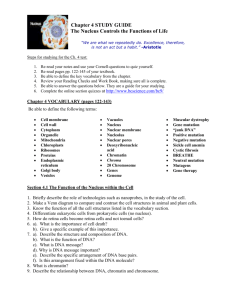
Genetics Chart
advertisement

List of Diseases/Disorders/Conditions detailed in Lectures 1-9 (10-11 don’t have any new conditions) Lecture 2: Chromosome Abnormalities: NONDISJUNCTION & ANEUPLOIDY AUTOSOMAL TRISOMIES Disease/Disorder Type of mutation Inheritance Symptoms Genetic Test Trisomy 18 (Edwards Autosomal Trisomy Non-disjunction Mental retardation, failure to thrive, severe heart Syndrome) 47, XX, Typical Karyotype defects, micrognathia, malformed ears, clenched +18 FISH fists w/ overlap. 2nd and 3rd digits, rocker-bottom -screening- PAPPfeet A is reduced in affected Trisomy 13 (Patau Autosomal Trisomy Non-disjunction Midline defects- holoprosencephaly, cyclopia, Syndrome) 47, XX, Typical Karyotype micropthlamia, absence of eyes, cleft lip and +13 FISH palate, rocker-bottom feet, congenital <3 and urogen. Defects Autosomal Trisomy Trisomy 21 (Down 1) 95% meiotic Hypotonia, short stature, short neck, flat nasal -Typical Karyotype Syndrome) nondisjunction bridge, protruding tongue, open mouth, short -FISH 2) 4% Robertsonian broad hands, transverse palmar crease, IQ= 30-Screening for translocation (14,21) 60 chromosome 3) 1% mitotic nondis.-congenital heart defects, leukemia, and early anomalies requires mosaic onset Alzheimers use of four analytes-First trimester screening for two analytes MSAFP and uE3 low Pregnancy associated plasma protein A (PAPPwhile hCG and A) low and b-hCG (high)both placental Inhibin are higher -First tri. Detection- 2 products- achieve a detection rate of 75% for analytes- PAPP-A fetal Down and free b-hCG -Ultrasound measurements of excess folds of skin increase detection to 86% SEX CHROMOSOME ANEUPLOIDY Turner Syndrome (45, Sex chromosome 1) 50% by 45, X Often detected at puberty in females X) monosomy karyotype Short stature, weebed neck, shiled chest with -Typical Karyotype 2) 25% mosaic wide-spaced nipples, lymphedema of hands and 3) 15% isochromosome feet, gonadal dysgenesis (streak gonads), of X (replace p arm primary amenhorrea, infertility, inc. risk for with second copy of q) cardiovasc abnormalities, intelligence normal Klinefelter Syndrome Sex chromosome 1) non-disj. During Tall stature, thin and long legs, hypogonadism, (47, XXY) monosomy meiosis infertility, gynecomastia, learning difficulties -Typical Karyotype 2) 15% Mosaic karyotypes Chromosome abnormalities in structure CHROMOSOME STRUCTURE: BALANCED REARRANGEMENTS Miscellaneous *80% are female *95% aborted spont. *Infants rarely survive past 1 month, *75-80% spont. Aborted *Three genetic events can account for Tri 21 *Risk of recurrence with Roberstonian Trans. ONLY- 12% for mothers and 3% for fathers 1/ 4000 livebirths Only viable monosomy 1/1000 (males) CML- Chronic Myelogenous Leukemia (46, XX t(9;22)(q34;q11) Reciprocal Translocation -Typical karyotype -SKY 1) reciprocal translocation -fusion of 2 genes bcr-abl increased and mislocalized tyrosine activity - Results in dominantly active kinase CML -Oncogenes created or activated by a chromosomal translocation Philadelphia chromosome= 22 Two derivative chromos carrying material from both chrom 9 and 22 -Because bcr-abl fusion is not found in normal cells, it is a perfect target for Gleevec- anticancer drug Chromosome abnormalities in structure CHROMOSOME STRUCTURE: UNBALANCED REARRANGEMENTS Cri-du-Chat (46, XX, Unbalanced 1) Deletion of Patients cry with a characteristic epicanthal del(5p15) rearrangement chromosome material folds, cat-like sound, mental retardation, karyotype microcephaly, low-set ears, heart defects Prader-Willi Syndrome (15q11-13) Deletion of imprinted gene karyotype 1) Paternal deletion of imprinted gene 2) Uniparental disomy Morbid trunk obesity, cognitive impairment, small hands and feet, short stature Deletion of 1) Maternal deletion of Children with devel. Delay, mvmt or balance imprinted gene imprinted gene problems,, microcephaly, seizures, abn EEGs karyotype 2) Uniparental disomy Lecture 3: Molecular Genetic Abnormalities: Molecular mutations that alter INDIVIDUAL GENES 1) MUTATIONS IN EXONS Disease/Disorder Type of mutation Inheritance Symptoms Genetic Test Missense mutation in Sickle Cell anemia Autosomal coSickling of RBCs – crisis- extreme pain, EXON- point dominant splenomegaly, jaundice, chronic ischemic leg mutation in 6th aa (Bulcers globin protein) HbS/A= sickle cell trait- heterozygote genotype= clinically norm but may show -heterozygote symptoms under low O2 pressure detection pre- Uniparental disomy= both copies of an individual’s chromosomes are maternally or paternally derived Angelman Syndrome (15q11-13) pregnancy (esp in blacks) -IEF (isoelectric focusing) – first screening -HPLC- confirmation -Gene therapy Miscellaneous Treatment- turn on expression of fetal hemoglobin genes by drug treatment/bone marrow transplant *try to treat symptoms *Heterozygote advantageincreased