC ...........................................................................................................................91 Range of supports accessed.............................................................................................91 In-house and brokered services ........................................................................................92 Appendix G Summary of key themes and issues from Ministerial and Departmental correspondence....................................................................................................................95 Analysis of Ministerial correspondence .............................................................................95 Analysis of Departmental telephone and email enquiries ..................................................96 Glossary Aged Care Assessment Programme Refers to the working arrangement between the Commonwealth and state and territory governments to operate Aged Care Assessment Teams (ACATs) or Aged Care Assessment Services (ACASs) across Australia. The core objective of this Programme is to assess the care needs of frail older people and to assist them to gain access to the most appropriate types of care, including approval for Commonwealth subsidised aged care services. Carer (or informal carer) In this report, refers to an unpaid person who helps a home care recipient with his or her activities of daily living. Care worker (or personal care worker, or direct care provider) In this report, refers to a paid person who helps a home care recipient with his or her activities of daily living, who may either be employed or sub-contracted (‘brokered’) by the recipient’s home care provider. Consumer A person who is receiving care and services under a Home Care Package funded by the Australian Government. In the Aged Care Act 1997, this person is referred to as a ‘care recipient’. Consumer directed care (CDC) An approach to the planning and management of care, which providers consumers and their carers power to influence the design and delivery of the services they receive, including what services are delivered, and where and when they are delivered. Commonwealth HACC Programme This Programme provides home and community care services for frail older people aged 65 years and over and Aboriginal and Torres Strait Islander people aged 50 years and over. The Commonwealth HACC programme does not currently apply in Victoria and Western Australia. Commonwealth Home Support Programme A programme commencing on 1 July 2015 in all states and territories except Victoria and Western Australia, which amalgamates the current Commonwealth HACC Programme with three other programmes providing basic support services for older people and their carers. Dementia and cognition supplement A supplement of 10 per cent to the daily home care subsidy payable for eligible consumers with dementia or cognitive impairments. Department Department of Social Services. Guidelines Refers to the Home Care Packages Programme Guidelines, July 2014, published by the Department of Social Services. Home care A type of aged care for which a home care subsidy is payable under Part 3.2 of the Aged Care Act 1997 and Aged Care (Transitional Provisions) Act 1997. Home Care Agreement An agreement entered into by a consumer and a home care Glossary provider outlining rights and responsibilities and what services will be provided to the consumer. Home Care Package A co-ordinated package of services tailored to meet a consumer’s specific care needs. Commonwealth subsidies under the package are paid to the provider at a fixed amount by care level. Home Care Packages Programme The Australian Government programme that provides a subsidy to home care providers to support people to remain living at home. Home care provider (or service provider, or provider) An organisation approved by the Department of Social Services under Part 2.1 of the Act as suitable to provide home care. In the Aged Care Act 1997, this person or body is referred to as an “approved provider”. Home Care Standards The Home Care Standards means the ‘Home Care Common Standards’, as set out in Schedule 4 to the Quality of Care Principles 2014. Home care subsidy (or subsidy) The subsidy payable to a home care provider by the Australian Government under Part 3.2 of the Aged Care Act 1997 and Aged Care (Transitional Provisions) Act 1997. Income assessment Refers to the means-testing conducted by the Department of Human Services (Centrelink) to determine whether an income tested care fee is payable by a consumer. Income tested care fee Refers to the fee a consumer may be asked to pay for their home care, based on an income assessment. Non-CDC package A Home Care Package that is not yet delivered on a CDC basis. From 1 July 2015, all Home Care Packages will be delivered on a CDC basis. Package (or place) A co-ordinated package of care and services tailored to meet the specific care needs of a consumer. Re-ablement (or reablement) The use of timely assessment and targeted interventions to assist people to maximise their independence, choice and quality of life and minimise support required – to enable people to actively participate and remain engaged in their communities. Also referred to as wellness or restorative approaches. Suspension Term used when a consumer takes a period of leave from their Home Care Package, and some or all services are suspended. Veterans’ supplement A supplement of 10 per cent to the daily home care subsidy payable for eligible consumers who are veterans. Abbreviations AACQA Australian Aged Care Quality Agency ACAP Aged Care Assessment Program ACAT Aged Care Assessment Team ACAS Aged Care Assessment Service ACCR Aged Care Client Record ACFA Aged Care Financing Authority ACQA Aged Care Quality Agency CACP Community Aged Care Packages CHSP Commonwealth Home Support Programme CDC Consumer-directed care DHS Department of Human Services DSS Department of Social Services DVA Department of Veterans’ Affairs EACH Extended Aged Care at Home EACHD Extended Aged Care at Home Dementia NACAP National Aged Care Advocacy Programme NDIS National Disability Insurance Scheme NRCP National Respite for Carers Programme 1 Introduction and purpose of this report Aged care reform in Australia has now been underway for a decade. As part of the Living Longer, Living Better reforms, the Australian Government announced the Commonwealth Home Care Packages Programme (the Programme) and implementation of Consumer Directed Care (CDC) by 1 July 2015. In April 2014, KPMG was engaged by the Department of Social Services (the Department) to conduct a formative evaluation of the implementation of the Programme, including the transition to a CDC model of aged care service delivery from 1 August 2013. The focus of a formative evaluation is the effectiveness of a programme’s implementation processes and structures (compared to a summative or outcomes evaluation, which focusses on the extent to which intended programme benefits have been achieved). Formative evaluations are usually conducted early in a programme’s life to assess the extent to which a programme is being implemented as intended, and to identify any areas where the programme could be strengthened or improved to better position it to deliver its intended outcomes and benefits. The purpose of this formative evaluation was to identify any operational issues or possible adjustments required to strengthen the Programme’s effectiveness, and to ensure the successful and complete conversion of all home care packages to CDC by 1 July 2015, as well as any longer-term policy considerations. The evaluation was conducted between April 2014 and February 2015, with core data collection activities occurring from November 2014 to January 2015. Data collection activities relating to consumers and carers were reviewed and approved by the Bellberry Human Research Ethics Committee in August 2014 in accordance with the National Statement on Ethical Conduct in Human Research (2007). The evaluation reported to the Department and an advisory committee of the National Aged Care Alliance (NACA). This report provides the detailed key findings from the formative evaluation, and identifies areas for consideration to strengthen or improve the Programme. 1.1 Programme context and background Home-based aged care services in Australia were significantly reformed in August 2013, with the allocation of almost 6,000 home care packages (also referred to as home care places) under the 4level Home Care Packages Programme, and the conversion of around 60,000 former Community Aged Care Packages (CACP), Extended Aged Care at Home (EACH) packages and Extended Aged Care at Home Dementia (EACHD) packages to the new care levels. The care level structure is as follows: • Home Care Level 1 – to support people with basic care needs (this care level did not exist prior to August 2013); • Home Care Level 2 – to support people with low level care needs (equivalent to the former CACP places); • Home Care Level 3 – to support people with intermediate care needs (this care level did not exist prior to August 2013); • Home Care Level 4 – to support people with high care needs (equivalent to the former EACH and EACHD places). Several new supplements were also introduced (including the dementia and cognition supplement), that can be applied at any care level. The Programme aims to provide a tailored, co-ordinated package of services that meet an individual’s specific care needs, thus assisting care recipients to stay living in their own home and providing them with choice and flexibility in the way the care and support is delivered. To facilitate choice and flexibility, all new packages allocated since August 2013 are delivered under CDC arrangements (that is, the 5,835 packages allocated in August 2013, and an additional 6,653 packages allocated in December 2014). Around 1,000 existing CDC packages, which had formed part of the CDC pilot in 2010-12, have also continued under the new Programme. By 1 July 2015, all remaining home care packages must convert to CDC arrangements. Over the past 18 months most providers have been gradually transitioning their existing consumers to CDC arrangements as part of their regularly scheduled reviews. Under CDC consumers have an individualised care plan and budget with providers holding and administering the budget on the consumer’s behalf. Commonwealth subsidies for care and services are paid to the provider at a fixed amount by care level. The consumer receives a monthly statement from the provider that itemises income (i.e. Commonwealth subsidies and supplements, plus consumer fees and any additional consumer contributions) against expenditure showing unexpended funds in their individualised budget. The introduction of CDC to all home care packages on 1 July 2015 is prompting all providers to reorient their business and review key elements of their organisation, including the organisational culture, staff training needs and administrative systems. Implementation of these arrangements has coincided with other aged care reforms, including the introduction in October 2013 of a new online system for home care providers to submit aged care subsidy claims to Medicare/Department of Human Services, and the introduction of income tested care fees for new home care consumers from July 2014. A number of other social service reforms have also occurred during this period, including changes to residential aged care; commencement of design of the Commonwealth Home Support Programme (CHSP) ; development of the aged care gateway (My Aged Care); and implementation of the National Disability Insurance Scheme (NDIS) at various national trial sites. Many home care providers are also providers of residential aged care, home support and/or disability support services, and have been involved in these other reform activities at the same time as they have been implementing home care packages and CDC. 1.2 Evaluation framework An evaluation framework was developed in May 2014 to guide the data collection activities and to provide the data analysis and reporting approach for the evaluation. Figure 1 below shows the Programme results logic developed for the evaluation. Figure 1: Results logic for the Commonwealth Home Care Packages Programme The framework identified the following evaluation questions: 1. How effective has the implementation of the Home Care Packages Programme been? This involves consideration of the following: How well are the new arrangements working for home care providers and ACATs? This includes processes for implementing home care places, and the development and transition to CDC models of service delivery (including different models of CDC); effectiveness of the new care level structure and assessment processes; effectiveness of the intended graduated continuum of care between care levels; effectiveness of the programme guidelines and information processes; and considerations for different types of providers. How well are the new arrangements working for consumers? This includes understanding the range of care and services being accessed (including use of brokered services); application and impact of fees; consumer perceptions of choice and control; consumer engagement with individualised budgets and financial statements; effectiveness of information and advocacy services; and considerations for special needs groups. How well are the new arrangements working for the aged care system? This includes the interface with other aged care services such as the current Commonwealth HACC Programme (Commonwealth Home Support Programme from 1 July 2015); effects of the new arrangements on consumer demand and expectations; waiting times; and provider capacity and capability. 2. Are there any operational issues or possible adjustments needed? This involves consideration of the following: • • Are there any specific aspects of the Programme that could be strengthened or improved to support the conversion of all home care places to CDC by 1 July 2015? Are there any other aspects of the overall Programme that could be strengthened or improved to meet its objectives? The framework also sets out the methodological considerations for the evaluation, including principles for conduct of the evaluation, issues and challenges to be managed, and the evaluation governance arrangements. Further detail on the evaluation methodology and data collection methods is at Appendix A of this report. 1.3 Spectrum of CDC - service orientation In this report, the concept of a spectrum of CDC orientation is used to describe and differentiate the relative position of different providers in terms of the extent to which their service delivery is more or less consumer-directed. Figure 2 below illustrates this spectrum. Figure 2: Spectrum of consumer-direction in home care Source: KPMG Where providers are less advanced in the implementation of CDC, services are primarily ‘providerdirected’, with providers acting as care coordinators who make decisions about what supports will be delivered to consumers based on their assessment of need, and their allocation from a centralised funding pool. Further along the spectrum, providers are more ‘person-centred’ in their approach acting as case managers, using individualised assessment (which may include self-assessment tools) and actively involving consumers in the planning of supports and offering them some level of choice over which supports they use. This however may be limited to a menu of available options with some level of control over when, how and by whom supports are delivered. Providers ask consumers about their preferences and seek to coordinate service delivery in response. Where consumers are less able to clearly express their preferences (i.e. those with dementia or cognitive impairment, and/or who are non-verbal), providers will seek to understand and respect the consumers’ lifelong habits and preferences, often through discussions with the person’s family or carers. This may or may not include an indivdualised budget for which the provider is accountable to the consumer. At the other end of the spectrum where providers are more advanced in the implementation of CDC, providers act more as care facilitators or care partners, assisting consumers to self-identify goals and develop a tailored package of individualised care and supports to achieve those goals. Consumers have choice and control over all aspects of service delivery, with an individualised budget. The provider may or may not hold the funds. 1.4 Structure of this report This report presents the detailed findings from the evaluation. This report is structured as follows: • Chapter 2 considers the effectiveness of programme implementation processes. • Chapter 3 looks at the development of and transition to a consumer-directed model of service delivery, focussing on home care provider readiness. • Chapter 4 examines the operation of CDC in action. • Chapter 5 identifies considerations for strengthening and improving home care packages and CDC. • The appendices set out the evaluation methodology and detailed data. 2 Implementation of the Home Care Packages Programme This chapter considers the effectiveness of the implementation of the Programme. The chapter articulates the implementation planning undertaken by the Department then highlights key challenges and considerations that have impacted implementation. It is focussed on the experiences of home care providers and the wider aged care sector, including Aged Care Assessment Teams (ACATs), also known as Aged Care Assessment Services (ACASs). These findings were drawn from interviews with 25 home care providers (primarily managers and care coordinators), 13 ACATs/ACASs across 10 aged care planning regions nationally, 14 aged care sector stakeholder groups and the results from a national online survey completed by 29 per cent of home care providers in December 2014. This information was supplemented with interviews conducted with 57 consumers and carers nationally. Summary of key points: programme implementation • Overall, the majority of providers considered that the implementation of home care packages has gone well. – The new care level structure is supported and providers consider that it is a simpler system that is easier to explain to consumers. The availability of supplements is also strongly supported as a simple, fair model of meeting additional care needs. – The transition from CACP/EACH to Level 2 and Level 4 has been more or less seamless, and this was confirmed in the consumer and carer interviews. – The introduction of Level 3 is widely supported by providers, ACATs/ACASs and other stakeholders. • However, several factors have impeded the smooth implementation of the Programme, notably: timeliness of advice and communications; the subsidy claiming processes; and access to the dementia and cognition supplement. • There have been some concerns raised regarding the interface between home care Level 1 and HACC/CHSP basic support services; this may be resolved as the CHSP implementation is progressed. • There are concerns regarding the potential impact of income tested care fees on occupancy of places, as it is has been anecdotally observed that some part-pensioners and self-funded retirees are declining subsidised home care, but this has not yet been validated by data. • Providers report that they have experienced considerable administrative costs associated with the implementation. • There is some inherent reluctance to implement CDC due to concerns regarding resourcing and costs; required changes to business models; and the perceived capacity of CDC models to respond effectively to special needs groups. • Stakeholders also suggested that leave (suspension) rules are too complicated, that ACAR allocation processes do not meet the needs of some vulnerable communities, and that the distribution of care level places may not be supporting a continuum of care for consumers. 2.1 Programme implementation timing The timetable for implementation of the Programme was announced in November 2012. Implementation commenced from 1 August 2013, with the new 4-level home care framework and broadbanded ACAP assessment framework, and the allocation of all new packages on a CDC basis. A date was set for the conversion of all existing home care places to CDC by 1 July 2015. In July 2014, income tested fees for home care consumers were introduced (additional to the existing basic care fee). 2.2 Implementation approach by the Department The Department undertook a number of activities to support programme implementation. These activities were coordinated as part of the wider Living Longer, Living Better reform processes, which were coordinated from a centralised project management team in Canberra. The centrepiece of these activities was a high-profile national campaign which addressed the raft of Living Longer, Living Better reforms, including the home care changes, and which was timed to align with the launch of MyAgedCare. The ‘Let’s talk about aged care’ campaign included mass media and ethnic media advertisements, brochures, posters, online stories and videos. A series of national Aged Care Reform Roadshows were also conducted between March and June 2014 held in all capital cities and several regional locations. In addition, the Department provided regular newsletters to service providers (of which there have been 11 issues released between September 2014 and February 2015), regular direct electronic communications with providers (of which there have been more than 40 releases since July 2014), and access to email-based support for providers seeking clarification of the guidelines. The Department also provides a regular newsletter for ACATs and ACASs (of which there were two issues in 2014), and the Aged Care Assessment Programme Guidelines were revised in January 2014. During this period the Department consulted extensively and regularly with the sector to discuss implementation, notably through the National Aged Care Alliance (NACA), a representative body of peak national organisations in aged care, including consumer groups, providers, unions and health professionals. The 2013 programme guidelines were co-designed by NACA and the Department, with NACA leading the development. This was the first time the Department had engaged in such a co-design process, rather than consultation process, and flagged the Department’s intention that the move to CDC would also align with a move away from prescriptive regulation and oversight of the sector towards a more consumer-driven market. 