Varicose Veins - Middlesex Surgical Associates
advertisement

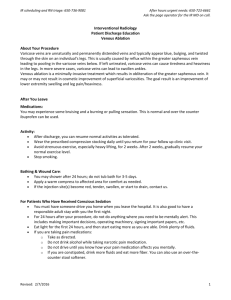
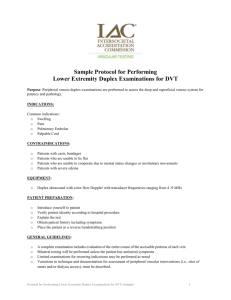
Knowing Your Vein Problems Varicose Veins Chronic Venous Insufficiency Deep Vein Thrombosis What Are Veins? Blood circulates throughout the entire body using a network of blood vessels. With each heartbeat, your blood is pumped from the heart to the rest of the body and then it returns back to the heart. Veins carry the blood back to the heart. When veins are damaged they have difficulty returning blood to the heart and can cause vein problems ranging in severity. Types of Veins: There are three types of veins that work together to carry blood back to the heart in your legs. Superficial veins are located just beneath the skin and move blood from the skin and surface tissues. They drain into the deep veins. Deep veins are located in the muscles of the legs and carry 80-90% of blood back to the heart via the inferior vena cava. Perforating veins connect superficial veins and deep veins. How Do Leg Veins Function? In order to move blood up the legs toward the heart, the veins and leg muscles work together against gravity. Along the inside walls of veins are flaps called valves that work like one-way doors. When the leg muscles contract, the valve opens and blood is pushed up deep veins. When the muscle relaxes, the valve closes and prevents blood from traveling back down the vein. Healthy veins have strong valves that keep blood moving in the correct direction. What Are Damaged Veins? Damaged Veins have weak walls or valves that are not strong enough to fully close the valves. Therefore, when the leg muscles relax, blood will leak back though the valve via gravity. This can also affect the health of other valves. The blood will travel to the next healthy valve, and the increase in blood will cause an increase in pressure. The extra pressure will eventually weaken the valve and the healthy valves below it. Thus, instead of the blood moving up the leg toward the heart, blood will began to pool in the vein. Consequently, varicose veins may form, swelling may occur in the leg, and blood clots may develop in veins where the blood is moving inefficiently. What are Varicose Veins? Varicose veins are abnormal superficial veins that become enlarged. Varicose veins are most often caused by damaged valves that do not close properly. The increase in pressure causes the veins to bulge out and become visible under the skin. Varicose veins often run in families and are common during the pregnancy. Some varicose veins may cause uncomfortable symptoms or may be a cosmetic concern: either way, treatment will help. Symptoms Bulging veins that appear as blue or green ropes in the legs (calves, thighs, behind the knees) Sting or ache in legs especially after prolonged standing or sitting Swelling in ankles or feet Itching Brownish or reddish discoloration of the skin Treatment for Varicose Veins To treat your varicose veins, your doctor may recommend you have a procedure. These procedures will either destroy or remove your damaged veins. There are many extra superficial veins in your leg and therefore destroying or removing your problem veins will not affect your leg function. Your blood will reroute using healthy veins. Endovenous Ablation Endovenous ablation is a minimally invasive procedure that uses heat to destroy a damaged vein. The heat source, radiofrequency (RF) or laser, is guided by a catheter into the vein. When the heat source is removed, it seals off the vein. Because the procedure is minimally invasive, you will be able to return to your normal routine soon after the procedure. Microphlebectomy Microphlebectomy uses short incisions to remove small varicose veins. A special hook is used to pull out the vein. It is often used with endovenous ablation or ligation with stripping. You may return home a few hours after surgery and recovery may take a few days. Ligation with Stripping Ligation with stripping is a surgical procedure performed to remove one or both saphenous veins. Incisions are made at both ends of the vein and the vein is tied off at both places. The vein is then removed using the lower incision. You may return home a few hours after surgery and recovery may take weeks. What is Chronic Venous Insufficiency? Chronic venous insufficiency (CVI) is an ongoing medical condition that occurs when varicose veins worsen or when a blood clot prevents valves from working properly. These damaged valves prevent your legs from pumping enough blood back to the heart and results in blood to pooling in the veins. The increased pressure in the veins causes to the legs to swell which can damage skin resulting in open wounds, inflammation or venous skin ulcers. Your doctor can provide you with steps to relieve symptoms and limit risk of ulcers. Symptoms Swelling in the lower legs and ankles Calves may feel tight Legs may feel tired, heavy, or achy Skin is dry, itchy, or discolored (red or brownish tinge) New formation of varicose veins Formation of ulcers How to reduce symptoms? To reduce your systems, you will need to follow daily self-care steps. You will need to wear elastic compression stockings