resistance to death from malaria *HbS allele is high freq (1/250) in areas where malaria is endemic *AFRICAN AMERICAN pop **black male/female- hereditary predisposition to develop hemolytic anemia after taking sulfa/other drugs Neurofibromatosis Nonsense mutation in EXON- early termination codon of NF1 gene Autosomal dominant NF1 gene is mutated cannot inactivate Ras highly active Ras promotes excess growth in Schwann cells benign neurofibromas *Lisch nodules (abn. Growths of the eye) *café-au-lait spots- less severe form *scoliosis, thinning of the bones in arms and legs, seizures, learning dis, and high BP Treatment- routine removal of neurofibromas *remaining normal copy is susceptible to second mutagenic hit Breast Cancer (familial) Frameshift mutation in EXON -genetic linkage study -single gene tests (limited bc so many genes involved) -Prenatal predictive diagnosis -Pre-symptomatic genetic testing Dominantly-inherited increased risk of devel. Breast/ovarian cancers Inactivation of BRCA1 gene by frameshift mutation (insertion/deletion that is not a mult of 3) -Appearance of breast cancer in a patient under age of 45 or cases of breast cancer in 2 or more close relatives is from familial mut. In BRCA1 *(lecture 5)- involvement with DNA repair pathway (ATM pathway) and genomic instability *BRCA2- assoc with 10-20% of male breast can 80% of patients with a mutated BRCA1 will develop breast cancer by age 70 -BRCA1 and BRCA2 muts account for 5% of breast cancers -heterozygous women consistently lose the 2nd normal copy 2 hit hyp. -incomplete penetrance Cystic Fibrosis Mult. Of 3 ins/del in CFTR gene Autosomal recessive 68% of cases = F508 mut in CFTR gene Treatment- interventions to minimize mucous accumulation and treatment of infections *whites- 1/25 chance of carrying the mutation -allelic heterogeneity Autosomal dominant Mutation loss of Phe protein misfolding Cl- channel is defective Cl- is not efficiently pumped out of lung cells water into lung cells remaining lung secretions are viscous and thick= found in lungs, pancreatic ducts, reprod. Systems *pulmonary infections, abn heart rhythms -Carrier testing- test for the most common 23 CF mutations and the most common is F508 Expansion of CAG repeat in exon (normal is 635 repeats vs. 36-121+ repeats in affected) -anticipation occurs and is manifest in the age of onset -CAG repeat expansion incr. size of glutamine tract polyglutamine domain huntingtin accumulates in nuclear inclusions or protein aggregates -Neuronal degeneration, increased number of involuntary movements, dementia, seizures Inheritance Symptoms Miscellaneous Huntington’s Disease Carrier testing (heterozygote testing rec.) esp for Caucasians -Sequence exons only- where most common muts are TRINUCLEOTIDE repeat (CAG) in EXON of huntingtin gene -Prenatal predictive diagnosis -Presymptomatic genetic testing -PCR/gel electro- for detecting repeats 2) MUTATIONS IN INTRONS Disease/Disorder Type of mutation No cure Patient usually dies within 17 years of diagnosis Phenylketonuria (PKU) B-thalassemia Genetic Test Mutation in INTRON of phenylalanine hydroxylase (PAH) gene PKU biochemical testing is required for newborns Point mutation in Bglobin gene – prevents normal splicing Autosomal recessive Trinucleotide repeat expansion in INTRON 3) MUTATIONS IN PROMOTER REGION Disease/Disorder Type of mutation Genetic Test Hemophilia B Small deletion or point mutation in promoter of factor IX gene Fragile X Trinucleotide Repeat in PROMOTER region (CGG) in Treatment- reduce dietary intake of Phe for life Deficient activity PAH In absence of treatment, severe to profound retardation occurs Autosomal recessive Point mutation in B-globin gene- destroys splice site, creates new sites, enhances donor sites Mutation reduction in B-globin production excess alpha to beta globin subunits precipitate destruction of RBCs and their precursors anemia *failt to thrive without treatment *with treatment- regular transfusions and chelation therapy= can live to 20-40s Autosomal recessive GAA expansion in intron of FRDA1 (frataxin gene) expanded (200-900) acts as a cryptic 3’ splice site OR formation of a structure that prevents transcription of the gene basically, UNKNOWN mechanism -Friedreich’s Ataxia = loss of voluntary muscle, enlargened heart, live to avg. age of 37 Inheritance Symptoms Miscellaneous X-linked Recessive (more common in males) Mutation in factor XI gene prevents binding of TF HNF-4 factor IX gene expression falls to below 5% deficiency in factor IX protein fibrinogen is not cleaved to fibrin malfunctioning in clotting cascade *Extreme bleeding in response to minor lesions X-linked recessive (more males affected) CGG expansion in promoter of FMR1 increases number of CpG dinucleotides in CpG island of promoter when expansion > 200 repeats, CpG dinucs are methylated silenced Treated b addition of clotting