2.3 Communication and support materials A range of support materials and activities were available to support programme implementation. The first version Home Care Packages Programme Guidelines were published by the Department on its website in August 2013. These were revised twice in July 2014. A series of fact sheets about the changes were also published on the Department’s website (https://www.dss.gov.au/our-responsibilities/ageing-and-aged-care/aged-care-reform/home-carepackages), aimed at home care service providers as well as consumers and carers, and on the MyAgedCare website (http://www.myagedcare.gov.au/help-home/) which was established as the national aged care entry point for consumers and carers in July 2013. A multi-platform advertising campaign was conducted advising consumers and carers about aged care reform, including but not limited to home care. COTA (formerly known as Council on the Ageing), the national peak body for older consumers, received Australian Government funding for its Home Care Today initiative which supports the implementation of the Home Care Packages Programme (and specifically the transition to CDC) with resources, advice and training for consumers and providers. The website (http://homecaretoday.org.au/) includes a range of resources including brochures for consumers and carers explaining CDC and templates for home care providers. The two aged care provider peak bodies, Aged and Community Services Australia (ACSA) and Leading Age Services Australia (LASA), also provide support services to their members. At the time of writing this report, Commonwealth funding for Home Care Today had been extended to the 2017-2018 financial year. 2.3.1 Effectiveness of support materials Interviews conducted for the evaluation indicated that there were variable views amongst providers and peak bodies on the effectiveness of support materials. This variability primarily related to where the provider is at with implementation of CDC, including their understanding of and experience with CDC practice. This was not influenced by provider size, type or location. The interviews indicated that: • Those providers that were further progressed in the implementation of CDC indicated that the materials were useful, although few made use of all of the available materials. The Programme guidelines, and the COTA, ACSA and LASA materials, were cited as the most useful materials. • Those that were less advanced in the implementation of CDC were often critical of the available material. They wanted more face-to-face support and collaboration with other providers rather than more written support, including increased direct access to the Department via a helpline for assistance in interpreting the guidelines (rather than via a generic email address), with clarification and examples of what was ‘in’ and ‘out’. It was evident that many providers – generally those that were more critical of the support materials – wanted more direction. They suggested that the guidelines did not offer sufficient clarity and ‘leaving too much open to interpretation’. A review of Ministerial correspondence and Departmental enquiries from providers conducted for this evaluation also found that the vast majority of enquiries related to matters of interpretation of the guidelines. Most providers expressed qualified support for the concept of CDC, accepting that CDC was ‘the way things are going’ but raised concerns as to their ‘duty of care’. These concerns were particularly in relation to frail or cognitively impaired consumers, those without family carers, or where there may be elder abuse. Such instances were often cited as a rationale for providers needing to have clear authority to restrict consumer choice and control. Although the guidelines (and messages from the Department and government) openly support consumer choice and control, these providers were worried as to whether the aged care regulatory framework was aligned to the changed policy environment – the concern being that providers do not want to be the subject of test litigation as to whether they breached a duty of care. Similar concerns were raised as to how the Australian Aged Care Quality Agency (AACQA) would interpret choice and flexibility during a provider’s quality review. The general consensus from the interviews was that it would be beneficial for providers to have more information and guidance as to how AACQA will assess performance against the Home Care Standards in the context of CDC. Most home care providers interviewed for the evaluation considered that they had sufficient information on the new arrangements from August 2013. This was substantiated by the results of the online survey conducted for this evaluation, which was completed by 29 per cent of providers. The majority of survey respondents indicated that they had sufficient information in relation to most aspects of the implementation although they would have valued more support in some areas. This related to income assessed care fees (47 per cent of respondents), access to the veterans’ supplement; oxygen and enteral feeding supplements (42 per cent) and broadbanded ACAT assessments (36 per cent of respondents). Table 1: Did this service have adequate information and support about the new arrangement prior to the transition to Home Care Packages by August 2013? Yes, we have had adequate information and support about this We have had enough information, but some support would have been helpful No, we have not had enough information or support Total responses to this question Percentage Percentage Percentage Number New package levels 1 and 3 27 51 22 143 Transition of CACP to level 2 37 49 14 152 Transition of EACH to level 4 35 49 16 136 Included care and services 35 45 20 147 Excluded care and services 28 46 26 144 Broadbanded assessments 25 39 36 148 Transition between care levels 26 45 29 149 Dementia supplement 18 49 33 149 Veterans' supplement 19 39 42 147 Yes, we have had adequate information and support about this We have had enough information, but some support would have been helpful No, we have not had enough information or support Total responses to this question Oxygen/enteral feeding supplements 20 40 40 148 Consumer fees policy 16 37 47 151 Source: KPMG analysis of provider survey data Survey respondents identified the Programme guidelines to be the most effective resource for implementing the Programme: 30 per cent of respondents said this resource provided effective information and support, and 63 per cent said it provided somewhat effective information and support but could be improved. Other resources that providers found to be somewhat effective were Australian Government websites (56 per cent) and email circulars (55 per cent). Table 2: How effective has this service found the resources that support the Home Care Package Programme? Please select one response. This resource has provided us with effective information and support This resource has been somewhat effective for us, but it could be improved Percentage Percentage This resource has not been effective for us Percentage We have not used this resource Percentage Total responses Number Home Care Packages Guidelines 30 63 5 2 152 Australian Government aged care reform roadshows 11 44 27 18 148 Australian Government reform readiness checklist 11 46 24 19 150 Australia Government fees booklet 13 39 27 21 150 Australian Government websites 16 56 26 2 151 Australian Government email circulars to providers 20 55 22 3 150 Support from Aged and Community Services Australia 29 32 21 18 148 Support from the National Aged Care Alliance 13 31 26 29 150 Support from Leading Age Service Australia 16 33 19 32 148 9 23 25 43 148 21 41 19 19 150 Support From the National Aged Care Advocacy Service Support from Home Care Today Source: KPMG analysis of provider survey data In contrast to providers, ACATs and ACASs almost universally did not feel they had sufficient information or support on the changes, and were concerned with regard to the accuracy of the information they received (particularly in relation to income tested care fees). ACATs/ACASs considered that they had not been provided with sufficient information about how CDC packages operate in practice, and how individualised budgets translate into ‘hours of care’ (which is how they are accustomed to assessing consumers’ level of need). This has resulted in ACATs/ACASs sometimes erring on the side of caution and approving a consumer for a higher care level where there were any doubts as to whether they might receive an adequate volume of care. 2.4 Assessment and referral processes Most stakeholders welcomed the more streamlined assessment processes. Many suggested that changes could go further, with a single non-lapsing eligibility assessment on entry and no requirement for a new assessment to move between the broadbanded low and high care levels (i.e. this could be determined by providers, in accordance with the guidelines and possibly using mandated assessment tools if necessary). A suggested alternative was for the re-assessment to be optional at the request of either the provider or consumer where it was unclear (or where there was disagreement) about whether a move to high care was required. At interview providers routinely reported no change in waiting time for ACAT assessments. There had been a change in waiting times to commence a package in some areas: waiting times for Level 1 and in some cases Level 2 have reduced and waiting times for Level 4 have increased. This was verified through the provider survey, where the majority of respondents reported that waiting times had not been affected (positively or negatively) by the new arrangements. Issues were raised regarding the current ACAT/ACAS assessment process. Most providers were critical, to varying extents, about what they perceive as a lack of training for and knowledge by ACATs/ACASs in relation to the changes. There were concerns that some ACATs/ACASs were too prescriptive in their assessments, for example specifying a Level 2 package, or providing incorrect or inadequate information to consumers about income assessments, fees and the ‘number of hours’ that would be available to them rather than the subsidy amount of an individualised budget. Some providers reported that ACATs/ACASs were giving opinions to consumers as to the fairness of certain providers’ prices, and/or suggesting that consumers utilise HACC instead of home care due to its affordability, which the providers considered to be unfair and inappropriate. Changes to ACAT and ACAS referral processes have occurred where the implementation of the Home Care Packages Programme has coincided with changes to internal ACAT and ACAS processes and structures. These processes are not consistent across Australia as the guidelines specifically allow for referral processes to be determined by local ACATs and ACASs. In some areas, particularly rural areas, ACATs and ACASs have either referred consumers directly to a provider or given notification of a new assessment to all providers. Some ACATs and ACASs have now changed their processes, and either provide a list of providers to consumers or refer them to the MyAgedCare website. Consumer and carers interviewed for the evaluation had variable experiences of assessment, with 18 of the 57 interviewees reporting that the ACAT/ACAS assessment was positive, person-centred and comprehensive. The remaining interviewees indicated that they felt ‘over-assessed’ or that their needs had not been sufficiently taken into account. There were no obvious response patterns with regard to jurisdiction, region or special needs groups. Despite a relatively high-profile media communications campaign in the months prior to the interviews for this evaluation, few consumers or carers were aware of MyAgedCare. Several younger carers had used the website and found it to be helpful though often an incomplete resource (in terms of local content). Most consumers and carers tended to come into contact with home care after a health crisis, such as hospitalisation after a fall, and were referred for ACAT/ACAS assessment through the hospital. Most consumers and carers indicated that they preferred to access information, particularly at the time of initial ACAT/ACAS assessment and entry to home care (or at the time of transition from CACP, EACH or EACHD to a CDC package), through some form of face-to-face process. Many consumers referred to ‘paperwork’ as something they filed for safekeeping but seldom read. Although most consumers and carers considered that the ACAT and provider assessment processes were timely, relatively straight-forward and comprehensive, some described them as repetitive, having to repeat their stories multiple times. Male consumers tended to find these processes more frustrating than females (this was the only area where there were notable gender differences in the interview responses). Some consumers and carers, particularly those undergoing assessments during or immediately following a health crisis, did not consider that the assessment process was person-centred and several reported that they felt pressured into accepting a package with a particular provider before they had time to think about what they wanted. Some examples of consumer and carer experiences with assessment, drawn from the evaluation interviews, are described below. Some consumer and carer perspectives on assessment (real names not used) Paul cares for his wife, who has dementia. She was hospitalised in early 2014 and the clinicians suggested that they should be assessed for a home care package. Paul found the ACAT assessment to be thorough, but on top of various geriatric and rehabilitation assessments, and assessment for respite care, it was exhausting. Following the ACAT approval, Paul was dismayed to experience a further assessment by the home care provider. ‘I’m bloody over it’, is how he describes it. He feels that he has had to repeat the same information over and over, and is surprised at how poor the communication seems to be between services. Paul is very pleased with the package now that services have commenced, and hopes not to have another assessment process for some time to come. Linda is a retired nurse and looks after her mother, a war widow who lives on her own. Linda’s mother was receiving Veterans’ Home Care services but Linda felt that these were no longer meeting her needs. She undertook some research into the offerings of local home care providers and then approached the ACAT. She found the ACAT to be very helpful, providing her with advice and information. This led to an assessment, which Linda said was thorough and took account of her mother’s wishes as well as her capacity as a carer. The ACAT provided them with written information and advice. Linda was soon able to access a Level 2 place with her preferred provider. Susan works full-time and cares for her invalid husband as well as her father, who has dementia and lives with them. About 18 months ago, her father was hospitalised after a serious fall. Her husband was in hospital at the same time and so it was a stressful time. She has little recollection of the assessment. She was given pamphlets which she did not really understand and felt that no-one was taking the time to talk to her, or giving her time to think. She felt ‘pressurised’ into accepting the first available place, and ‘threatened’ that if she did not accept it she would have to put her father into residential care. Things did not improve when the package commenced, as she felt that she was told what services could be provided and when they would be delivered, even though it was a CDC package. After several disputes with the home care provider, she recently cancelled the package and is thinking about what to do next. 2.5 Consumer care fees Introduction of income tested fees for consumers from July 2014 presented challenges for providers. The majority of providers indicated that there had not been enough information provided prior to the commencement of this policy (to providers, ACATs or consumers). There were concerns raised regarding the assessment process being too complex for consumers, and taking too long – up to three months in some cases. The retrospective application of the fees was problematic for many providers (especially smaller providers), as it often came as a shock to consumers and in some cases resulted in them cancelling their packages, and sometimes refusing to pay the retrospective fees for the period that they had already received services. A small number of providers pre-empted this issue by giving the consumer an estimate of their income-assessed fees using the MyAgedCare calculator and/or their own ready reckoners and charging interim care fees. Ten of the 25 providers interviewed reported that some consumers were declining packages as a result of the income tested fees, which was considered to be particularly problematic for Level 1 packages. It was reported that these consumers turned instead to HACC services to meet their needs, where they could obtain similar levels of service for lower fees, or to private services (often through the same provider as the one offering the subsidised home care package), or decided not to have any home care services at all. This raised a number of concerns for providers, specifically: • Provider income flow – some providers with Level 1 and Level 2 packages reported that they were becoming difficult to fill, and/or those located in areas with more self-funded retirees and part-pensioners who would be more likely to have to pay income tested fees • The quality of care that consumers may be receiving from private providers who may not be subject to the Home Care Standards and the scrutiny of the AACQA • The potential for consumers’ health to deteriorate, making them more likely to present to hospital or required a higher level of home care or residential care. Some not-for-profit providers (generally faith-based providers) do not have a strong history of collecting basic care fees and have historically waived or reduced fees for many or even most of their consumers. The providers who were interviewed for the evaluation reported that long-time employees of these organisations often see themselves as providing a benevolent community service to vulnerable older people and can resent having to collect user fees (these employees are also likely to be those struggling with the move to CDC). Some of these providers were concerned that consumers might ‘blame’ providers for the government’s policies. On the other hand, a number of providers – including several faith based not-for-profits – had accepted and supported the reality of means-tested contributions to care. These providers were more likely to be delivering other forms of community services in addition to home care (thus having prior exposure to user fees policies), and had often undertaken specific cultural change training with their staff which included addressing attitudes to user fees and collection of fees within a valuesbased, not-for-profit service environment Only one consumer interviewed for the evaluation was subject to income tested care fees, and they felt that the fees were reasonable. A number of consumers interviewed indicated that they were paying a basic care fee, and most of them considered that the fees were fair for the services they received. 2.6 Administration and case management fees The issue of administration and case management fees was frequently raised during the consultations. Many providers have faced challenges in pricing these components, with some wanting the government to provide guidance on what was a ‘fair and reasonable’ price to charge for administration and case management. Although the guidelines clearly separate administration and case management, a small minority of providers indicated some confusion about the difference between the two. The survey showed that the average proportion of a home care budget for administration and case management combined (across all care levels) was 27 per cent of the total subsidy. The proportions were slightly higher for the lower care levels, as demonstrated in the table below. Table 3: Average case management and administration fees Home care level Average case management fee (per week) Average administration fee (per week Maximum baseline subsidy (per week) Proportion of subsidy spent on case management & administration Level 1 $23.81 $20.14 $150.01 29% Level 2 $40.72 $36.55 $272.93 28% Level 3 $96.41 $79.81 $600.11 29% Level 4 $90.08 $99.00 $912.24 21% Source: KPMG analysis of survey results Note average case management and administration fees are based on the median fees reported by providers completing the data collection template (n=77) and exclude any additional supplements and consumer fees received. The way in which providers structured their administration and case management fees differed considerably, with most charging between 20 and 30 per cent for administration, usually with a ‘built in’ amount for required case management (care planning, reviews, an allowance for monthly contacts) and then an hourly fee for additional case management services. Some providers incorporated these built in costs to their administration fee rather than charging additional case management fees. Approximately half of the providers interviewed reported that they had undertaken some form of detailed cost modelling to develop these structures; whilst others (usually those charging at the lower end) set the fees based on what they thought was ‘fair’. A snapshot of different administration and case management pricing structures is set out over the page. Snapshot of some administration and case management pricing structures Provider 1 (rural, medium not-for-profit): Charges 15 per cent administration fee and no additional case management charges. Provider 2 (metro, large for-profit): Charges a 30 per cent administration and case management fee across all care levels (this can be reduced to a 20 per cent for administration only where consumer takes on responsibility for scheduling). Provider 3 (metro and rural, large not-for-profit): Charges a 10 per cent administration fee, plus a $50 invoicing and statement fee per month, plus case management charged at an hourly rate on a case-by-case basis. Provider 4 (metro, small for-profit): Charges a 20 per cent administration fee, plus case management charged at an hourly rate on a case-by-case basis. Provider 5 (metro, large not-for-profit): Charges a 25 per cent administration fee, plus case management and an hourly rate. Provider 6 (rural, small not-for-profit): Charges a 19 per cent administration fee, plus an 8 per cent case management fee across all care levels. Provider 7 (metro and rural, medium not-for-profit): Charges a 30 per cent administration fee, plus a tiered case management fee: the first tier varies between 5 per cent and 17 per cent depending on the care level and incorporates initial assessment and planning, six monthly reviews, and up to one hour of monthly contacts; the second tier is an hourly rate for any additional case management and advisory services in excess of the allowed number of contacts. Provider 8 (rural, small not-for-profit): Charges a 25 per cent administration fee, plus an initial flat fee for setup/establishment case management, plus additional case management charged at an hourly rate on a Snapshot of some administration and case management pricing structures case-by-case basis. A number of consumers and carers indicated that they were confused about how these fees were calculated. A few felt that the fees were excessive for what they understood the fees covered. Where consumers (and especially carers) took particular exception to these fees was where they had taken on what they considered was a significant degree of self-management and felt that the fees should have been reduced accordingly. 