and elevate your legs above heart level. This will help lower the pressure in your leg veins, thus helping to decrease swelling and prevent ulcers. Ulcers can result from CVI If high pressure and swelling caused by CVI are not controlled, CVI will worsen causing more serious symptoms. Skin and surface tissues will break down increasing the chances of ulcer formation. Ulcers form in different shapes and sizes and often develop on the lower legs and ankles. Ulcers are watery and seep fluid. Because of inefficient blood flow and swelling to the skin, they take a longer time to heal. How to treat an ulcer If you believe you have an ulcer, contact your doctor right away and follow your doctor’s home care instructions. Steps may include: Elevate legs and wear elastic bandages or compression stockings to reduce swelling Apply various dressings to the ulcer. The dressings are often moist and have medications that will improve healing. Dressings may need to be changes very 1-2 weeks Your doctor may prescribe antibiotics to fight infection You may be referred to the Winchester Wound Healing and Hyperbaric Center to further treat your ulcer. What is Deep Vein Thrombosis? A deep vein thrombosis (DVT) is a blood clot that develops in a deep vein. With time, the blood clot can enlarge and eventually block the vein. This increases blood pressure in the vein and results in damaged veins with weakened valves. You do not need to have a vein problem to be at risk for DVT. DVT often develops when blood is moving too slowly such as after prolonged periods of inactivity. Part of the blood clot may fall off and travel to the lungs. This will cause a pulmonary embolism, which can be fatal. Symptoms Usually affects only one leg Symptoms may not occur if the body is able to break down the clot on its own May experience pain and/or swelling Sudden, continuous pain in deep muscle is common Pain may increase after walking or standing still for expended period Treatments for DVT A DVT is treated in order to restore blood flow in a vein and to prevent a pulmonary embolism and more DVTs from occurring. The treatment works to control the clot size and prevent additional clots from developing. Medications are usually prescribed first and if the medication is not effective, other procedures may be necessary in order to destroy a large clot or reduce chances of pulmonary embolism. You doctor will suggest your best treatment option. Anticoagulants Anticoagulants, or blood thinners, are often the first step in treatment for DVT. These medications help prevent blood from clotting. You will be prescribed more than one anticoagulants and at first they be given via IV or injections, then later by mouth. You doctor will provide you with medication instructions. You may need regular blood tests in order to make sure your medications are working properly and make any adjustments. While taking your anticoagulants, check with your doctor before using other medications. Additionally, watch your diet closely. Certain foods alter the effectiveness of anticoagulants, so follow the diet provided by your doctor. Thrombolysis Thrombolysis dissolves large clots by using a catheter. The catheter is guided into the affected vein and x-rays are taken of the vein and clot. A special clot-dissolving medication is then infused into the clot via the catheter. Sometimes, a mechanical device is additionally used to break up the clot. Inferior Vena Cava Filter An inferior vena cava (ICV) filter is a device that traps a blood clot in the lower body, thus preventing a pulmonary embolism. The filter is guided by a catheter and inserted in the inferior vena cava. This procedure will be performed if you have a blood clot in your leg and are at risk for a pulmonary embolism and cannot take blood thinning medications. Self-Care Steps You Can Follow To Prevent Vein Problems These self-care steps can reduce your chances of further vein problems no matter what vein problem you have. Self-care is the simplest form of treatment and very effective if done every day. Therefore, it is important to follow your doctor’s instructions and stick to your daily self-care program. Compression Stockings: Wearing elastic compression stockings helps vein problems and will help relieve symptoms. The stockings fit around the ankle and reduce pressure as they extend up the leg. The stockings keep blood flowing toward the heart; therefore it is less likely to pool in the legs. Thus, swelling and the risk of ulcers are reduced. Your doctor will prescribe stockings at a safe pressure for you. Talk to your doctor before purchasing them. Exercise: Exercise helps to promote blood flow from your legs and back to the heart. Elevation: By elevating your legs above your heart level, you can prevent blood from pooling in the leg veins. This will reduce swelling. Keep Blood Moving: When sitting or standing for extended periods of time, do leg exercises (writing letters of alphabet with toes, heel raises) every half hour to improve blood flow. Healthy Weight and Diet: Being overweight can add extra pressure on your veins. Also try to limit your sodium intake which causes your body to retain water and increases swelling.