factors from blood donors or recombinant factor IX by genetic engineering *Factor VIII is mutated in Hemophilia A (90% of hemophilia cases) -Southern blotting used to detect CGG repeat expansion in promoter and the methylation status of the gene. DNA is -Heterozygote detection prior to pregnancy (Mediterranean; Asians) -Gene therapy Friedreich’s Ataxia Inablity to remove introns recessive allele that produces a defective protein product protein cannot convert Phe to Tyr incr. phe= toxic to brain and can cause mental retardation Variable subtypes B0 = no detectable B-globin B+ = variable amounts of reduction and slightly less severe presentation *Italian-American or GreekAmerican have a 1/12 chances of carrying the mutation *Chinese have 1/20 chance of carrying mut for Alpha-thal FMR1 gene In 5’UTR -Molecular analysis for common mutations -Southern Blotting expression of FMR1 gene -mental impairment in 1/2000 male, long faces, large ears, prominent jaws, irregular teeth, macroorchidism (larger testicles) 4) MUTATIONS IN 3’ Untranslated Region ((UTR) Disease/Disorder Type of mutation Inheritance Genetic Test Myotonic Dystrophy TRINUCLEOTIDE Autosomal dominant repeat expansion in 3’ -Molecular analysis for common mutations -Prenatal predictive diagnosis 5) Mitochondrial disorders Disease/Disorder Type of mutation Genetic Test MERFF/MELAS Mutation in mitochondrial DNA -Fragile X associated tremor/ataxia syndromeassociated with pre-mutation allele (pre-mut allele may lead to development of FXTAS digested with EcoRI sites flank the promoter and a methylation sensitive restriction enzyme EclXI—only digests unmethyl. DNA so it is able to distinguish b/w expanded/ unmethylated alleles and expanded/methylated affected alleles Symptoms Miscellaneous CTG repeat in 3’UTR of DMPK gene--? Compromises the mRNA’s stability or makes the mRNA a target for translational repression by CTG repeat-binding miRNAs dec. expression of DMPK myotonic dystrophy *classical symptoms of myotonia- prolonged muscle contraction and relaxation, muscular dystrophy, hypogonadism, frontal balding, arrhythmia Inheritance Symptoms Maternal descent- 100,000 mito in eggs vs. 100 in sperm Heteroplasmy- variance in inheritance because mitochondria are inherited with the cytoplasm in which segregation is not regulated so fraction of mitochondria that are inherited varies Miscellaneous A woman with a mitochondrial disorder has children who are at risk for developing the same disorder, regardless of their gender. If her oocytes have a higher % of mutant mito than her body- she will be asymptomatic but children can be affected Lecture 4: Gene regulation and Development INHERITED BIRTH DEFECTS Disease/Disorder Achondroplasia Type of mutation Genetic Test Mutations in the receptor for FGF (fibroblast growth Inheritance Symptoms Miscellaneous Inherited birth defect Mutations in FGF receptor activate the FGFR3 receptor even in absence of ligand inhibition of chondrocyte Controversial therapies 1. growth hormone therapy 2. surgical lengthening of lower factor) Holoprosencephaly proliferation within the growth plate shortening of long bones and abn. Differentiation of other bones Mutations in SHH result in vastly different phenotypes bc there are diff in modifier loci variable expressivity legs Sex determination is very sensitive to gene dosage- some XY individuals who are heterozygous for certain genes are sex reversed and develop as females bc a single dose of these genes (SOX9, WT1, or SF1) is not enough for normal testis develop. HAPLOinsufficient 8% of all pediatric cancers 1) 25-50% chromosomal abn. 2) 30-40% single gene (SHH gene) defects 3) mutations in SHH gene, TGIF, SIX3, ZIC2 Point mutation/del/translo Of SRY gene Inherited birth defect Inherited birth defect SRY XY female- appear normal but lack copy of 2 X, do not develop secondary sexual characteristics, don’t menstruate, have streak gonads SRY XX males- develop as males but missing critical genes from Y- unable to promote normal sperm develop. Believed to develop from malignant transformation of renal system cells that remain undiff. -WT1 gene, glypican-3 gene affected Lecture 5: cancer genetics and Genomics CANCER Disease/Disorder Type of mutation Genetic Test Sporadic Oncogene-based tumors Inherited birth defect Associated with WAGR syndrome that is characterized by susceptibility to Wilem’s tumor WT1 gene- complex- encodes multiple proteins- a modulator of transcription Inheritance Symptoms Sex reversal Wilms’ Tumor Both genetic and envt. Causes Can be caused by ingestion of cyclopamine (from corn lilies) Acquired mutations in oncogenes such as ras, myc, src Act in a dominant fashion Homozygous Recessive Mutations cause Chromosome instability syndromes Xeroderma Mutation in gene Autosomal Nucleotide excision repair is defective problems pigmentosum required for recessive with repairing the type of damage in DNA upon Nucleotide excision exposure to UV radiation Show variable expressivity Genetic heterogeneity= cam ne caused by mutations in multiple genes Locus heterogeneity- mutations in diff genes can case the same clinical phenotype Miscellaneous Wear UV protective suits, get significant sunburns/ blistering, median age for skin cancer = <10 Ataxia telangiectasia Fanconi anemia Bloom Syndrome repair Mutation in ATM gene Genetic lesions in proteins interacting with ATM gene -heterozygote testing rec. Mutation in a protein complex that interacts with ATM/Fanconi prot -heterozygote testing rec.