2.7 Implementing new administrative requirements Results of the online survey suggest that providers believe they have experienced a considerable increase in administrative activity through the introduction of the Home Care Packages Programme (61 per cent of respondents strongly agreed with the statement that ‘The Home Care Packages Programme has increased the administrative burden on providers’, with 23 per cent agreeing). At interview all providers indicated that there had been a substantial financial and administrative burden associated with the implementation, which exceeded their anticipated costs. This included the expected transitional costs of information technology upgrades, staff training, development of new processes and materials, and consumer education and information. This was compounded by the additional administrative burden associated with the Medicare claims processing problems (discussed further below), a reported high error rate with income assessments, lost revenue as a result of consumers refusing to pay backdated income assessed fees, and two revisions to the guidelines in July 2014. Furthermore, most providers have found that more staff time is required to deliver packages under a CDC model due to the consumer-driven planning process, which can take longer. Many providers explained that they were investing significant time undertaking initial discussions with consumers – sometimes to the point of developing an initial care plan and budget – only to have the consumer take up a place with another provider. Processing of subsidy claims by the Department of Human Services (Medicare) The inability for Home Care Package providers to utilise the Aged Care online claiming system following the introduction of the new Aged Care Management Payment System (ACMPS) and subsequent errors and delays in payments of Commonwealth subsidies created financial and administrative problems for providers, especially smaller providers. The concurrency of these issues with the implementation of the Home Care Packages Programme was cited as a key challenge. More than a year after the claiming issues commenced, eight of the 25 providers interviewed in November 2014 reported that the issues still had not been fully resolved and that their subsidy payments are significantly in arrears and/or incorrect, and that they are still required to submit time-consuming manual claims. Peak bodies interviewed in February 2015 also reported that this remained an issue for many of their members. DHS introduced case management support for providers in response to these concerns. Role of aged care advocacy services A small number of stakeholders suggested that there was a need for an independent third party to assist new consumers to understand fees and service pricing. When it was suggested that the National Aged Care Advocacy Programme (NACAP) might fulfil this role, they indicated that the existing advocacy services do not understand how CDC and individualised budgets operate, and that they are not sufficiently equipped to assist consumers with these issues. A number of examples were provided of instances where providers considered the advocacy services had misunderstood the intention of home care and CDC, usually by insisting that providers should not reduce ‘hours of care’ when existing consumers were transitioned to CDC (even where their expenditure was beyond the individualised budget). The evaluation consulted with one of the nine services currently funded to deliver NACAP services. This service confirmed that there had been a lack of training and education for advocates on CDC. However, they also provided a number of examples where they considered providers had either not understood or failed to implement CDC, including examples of telling consumers their ‘hours of care’ would reduce but not giving the consumers any say over how to restructure the package, refusing to provide financial statements, and severely limiting consumer choice and control. The Department is currently identifying resources and training for advocates so they can better support home care clients in making decisions around CDC. Additionally, a review of the Commonwealth Aged Care Advocacy Services is currently underway and will examine how advocacy services can support aged care clients within a CDC focussed environment. The findings of the review will be used to inform the Department on design of a new aged care advocacy programme that can provide a strong platform to support aged care clients across the spectrum of aged care services. 2.8 Interface with other services The evaluation was tasked with specifically considering the interface of home care packages with a number of other services, specifically: • • • • • • Commonwealth HACC Programme / Commonwealth Home Support Programme (CHSP); National Respite for Carers Programme; Department of Veteran’s Affairs Programmes; Community Visitors Scheme; Continence Aids Payment Scheme; and National Disability Insurance Scheme. Overall, the interface with these programmes appears to be operating as intended (as per Part J of the Programme guidelines), with relatively clear funding boundaries whilst still providing flexibility for consumers to access a range of available services. The key exception relates to the interface with HACC/CHSP. Of the 25 providers interviewed, 24 raised concerns regarding unclear boundaries between home care Level 1 and HACC / CHSP services, which currently provide similar services at a similar or higher level for a much lower consumer contribution. All of the ACATs/ACASs interviewed expressed similar concerns, as did most of the other stakeholder groups. The subsidy for a Level 1 place is $7,822 per annum (almost half that of Level 2), limiting the level of supports that can be offered. Consumers may also be required to pay an additional income assessed fee up to the full value of that subsidy. Providers and ACATs suggested that many consumers do not see this as good value for money when in most regions they can access similar services through HACC/CHSP. In some regions consumers can reportedly access up to $12,000 in annual HACC/CHSP services, without having to pay an income assessed fee and sometimes without having to pay a basic care fee or equivalent. It is noted that the policy intention of introducing Level 1 was to allow a low care bridge between HACC/CHSP services for those consumers whose level of service need is not high, but who would benefit from some case management and coordination of supports. Case management and coordination of supports will not be available under CHSP from 1 July 2015. It is also noted that the CHSP National Fees Policy may reduce some of the financial disincentives for consumers to access a Level 1 package. Sector understanding of the potential of Level 1 places may therefore change after the implementation of CHSP later this year, but at this time Level 1 is not seen as a useful addition to the suite of packaged care. Some providers reported a positive interface with HACC/CHSP in relation to accessing ‘top up’ services in cases of emergencies, or where consumers were eligible for a high care package but were on a low care package due to waiting lists. However, for this to occur home care providers needed to have a good relationship with local HACC/CHSP providers (or be the same provider), which was not always the case and so the level of collaboration was considered to be lower than desirable. Few issues were raised about the interface between home care packages and the NRCP, although some stakeholders raised concerns that the consumer contribution component of respite services could not be paid from home care budgets. This was a particular issue for special needs groups, including Aboriginal and Torres Strait Islanders, people living in rural and remote areas (who may incur additional transports costs for respite), and people who are financially and socially disadvantaged. Similarly, a small number of providers were concerned about what they considered to be a lack of access to the Continence Aids Payment Scheme (CAPS) for high care home care recipients (although it is noted that the Home Care Packages Programme Guidelines 2014 specifically address access to CAPS). The guidelines state that ‘a person receiving a Home Care Package may be able to receive a payment under the Continence Aids Payment Scheme. However, if the provision of continence aids is identified in the home care consumer’s care plan, they will not be eligible for the Scheme’. There were some examples given at interview of the capacity for positive collaboration between DVA and home care packages. Specifically, these related to the pooling of resources for consumers without ‘double dipping’ (i.e. where a consumer is entitled to a Level 4 package but is on a Level 2 due to no Level 4 places being available, the home care provider funds the clinical services and DVA funds the domestic assistance). This flexibility was seen as being beneficial for eligible consumers, although there is a question of equity for those consumers in similar circumstances but who not eligible for DVA and who live in an area where there may not be HACC top up funds available. The interface between home care and the NDIS is yet to be fully understood given the early stages of scheme implementation is focused on trial sites. A number of consumers indicated that one of the aspects they valued most about their home care services was the companionship and social contact with care workers. Receiving personal care can be very intimate, particularly for consumers who have been on packages for many years, and some of them describe their regular care workers as being ‘part of the family’. These consumers were often frustrated that care workers were now much more time-conscious and being forced to ‘hurry’ and did not have time to ‘stop for a chat’ as much as the consumer desired. This may suggest that there is potential for a closer interface between home care and the Community Visitors Scheme (CVS), which is not prohibited under the guidelines but which does not appear to be particularly strong at this time. In 2013-14 as part of aged care reform, the CVS expanded to include one-on-one volunteer visits to recipients of Home Care Packages who have been identified as socially isolated or at risk of social isolation. At the time of this report, the Department of Social Services was developing communication activities to promote awareness of CVS with Home Care Package providers. 2.9 Other issues relevant to the Programme implementation Some providers and ACATs/ACASs indicated that the leave (suspension) requirements for home care places are overly complicated. The guidelines currently differentiate between cumulative days and consecutive days for different types of suspension which determines when the subsidy payment is reduced. Many stakeholders suggested that the current mix of care levels did not seem to be well-matched to demand, with a surplus of Level 1 places (and, in some regions, Level 2 places) and insufficient Level 4 places. Stakeholders suggest that an analysis of actual occupancy rates since the commencement of the new arrangements would verify this. It is noted that the Aged Care Financing Authority (ACFA) will be monitoring occupancy rates as part of its regular reports on Impact of the 1 July 2014 Financial Reforms on the Aged Care Sector; these data were not available to the evaluation at the time of this report was written). Many stakeholders expressed concerns that the new arrangements may not offer a streamlined continuum of care for consumers as (a) there is still a need for a new ACAT assessment before moving between the low and high care levels; and (b) not all providers are allocated places at all care levels in a region, meaning that consumers may need to change provider if a place is not available with their current/preferred provider at that level. This was particularly pertinent in the context of rural providers, or providers who specialised in provision for special needs groups. Two potential solutions were suggested: • that all providers are allocated a minimum ‘set’ of all care levels; or • that no specific care level are allocated to providers, meaning that consumers could take an assessment for any level of care to any provider of their choice. The second suggestion was seen as more aligned to the values of consumer-direction, although it may present allocation and budgeting challenges to the Department (as well as requiring changes to the current aged care regulations). It may also necessitate changes in providers’ business models, as they would no longer be ‘assured’ of a certain number of places at a certain subsidy level, and this could potentially drive an increase in ‘cherry picking’ behaviour with providers giving preference to higher care consumers over lower care consumers. At least three of the ACATs/ACASs interviewed suggested that ‘cherry picking’ is already an issue in some areas, as consumers with dementia or from certain special needs groups can often wait much longer for a package than other consumers assessed as eligible for the same care level, even where there are known to be vacancies at that care level in the region. Several stakeholders also suggested that ACAR allocation processes should be reviewed. Three smaller providers, and a number of other stakeholders representing the interests of various special needs groups, indicated frustration with the ACAR allocation processes suggesting that not enough high care places were allocated to rural areas, and that there was little if any feedback given to unsuccessful ACAR applicants for special needs places (Aboriginal and Torres Strait Islander, and culturally and linguistically diverse). Two of the ACATs/ACASs expressed concern that whilst recent ACAR rounds appeared to have focussed on increasing the number of providers operating in rural areas rather than allocating addition places to existing providers to increase consumer choice and competition, this often did not occur in practice. In some areas it was reported that providers refused to fill places in difficult-toaccess areas, and that having a large number of providers with only a small number of packages each was not conducive to offering a continuum of care for consumers (because they would likely need to change provider to change care level). Dementia and cognition supplement Stakeholders were very supportive of the concept of supplements. However, smaller providers expressed concern regarding the processes for accessing the dementia and cognition supplement, specifically the requirement for a Registered Nurse to undertake the assessment. This means they must broker a nurse if they do not have one on staff, incurring costs that may not be recoverable. The need to undertake an assessment for consumers that already have a dementia diagnosis was also seen as duplicative. The effectiveness of the mandated assessment tool was questioned. The Psychogeriatric Assessment Scale (PAS) assessment is seen as too narrow as it focusses on memory not behaviours. The alternative Rowland Universal Dementia Assessment Scale (RUDAS, which is the mandated tool for assessing CALD consumers for the dementia and cognition supplement), was suggested as better tool for use with all consumers 2.10 Acceptance of programme change and commitment to CDC Thirty two per cent of providers in the survey strongly agreed or agreed that the Home Care Packages Programme has improved home care and services for consumers and carers, with 31 per cent either strongly agreeing or agreeing that most consumers are getting the level of supports they need. However, both the survey responses and the interviews found there is still some reluctance about implementing CDC amongst providers. This is primarily due to the perceived workload and resources required to implement CDC, as well as some concerns about the implications of change on provider business models and viability. There is also considerable concern regarding CDC amongst ACATs/ACASs. Of the 13 ACATs/ACASs interviewed, all said that they were supportive in-principle of the new care level structure and supplements, however only one indicated unqualified support for CDC. Many ACTS/ACASs were particularly concerned as to the appropriateness of a CDC approach for vulnerable consumers (such as those with dementia or cognitive impairment, the frail elderly without carers, consumers from special needs groups). They were concerned as to the lack of clarity around the ‘hours of care’ available under packages, and whether case management could be ‘traded off’ by consumers. Many of the interviewed ACATs/ACASs were looking for some persuasive clinical evidence that a CDC approach could work for different types of consumers. It was commented that the available information focussed more on theory and policy rationale rather than clinical evidence, particularly for vulnerable cohorts. In addition, a number of ACATs/ACASs expressed concern that income tested care fees would lead to consumers declining home care places which would see their health condition deteriorate. Several providers also raised this concern. It is noted, however, that when consumers do decline packages and cite the fees as a reason, anecdotally they often decide to purchase at least some unsubsidised supports – and often from the same provider. There are currently no data available to quantify the extent to which this is occurring. 3 Transitioning to consumer-directed care This chapter considers provider readiness for CDC and providers’ transition to a consumer-directed approach. It is focussed on the experiences of home care providers, consumers and carers, as well as the wider aged care sector (including ACATs/ACASs). The findings in this chapter were drawn from the interviews with 25 home care providers, 57 consumers and carers, other aged care sector stakeholder groups; and an online survey completed by 29 per cent of home care providers. Summary of key points: development of and transition to CDC • Transition to CDC is ongoing, with many providers working towards full implementation of CDC by July 2015. Most providers had developed their ‘approach’ to CDC, having either developed or were developing revised policies and procedure documents, and new or revised templates and tools (such as care planning templates and budgeting tools). • Most consumers on existing packages (approximately 80 per cent as at December 2014) have not yet transitioned to CDC. However, almost all providers had implementation plans in place to gradually transition existing consumers by July 2015, with most using the care plan review as the trigger for transition. • There are a small number of ‘early adopters’ who had fully embraced CDC and had reoriented their organisations to be more consumer directed (about 5 of the 25 providers in the interview sample fell into this category). These organisations had largely completed their transition to a CDC approach, and all or most of their packages were being delivered on a CDC basis. • There were also a small number of organisations who were resistant to or not supportive of the CDC philosophy or CDC principles, and who not made significant progress in terms of implementing CDC arrangements in their organisations. About 6 of the 25 providers in the interview sample fell into this category. • Most organisations were placed somewhere between these two perspectives: committed to CDC and making progress to implementing CDC in their organisation, though at different stages of ‘readiness’ and with some wide variations in their CDC approaches. Main considerations for providers in transition were: • Transitioning ‘high cost’ consumers. Transitioning higher cost consumers involved some ‘difficult conversations” with consumers, reductions in services, examining alternative sources of support and in some case considering residential care. • Systems changes and costs, including the scale of changes and integration to fully support CDC (and to automate many processes which were being done manually), and the cost of these changes. • Reorienting their service delivery model, including time spent on planning, coordinating and administering CDC packages, which is incurring higher costs. • Embedding cultural and practice changes, which will occur over time. 3.1 Provider readiness for CDC Despite there being a lead-in period of more than two years (from November 2012), readiness for CDC transition in July 2015 varies significantly across providers. Based on the interviews, there appeared to be a small number of ‘early adopters’ who had fully embraced CDC and had reoriented their organisations to be more consumer directed. At the opposite end of the spectrum, there were also a small number of organisations who were resistant to or not supportive of the CDC philosophy or CDC principles, and who had not made progress implementing CDC arrangements in their organisations. Most organisations were placed somewhere between these two spectrums: committed to CDC and making progress to implementing CDC in their organisation, though at different stages of ‘readiness’. This is supported by survey data, which indicated that as at December 2014, 78 per cent of providers were ‘still preparing for the implementation of CDC’, and 20 per cent considered themselves ‘wellprepared’ – as illustrated in the figure over the page. Figure 3: Provider responses to the survey question ‘How would you describe this service’s current state of preparation for the transition of all places to CDC from 1 July 2015’ 3.1.1 Classifying providers’ level of CDC readiness The providers interviewed as part of the evaluation were categorised into three broad categories reflecting their state of readiness for CDC: • Early adopters or leaders – fully embraced CDC and have largely completed the transition to CDC • Proactive – implementation of CDC is a work-in-progress, wide variations in different aspects of approach and transition • Reactive or resistant – not supportive of CDC, little or no progress in terms of implementing CDC, CDC approach is similar to approach for usual care. These are briefly described in the table below Strategy and approach Systems Management Staffing Culture and practice Early adopters or leaders Proactive Reactive or resistant clear, goal-based approach to CDC; significantly different from usual care approach approach to CDC is developing/evolving do not have a CDC approach or approach little different from usual care approach have organisation-wide CDC implementation plans, and have reviewed strategic plans to ensure alignment with CDC have organisation-wide CDC implementation plans typically have not examined organisational-wide strategy may or may not have implementation plans; transitioned few if any consumers to CDC have invested in finance/IT systems changes and integration; systems already in place have made some changes to finance/IT systems, or at planning stage Little investment in finance/IT systems; CDC processes still manual can demonstrate strong management/CEO support for CDC and willingness to invest in CDC transition varying levels of understanding of CDC and varying levels of commitment management support unclear or resistant; concerns about business viability have invested in staff training and development, including coordinators and care workers have invested in staff training and development for managers, though rarely for care workers some staff training undertaken (general training available to all organisations); limited to managers talk about the potential and possibilities of CDC more than they do about the challenges some practice changes, though variable; though some practices not significantly different from usual care very few practice changes; practices not significantly different from usual care Figure 4: Classification of providers Source: KPMG 3.1.2 Activities undertaken to prepare for CDC implementation Providers undertook or participated in a number of internal and external activities to prepare for the CDC transition. Internally, activities included: • their own research on consumer-directed approaches (a small number of providers) • development of their CDC model or approach based on research, the guidelines, external training and information sessions, and their own experiences of CDC and other individualised planning and funding (most providers, though noting variable levels of effort) • revision of policies and procedures and development of new care planning templates, budgeting and expenditure reporting template, and care planning tools (some providers) • staff training sessions, including for coordinators (most providers), and care staff (a small number of providers). • Providers participated in a range of external information and training activities, as illustrated in the following figure. Figure 5: Provider responses to the survey question ‘What activities (if any) has this service undertaken, or does this service plan to undertake, to prepare for the implementation of CDC from 1 July?’ Source: KPMG analysis of survey responses Aspects of provider readiness In examining provider readiness for CDC, the following aspects were considered: • • • • • Strategy and approach – whether providers had developed an organisational approach to consumer-directed care, and whether providers had an overarching corporate or organisational strategy which was consistent with CDC principles. Systems – whether providers had in place appropriate and integrated systems to support a consumer-directed care approach, including finance, client management and other systems. Management commitment – whether provider management, including the chief executive and senior management team, were committed to the principles and intent of CDC, and were driving organisational and practice change as part of implementing CDC. Staff commitment, skills and capabilities – whether providers had staff committed to the principles and intent of CDC, and had invested in education, training and development to ensure staff had the skills and capabilities to work in a consumer-directed way. This included investment in care managers and coordinators, as well as direct care workers. Culture and practice changes – whether providers had an overarching philosophy which reflected CDC principles and were embedding practice changes in the organisation. Strategy and approach Most providers interviewed as part of the evaluation had developed, or were developing, an organisational approach to CDC, including an approach to planning and goal setting. In reviewing materials provided by these providers, it was clear that some providers had developed a range of innovative tools and approaches to CDC which were fully consistent with the philosophy of CDC and CDC principles. This included care planning tools and guidance, materials for consumers to prompt thinking and discussion, user-friendly and easy to understand care planning templates, and supporting tools and guidance for staff (such as simple, online budgeting tools). However for some providers, their CDC approach and underlying materials, tools and guidance were similar to usual care – that is they were providing some (but limited) choice, they were focussed on services rather than goals or needs or saw CDC as usual care with an individual budget component. There were few examples of providers reorienting or revising their overarching corporate or organisational strategy to be consistent with CDC principles, though this was evident for a small number of providers who had clearly embraced the CDC approach and were well advanced in implementing CDC. Most providers stated that their approach to CDC was in development and/or evolving and changing over time as they gain more experience with working with consumers in a consumer-directed way. This was reflected in provider survey responses – as illustrated in the figure below. Figure 6: Provider responses to the survey questions relating to the evolution of their CDC approach Source: KPMG analysis of survey responses Systems Providers are at varying levels of progress with developing or upgrading their client management and finance systems and integrating these systems. Larger providers reported that they were closer to having the necessary system changes in place, whereas medium or smaller providers were less prepared. In some cases (about a quarter of the providers interviewed), providers have adopted a ‘wait and see’ approach, intending to maintain their current systems post-July 2015 and undertake specific CDC processes manually (for example, preparation of individual expenditure statements). A number of providers noted that systems/software vendors were not adequately prepared for the changes or the timeframes, and were not capitalising on the opportunities that the move to CDC was providing in terms of off-the-shelf or easily-adapted software and systems solutions. Management and board commitment Executive commitment to CDC was one of the key driving factors in providers developing a CDC approach and in successfully and seamlessly transitioning to CDC. Again, there was a notable level of variation, with some providers highlighting the high-level of engagement from their boards, CEO and senior management and a high level of commitment to CDC (and willingness to invest in CDC). However, there were providers for whom CDC was more of a business change rather than a strategic change, and for whom transition was being driven by line managers and coordinators. There were some providers who had CEOs/senior managers who were not engaged or were unsupportive, and were concerned as to the cost of CDC on the business and the impact of CDC on business viability. A simple indicator of executive commitment to CDC was whether or not the board received regular reports on CDC implementation. Staff commitment, skills and capabilities All providers interviewed had delivered some training to staff on CDC, and/or had facilitated staff attending external training and information sessions. There were differences in the level and depth of training provided, and the coverage of training, with some providers seeking to ensure that all staff (managers, coordinators, care workers) had the required knowledge and understanding of CDC and the skills to work in a CDC frame, and were (or will be) supported to change practice, and others who had limited training for package managers and coordinators. A small number of providers highlighted difficulties in gaining sufficient commitment to CDC from some coordinators (typically those who had been a coordinator for a number of years), which affected their ability to implement a true CDC approach. Culture and practice changes Cultural and practice change involves management and staff reorienting their way of thinking and approaching package care to be consumer-focussed, and changing their behaviours and practices to be consistent with this new way of thinking. Often, culture and practice changes are only observed in the longer-term – as people and organisations start to see the benefits of the new approach or change and evolve their behaviours and practices as a result. There was evidence of culture and practice changes emerging in some organisations interviewed for the evaluation, though it is too early to observe wide-scale practice changes at this stage of transition. Organisations that had fully embraced CDC (early adopters) highlighted the importance of embedding change throughout the organisation – from managers through to direct care workers – and had started to see changes in practice. This included coordinators having a different mindset and approach to care planning, and care workers being more flexible and responsive to consumers’ day-to-day preferences. However, many providers interviewed had yet to see any significant change in practice, with some providers not driving or supporting cultural and practice change in their organisations, instead focussing on administrative aspects of CDC such as individualised budgets and expenditure statements. 3.1.3 Provider transition and readiness for CDC – key considerations Providers raised a number of concerns with regard to the CDC philosophy and overall approach, as well as the implementation and transition to CDC. Main concerns included: • • • • • Questions as to whether consumers wanted more choice and to be more involved in their care planning, and concerns about over-burdening already vulnerable people (note that this was largely discounted by consumers themselves) The level of time, effort and investment required to implement CDC, in the absence of any additional funding or one-on-one support. Providers highlighted changes to IT systems as a particular concern Lack of standardised information resources for consumers and planning guidance and tools for providers The tension between service pricing to enable cost recovery whilst being competitive The viability of organisations in the face of increasing competition and flexibility to choose brokered services rather than use in-house services. The provider survey sought information regarding key provider concerns. These are illustrated in the following table. Figure 7: Top 5 concerns of providers regarding the implementation of CDC from 1 July 2015 Source: KPMG analysis of survey responses 3.2 Transitioning existing consumers to CDC Extent to which existing consumers had been transitioned to CDC arrangements Providers varied in the extent to which they had transitioned existing consumers to CDC arrangements: • A small number of providers had transitioned all of their existing consumers and were delivering all packages on a consumer-directed basis. • • • • • The majority of providers had commenced the transition, and were expecting to complete the transition by June 2015. However many had not made significant progress at the time of interview and were expecting most consumers to transition during the first half of 2015. A small number of providers had yet to commence transition, and had not developed a plan to manage the transition. The provider data indicated that as at December 2014, 11 per cent of packages allocated before 2013-14 had been transitioned to CDC arrangements. There were minor differences across care levels, though there were notable variations by size of provider and level of remoteness: Small providers (those with less than 50 packages) had transitioned fewer packages to CDC arrangements than larger providers (those with more than 100 packages) – 7 per cent compared with 12 per cent for large providers Providers in outer regional areas had transitioned fewer packages to CDC arrangements than providers in inner regional and metropolitan locations – 7 per cent compared with 13 per cent (inner regional) and 11 per cent (major cities) . This is illustrated in the figure below: Figure 8: Proportion of existing packages (allocated before 2013-14) transitioned to CDC arrangements, December 2014 Source: KPMG analysis of survey responses Overall, including new home care packages allocated from 2013-14 and packages allocated in the CDC pilot period, 31 per cent of packages were being delivered on a CDC basis as at December 2014. There were some variations across care levels, provider size and remoteness, as illustrated in the figure over the page. Figure 9: Proportion of all home care packages delivered on a CDC basis, December 2014 Source: KPMG analysis of survey responses Process for transitioning existing consumers The majority of providers had a CDC transition plan and were transitioning consumers to CDC arrangements gradually – either at the point of each consumer’s annual care plan review, or based on another schedule developed by the provider. This enabled providers to manage the transition workload over time, and enabled coordinators to develop the skills required to effectively develop a consumer directed care plan. A smaller number of providers (generally those that had completed the transition process), had transitioned consumers over a short period of time (e.g. a 2-3 month period). The process for transitioning existing consumers varied across providers, and largely reflected their overall CDC approach: • • Some providers were transitioning consumers as if they were new CDC package consumers, fully explaining CDC to each consumer (including written information and resources), using their new approach to planning and goal setting, helping consumers identify changes to their support arrangements and new supports, and working through an individual budget Many providers explained CDC in a general sense to consumers who were transitioning, and undertook a more in-depth review than they generally would have otherwise – discussing and reviewing current support arrangements with consumers to determine whether they were still meeting need, helping them to identify changes and new supports (and explaining what is possible under CDC), and providing them with an individual budget • Some providers were transitioning consumers as per a regular ‘review’, reviewing current support arrangements, making minor changes and providing them with an individual budget, often with minimal reference or explanation of CDC or what is possible under CDC. Consumer experience of transition to CDC Consumer and carer experience of the transition to CDC from existing packages was highly variable, with consumers tending to fall into three groups: • • • those that said that there was ‘no change’; those that said they received ‘reduced hours’ and a decline in the amount of services available. This tended to be slightly more likely in rural areas; and those that said that the transition had improved their package by making it easier to get additional services or equipment, and especially through improved flexibility. The difference in consumer perception of CDC and whether transition was positive or negative appears to be related to whether the provider presented it as a government imposed change, or as a change to allow more flexibility for consumers. The majority of consumers who had transitioned to CDC understood at a broad level what the change meant and the reasons for it (often described by the providers as being ‘government regulations’), and they were given written materials. These were the consumers that were more likely to say that there had either been no fundamental changes to their package or a reduction in services as a result of CDC. A minority of consumers described having one-on-one discussions with their providers and, sometimes, attending information sessions about CDC where providers explained that there was more flexibility in how packages could be used. Overall, these consumers tended to be more positive about CDC. Some examples of consumer and carer experiences with the transition to a CDC packages are provided below. Some consumer and carer perspectives on transition to CDC (real names not used) John has been a widower for six years. Not long after his wife died, his daughter, who is a social worker, convinced him that he needed help around the home and arranged for an ACAT assessment. He has been on a CACP package ever since. About 9 months ago he was transitioned onto a CDC Level 2 package. He was given a letter and some brochures explaining the changes but he ‘never bothers with that stuff’. The coordinator explained to him that the services would be the same but he would now have an individual budget. He receives domestic assistance and help with meals preparation. He used to receive services twice a week, but this was recently changed so that he received more visits each week. This change was made after his daughter suggested that it would be better to have someone visit more often. He likes most of the care workers and gets annoyed when the provider sends ‘new faces’. He does not think the he has much scope to influence who the provider will send on any given day. Louise cares for her mother, who is deaf and blind and has been receiving an EACH package for some years. At the time of the interview, Louise’s mother was being transitioned to a CDC Level 4 package, which she described as a very traumatic experience because the provider said there would be less funding available and that the services would need to be reduced to only the essential care (personal care, medication Some consumer and carer perspectives on transition to CDC (real names not used) management and meals assistance three times daily). They had to cancel domestic assistance, continence pads, social activities and some of the meal services. The provider told them they would have to pay an additional $700 per month to maintain those services. Louise feels that there should be additional supplements for people who are deaf and blind. Louise also feels that they have little if any control over the times of day services are delivered: sometimes they provide breakfast at 9.30am and then the lunch person will arrive at 11.00am. Although Louise thinks that her mother usually receives good quality care, she has found some of the provider’s care workers unreliable, particularly with medication management. They have not considered changing providers, however, even with these problems. Dwayne has been receiving a home care package for about 4 years. He transitioned to CDC a few months ago. A lady from the home care provider came to his house and explained what the changes would mean, mostly emphasising that there would now be an individualised budget and that he would receive an itemised monthly statement The provider sat down with him to explain how the statement works using a ‘dummy sheet’. Although he has not changed any of his services, he knows that he has the ‘freedom’ to say what he would like and to change his care plan if he wishes to. He also says when he wants them to come and knows that he can request certain workers if he would like to. He is very satisfied with his arrangements. Wanda lives in a regional area and has been on a CACP for about four years. She recently transitioned to a CDC Level 2 package. Her case manager visited her to explain the changes and was very thorough. She has noticed a few changes since she moved to CDC: she now has to pay a fee for transport to medical appointments (previously this was paid by the provider, but there is not enough funding in her budget to cover these costs). She also has to make arrangements to book the transport herself, whereas before the case manager did that for her. She receives meals assistance which was fully covered before, but for which she now has to pay an additional fee from her own pocket. She finds it more difficult to contact her case manager. Wanda thinks that things have become a lot more complicated with CDC. Before if she wanted extra help, in the garden for example, she would just ask her case manager and it would get done; now the case manager needs to ‘consult the paperwork’ and see if there is enough money in the budget. It seems very bureaucratic. She preferred it the way it was before. 3.3 Key transition considerations for providers Transitioning ‘high cost’ consumers Providers highlighted that under existing package arrangements, some consumers were receiving more support, and some were receiving fewer supports, than would be possible under a CDC package.. This was due to providers’ flexibility under current arrangements to vary the level of support provided in each package to reflect individual needs, something which is not possible under CDC arrangements. Transitioning those who were receiving more supports than would be possible under a CDC package was identified as particularly challenging. Providers highlighted a number of strategies for managing this: • moving the consumer to a higher-level package if there was one available and they had been assessed for a higher package level – this was only possible where a person was on a Level 2 package (CACP), and there was a Level 3 or Level 4 package available; • discussing the need to reduce the levels of support at the care plan review point, and working with consumers and families to identify alternatives – for example, reducing higher costs services (such as support on weekends) and replacing with informal supports; • for some consumers on Level 4 packages and high levels of support, discussing the possibility of the person moving to residential care; and • some providers had committed to covering the additional cost of supports themselves, thereby ensuring that no consumer was worse off in the transition to CDC. • It was noted that, at the time of the provider interviews in November 2014, a third of the sampled providers had yet to address this issue in their transition process. Systems changes and costs Most providers had or were planning to upgrade or replace their client management systems, and establish interfaces with their financial management systems, to support CDC implementation. However, a number of providers noted that: • the cost of systems and software development was a significant one-off cost which is not able to be recouped; and • they were delaying implementation of systems changes until the detailed requirements of CDC were fully understood internally and their CDC approach had been embedded – this meant that processes around current CDC packages were being conducted manually for example, preparation of individual expenditure statements. Administrative and coordination costs Providers reported that they were spending more time on planning, coordinating and administering CDC packages than is required for other care packages, thus increasing a range of costs. Providers stated that higher costs were attributed to a number of features of CDC: • • • • providers are spending more time on planning with consumers at the commencement of a package; consumers are taking more time to consider their options and the costs, often delaying when the package commences; in supporting greater choice some providers were brokering additional services, which added administration time when establishing the service arrangements (however, most recognised the additional upfront costs were relatively minor, compared to ongoing coordination and administration costs); and providers are spending time tracking expenditure at an individual level and reporting package expenditure to consumers, which resulted in additional administrative costs (which were in turn being driven by the level of automation of the expenditure recording processes and the sophistication of their financial systems). Providers stated that these costs were being passed on to consumers through administration fees and coordination charges. Some consumers were raising concerns regarding the level of administration and case management fees, particularly where they were impacting on the amount available to be spent on supports. It was also noted by providers that the administration and case management fees were being disclosed to consumers for the first time, and that this transparency was prompting questions and concerns from consumers. Figure 10: Provider responses to the survey questions relating to the administration of CDC Source: KPMG analysis of survey responses Embedding practice changes Many providers highlighted that CDC was a different way of working with consumers, and that it will take some time to embed the new approach into their organisation. Some providers noted that they understood the theory and principles of CDC, though were challenged in changing their practices and behaviours. Providers who had CDC packages from the pilot period were much further advanced than providers who had recently been allocated CDC packages. Other considerations Other considerations raised by providers included: • • • • Workforce – including lack of staff skills and capabilities to work in a CDC context, including a lack of commitment to CDC by some staff (mainly those involved in care planning), which affected providers’ ability to implement a true CDC approach. Large providers noted the challenge of rolling out training and sustaining change across multiple areas of operation. The need for coordinators to develop finance and budgeting skills with the ability to have discussions with consumers about the cost of care (including fees and contributions). The ‘values’ of the organisation influenced this. Individual budgets and monthly expenditure statements – there was wide variation in providers approach to budgeting and developing monthly expenditure statements, significant variation in the systems available to support budgeting and expenditure reporting, and in some cases considerable time and effort in undertaking these processes manually. Some providers suggested a sample budget and sample expenditure statement would have been useful. Pricing services and overheads – some providers are still developing unit prices for their services, or have implemented price structures that may not be reflective of the actual costs incurred (in the not-for-profit sector, these are usually under-estimated). Survey results The provider survey conducted as part of the evaluation sought information on the key issues or challenges faced by providers in implementing CDC arrangements. The figure below illustrates the key challenges reported by providers: Figure 11: Provider responses to the survey question ‘Has this service encountered any significant problems during the implementation of CDC?’ Source: KPMG analysis of survey responses 4 Consumer-directed care in action This chapter considers the operation of CDC in practice. It is focussed on the experiences of consumers, carers and home care providers. Specifically it considers how CDC is operating in practice at this relatively early stage, using the CDC principles set out in section 2.2 of the Home Care Packages Programme Guidelines 2014 as a framework for good practice and the intended policy outcomes of CDC in home care. The findings in this chapter were drawn from the interviews with home care providers, ACATs/ACASs, consumers and carers and other aged care sector stakeholder groups; the online survey of providers; and the provider service data collection. Summary of key points: CDC in action • • • • • 4.1 The transition to CDC is still in its early stages and will take some time to be embedded in practice. Assessing the current state of CDC against the framework of the CDC principles, it appears that some steps have been made towards increasing consumer choice and control, acknowledging the right to individualised care and support, and respectful and balanced care partnerships. The extent to which these steps have been made varies depending on a provider’s current position on the CDC spectrum. Limited progress has been made towards the use of CDC to support community and civic participation, and wellness and re-enablement. The most notable accomplishment of CDC to date relates to the principle of transparency, due to the implementation of individualised budgets and reporting. There is still some work to be done around the transparency of administration and case management pricing. Some special needs groups may not be benefiting from CDC to the same extent as the wider population. Consumer choice and control Principle: Consumers have managed their own lives for a long time. They should be empowered to continue to manage their own life by having control over the aged care services and support they receive. This requires the provision of, and assistance to access, information about service options that enable a consumer to build a package that supports them to live the life they want. Many providers reported that consumers were not making significant changes to their support arrangements when they transitioned to CDC arrangements, and new consumers were not accessing substantially different services from usual care consumers. They reported that in the main, CDC consumers were continuing to access ‘core services’ such as personal care, assistance with household tasks, and clinical (nursing) care, with some variation and new services at the margins. Notable differences between consumer preferences for CDC and non-CDC consumers were observed for supports to access social and community-based activities, transport, and in some cases specific equipment designed to increase independence (and not available through other programmes). Data relating to the range of supports accessed by CDC consumers is presented in Appendix C It should be noted that the extent to which consumers were able to choose different services was driven by the opportunities and information that providers gave them, and the support provided to make choices – in effect the quality of the CDC transition (for existing consumers) or planning process and the planning approach (for new consumers). A number of consumers stated that they “don’t know what they don’t know” – they did not know what was possible or even what was available, and they relied on their package provider to explain this to them, give them information, and help them to develop a care plan which met their needs and goals. There were some providers whose planning approach fully supported people to make choices based on their identified needs and goals, whereas others provided more limited information and support and hence much more limited choices to consumers. Commonly, consumers expressed a lack of understanding about what else might be available and a reluctance to ask for it unless the provider made an effort to start a discussion about what else might be possible. A small number of consumers and some carers suggested that they had to take the initiative in educating providers about the potential flexibility under a CDC package (which often arose when requests were made for different kinds of services or equipment that were not part of the ‘standard’ care and services highlighted in the guidelines). Most consumers do exercise some limited control over their package, which is mostly around the times that home care services are delivered and, to a lesser extent, by whom those services are delivered. A few consumers and some younger carers indicated that they exercised more control over the package, although this sometimes led to disputes with providers over appropriate reductions in administrative fees to offset the self-management (generally settled through negotiations). There appeared to be frequent disagreement with providers relating to the use of package funds for equipment purchases, and the policies for return of equipment purchased from package funds. Overall, however, the vast majority of consumers and carers interviewed for the evaluation rated their satisfaction with home care 4 or 5 out of 5 (satisfied or very satisfied). Scores were high even where they expressed concern about having limited choice or control, or as to the quality of services. Male consumers were most likely to rate their satisfaction higher. 4.2 Rights Principle: CDC should acknowledge an older person’s right (based on their assessed needs and goals) to individualised aged care services and support. Although most providers appear committed to this principle, they are at different stages. This can be related to their current position on the CDC spectrum. At the more advanced end of the CDC spectrum, providers often use self-assessment tools and there is a strong focus on unhurried, individualised assessment and planning. Providers spoke of the need to encourage consumers to think more creatively about how packages might be individualised, acknowledging that sometimes this had to be a gradual process. A consumer might need to get initial supports in place and feel safe at home before they can think more about community and civic participation, for example, particularly if they have entered the home care system after a health crisis. At the other end of the spectrum are providers who continue to focus on a relatively standard set of care and services, with preoccupation on the inclusions and exclusions in the guidelines. Some consumers expressed frustration about having to ‘fight’ for certain equipment purchases or other one-off expenditure. 4.3 Respectful and balanced partnerships Principle: The development of respectful and balanced partnerships between consumers and home care providers, which reflect the consumer and provider rights and responsibilities, is crucial to consumer control and empowerment. Part of creating such a partnership is to determine the level of control the consumer wants to exercise. This will be different for every individual, with some people requiring or wanting assistance to manage their package and others choosing to manage on their own. Consumers should have the opportunity to work with the home care provider in the design, implementation and monitoring of a CDC approach. Home care providers should be encouraged to include consumers in their CDC redesigns. As with the rights principle, the respectful and balanced partnerships principle is still evolving at this stage of maturity within the Programme’s life. This is particularly so when it comes to determining the level of control that the consumer wants to exercise over their package. Some providers candidly reported that some of their staff were struggling with the concept – and the practice – of shifting authority to the consumer. The importance of CDC champions and mentors for staff was emphasised, and this was an area where providers who had participated in the CDC pilots had a significant advantage. The overall message is that it takes time for staff to change their practice, just as it takes time for many consumers to be comfortable in asserting and exercising some control. The transition from a service provider/care recipient relationship, to a more partnership-based approach to care, will also take time. The second part of this principle envisages a level of co-production between providers and consumers in the development of CDC approaches. Arguably, this is an ‘aspirational’ principle and a relatively mature indicator that would not be expected to be evident so early in the implementation of a new programme. As such, it is not surprising that there was not any evidence of co-production occurring in any meaningful way at this time. Several providers spoke of seeking feedback from consumers through satisfaction surveys or similar exercises, although only 3 of the 25 providers in the interview sample spoke about actively involving consumers in the design and development of their service delivery models. At this time, many providers appear to be more focussed on complying with the required timeframes for CDC implementation. 4.4 Participation Principle: Community and civic participation are important aspects for wellbeing. CDC in aged care should support the removal of barriers to community and civic participation for older people, if they want to be involved. Some providers spoke about the importance of community and civic participation and it was clear that, where possible, this was considered as part of CDC. The evaluation interviews suggest that for most providers this does not appear to be a priority. That said, there were a few of examples of CDC enabling consumers to participate in community and civic activities, as well as simply maintaining social connections or interests of importance to them. For example: • An online home delivery grocery order was established for a woman with dementia living in a rural town, so that instead of having a care worker accompany her on a weekly trip to the supermarket, package funds could be used for a monthly visit to a nearby larger town where the woman enjoyed browsing, window shopping and watching the passing parade at a café as she had enjoyed doing for much of her adult life. A man from a culturally and linguistically diverse background with limited mobility, in consultation with his provider and doctor, decided that he was capable of managing his medication and did not need that service provided through his home care packages once it converted to CDC. Instead, he used funds for transport to regular club meetings in his native language and some cultural events. • 4.5 Wellness and re-enablement Principle: CDC packages should be offered within a restorative or re-enablement framework to enable the consumer to be as independent as practical, potentially reducing the need for ongoing and/or higher levels of service delivery. Many people enter the aged care system at a point of crisis. Such situations may require the initial provision of services designed to address the immediate crisis. However, there should always be an assumption that the older person can regain their previous level of function and independence with re-enablement services being offered at a time that suits/supports the individual circumstances. Although there was a great deal of interest in the concepts of wellness and re-enablement by the majority of providers and other stakeholders, as well a very high level of support for the idea that packages could support wellness and re-enablement, there was little evidence that it currently occurs. • One for-profit provider – that also has strong links to the acute care sector as a provider of post-acute services – gave a very salient description of a planned re-enablement strategy for new consumers, which would often involve ‘frontloading’ the package with higher levels of supports in the first few months, tapering off as the consumer’s reenablement goals were met. This meant that, contrary to the common practice of spreading package funds more or less evenly across a year in the initial planning, they • planned to spend a greater proportion of it earlier with the objective being that the consumer’s care needs would then decrease. Only one provider spoke about moving consumers down care levels with the consumer’s agreement once their re-enablement goals were met and ‘celebrated’, including from a Level 4 back to a Level 2 in one case. These were isolated examples, however, and the concept of moving consumers to lower care levels in particular seemed a foreign concept to many providers. 4.6 Transparency Principle: Under a CDC package, older people have the right to use their budgets to purchase the aged care services they choose. To make informed decisions about their care, older people need to have access to budgeting information, including the cost of services, the contents of their individualised budgets and how their package funding is spent. Of all the CDC principles, this is closest to being achieved as a result of the mandated individualised budgets and monthly statements. The majority of consumers and carers interviewed indicated some level of engagement and interest in their individualised budget and expressed an appreciation for the monthly statements. Approximately half of the consumers and carers read these statements thoroughly and indicated that they valued the information, while others appreciated the transparency of the statements but felt they were too complex or confusing or simply were not interested in the details. Younger carers were all very engaged with the budget statements. There were variable views expressed regarding contingency funds. The majority of consumers and carers thought it was good to have a contingency, and some described how they worked with their provider to plan the use of the contingency over time (i.e. for large equipment purchases or buying blocks of respite time for weekend services for special occasions), whilst others indicated that the contingency sat in their budgets accumulating and they had little understanding of what it was for or even whether it was capped. 4.7 Considerations for special needs groups A number of issues were identified relating to the aged care special needs groups. These are considered below. 4.7.1 People from Aboriginal and Torres Strait Islander backgrounds Stakeholders identified a number of issues relating to home care and CDC for people from Aboriginal and Torres Strait Islander backgrounds. Many of these issues are similar to those identified in the evaluation of the CDC pilots. Many stakeholders consider that the guidelines do not allow sufficient flexibility to meet the diverse needs of Indigenous communities, particularly in terms of the inclusions and exclusions. It is suggested that the relatively low take-up of home care by Indigenous communities is a result of this inflexibility. More specifically, some providers are hesitant of individual budgets for Indigenous consumers because of their long-standing practice of pooling funds for community use. There is disagreement as to whether individualised budgets are suitable for Indigenous consumers, with some suggesting it can be stressful for the recipient to have an individualised budget that others in the community think should be shared. This is however not a consensus view. Additionally some providers are concerned that identifying and pricing case management as a discrete service in an individual budget will disadvantage Indigenous consumers who need case management but may not want to pay for that service from their individual budget. The general exclusion of using home care funds to pay consumer fees or contributions for other Australian Government services, particularly ‘gaps’ for Medicate Benefits Scheme and Pharmaceutical Benefits Scheme rebated services, and co-payments for Australian Government funded respite services was contentious. Some stakeholders suggest that package funds should be available to cover these costs given the very low incomes of many Indigenous consumers. Some stakeholders are concerned that guidelines are too inflexible for Indigenous communities. It was suggested that Part E of the guidelines should make specific reference to meeting the cultural needs of Indigenous peoples, which would allow clarity that package funds could be used for travel to funerals and return to country. They argue that if there are specific sections on aids and equipment and digital technology in the guidelines, there could also be something about cultural wellbeing. Some Indigenous-specific providers are concerned as to the fairness of ACAR allocation processes, indicating a low success rate in ACAR allocation rounds and a lack of feedback to help them improve their applications. It is noted that the Department does provide generalised feedback for all applicants on its website and, on request, provides written feedback to individual applicants. At the time of writing this report, Outcomes Plus and the Australian Government were finalising an Overview document and Guide to assist culturally and linguistically diverse (CALD) communities and other stakeholders to understand the Aged Care Approvals Round (ACAR) process. It is anticipated that this document will be published prior to launching the next ACAR. 4.7.2 People from culturally and linguistically diverse backgrounds A key concern raised by stakeholders in relation to people from CALD backgrounds was the cost of interpreting services. TIS National provides on-site and phone interpreting services to Australian Government subsidised home care and residential aged care providers at no cost to the approved provider or consumer to negotiate the Home Care Agreement, co-design the care plan and individualised budget, and when discussing the consumer’s monthly income and expenses statement. This ensures consumers can fully participate in the assessment, care planning and review of their Home Care Package. Consumers are, however, charged for interpreters when receiving personal care and other services that have been agreed through the development of the care plan. Some stakeholders considered that it was inequitable for CALD consumers to have the value of their package reduced to pay for these services. The relatively low number of home care places with a condition of allocation for priority of access for people of CALD background was raised. Similarly to Aboriginal and Torres Strait Islander services, stakeholders suggested that CALD services should be provided with better feedback on unsuccessful ACAR applications to help increase their success in future competitive application rounds, and to increase the number of home care places with a condition of allocation for priority of access for people of CALD background. It is noted that the Department does provide generalised feedback for all applicants on its website and, on request, provides written feedback to individual applicants. The National Ageing and Aged Care Strategy for People from CALD Backgrounds was released in 20121. The strategy will inform the way the Australian Government supports the aged care sector to deliver care that is appropriate and sensitive to the needs of older people from CALD backgrounds. It includes a number of activities that aim to address the areas of concerns raised by stakeholders, including enhancing the capacity of existing and emerging CALD communities as potential aged care service providers and developing relevant service models and partnerships, addressing any existing ‘stigma’ in CALD communities that inhibits aged care service access, and encouraging members of CALD communities to consider employment, volunteering and training in the aged care sector. The Partners in Culturally Appropriate Care (PICAC) initiative is one such initiative that aims to address CALD barriers to aged care access. It was developed by the Australian Government to improve the capacity of aged care services to respond to the differing needs of older people from CALD communities. Organisations are funded in each state and territory to provide PICAC projects. 4.7.3 People who live in rural or remote areas Two key considerations were raised for people who live in rural and remote areas. The first related to access to sufficient care levels, with stakeholders reporting that there were not enough high care packages available in rural and remote areas. Further there was a perception that some providers ‘cherry picked’ the location of consumers they offered a package to, prioritising those living closer to town. The second issue related to the additional costs involved in delivering services to rural and remote areas. Most providers charged travel costs to the consumer (in some cases, they allowed a ‘free’ kilometre allowance based on the distance from the provider’s office, with consumers paying a perkilometre cost for travel outside of the free radius). There were concerns that this effectively lowered the value of the package for rural and remote consumers compared to those living in urban areas, raising equity concerns. Previously these additional costs would have been cross-subsidised by other packages 4.7.4 People who are financially or socially disadvantaged There was limited information in relation to this group. However, some stakeholders raised similar issues as for Aboriginal and Torres Strait Islanders regarding the use of package funds to pay consumer fees or contributions for other Australian Government services, particularly ‘gaps’ for Medicare Benefits Scheme and Pharmaceutical Benefits Scheme rebated services, and co-payments for Australian Government funded respite services. Some stakeholders suggest that package funds should be available (or, more appropriately, cashed out) to cover accommodation costs and food purchase costs in emergency circumstances. 1 https://www.dss.gov.au/our-responsibilities/ageing-and-aged-care/older-people-their-families-andcarers/people-from-diverse-backgrounds/national-ageing-and-aged-care-strategy-for-people-from-culturally-andlinguistically-diverse-cald-backgrounds Comments relating to people who are homeless or at risk of becoming homeless are also broadly applicable to the financially and socially disadvantaged group. 4.7.5 Veterans There was insufficient information available to make any specific comment in relation to this group. 4.7.6 People who are homeless or at risk of becoming homeless A peak body representing providers that specialise in providing services to consumers who are homeless or at risk of homelessness, and consumers who are socially and financially disadvantaged, reported that, despite the removal of age-based entry criteria for aged care eligibility, further work is required to ensure that ACATs/ACASs and other stakeholders understand the early ageing effects of chronic homelessness. It was noted that many consumers from this group experience assessment delays because they are aged under 65 years. It was suggested that consumers identified as being members of the homeless special needs group – as well as care leavers – should be generally classified as ‘aged’ from 50 years plus, as per the current situation with consumers in the Aboriginal and Torres Strait Islander special needs group. Concerns were raised regarding potentially reduced case management hours under CDC packages. Providers reported that care coordinators accustomed to working with homeless consumers were in the habit of regularly ‘dropping in’ on their clients. Some providers said they were able to less of this activity under the new arrangements. These changes were reported to be negatively impacting on some consumers as well as staff, who were having to adjust their practice. This is consistent with the CDC pilot evaluation, which found that homeless consumers particularly valued case management and face-to-face contact with care coordinators more than they valued having choice and control or services, and considerably more than they valued budget transparency. One consumer from the homeless special needs group was interviewed. She had been receiving a home care package for about three years, having settled in a public housing property after many years of housing instability and homelessness complicated by financial difficulty, family conflict and severe health problems. She reported being generally satisfied with her care and services, and appreciates receiving the regular financial statements since she was transitioned onto a CDC package. However, she is dismayed by what she considers considerably reduced case management hours under the new arrangements. She has had the same care manager for many years and trusts her, but now feels that she is unable to access the same level of support and assistance that she previously did. Providers also referred to the time needed to establish relationships and build trust with homeless consumers (an issue that was also identified in the pilot evaluation), indicating that there is currently no financial provision for the ‘pre-planning’ time needed with consumers. Despite these concerns, providers report that the transparency provisions of CDC work very well for most consumers in this group and, similarly to mainstream consumers, care coordinators have adopted the budgeting tool as part of the care planning process. Overall, it is reported to have increased consumer participation and involvement in care planning. 