- Autosomal recessive Autosomal recessive Autosomal recessive Hypersensitive to ionizing radiation bc ATM mutation prevents proper DNA damage repair for doublestranded breaks *symptoms = loss of balance, slurred speech during toddler years, cerebellar degen, radiosensitivity, sterility, immunodeficiency, pre-disp to develop tumors Sensitive to ionizing radiation and agents that cause double-stranded breaks *symptoms- bone marrow failure, skeletal abn, increased risk of malignancy Acutely sensitive to ionizing radiation *symptoms- severe growth deficiency, early menopause, recurrent infections, more susceptible to tumor-devel yo Patients should be spared repeated exposure to radiography and have surveillance for tumor development Higher prevalence in Ashkenazi Jews. Patients should be spared repeated exposure to radiography and have surveillance for tumor development Patients should be spared repeated exposure to radiography and have surveillance for tumor development TUMOR SUPPRESSOR GENE INACTIVATION Retinoblastoma Mutation in RB1 gene (tumor sup gene) (TSG) Although TSG harbor recessive loss of function mutations, they appear to be inherit. In a dominant fashion Two-hit hyp- hetero carrier of RB1 mutation has a high prob of getting a second mutation in the good copy retinoblastoma tumor *Acquiring a hereditary mutation in TSG predisposes an individual to the effects of a loss of heterozygosity (LOH) = dominantly inherit. The predisp for acquiring a mutation in the single wild type allele Li-Fraumeni syndrome Mutation in p53 gene P53 important for cell cycle regulation. Mutant p53 predisposes individual to a large variety of cancers that arise when second copy of p53 is inact. OTHER CANCERS – Mentioned in regards to expression profiling in cancer diagnostics Disease/Disorder Type of mutation Inheritance Symptoms Genetic Test Diffuse Large B-cell Expression profiling, Two main subtypes of DLBCL Lymphoma (DLBCL) hierarchical clustering 1) germinal center b-like subtype had more fave outcome 2) activated b-like subtype less fave. Breast cancer Expression profiling Two subtypes- Her2 and luminal epithelial cell-like tumor types- different response for each to taxol treatment basal epithelial < luminal epithelial Incompletely penetrant- some pp have the predisposition for RB but don’t develop Miscellaneous Importance of testing to differentiate bw two subtypes Importance of testing to differentiate bw two subtypes Prostate cancer survival rate Two subtypes id- each subtype seemed to correspond to upreg of expression of a particular small set of biomarkers- these signs could serve for faster single gene tests for prostate cancer Expression profilinghierarchical clustering Lecture 7: Genetic Screening and Prenatal Diagnosis Disease/Disorder Type of mutation Inheritance Genetic Test Hemochromatosis Most common Autosomal mutation- (C282Y) recessive -DNA analysis -Population screening Symptoms Miscellaneous Iron overload disorder- primarily affects the liver (cirrhosis), heart, pancreas (diabetes), skin (bronzing) and testes (atrophy) -**Affects Caucasians- 1/10 but fewer because of reduced penetrance** -Population screening is more controversial than DNA analysis Frequency of abnormalities relates to degree of elevation of maternal Phe during pregnancy Maternal PKU -Newborn screening Congenital hypothyroidism -Newborn screening via measurement of thyroxine followed by TSH Usually sporadic Non-syndromic Deafness -Two Connexin-26 gene mutations (mst common) -Mutation in connexin30 gene DNA mutation analysis -heterozygote detection prior to pregnancy Autosomal recessive If uncontrolled results in about double the risk for spontaneous miscarriage (24%) and increased risks of intrauterine growth restriction for fetus (40%) microcephaly (73%), psychomotor retardation (92%), congenital heart defects (10%) Deficient in circulating thyroid hormone, thyroxine -prolonged jaundice, enlarged tongue, abdominal distension, muscle hypotonia, delayed skeletal maturation, -Failure to initiate timely treatment = neurologic damage w/ mental retardation, growth retardation Goal is to initiate treatment within 3 weeks of birth Non-syndromic deafness is not associated with additional abnormalities Tay-Sachs Disease Screening for heterozygotesHexosaminidase A screening Blood sample DNA analysis for common mutations Screening for Autosomal Recessive Affected children usually die between ages 2-5- fatal neurodegenerative disease Canavan disease Importance of testing to differentiate bw two subtypes Severe neurodegenerative lethal condition with death 1/4000 babies born -Racial/ethnic differences -Black infants have 50% the rate of white infants -Hispanics have 40% higher than whites -Common mutation or common Ashkenazi Jew mutation *Whites- have a 1/31 chance of carrying the mutation -Prevalent in Ashkenazi Jewish population but with success of screening, number of Tay-Sachs births to Ashkenazis is less than those for non-Ashkenazi jews -Increased frequency in French Canadians too -heterozygote frequency heterozygotes=Detected prenatally-DNA analysis for 3 mutations assists in detection of heterozygotes Familial dysautonomia -Molecular analysis for common mutations Screening for heterozygotes- DNA analysis for 2 mutations assists in the detection of heterozygotes in 99% cases often by 10 years of age approximates 1/40 Ashkenazi jews -Ashkenazi jew- 1/40 Progressive neurodegenerative condition that may have a variety of sensory/neuronal disturbances and a decreased life expectancy Common features include alacrima (lack of tearing), absence of lingual fungiform papilla, impaired taste, hypoactive or absent deep tendon reflexes, vasomotor instability, indifference to pain and temp Lecture 8: Testing for disease susceptibility Disease/Disorder Type of mutation Inheritance Symptoms Genetic Test Disorders in chapter but already detailed above: Huntington’s disease, PKU, CF, Fragile X Duchenne’s Muscular X-linked dystrophin x-linked Progressive deterioration of muscle tissues and Dystrophy (DMD) gene recessive weakness in the childhood yrs- most patients unable -linkage testing in to walk at 12 years old. families Lecture 9: Genetic Frontiers Disorders in chapter but already detailed above: SCID, Sickle cell anemia, Hemophilia B, B-thalassemia, CML Disease/Disorder Type of mutation Inheritance Symptoms Genetic Test Acute Lymphoblastic Childhood leukemia caused by low activity of TPMT Leukemia (ALL) Pharmocogenetics used enzyme—> prevents methylation and inactivation of as a treatment to detect 6MP accumulation of 6MP converted into a toxic low TPMT activity byproduct that inhibits DNA replication Diabetes Microarray analysis Complex disease in which microarray is used to determine factors contributing to disease Obesity Microarray analysis Complex disease in which microarray is used to determine factors contributing to disease AIDS Gene therapy via RNAi delivery of genes Miscellaneous Miscellaneous Charts specific for lectures 6-9 Lecture 6: ID Genetic basis of disease Phenotypic Variability Markers for variability SNPs- Single Nucleotide Polymorphisms Loci in the genome where the sequence varies at the position of a single nucleotide from person to person Alternative splicing Mechanism of genome variation uses different combos of splicing sites from the same gene to produce mature mRNA molecules that exhibit differential use of the gene’s exons= protein products with different combos of segments encoded by various exons Copy Number Variation (CNV) Regions of the genome that differ in the total number of copies per genome in diff people. Can include regions that are deleted, duplicated, inserted, otherwise altered -Bias AGAINST deletions in genecontaining regions vs. bias FOR duplications in gene-cont. regions Epigenetic modifications Contribute to phenotypic variability as seen by 50% of genes that show 2-4 fold allelic variation in expression levels -results from differential expression of genes, particularly at imprinted loci -differences in long-range enhancers can also lead to variability 0.1% of genomic variability -3 SNPs/ kilobase (3 million SNPs) -80-85% in exons -1500 unique sites of CNV -12% of the genome Lecture 6: ID Genetic basis of disease Study designWhat it tests for: Tests for genetic Basis but does not investigate Genetic Basis of Disease what the specific genetic contributions are Familial clustering Tests for a genetic basis Compares the probability of developing a disorder for a relative of the affected proband versus a member of the general population Twin studies Adoption studies Study designLinkage studies Standard Linkage analysis- Affected Sib Pair Analysis Tests for a genetic basis Compare concordance of developing the disorder in monozygotic vs. dyzygotic twins where concordance= the phenotypic similarity of the pair of twins in question Tests for a genetic basis Strong method of identifying the role of genetics in disease Scientists compare monozygotic twins who have been raised in different families to see if they show the same propensity toward developing a disease- nature vs. nurture What it tests for: Tests to identify the genes themselves that lead to a particular phenotype Based on the principle that genes whose loci are close together will often be inherited together. Understand the Mechanism by which genes sort during meiosis easiest level of sorting is with chromosomes themselvesfirst separate from homologs then from sister chromatids resulting gamete has a single copy of each chromosome, purely by chance. Through meiotic recombination, genes are randomized so an ind. Will inherit maternal chromosome that is a combo of both their mother’s chromosomes. Genes that are close to each other are often inherited together = linked genes LINKAGE ANALYSIS- takes advantage of this and looks for loci that seem to segregate more often with the disease phenotype than with chance search for markers that show an overrepresentation of nonrecombinant offspring with the parental haplotype -subjects from families with multiple cases of a partic. Disease are genotypes and the markers are analyzied to id a locus where the particular allele seems to cosegregate with the disease at a sign. Freq. -Then construct a haplotype (series of alleles found at linked loci on a single copy of a chromosome) and compare- est. a region of interest then use Human Genome project to determine genes in that region Complication- require specific and hard to find family structure Alternate study design that relies on the principles of linkage seeks to Result Those disorders that are influenced by a genetic contribution will show significantly increased risk for immediate fam members amd modestly inc. risk for distant fam members If disorder is genetic basis, higher degree of concordance in mono vs. dizygotic twins Practically, to id monozygotic twins who know their biological origins, who have one or both siblings who are affected by a particular condition is a difficult proposition. Not used often. Result -To identify loci throughout the genome that might be linked to the disease gene, linkage analysis uses a panel of silent DNA markers -Three types 1. RFLPs 2. SSLPs 3. SNPs These linked markers should be transmitted alongside the disease gene a high fraction of the time, and mathematical analysis in the form of LOD score can confirm that these cotransmissions are stat. significant and due to tight genetic linkage. -parametric analysis- requires use of a genetic model that describes the mode of inheritance, penetrance, the gene freq, and the # of loci involved -Large pedigrees with mult cases of affected ind needed to gain enough statistical power -Potential problem- DNA samples aren’t id loci throughout the genome that segregate with the disease trait -Uses samples only from affected siblings who can share 0, 1, or 2 of their marker alleles but if a certain marker is linked to a disease gene, one would expect to see a skewing of the distribution of allele sharing in affected siblings. -Next step- evaluate the statistical significance for the various marker loci tested Complications- cannot distinguish IBS from IBD Study designAssociation studies Case control study Transmission disequilibrium test What it tests for: Association studies specifically look for a statistical assn between an allele and a disease phenotype in the general population = linkage disequilibrium Design: most common study design in the genome-wide assn study group (GWAS). Divide the population into 2 groups, the affected group and an unaffected control group look for a diff. freq of marker alleles bw the two groups no need to find subjects with any particular family structure but the control group must be PERFECTLY matched Complications- any imperfection in control matching can result in spurious associations Developed to avoid complications of doing a case control with imperfectly matched controls -Internal controls in the form of parental genotypes measure the deviation from expected transmission of a maker allele from a hetero to its affected offspring -SNP markers useful because they are less mutable and are more densely spaced -complication- requires parental samples collected from the parents of the affected and so it isn’t possible to distinguish between situations where allele sharing results from Identity by state or identity by descent. IBS= when both parents have a copy of the same allele for a given marker locus IBD= two siblings inheriting the same copy of an allele from the same parent Correct for this by choosing a marker (SNP) that has multiple, LOW FREQ alleles = less likely that the 2 parents will have the same allele for a given marker Miscellaneous Example of case control gone wrong- chopstick study where it was found that “a gene exists which controls both eye color and ability to use chopsticks” except that the two groups were not controlled for ethnically. If a marker allele is not associated with a particular phenotype, then it and the second allele in the hetero parent should be transmitted to an affected offspring with equal probability -If a marker IS associated with a disease phenotype, then it will statistically OVERTRANSMIT to affected offspring General Principles for Screening: 1. The disorder should be an important problem (morbidity and mortality), such as common occurring conditions 2. The disorder or condition should be common (prevalence and incidence), sufficiently high so cost-benefit is justified. Screening for a disorder of short duration is not recommended. Rather, those with long pre-clinical duration (breast, cervical, colon cancers) offer opportunity for benefit from screening. 