4.7.7 Care leavers Care leavers includes the Stolen Generations of Indigenous people forcibly separated from their parents, the Forgotten Australians of people raised in institutional care settings during the 20th century, and former child migrants. Stakeholders interviewed for the evaluation indicated that there has been little substantive action to recognise and address the needs of this group in home care to date (what action there has been has focussed on the residential care sector). Unlike the CALD and LGBTI special needs groups, there is no national aged care strategy for care leavers. Often wary of authority, institutions and bureaucracy, care leavers may choose not to participate in traditional assessment processes. They often do not actively seek out services. They can experience early ageing as a result of long-term trauma and social isolation, and may require a trusted advocate to help them access aged care services. Since 2010, a number of community organisations, including a small number of aged care providers, have worked with the government to develop care leaver education and resources for the aged care sector. At the time of writing this report, the Department was working towards making the resources available to the aged care sector. Stakeholders suggest that there is a need for care leaver training, similar to what has occurred with the LGBTI special needs group, as well as allocating some dedicated care leaver packages. Comments relating to people who are homeless or at risk of becoming homeless are also broadly applicable to the care leavers group. 4.7.8 Parents separated from their children by forced adoption or removal There was insufficient information available to make any specific comment in relation to this group. 4.7.9 Lesbian, gay, bisexual, transgender and intersex people A minority of providers referred to the LGBTI special needs group at interview. Of those that did, one provider was working with a local LGBTI health organisation to obtain accreditation as an ‘LGBTI friendly’ aged care provider, and another was reviewing their promotional and information materials to ensure that they did not exclude LGBTI people. A third provider had several home care packages dedicated to LGBTI consumers, and spoke of the particular needs for this group including wariness of receiving services in their home, reluctance to disclose relationship status or personal circumstances, and early ageing issues due to long-term HIV treatment. Stakeholders indicated that the implementation of home care packages and CDC had only marginally addressed ongoing concerns for LGBTI older people. Consumer representative groups reported that many providers are still struggling to provide relevant information to LGBTI people. Although training and support projects such as the LGBTI Health Alliance’s Silver Rainbow are widely available and have been well-received, these are yet to reach the critical mass of providers necessary for them to have a discernible impact at this time. Stakeholders report that LGBTI consumers and carers often find the aged care assessments does not adequately consider or address their needs, and that it is a particular problem for people who do not use identity labels, those with disclosure and privacy concerns, people with intersex characteristics, men of trans experience (assigned 'female' at birth), women of trans experience (assigned 'male' at birth), and people with non-binary genders. LGBTI consumers commented that most providers are generally unfamiliar with LGBTI support organisations and activities, and do not know how to connect LGBTI people with their community. In addition, many mainstream support organisations for older people are not structured to cater for LGBTI people. For example, the Community Visitors Scheme has not, until recently, had any LGBTI community visitors. There is currently only one LGBTI visiting service (which operates in the same region as the only currently designated LGBT home care places). It is based in a metropolitan area and was established in 2012. • One consumer from this region was interviewed for the evaluation. He was connected to the visiting service through his home care provider, and he reported that the service had made an immense difference to his quality of life. Although he was very satisfied with the quality of care offered by his home care provider, and with the level of choice and control he had over his package, he still did not feel entirely free to be himself around his care workers. The volunteers from the LGBTI visiting service made him feel less isolated and this, he reported, had reduced the severity of depression he regularly experienced. He considered that the home care package and the visiting service complemented each other and that together they provided him with an improved quality of life. Stakeholders suggest that further training is needed for ACATs and providers, particularly on issues for people of trans experience, people with non-binary genders, and people with intersex variations. 5 Considerations for strengthening and improving home care and CDC This chapter draws on the findings from the evaluation to identify opportunities to strengthen and improve the Programme. This includes areas to support the conversion of all home care places to CDC by 1 July 2015, as well as longer-term considerations. Key areas identified include: • • • • • • • 5.1 supporting providers to implement CDC; strengthening the focus on re-enablement and wellness; clarifying the basic care interface; increasing knowledge of CDC across key agencies and services; trialing new approaches for underrepresented special need groups; improving the continuum of care; and increasing consumer control through self-directed funding and portability. Supporting providers to implement CDC Providers continue to require support to effectively implement CDC from both an administrative and practice perspective. From an administrative perspective there are two key areas that need resolution and / or support: • the Medicare claims process and the time taken for income assessments – it is noted that DHS established a specialist team to address the timeliness of income assessments, however complex assessments involving complicated financial structures do take more time to process – now that the processes are established, it may be helpful for DHS to disseminate some general information about processing times, as providers may not be aware of the degree of complexity in individual cases • the Information Technology (IT) upgrades required to link their client and financial management systems which are required to establish client-level cost centres and generate the individual monthly statements required for CDC. This is a costly and timeconsuming process, particularly for smaller providers. There is opportunity for providers to examine the feasibility of shared service arrangements for financial and IT management activity. This could be particularly beneficial for smaller providers, allowing them to focus on their service provision rather than financial and IT management. There a number of other areas where assistance could be provided to support more timely and effective transition to CDC. Such efforts could be targeted towards specific special needs groups whose needs may not be being met under current arrangements, or to regions where there are thin markets or potential market failure, for example in rural and remote environments. Support could include: • IT system adaption; • understanding cost of delivery and associated unit pricing of services; • service reorientation to enable more contemporary models of delivery within a CDC framework; and • practice development and support for care coordinators and care workers in CDC practice. Existing and developing practice could be leveraged more broadly to enable sharing of experience and practical support for application of CDC. This may include expanding the current repository of tools and mechanisms, as well as collating and sharing information and other relevant materials across the sector. Ideally, responsibility for leading this should come from within the sector itself. 5.2 Strengthened focus on re-enablement and wellness Re-enablement and wellness has yet to be embedded as a core objective of care and support with many providers unclear as to how to reorientate practice to do this. At this early stage of implementation, it is not unexpected that substantive progress has not been made in this area. However, there is a clear desire amongst providers to strengthen the focus on re-enablement and wellness for consumers, and this presents an opportunity to further the implementation of this policy objective. Documenting and disseminating good practice examples of re-enablement and wellness support could assist providers to examine their own practice and consider new ways of working with consumers and health providers to achieve this. At the time of report writing, a good practice guide for re-enablement and wellness in the context of the CHSP was being developed, with a focus on maximising consumer independence to prevent or reduce the need for ongoing care where possible (i.e. applying re-enablement and wellness approaches to basic support services, with the objective of preventing or delaying a need for ongoing home care and/or residential care). A similar guide could be developed for home care, highlighting and explaining exemplars, to show how re-enablement and wellness approaches can be applied to home care to prevent or delay the need for higher levels of care. 5.3 Clarifying the basic care interface The current service boundaries between home care Level 1 and the CHSP should be resolved as soon as possible, including addressing the perceived financial disincentive for eligible consumers to take up a lower level home care package. Demand (occupancy) of Level 1 places should be monitored over time to assess whether there is any change in demand once the CHSP boundary issues are resolved. Some providers already successfully utilise Level 1 places. Supporting material should be made available to the sector showing how Level 1 places can provide be a viable option for their service, and an attractive option for consumers. 5.4 Increasing knowledge of CDC across key agencies and services ACATs/ACASs, the AACQA, NACAP service providers and the Aged Care Complaints Scheme all require detailed knowledge and understanding of CDC policy and programme objectives. These agencies and services are key players in supporting decision making and access to packages and the effective implementation of CDC. A tailored package of information and education to uplift understanding of CDC amongst these agencies would help embed CDC within the aged care system. Any education activities aimed at ACATs/ACASs should include a particular focus on the benefits of CDC from a clinical perspective, explaining how individualised budgets translate into a package of care and supporting consumer-led decision making regarding health and wellbeing. 5.5 Trialling new approaches for under-represented special needs groups Many stakeholders consider that some special needs groups are under-represented in home care, and/or that their specific needs are not currently being met. Consideration should be given to trialling and evaluating new approaches for delivering home care in a CDC framework to these groups, with an objective of documenting and disseminating evidence on what works to meet their needs. From the evaluation findings there are three special needs groups that would benefit from this: • • • 5.6 People from Aboriginal and Torres Strait Islander backgrounds – there was consistent feedback from stakeholders that alternative models of CDC need to be developed for many, if not most, consumers who fall within this group, and that these models may include options for some communal use of package funds; Lesbian, gay, bisexual, transgendered and intersex people – although there has been considerable activity to address the specific needs of this group, it appears that the majority providers are still uncertain how to identify and address those needs, with many LGBTI consumers uncertain as to how they can safely articulate their individual needs to mainstream service providers; and Care leavers –this particular group have yet to be properly explored in the context of home care, and the anecdotal information suggests that they are not accessing services to the extent that might be expected. Improving assessment and the continuum of care The future potential for a single ACAT entry assessment should be explored, with an optional reassessment for moves between low and high care at the request of a provider or consumer. Stakeholders indicate there is limited clinical benefit in requiring a re-assessment for consumers to move from Level 2 to Level 3. The intended policy objective of requiring an ACAT/ACAS reassessment to move between low and high care relates more to the perceived need for an independent ‘gatekeeper’ than it does to the need for a clinical assessment. There are options for managing this gatekeeping objective without requiring an ACAT/ACAS re-assessment. For example, providers could be required to assess and document the need for a low care recipient to move to high care with a mandated tool (linked to the ACCR), and a regime of random audits could be put in place to ensure the quality and integrity of the assessments. Such an approach could potentially be trialled in a sample of aged care regions. Consideration should be given to adjusting the allocation process to better promote the continuum of care. In a fully operational CDC environment consumers would be able to access any assessed level of care through any provider of their choice. To facilitate this all providers could be allocated a minimum mix of all care levels. A consumers’ care level would then be able to increase without changing provider (i.e. an ageing in place policy, and places would be portable. This would require some adjustment and reconsideration of current policy and processes. 5.7 Increasing consumer control through self-directed funding and portability Consumers now have more choice of services and control of their budget, however they still have limited choice and control over the provider who holds their funds – and who, therefore, still holds authority in an entry-controlled market with minimal competition. Establishing portability by allocating subsidy funds directly to the consumer rather than the provider would significantly increase consumer control and give effect to the key objectives envisaged in the CDC policy discourse. This would require safeguards and consumer protections, together with fundamental change to the current operating environment and business models of home care providers. Providers would need to more actively identify and promote their service offerings and their value proposition to the marketplace, responding to consumer demand and preferences as part of a competitive and dynamic market. Consumer feedback to this evaluation suggests that they still feel somewhat disempowered through the lack of capacity to easily change provider, whether it be for poor performance or that they are no longer suitable to meet their changing needs or simply because they want a change. Portability of home care places would enable greater self-direction for consumers and support competitive market dynamics. Self-directed funding and portability are two key policy areas for consideration once CDC has reached a relative point of implementation maturity where this would be seen as the natural next steps in practice and market capacity. Learnings could be taken from the implementation of the NDIS where self-directed funding and portability are key policy objectives, and the provider market is undergoing significant reorientation. Appendix A Evaluation methodology This appendix sets out the evaluation methodology. Background The Home Care Packages Programme commenced in August 2013, with the commencement of a new 4-level care structure for home care places that replaced for former Community Aged Care Packages (CACP), Extended Aged Care at Home (EACH) places and Extended Aged Care at Home Dementia (EACHD) places to the new care levels. The care level structure is as follows: • • • • Home Care Level 1 – an individualised and coordinated package to support people with basic care needs with a Commonwealth subsidy of $21.43 per day or $7,822 per annum using 2014-15 rates (this care level did not exist prior to August 2013); Home Care Level 2 – an individualised and coordinated package to support people with low level care needs with a Commonwealth subsidy of $38.99 per day or $14,231 per annum using 2014-15 rates (this care level is equivalent to the former CACP places); Home Care Level 3 – an individualised and coordinated package to support people with intermediate care needs with a Commonwealth subsidy of $85.73 per day or $31,291 per annum using 2014-15 rates (this care level did not exist prior to August 2013); Home Care Level 4 – an individualised and coordinated package to support people with high care needs with a Commonwealth subsidy of $130.32 per day or $47,567 per annum using 2014-15 rates (this care level is equivalent to the former EACH and EACHD places). A number of new supplements were also introduced (including the dementia and cognition supplement and the veteran’s supplement, which each provide for an additional daily payment of 10 per cent of the daily care subsidy), that can be applied at any care level. The 2013-14 Report on the Operation of the Aged Care Act 1997 states that, as at 30 June 2014, there were 66,149 home care places nationally. Of these, 1,303 were Level 1; 50,157 were Level 2; 1,010 were Level 3; and 13,679 were Level 4. The Australian Government is gradually increasing the number of home care packages to 100,000 by 2017, with 40,000 additional packages over the following five year period to 2021-2. The aged care provision ratio for home care places (that is, the target number of places available for the number of people aged over 70 years) will increase to 45:1,000 from the current actual national ratio of 28.7: 1,000. Objectives of the Home Care Packages Programme The objectives of the Programme, as outlined in the Home Care Packages Programme Guidelines July 2014, are: • To assist people remain living at home; and • To enable consumers to have choice and flexibility in the way that their aged care and support is provided at home. The target population for home care packages is older Australians, particularly frail older people (although there are no minimum age eligibility requirements). A number of special needs groups are specified in the aged care legislation, specifically: • • • • • • • • • People from Aboriginal and Torres Strait Islander communities; People from culturally and linguistically diverse backgrounds; People who live in rural and remote areas; People who are financially or socially disadvantaged; Veterans; People who are homeless or at risk of becoming homeless; People who identify as lesbian, gay, bisexual, transgender or intersex; People who are care leavers; and Parents separated from their children by forced adoption or removal. In some cases, home care places may be specifically allocated to provide priority of access to particular special needs groups, however all home care providers are expected to ensure that their internal policies and practice ensures that services are accessible to people with special needs. Consumer-directed care (CDC) To facilitate choice and flexibility, all new home care places allocated since August 2013 are delivered within a consumer-directed care framework. At the time of the evaluation, there were around 1,000 existing CDC places from the 2010-12 CDC pilot, plus 5,835 places that were allocated in August 2013, and an additional 6,653 places that were allocated in December 2014 (during the evaluation period). All future places will be allocated on a CDC basis. By 1 July 2015, all existing home care places must convert to CDC arrangements. Many providers have been gradually transitioning their existing consumers to CDC arrangements since August 2013 as part of regularly scheduled home care reviews. The Home Care Packages Programme Guidelines July 2014 define CDC as follows: A way of delivering services that allows consumers to have greater control over their own lives by allowing them to make choices about the types of aged care and services they access, including who will deliver the services and when. Under a CDC approach, consumers are encouraged to identify goals, which could include independence, wellness and reablement. These will form the basis of the Home Care Agreement and care plan. Under CDC consumers have an individualised budget to give effect to their care plan, with providers holding and administering the budget on the consumer’s behalf. Commonwealth subsidies for supports are paid to the provider at a fixed amount by care level (which is the same for all consumers at the same care level, plus any additional supplements the consumer is eligible for). The consumer receives a monthly statement from the provider that reconciles income (i.e. Commonwealth subsidies and supplements, plus consumer fees and any additional consumer contributions) against expenditure and showing accumulated unspent funds in their individualised budget. Purpose of the formative evaluation The purpose of this formative evaluation was to identify any operational issues or possible adjustments required to strengthen the Home Care Packages Programme’s effectiveness, and to ensure the successful and complete conversion of all home care packages to CDC by 1 July 2015, as well as any areas requiring longer-term policy consideration. Evaluation questions An evaluation framework was developed in May 2014 to guide the data collection activities and to provide the data analysis and reporting approach for the evaluation. The framework identified the following evaluation questions: 1. How effective has the implementation of the Home Care Packages Programme (including CDC) been? 1.1 How well are the new arrangements working for home care providers and ACATs? This includes processes for implementing home care places, and the development and transition to CDC models of service delivery (including different models of CDC); effectiveness of the new care level structure and assessment processes; effectiveness of the intended graduated continuum of care between care levels; effectiveness of the Programme guidelines and information processes; and considerations for different types of providers. 1.2 How well are the new arrangements working for consumers? This includes understanding the range of care and services being accessed (including use of brokered services); application and impact of fees; consumer perceptions of choice and control; consumer engagement with individualised budgets and financial statements; effectiveness of information and advocacy services; and considerations for special needs groups 1.3 How well are the new arrangements working for the aged care system? This includes the interface with other aged care services such as the current Commonwealth HACC Programme (Commonwealth Home Support Programme from 1 July 2015); effects of the new arrangements on consumer demand and expectation; effects of the new arrangements on waiting times; and effects of the new arrangements on provider capacity and capability. 