3. 4. 5. 6. The disease/condition should have a readily available and acceptable treatment or remedy Screening tests should be accurate in terms of sensitivity (high), specificity (high), and predictive value Screening should be relatively inexpensive- benefits should far outweigh costs Screening procedures should be acceptable by both patient and society- tests should be safe and provide a minimum of discomfort Lecture 7: Genetic Screening and Prenatal Diagnosis—types of genetic screening Screening Type Description Mass screening of a population for bp, blood sugar or cholesterol levels Population Screening aims to assist people in recognizing that they need special medical attn bc of their risk profile Newborn Genetic Screening Screening for Heterozygotes Mandated in all states for specifically named biochemical genetic disorders Key elements of BIOCHEMICAL GENETIC screening are to recognize disorders for which treatment is necessary in order to avoid develop of mental retardation -screening for Severe Combined Immunodeficiency (SCID) –disorder that is uniformly fatal by one year if not treated with a bone marrow transplant- before 3 months has the best outcome—most affected individuals do not have a family history so newborn screening is a good strategy. Affected have low or absent T-cells tests quantify T-cell receptor excision circles (TRECs). Normal individuals will have a high number of TRECs while those with SCID will have decreased #s at birth and few detectable TRECs -Hearing loss screens- 50% of hearing loss is inherited; 70% of which is non-syndromic vs. 30% assoc with addl abnormalities (syndromic)Mutation Analysis Screening for Tay Sachs-disease- screening by assay for the lysosomal enzyme hexosaminidase A if half the activity of the enzyme = heterozygosity for Tay Sachs it is less reliable or when the patient is taking an oral contraceptive -A more reliable test is a second blood sample or DNA analysis for the common mutations= 98.6% accurate -Hexosaminidase A screening is extremely effective bus also associated with a number of false pos results- largely related to the serum hexosaminidase assay being done during an est. pregnancy w -success of screening has reduced the number of Tay-Sachs births to Ashkenazi Jewsand more affected babies are born to non-jewish couples Examples Pap-smears to detect cervical cancer Prostate cancer screening- men > 50 years Mammography- for breast cancer Colon cancer- stool screening Transferrin saturation- best test for diagnosis of hemochromatosis -PKU -Congenital hypothyroidism -Inborn errors of metabolism including Galactosemia, Maple Syrup Urine disease-CF (but controversy because CF screening often associated with false pos. results and some evidence suggests that early diagnosis may make no difference -SCID- 1/50,000 births -Newborn hearing screening programs- institute early intervention (hearing aids). -non-syndromic deafness- most common cause is having 2 connexin-26 gene mutations- use DNA mutation analysis -Prevalent in Ashkenazi Jew population— between 1/27 and 1/30 Ashkenazis carry a Tay-Sachs gene mutation with about 1/3600 births being an affected ind.= 100x more frequent than non-Ashkenazi -Increased frequency among French-canadians where the carrier risk is similar to that for Ashkenazi Jews -Screening for heterozygotes- carrier frequency is at least 0.5-1% and are found frequently in Ashkenazim = Bloom syndrome, Fanconi anemia, Gaucher Disease, Maple syrup urine disease, mucolipidosis type IV, Niemann-Pick disease type Screening in Pregnancy Diagnostic procedures1. amniocentesis 2. chorion villi sampling 3. cordocentesis or PUBS 4. ultrasonography or couples of mixed Jewish/non-Jewish parentage -Aim of maternal serum screening is to ID pregnancies where the fetus has a serious defect such as neural tube defects or a chromosome anomaly such as down syndrome -screening developed bc 95% neural tube defects occurred without prior history and 95% of Down syndrome infants were unexpected too -Quadruple Screening in the 2nd trimester involves the assay of maternal serum for alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), unconjugated estriol (uE3), and serium Inhibin -Assay for