2. Are there any operational issues or possible adjustments needed to strengthen the Home Care Packages Programme’s effectiveness in meeting its objectives? Data collection methods There were three levels of data collection to gather the information needed to address the evaluation questions: • National data collection • Sample regions analysis • Targeted supplementary stakeholder consultations. National data collection This involved collection of information from home care providers. There were three methods of data collection: • Online survey for all 504 home care providers • Review of a sample of de-identified Ministerial correspondence and Departmental communications • Template report for home care providers delivering CDC places. These methods are described in more detail below. Online survey for all Home Care Packages Programme home care providers This method was used to collect information to address questions 1.2 and 1.3. The survey explored service provider experiences, views and insights with the Home Care Packages Programme implementation. This included: • Experience with the transition to and implementation of the new Home Care Packages Programme care levels • Perceived effectiveness of the new ACAT assessment arrangements • Information on the nature and extent of interface with other aged care services • Experience with the transition to and implementation of CDC (for those providers delivering CDC places). A link to the external online platform hosting the survey was distributed to all 504 home care providers by the Department. In the results analysis, home care providers were stratified by their sub-group (new CDC provider, ongoing CDC provider, non-CDC provider). Review of de-identified Ministerial correspondence and Departmental communications This method was used to collect information to address questions 1.1, 1.2 and 1.3. A qualitative coding analysis was conducted on a sample of de-identified Ministerial correspondence and Departmental communication logs from providers, consumers and carers. Template report for Home Care Packages Programme providers delivering CDC places The Excel template report sought six months of retrospective data from providers with home care places (up to and including places allocated in the 2013 ACAR round) to understand the range of supports provided under CDC places, the extent of brokered services, the level of care fees and consumer funding top-ups, and general information about the range of CDC tools and processes used by providers. The purpose of this request was to collect information that would demonstrate how CDC consumers are using their places, and thereby providing data to address components of evaluation question 1.1. Sample regions analysis This level of data collection involved a more in-depth focus in 10 aged care planning regions across all mainland states and territories except the Australian Capital Territory. The focus regions were selected with assistance from the Department based on identified characteristics of interest including a mix of different types of providers, regions and jurisdictions, and different mixes of consumers (including a proportion of consumers from special needs groups). The sample included a mix of: • Different types of provider (size, organisation type) • Different locations (jurisdiction, metropolitan, regional, rural/remote) • Providers specialising in or having notable proportion of consumers from special needs groups • Providers with experience of the CDC pilot as well as those that were new to CDC from August 2013 • Representation of all four care levels. There were four methods in this data collection tier: • Interviews with a sample of home care providers (25 in total across the 10 aged care planning regions) • Review of de-identified home care and CDC documentation from a sample of home care providers • Interviews with a sample of ACATs (13 in total, covering the 10 aged care planning regions – noting that ACAT catchments do not align to planning regions) • Interviews with a sample of consumers and carers/families from the sample of home care providers (roughly 2 per provider, or 55 in total). These methods are described in more detail below. Interviews with a sample of 25 home care providers This method was used to collect information to address questions 1.2, 1.3 and 2. The interviews explored provider experiences and insights concerning the transition to and implementation of the arrangements, key successes and challenges, lessons learnt and opportunities for improvement. The service providers were sampled from the following 10 aged care planning regions: • • • • • • • • • • Cabool (Queensland) Darwin (Northern Territory) Hume (Victoria) Metro East (South Australia) Metro North (Western Australia) Northern Metro (Victoria) Riverina Murray (New South Wales) Southern (Tasmania) Sunshine Coast (Queensland) Western Sydney (New South Wales). At least two and generally three service providers were sampled from each of the 10 regions. They were purposively sampled to ensure a mix of different provider sizes and type, different types of geographical regions, different levels of experience with CDC, and a mix of providers with notable proportions of clients from special needs groups. Review of documentation from a sample of providers This method was used to collect information to address question 1.2 and question 2. The selected providers were asked to provide a sample of de-identified Home Care Agreements (including consumer goals and care plans) and individual budget statements, copies of CDC and special needs group’s policies and procedures, and copies of information materials for consumers and carers. Interviews with a sample of ACATs This method was used to collect information to address questions 1.2, 1.3 and 2. The interviews explored ACAT experiences with and insights about the new arrangements, including the new assessment processes, the new care levels and supplements, and CDC arrangements. All ACATs and ACASs operating in the 10 aged care planning regions from which the providers, consumers and carers were drawn were invited to participate in an interview. As ACAT and ACAS catchments do not align to aged care planning regions, there were more ACATs and ACASs (n=13) than aged care planning regions (n=10) Interviews with consumers and carers/families This method was used to collect information to address question 1.1 and 2. The interviews explored consumer and carer experiences with the transition to new places and with CDC. The sample was drawn from a pool of expression of interest voluntarily submitted by consumers of the 25 home care providers (the providers distributed a general information sheet about the evaluation with an expression of interest form and Reply Paid envelope directly addressed to KPMG to their home care consumers; expressions of interest were collated confidentially by KPMG). Providers were not informed whether or not their consumers either submitted an expression of interest, or participated in an interview. In selecting the interview sample, the evaluation sought to include the following broad mix of characteristics: • • • Consumers/carers with experience of CDC places prior to August 2013 (i.e. continued from the CDC trial) Consumers/carers new to CDC from August 2013 Consumers/carers from a range of special needs groups, as well as people with dementia or their carers. The evaluation sought to establish a total sample of 75 consumers and carers (aiming for approximately half of each), however a number of consumers and carers who had initially expressed interest either declined when they were contacted for interview (due to changed circumstances, inconvenience of the proposed interview timing, or simply having forgotten or changed their mind), leaving a total final sample of 55. Selected service providers were asked to distribute an expression of interest for participating in an interview to all of their consumers (carers were also able to submit an expression of interest). The 55 consumers and carers were drawn from the pool of those that returned their expressions of interest to KPMG in a Reply Paid envelope (i.e. their providers were unaware of whether they had submitted an expression of interest or not). Selected consumers and carers were provided with an information sheet and consent form, in a format approved by a Human Research Ethics Committee specifically for this evaluation. Expressions of interest to participate in an interview were received from 125 consumers or carers (from a total pool of 1,342 home care packages administered to the 25 home care providers included in the evaluation interview sample; this is a response rate of about 9 per cent – not making allowances for places there were unoccupied at the time expressions of interest were distributed, and assuming that all providers distributed the expressions of interest). From the pool of 125 expressions of interest, a total of 55 telephone interviews were conducted with consumers and carers across Australia. Of these, 56 per cent were consumers (care recipients) and 44 per cent were carers. A breakdown of demographic details for the consumer and carer interviews is set out in the table below. Table 5: Demographic details of consumer and carer interviewees Aboriginal & Torres Strait Is. CALD Rural / remote Veteran Homeless Care leaver LGBTI Dementia Number 1 12 8 7 1 0 1 15 Percentage 2 22 15 13 2 0 2 27 Source: KPMG (note: there is no total column as some people fall into multiple categories). A number of critical special needs groups were under-represented in the expressions of interest pool (specifically, consumers and carers from the LGBTI, Aboriginal and Torres Strait Islander, care leavers, and homelessness special needs groups). The following actions were undertaken to redress this lack of representation: • • • • • • Interviews were conducted with several peak bodies and consumer reference groups (including the LGBTI Health Alliance and the Alliance for Forgotten Australians auspiced by Families Australia). A round table of metropolitan Indigenous stakeholders was held in Victoria which included several service providers, two consumers and one carer representative. An interview was conducted with an additional service provider servicing remote Australia including remote Indigenous communities. Interviews were conducted with 2 home care consumers and carers – one of whom was a client of one of the 25 service providers included in the evaluation sample and one of whom was not; both were recruited through the consumer outreach networks of the LGBTI Health Alliance. Additional written information on the experiences of LGBTI consumers and carers was provided from care coordinators at a service provider with dedicated LGBTI home care places (this provider was included in the evaluation sample). Additional written information on the experiences of consumers and carers at risk of homelessness or who have experienced homelessness was provided by service providers with dedicated homelessness home care places (this information was coordinated by LASA). • Additional written information on the experiences of consumers and carers from culturally and linguistically diverse consumers was provided by service providers with dedicated CALD home care places (this information was coordinated by FECCA). Attempts were also made to directly recruit additional consumers and carers from Aboriginal and Torres Strait Islander backgrounds for interview or participation in an informal focus group via direct approaches to two home care providers with significant proportions of Indigenous consumers, and a direct approach to one of the NACAP service providers. These attempts were not successful. Supplementary interviews with other stakeholder groups The final level of data collection involved conducting supplementary interviews with a targeted sample of other key stakeholder groups. These stakeholders are detailed below. Table 6: Schedule of evaluation consultations Organisation / agency Date(s) of consultation Leading Age Services Australia (LASA) February 2015 Aged and Community Services Australia (ACSA) February 2015 COTA Australia (formerly known as Council on the Ageing) February 2015 Carers Australia February 2015 Alzheimer’s Australia February 2015 Federation of Ethnic Community Councils of Australia – for comment on CALD perspectives February 2015 Families Australia (Alliance for Forgotten Australians) – for comment on care leavers perspectives February 2015 Australian Regional and Remote Community Services (ARRCS) – for comment on rural/remote and remote Indigenous perspectives February 2015 Focus group of Indigenous stakeholders from Victoria (3 service providers, two consumers, one carer, and Victorian Aboriginal Community Controlled Health Organisation) – for comment on metropolitan Indigenous perspectives November 2014 LGBTI Health Alliance – for comment on Lesbian, Gay, Bisexual, Trans-gender and Intersex perspectives February 2015 ACT Disability and Aged Care Advocacy Service – for comment on aged care advocacy perspectives February 2015 National Home Care IT Group – for comment on assistive technologies and digital solutions under CDC February 2015 Department of Social Services February 2015 Source: KPMG Evaluation governance and ethics The evaluation reported to the Home Care Packages Programme Section, Department of Social Services. KPMG met with the Department approximately every three weeks during the data collection and report writing phases of the evaluation. The Department approved the evaluation framework and data collection tools. The Department was advised by the National Aged Care Alliance (NACA) home care packages working group during the evaluation. KPMG presented to the NACA working group and the Department on two occasions during the evaluation period: prior to finalisation of the evaluation framework; and to present preliminary findings arising from the evaluation data collection. The consumer and carer consultation component of the evaluation, including the participant information sheets, consent forms and interview questions, received ethical approval from the Bellberry human research ethics committee (reference number 2014-05-271). The online provider survey was approved by the Australian Government Statistical Clearing House (Approval Number: 02408-01) Appendix B Provider survey – detailed tables This appendix sets out the detailed results from the online survey of home care providers conducted in December 2014 – January 2015. The survey was approved by the Australian Government Statistical Clearing House (Approval Number: 02408-01). The survey was comprised of 17 questions. To minimise the burden of responding to the survey, several filter questions were added into the structure of the survey. This ensured that only relevant questions were presented to respondents. The survey opened on 28 November 2014 and closed on 9 January 2015. It was distributed by the Department to providers via an email containing a link to an external secure online survey platform. Participation in the survey was voluntary and open to all home care providers. One reminder email was distributed by the Department during the survey period. A free call 1800 phone line and email address was established to respond to technical enquires about the survey. In total, only 5 emails and 4 phone calls were received in relation to the survey. In total, the survey was started by 410 respondents and data was submitted by 402. In 140 instances surveys were submitted without any answers being provided. These responses were not used in the analysis. Of the remaining 262, a further 96 were not used as they did not provide any data beyond the initial demographic questions. This left 166 valid responses to the survey that provided at least one response to the substantive questions in the main sections of the survey. Respondents were not required to answer every question. As such the responses to each question do not total 166. Accordingly, responses are presented in total numbers (as well as percentages where relevant). Respondent demographics Table 7. What is the aged care planning region where this service is located? (State) State or Territory Number of respondents Percentage of respondents New South Wales 48 32 Victoria 37 25 Queensland 31 21 Western Australia 14 9 South Australia 8 5 Tasmania 8 5 Australian Capital Territory 1 1 Northern Territory 1 1 148 100 Total responses Source: KPMG analysis of survey data Table 8. What is the aged care planning region where this service is located? Aged care planning region Number of respondents Aged care planning region Number of respondents Brisbane South 7 Southern Highlands 2 Eastern Metro 7 Wide Bay 2 Southern 6 Australian Capital Territory 1 Southern Metro 6 Cabool 1 Northern Metro 5 Darling Downs 1 South East Sydney 5 Darwin 1 Brisbane North 4 Eyre Peninsula 1 Central Coast 4 Great Southern 1 Gippsland 4 Kimberley 1 Hume 4 Mackay 1 Hunter 4 Mid North 1 Illawarra 4 Mid West 1 New England 4 North West 1 South West Sydney 4 West Moreton 1 Western Metro 4 Wheat Belt 1 Inner West 3 Yorke Lower North & Barossa 1 Metropolitan East 3 Total responses Northern 3 Source: KPMG analysis of survey data South West 3 Sunshine Coast 3 Western Sydney 3 Barwon South Western 2 Central West 2 Far North 2 Far North Coast 2 Fitzroy 2 Grampians 2 Loddon-Mallee 2 Metropolitan North 2 Metropolitan South 2 Metropolitan South West 2 Metropolitan West 2 Mid North Coast 2 Nepean 2 Northern Sydney 2 Riverina Murray 2 South Coast 2 140 TABLE 9. HOW MANY HOME CARE PLACES ARE ALLOCATED TO THIS SERVICE? Number of respondents Number of packages Level 1 Level 2 Level 3 Level 4 1 to 10 24 9 25 23 11 to 25 5 30 3 21 26 to 50 1 39 0 19 51 to 75 1 15 0 5 76 to 100 0 13 0 2 100+ 0 30 0 1 166 166 165 165 Total responses SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 10. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE ABORIGINAL AND TORRES STRAIGHT ISLANDERS? Percentage of consumers Number of respondents Less than 1% 106 1% to 10% 36 11% to 25% 1 26% to 50% 1 51% to 75% 0 76% to 90% 0 91% to 100% 1 Total responses 145 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 11. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE PEOPLE FROM CULTURALLY AND LINGUISTICALLY DIVERSE BACKGROUNDS? Percentage of consumers Number of respondents Less than 1% 62 1% to 10% 36 11% to 25% 22 26% to 50% 10 51% to 75% 2 76% to 90% 0 91% to 100% 10 Total responses SOURCE: KPMG ANALYSIS OF SURVEY DATA 142 TABLE 12. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE PEOPLE LIVING IN RURAL AND REMOTE AREAS? Percentage of consumers Number of respondents Less than 1% 91 1% to 10% 15 11% to 25% 9 26% to 50% 7 51% to 75% 3 76% to 90% 1 91% to 100% 16 Total responses 142 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 13. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE PEOPLE WHO ARE FINANCIALLY OR SOCIALLY DISADVANTAGED? Percentage of consumers Number of respondents Less than 1% 53 1% to 10% 23 11% to 25% 20 26% to 50% 13 51% to 75% 14 76% to 90% 11 91% to 100% 6 Total responses 140 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 14. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE PEOPLE WHO ARE VETERANS OF THE AUSTRALIAN DEFENCE FORCES, WAR WIDOWS OR WIDOWERS? Percentage of consumers Number of respondents Less than 1% 64 1% to 10% 60 11% to 25% 10 26% to 50% 2 51% to 75% 0 76% to 90% 0 91% to 100% 1 Total responses SOURCE: KPMG ANALYSIS OF SURVEY DATA 137 TABLE 15. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE PEOPLE WHO ARE HOMELESS OR AT RISK OF BECOMING HOMELESS? Percentage of consumers Number of respondents Less than 1% 104 1% to 10% 31 11% to 25% 4 26% to 50% 3 51% to 75% 0 76% to 90% 1 90% to 100% 1 Total responses 144 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 16. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE PEOPLE WHO IDENTIFY AS LESBIAN, GAY, BISEXUAL, TRANSGENDER OR INTERSEX? Percentage of consumers Number of respondents Less than 1% 114 1% to 10% 21 11% to 25% 0 26% to 50% 0 51% to 75% 0 76% to 90% 0 90% to 100% 0 Total responses 135 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 17. APPROXIMATELY WHAT PERCENTAGE OF THIS SERVICE’S CONSUMERS ARE CARE LEAVERS OR PARENTS SEPARATED FROM THEIR CHILDREN BY FORCED ADOPTION? Percentage of consumers Less than 1% Number of respondents 121 1% to 10% 15 11% to 25% 0 26% to 50% 0 51% to 75% 0 76% to 90% 0 90% to 100% 0 Total responses SOURCE: KPMG ANALYSIS OF SURVEY DATA 136 TABLE 18. WHICH OF THE FOLLOWING BEST DESCRIBES YOUR ORGANISATION? Organisation type Number of respondents Percentage of responses 12 5 126 54 Religious 21 9 Charity 23 10 Mutual 1 0 51 22 234 100 For profit Not for profit Community based Total SOURCE: KPMG SURVEY DATA ANALYSIS. NOTE MULTIPLE RESPONSES WERE ALLOWED MEANING TOTAL EXCEEDS 166 TABLE 19. WHICH OF THE FOLLOWING BEST DESCRIBES THE SIZE OF YOUR ORGANISATION? PLEASE SELECT ONLY ONE OPTION. Organisation size Number of respondents Percentage of responses Large (multiple sites across multiple states/territories) 39 26 Medium (multiple sites within 1 or more regions) 59 39 Small (single site service) 52 35 150 100 Total responses SOURCE: KPMG SURVEY ANALYSIS. These definitions of organisation size were developed specifically for this evaluation, based on descriptors used in previous data collection activities with aged care providers. It should be noted that they are not based on any formal or validated definition used by the Department of Social Services, the Australian Bureau of Statistics, the Australian Institute of Health and Welfare or any other Australian Government agency. There is currently no such formal or commonly used classification of provider size. Appendix C Survey results: Implementation of the Home Care Packages Programme TABLE 1. DID THIS SERVICE HAVE ADEQUATE INFORMATION AND SUPPORT ABOUT THE NEW ARRANGEMENT PRIOR TO THE TRANSITION TO HOME CARE PACKAGES BY AUGUST 2013? PLEASE SELECT ONE RESPONSE WHICH BEST DESCRIBES YOUR EXPERIENCE FOR EACH ELEMENT IN THE LIST. Yes, we have had adequate information and support about this We have had enough information, but some support/ guidance would have been helpful No, we have not had enough information or support Total responses to this question No. % No. % No. % No New package levels 1 and 3 38 27 73 51 32 22 143 Transition of CACP to package level 2 56 37 74 49 22 14 152 Transition of EACH to package level 4 48 35 66 49 22 16 136 Included care and services 51 35 67 45 29 20 147 Excluded care and services 41 28 67 46 36 26 144 New broad-banded ACAT assessments 36 25 58 39 54 36 148 Processes for consumers to transition between package levels 39 26 67 45 43 29 149 New dementia and cognition supplement 26 18 73 49 50 33 149 New veterans' supplement 28 19 58 39 61 42 147 Process for consumers to access oxygen and enteral feeding supplements between package levels 30 20 59 40 59 40 148 Consumer fees policy (from July 2014) 24 16 56 37 71 47 151 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 2. WHAT OTHER INFORMATION OR SUPPORT WOULD HAVE BEEN HELPFUL FOR YOU? PLEASE SELECT ONE RESPONSE WHICH BEST DESCRIBES YOUR OPINION FOR EACH OF THE ELEMENTS IN THE LIST. Written information packs and newsletters Information sessions and seminars Training sessions, workshops or conferences One-on-one support for providers Total responses No. % No. % No. % No. % No New package levels 1 and 3 29 28 33 31 29 28 14 13 105 Transition of CACP to package level 2 29 31 25 26 22 23 19 20 95 Transition of EACH to package level 4 29 33 26 30 18 21 14 16 87 Include care and services 30 32 28 30 23 24 13 14 94 Excluded care and services 36 35 30 29 26 25 11 11 103 New broad-banded ACAT assessments 40 36 38 34 27 24 6 5 111 Processes for consumers to transition between package levels 38 34 26 23 34 30 15 13 113 New dementia and cognition supplement 40 34 32 27 35 29 12 11 119 New veterans' supplement 45 38 31 26 34 29 9 7 119 Process for consumers to access oxygen and enteral feeding supplements between package levels 43 38 27 23 33 29 11 10 114 Consumer fees policy (from July 2014) 25 20 29 23 42 33 30 24 126 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 3. HOW EFFECTIVE HAS THIS SERVICE FOUND THE RESOURCES THAT SUPPORT THE HOME CARE PACKAGE PROGRAMME? PLEASE SELECT ONE RESPONSE. This resource has provided us with effective information and support This resource has been somewhat effective for us, but it could be improved This resource has not been effective for us We have not used this resource Total responses No. % No. % No. % No. % No Home Care Packages Guidelines 45 30 96 63 8 5 3 2 152 Australian Government aged care reform roadshows 16 11 65 44 40 27 27 18 148 Australian Government reform readiness checklist 17 11 69 46 36 24 28 19 150 Australia Government fees booklet 20 13 58 39 40 27 32 21 150 Australian Government websites 24 16 84 56 40 26 3 2 151 Australian Government email circulars to providers 30 20 82 55 33 22 5 3 150 Support from Aged and Community Services Australia 43 29 47 32 31 21 27 18 148 Support from the National Aged Care Alliance 20 13 47 31 39 26 44 29 150 Support from Leading Age Services Australia 24 16 49 33 28 19 47 32 148 Support from the National Aged Care Advocacy Service 14 9 34 23 37 25 63 43 148 21 62 41 28 19 28 19 150 Support from Home Care 32 Today (COTA) Source: KPMG analysis of survey data TABLE 4. PLEASE INDICATE YOUR LEVEL OF AGREEMENT WITH THE FOLLOWING STATEMENTS ABOUT THE HOME CARE PACKAGES PROGRAMME. PLEASE SELECT ONE RESPONSE WHICH BEST DESCRIBES YOUR EXPERIENCE FOR EACH ELEMENTS IN THE LIST. Strongly agree Agree Neither agree or disagree Disagree Strongly disagree Total responses No. % No. % No. % No. % No. % No. Staff at this service have a good understanding of the Home Care Packages Programme 30 21 80 55 23 16 7 5 5 3 145 Consumers and carers/families have a good understanding of the Home Care Packages Programme 4 3 31 21 39 27 47 32 24 17 145 ACATs/ACASs have a good understanding of the Home Care Packages Programme 6 4 33 23 54 37 37 26 15 10 145 The Guidelines provide a good balance between guidance and flexibility for providers 6 4 54 37 58 40 22 15 6 4 146 The Australian Government gives enough support and advice for providers on the Home Care Packages Programme 4 3 20 14 35 24 52 36 35 24 146 The Home Care Packages Programme has improved home care services for consumers 13 9 32 22 47 32 30 21 23 16 145 Most consumers are getting the right level of care and services they need under the Home Care Packages Programme 9 6 36 25 33 23 44 30 23 16 145 The Home Care Packages Programme has improved home care services for carers/families 13 9 33 23 48 33 28 19 23 16 145 The Home Care Packages Programme has increased the administrative burden on providers 88 61 33 23 12 8 4 3 8 6 145 Waiting times for ACAT/ACAS assessments have reduced with the new Home Care Packages Programme arrangements 3 2 16 11 62 43 28 20 34 24 143 Waiting times for consumers to access a package have reduced with the new Home Care Packages Programme arrangements 6 4 9 6 42 29 52 36 36 25 145 The Home Care Packages Programme offers more choice and flexibility for consumers 21 14 55 38 37 25 19 13 14 10 146 It is easier now for consumers to move between package levels 9 6 27 19 49 34 39 27 20 14 144 The Home Care Packages Programme providers a graduated continuum of care 8 5 64 44 40 27 20 14 14 10 146 Source: KPMG analysis of survey data Appendix D Survey results: Transition to Consumer Directed Care This section asked questions about providers experience in administering CDC packages. The subsequent questions were filtered based on respondent’s answer to this question. TABLE 5. DOES YOUR SERVICE PROVIDE ANY CDC PLACES? No % Yes 71 48 No 77 52 Total 148 100 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 6. WHEN DID THIS SERVICE FIRST PROVIDE CDC PLACES? Number of respondents Percentage of respondents Prior to 1 August 2013 15 21 After August 1 2013 36 51 Unanswered 20 SOURCE: KPMG ANALYSIS OF SURVEY DATA 28 TABLE 7: HOW DIFFERENT WOULD YOU SAY YOUR CDC MODEL IS FROM YOUR USUAL APPROACH TO HOME CARE (I.E THE APPROACH FOR NON-CDC PLACES)? PLEASE SELECT ONE RESPONSE WHICH BEST DESCRIBES YOUR EXPERIENCE FOR EACH OF THE ELEMENTS ON THE LIST. The CDC approach is very different to the usual approach The CDC approach is somewhat different to the usual approach The CDC approach is the same as the usual approach Total responses No % No % No % No Assessment process 29 43 19 28 20 29 68 Care planning process 31 46 20 29 17 25 68 Involvement of carers/families in care planning process 26 38 21 31 21 31 68 Cost of care and service delivery 41 59 16 23 12 17 69 Consumer choice of care and service delivery 34 50 21 31 13 19 68 Provider approach to administration of the places 46 68 14 21 8 12 68 Provider approach to case management 40 59 20 29 8 12 68 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 8. HAS THIS SERVICE ENCOUNTERED ANY SIGNIFICANT PROBLEMS DURING THE IMPLEMENTATION OF CDC? PLEASE SELECT ONE RESPONSE WHICH BEST DESCRIBES YOUR EXPERIENCE FOR EACH OF THE ELEMENTS IN THE LIST. This has been a significant problem for us This has been somewhat of a problem for us This has not been a problem for us Total responses No % No % No % No Unanticipated extra administrative burden or overheads 41 62 21 32 4 6 66 Training staff to a CDC approach 13 20 28 42 25 38 66 Explaining CDC to consumers 17 26 38 58 11 17 66 Explaining CDC to carers/families 15 23 35 53 16 24 66 Insufficient package budget to meet consumer needs 24 36 26 39 16 24 66 Consumer unable or unwilling to engage with CDC 11 17 33 50 22 33 66 Insufficient choice of care and services available in the area to meet consumers' need and preferences 5 8 14 21 47 71 66 Insufficient choice of providers in the area to meet consumers' need and preferences 4 6 15 23 47 71 66 Providers in the area increasing their prices for care and services 7 11 32 49 26 40 65 Consumers declining care services assessed as being essential for their health and well-being 15 22 36 54 16 24 67 Consumers wanting to access excluded or inappropriate services 7 11 28 42 31 47 66 Consumers wanting to 'save' funds or a contingency higher than 10% of their budget 3 5 23 35 40 61 66 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 9. PLEASE INDICATE YOUR LEVEL OF AGREEMENT WITH THE FOLLOWING STATEMENTS ABOUT CDC. PLEASE SELECT ONE RESPONSE WHICH BEST DESCRIBES YOUR EXPERIENCE FOR EACH OF THE ELEMENTS IN THE LIST. Strongly agree Agree Neither agree nor disagree Disagree Strongly disagree Total responses % No % No % No 9 13 2 3 0 0 70 32 27 39 15 22 4 6 69 12 17 40 57 9 13 7 10 70 3 22 32 36 53 5 7 3 4 68 4 6 27 39 31 45 5 7 2 3 69 CDC places have increased administrative burden on providers 44 64 19 28 6 9 0 0 0 0 69 The increased administrative requirements have been a significant challenge for us 33 48 26 38 8 12 2 3 0 0 69 Most consumers benefit from a CDC approach compared to a non-CDC approach 11 16 31 45 19 28 3 4 5 7 69 CDC makes providers more accountable to consumers 32 47 22 32 9 13 2 3 3 4 68 The benefits to consumers outweigh the challenges of CDC 20 29 18 26 21 30 5 7 5 7 69 No % No % Staff at this service have a good understanding of CDC 15 21 44 63 Consumers and carer have a good understanding of CDC 1 1 22 ACATs/ACASs have a good understanding of CDC 2 3 The broadbanded assessment process work well 2 The Guidelines provide a good balance between guidance and flexibility in relation to CDC No Strongly agree Agree No % No % Our approach to CDC has changed over time as we have learned more 20 30 30 45 Our approach to CDC is still evolving as we learn more 25 37 31 The approach to CDC needs to be 26 38 23 different for some special needs groups SOURCE: KPMG ANALYSIS OF SURVEY DATA Neither agree nor disagree No Disagree Strongly disagree Total responses % No 1 1 67 1 0 0 68 1 1 1 68 % No % 15 22 1 1 46 11 16 1 34 17 25 1 No Appendix E Survey results: Preparing for Consumer Directed Care The 77 respondents that answered ‘No’ to question 10. (Does your service provide any CDC places?) were directed to the following section which asked about providers preparedness, sources of information and concerns regarding the transition of all packages to CDC arrangement on July 2015. The denominator used to derive percentages for this section is 77 unless otherwise stated. TABLE 10. HOW WOULD YOU DESCRIBE THIS SERVICE’S CURRENT STATE OF PREPARATION FOR THE TRANSITION OF ALL PLACES TO CDC FROM 1 JULY 2015? PLEASE SELECT ONE RESPONSE WHICH BEST DESCRIBES YOUR EXPERIENCE. Statement Number of respondents Percentage of respondents We are still preparing for the implementation of CDC 56 73 We are well prepared for the implementation of CDC: our tools and processes are developed, managers and staff are trained and systems are in place 14 18 We have not commenced preparing for the implementation of CDC 4 5 Unanswered 3 4 Total 77 100 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 11. WHAT ACTIVITIES (IF ANY) HAS THIS SERVICE UNDERTAKEN, OR DOES THIS SERVICE PLAN TO UNDERTAKE, TO PREPARE FOR THE IMPLEMENTATION OF CDC FROM 1 JULY? Activity Number of respondents Percentage of respondents Attendance at non-government workshops, seminars or conferences 65 84 Reading Department of Social Services website information and email circulars 65 84 Internal training or change management activities for managers 56 73 Support/advice from provider peak bodies or advocacy groups 56 73 Attendance at Australian Government information sessions or roadshows 55 71 External training or change management activities for managers 51 66 Use of Home Care Today Home Care Provider web portal and/or phoneline 39 51 External training or change management activities for staff 39 51 Use of Home Care Today Home Care Consumer web portal and/or phoneline 27 35 Other 16 21 SOURCE: KPMG ANALYSIS OF SURVEY DATA TABLE 12. WHAT CONCERNS DOES THIS SERVICE HAVE ABOUT THE IMPLEMENTATION OF CDC FROM 1 JULY 2015? Number of respondents We are very concerned about this We are somewhat concerned about this We are not concerned about this Total responses Problem or issue No. % No. % No. % No. Lack of shared understanding about CDC across the home care sector 34 46 34 46 6 8 74 Lack of information and support for providers about CDC 38 51 30 40 7 9 75 Lack of clarity in the Guidelines about CDC 28 37 34 45 13 17 75 Concern about how to manage consumers who want 'trade off' required care and services2 41 55 27 36 7 9 75 Concern for our business model viability under a CDC approach 52 69 17 23 6 8 75 Need for more training and mentoring about CDC for our managers 34 45 25 33 16 21 75 Need for more training and mentoring about CDC for our staff 36 48 32 43 7 9 75 Concern about capacity of consumers and nominated representatives to engage with CDC 49 65 25 33 1 1 75 New administrative and reporting requirements may be too onerous 57 77 16 22 1 1 74 Concerns about the provider payments system 60 81 13 18 1 1 74 Difficulty in pricing our services 43 57 29 39 3 4 75 Difficulty in brokering other services 28 37 27 36 20 27 75 Uncertainty about whether CDC really is better for consumers 40 55 26 36 7 10 73 Concern about how to deliver CDC approaches for special needs groups 34 46 31 42 9 12 74 37 52 26 37 8 11 71 Not enough 'good practice' examples to draw on Source: KPMG analysis of survey data 2 This refers to the provider’s perceptions around balancing their duty of care with principles of consumer choice and control (i.e. how to manage a situation where a consumer does not want to use the package funds to purchase care and services that the provider considers are important to maintain their health and wellbeing) Appendix F Summary of key service provider data: range and cost of supports delivered under CDC This appendix provides a summary of the information obtained from data provided to the evaluation by 163 CDC service providers using an Excel-based template. Providers were asked to report data for a retrospective six month period (January 2014 to June 2014). Range of supports accessed Providers reported that consumers on CDC or transitioning to CDC packages were not making significant changes to their support arrangements, and were still accessing ‘core services’ such as personal care, help with household tasks, and clinical (nursing) care. Similarly, consumers accessing a package for the first time were also choosing to use their package on core services. Differences between consumer preferences for CDC and non-CDC consumers were observed for supports to access social and community-based activities, transport, and in some cases specific equipment designed to increase independence (and not available through other programs). The table below indicates that the most common support types accessed by CDC consumers. The table illustrates that for level 1 and 2 consumers the most common support types accessed are personal care services, support services (help with household tasks), and support with leisure, interests and activities. Level 3 and 4 consumers are using their package budget for similar services, though a higher proportion of support expenditure is used for client-related transport. This is unlikely to be significantly different for non CDC package care consumers. TABLE 13: MOST COMMON SUPPORT TYPES ACCESSED (PROPORTION OF SUPPORT EXPENDITURE) Services Level 1 Level 2 Level 3 Level 4 Personal care services 26% 29% 40% 37% Support services 48% 40% 31% 25% 2% 6% 3% 10% 10% 8% 5% 7% Nutrition, hydration, meal preparation & dietary services 1% 3% 5% 4% Activities of daily living 8% 8% 5% 4% Clinical care 1% 1% 4% 4% Client-related transport Leisure, interests and activities SOURCE: KPMG ANALYSIS OF PROVIDER SERVICE DATA Note that some providers reported data for all package care consumers, rather than for CDC consumers, hence this data does not fully reflect the supports accessed by CDC consumers The figure below illustrates the proportion of support expenditure by different categories of support (care services, support services, clinical services and other). Again, these proportions are unlikely to be significantly different for non CDC package care consumers. The figure shows that a greater proportion of a CDC level 3 or 4 package is spent on clinical and other services compared with a level 1 or 2 package, and a higher proportion spent on care services such as personal care and assistance with activities of daily living. FIGURE 12: EXPENDITURE ON SUPPORTS, BY SUPPORT CATEGORY AND CARE LEVEL SOURCE: KPMG ANALYSIS OF PROVIDER SERVICE DATA Note excludes expenditure on administration and case management/coordination Note that some providers reported data for all package care consumers, rather than for CDC consumers, hence this data does not fully reflect the supports accessed by CDC consumers In-house and brokered services Providers reported that there was a tendency for consumers to choose in-house services (services provided by the CDC package provider). Providers stated that in the main consumers chose their services as they were often cheaper than brokered services which meant that the consumer was not incurring additional administrative and coordination fees which would be charged for arranging brokered services. They also stated that consumers chose in-house services due to their level of trust and confidence in the package provider, and the convenience of having all services provided by one organisation. Providers stated that consumers had the option of using their package for services provided by other organisations (for example, if they preferred a care worker from another organisation, or they wanted to access a service not provided by the package care provider). However the extent to which providers gave consumers information about brokered service options varied. In many cases providers stated that they explained to consumers ‘in a general sense’ the options to broker services at the planning stage, though they did not always present information on the services available from other organisations or the prices of these services (whereas they would present this type of information for their own in-house services). Further, it was noted that there is an incentive for CDC providers to encourage consumers to use their own in-house services – to ensure that their organisations had a steady revenue stream and remained viable. Based on expenditure data reported by providers, 60 per cent of CDC support expenditure is for services provided by the package care provider (that is, in-house services). This varies across care levels: a higher proportion of support expenditure was used for in-house services for consumers on a level 1 or 2 package, compared with consumers on a level 3 or 4 package – overall and for individual service categories. In-house service provision varies across support categories, with higher rates of in-house service provision for care services (personal care, assistance with activities of daily living) – as illustrated in the figure below. FIGURE 13: PROPORTION OF SUPPORT EXPENDITURE ON IN-HOUSE SERVICES, BY SUPPORT CATEGORY AND CARE LEVEL SOURCE: KPMG ANALYSIS OF PROVIDER SERVICE DATA Note excludes expenditure on administration and case management/coordination Note that some providers reported data for all package care consumers, rather than for CDC consumers, hence this data does not fully reflect the supports accessed by CDC consumers The table below illustrates the proportion of support expenditure used for in-house services, by individual support type (as reported by providers). TABLE 14: PROPORTION OF SUPPORT EXPENDITURE ON IN-HOUSE SERVICES, BY SUPPORT TYPE Support type Management of skin integrity % of expenditure in-house 100% Activities of daily living 86% Leisure, interests and activities 80% Nutrition, hydration, meal preparation & dietary services 79% Personal services 62% Support services 56% Access to other health and related services 51% Clinical care 46% Continence management 40% Client related transport 33% SOURCE: KPMG ANALYSIS OF PROVIDER SERVICE DATA Note excludes expenditure on administration and case management/coordination Note that some providers reported data for all package care consumers, rather than for CDC consumers, hence this data does not fully reflect the supports accessed by CDC consumers Costs per unit (hour) of service were calculated based on data reported by providers – for both in-house and brokered services, and these are reflected in the table below. The data does not fully support claims that brokered services are more expensive than in-house services, and for a number of different support types, brokered services are less expensive. TABLE 15: UNIT COSTS REPORTED BY PROVIDERS – IN-HOUSE AND BROKERED SERVICES, BY CARE LEVEL AND SUPPORT TYPE Level 1/2 Level 3/4 In-house Brokered In-house Brokered Personal services $41.23 $53.88 $47.93 $45.65 Activities of daily living $48.38 $51.41 $47.85 $65.01 Nutrition, hydration, meal preparation & dietary services $33.09 $20.16 $36.90 $34.57 Management of skin integrity $50.84 na $49.96 na Continence management $69.53 $20.86 $72.85 $21.48 Support services $38.50 $39.45 $41.29 $40.46 Leisure, interests and activities $37.99 $30.15 $42.99 $36.48 Clinical care $75.18 $32.27 $63.33 $75.36 Access to other health and related services $68.89 $90.83 $56.22 $80.36 $2.04 $4.70 $2.71 $8.54 Average cost per hour Care services Support services Clinical services Other Client-related transport (cost per trip) SOURCE: KPMG ANALYSIS OF PROVIDER SERVICE DATA Appendix G Summary of key themes and issues from Ministerial and Departmental correspondence This appendix summarises the key themes and issues arising from an analysis of de-identified Ministerial and Departmental correspondence and communications relevant to the Home Care Packages Programme and CDC, which was provided by the Department. Analysis of Ministerial correspondence KPMG also undertook a review of a sample of de-identified responses to Ministerial correspondence relating to home care and CDC. Much of this correspondence (n=13) related to waiting times to receive a home care package. In most cases, the Minister or his delegate responded by clarifying the availability of, and release schedule for, packages in the person’s area. The Minister or his delegate also recommended that the consumer/carer stay in close contact with their provider, as well as to accept a lower level package (level 1 or 2) as an interim measure. Waiting times was not a significant issue for the majority of consumers and carers interviewed for the evaluation (although it was a concern in some cases), however the issue was raised by providers and ACATs in some areas. Some of the Ministerial correspondence related to concerns by consumers or their carers in relation to the quality of supports they were receiving (n=4), the cost of supports (n=4), or the ability to access particular supports (n=4). In all cases of service quality concerns, the Minister or his delegate responded to by referring consumers to the Aged Care Complaints Scheme. This range of concerns is broadly similar to the range of issues identified in the consumer and carer interviews for the evaluation. A number of people wrote to the Minister with concerns regarding becoming ineligible for state-based support programmes as a result of taking up a home care package. The Minister usually replied by indicating that this was a matter for their own state government. This issue was not directly identified in the consumer and carer interviews conducted for the evaluation, although it was identified (usually in relation to aids and equipment) in discussions with some other stakeholders, including an aged care advocacy service provider. The following figure provides an indication of the range of issues identified in the correspondence, and their frequency. FIGURE 14: THEMES OF MINISTERIAL RESPONSES TO LETTERS REGARDING THE COMMONWEALTH HOME CARE PACKAGES PROGRAMME Waiting time for HCPs Access to services Cost of services Service quality concerns Resulting ineligibility for state-based programs Carers support Charged for services while away from home Enquiry topic Cost of interpreting services Aged care funding Aids and equipment Insufficient package size Medication management OHS restrictions on care providers Oxygen supplement Payment system issues Red tape Reduced services Respite fees Specific subsidy for macular degeneration Tax queries 0 2 4 6 8 10 12 14 Frequency SOURCE: KPMG ANALYSIS OF DE-IDENTIFIED MINISTERIAL CORRESPONDENCE (DSS) Analysis of Departmental telephone and email enquiries The Department received a considerable number of enquiries by telephone, email and letter in 2014. An analysis of a de-identified sample 197 enquiries was undertaken, which is summarised in the following figure. The qualitative themes have been arranged in order of highest frequency, and then by alphabetical order. FIGURE 15: HOME CARE PACKAGES PROGRAMME TELEPHONE AND EMAIL ENQUIRIES BY ENQUIRY TOPIC AND SENDER TYPE Care and service provision Financial report Care fees query Miscellaneous and general Home Care Packages availability Leave queries CDC issues Administration costs enquiry Unders and overs/funding level cuts Aids and equipment Enquiry topic Legislative clarification Guidelines issues Formative home care evaluation Supplements Input to briefing/coord Aged care reform clarification Respite Quality of care principles Interface with other programmes Software issues Security of tenure Provider number queries Financial management query Combining Home Care Packages Clarification of effect of changes CDC reforms ACAT assessment queries 0 5 10 Key to enquirer type: Aged Care Complaints Scheme Departmental Minister's office Other Service provider SOURCE: KPMG ANALYSIS OF DE-IDENTIFIED DSS ENQUIRY LOGS 15 20 25 Frequency Consumer Dr MP/Senator's Office Other Commonwealth Department State Government body 30 The most frequent enquiry topic was in relation to care and service provision (n=30), followed by financial reporting f (n=26), care fees (n=25) and miscellaneous or general enquiries relating to the administration of the Programme (n=23). Enquiries in relation to care and service provision were mostly generated by service providers (n=11) and consumers (n=8) and sought to clarify whether certain supports could be provided under the guidelines. Examples of questions are set out below. Can a client’s daughter be the sole contractor for the provision of his home care services? (Service provider) Is dental care covered under the package? (Service provider) Can people on any level of package access Centre Based Day Respite care services? (Service provider) Is the list of care services in the guideline a suggested list only and not a comprehensive list, so that as long as we don't fund any services from the excluded list we can tailor the package to the individual? (Service provider) I would like clarification regarding what I am and what I am not able to use home package funds for. (Consumer) Can service providers refuse to lift the care recipient because they have a ‘no lift’ policy? (Carer) As can be seen from these examples, the majority of these enquiries sought clarification of information that was already available in the programme guidelines (or assistance in interpreting that information). Enquiries in relation to the financial reporting topic were mostly from service providers (n=23). Most of these related to specific acquittal processes, changes to their financial accountability requirements and the availability of acquittal templates for financial reports to clients (it is noted that such templates are available from the COTA website). Enquiries about care fees were predominantly from service providers (n=14), with some correspondence from consumers (n=5). These queries varied in nature, with service providers enquiring about the status of income assessments and technical funding questions, and consumers raising concerns about the cost of their care or enquiring about the rules of their package. These issues were also regularly raised in the provider and consumer and carer interviews conducted for the evaluation