acetylcholinesterase inclines diagnosis towards neural tube defect, but is not absolutely specific for that lesion -elevated AFP directly from fetus to maternal circulation can indicate problems with placenta—indicated by elevated MSAFP= pregnancy at higher risk for later obstetrical complications -Amniocentesis for prenatal genetic studies is recommended when odds of Down syndrome is 1/270 A, glycogen storage disease type 1A -Maternal serum AFP= MSAFP= if elevated increased leak of this protein into the maternal circulation leakage from an open defect such as spina bifida, anencephaly, or encephalocele raises the conc. In the surrounding amniotic fluid and the maternal serum as well -Other defects that leak AFP directly into amniotic fluid – renal defect, autosomal recessive weeping skin defect -Leak of neuronal origin, Acetylcholinesterase is also spilled into amniotic fluid -screening for Down syndrome, neural tube defects –anencephaly, Lecture 7: Genetic Screening and Prenatal Diagnosis SCOPE FOR PRENATAL DIAGNOSIS CYTOGENIC DISORDERS BIOCHEMICAL GENETIC DISORDERS MOLECULAR GENETICS Detection of all recognizable chromosome anomalies, use of FISH for rapid diagnosis of numerical chromosomal disorders/structural rearrangements including deletions/duplications/translocations -Detection of >100 biochem metabolic disorders by enzyme analysis of amniotic fluid cells- ex. Tay-Sachs (Hexosaminidase A assay), Hurler syndrome (alpha-iduronidase) -Complication- the many diff mutations in each disorder makes mutation analysis impractical/costly except for Tay-Sachs and Canavan’s disease -so enzymatic analysis remains the accepted method for majority of inborn errors of metabolism -Detection of any recognized mutation is now possible, through PCR and if needed, gene sequencing of DNA from amniotic fluid cells/ chorionic villus tissue -For disorders in which gene loci have been discovered but mutation detection is too costly, DNA linkage analysis is used (95-98% certainty) -Molecular analysis for common mutations include: Canavan disease, CF, duchenne/Becker muscular dystrophy, fragile X, gaucher, Myotonic MD -Heterozygote detection prior to pregnancy: CF (Caucasians), sickle-cell (Blacks), Tay-Sachs (Ashkenazi Jew/ French-Canadian), thalassemia (Mediterranean; Asians) -Paternity Testing PRENATAL DETECTION OF LEAKING FETAL MALFORMATIONS Problems encountered in PRENATAL DIAGNOSIS -Prenatal Predictive diagnosis- diagnostic tests that accurately predict serious-fatal genetic disorders that many manifest decades after birth. In absence of a cure, couples with a 25-50% of having affected offspring consider this testing – neurodegenerative disorders/ neuromuscular disorders, or those with inherited cancer. Ex. Huntington’s Disease, myotonic muscular dys, sponcerebellar ataxia, hereditary breast/ ovarian cancer or colon cancer Analysis of amniotic fluid for AFP opportunity to detect fetal defects that leak fetal serum indicative of open spina bifida, anencephaly, omphalocele, etc. -Optimal time for detection – 16-18 weeks of gestation -Exception 5% of spina bifida lesions are closed and don’t leak false negative because of skin-closed lesion -Acetylcholinesterase- found in the amniotic fluid when a neuronal leak is present 1. Pseudomosaicism- results when cultivated amniotic fluid cells with an abnormal karyotype in a single tissue culture dish arise as an artifact of cell culture or as a derivative of placental tissue not rep. of the fetus. True mosaicism is distinguished by the finding of cells with both norm/abn karyotypes in the SAME amniotic fluid specimen in at least TWO cell culture dishes 2. Multiple fetuses-discordancy for specific defects (i.e. one fetus has Down syndrome and the other has spina bifida) 3. Cell growth failure (rare)- bacterial/fungal infection may ruin a sample as may excessive heat or cold. Toxic substances within syringes/tubes may also prove lethal to amniotic fluid cells 4. Maternal cell contamination- maternal cells may adhere to the amniocentesis needle and cause serious erros in prenatal diagnosis 5. Unexpected diagnosis- prenatal genetic studies performed for specific indications may reveal an unexpected diagnosis. Ex. XYY male. Refer for genetic counseling Lecture 8: Testing for disease susceptibility—Types of testing Abnormal events during meiosis can cause disruption of normal Genetic testing: chromosome number/structure Chromosomal abnormalities -Traditional karyotype- allows visualization of metaphase chromosomes- resulting banding patterns can be used to id chromosomes, determine how many homologs of each chromo are present, and visualize any large structural rearrangements -SKY- simplifies typical karyotype- paints each chromosome a dif color using labeled DNA probes that target specific chromosomes – ID large-scale chromosomal rearrangements Genetic testing: Direct mutation testing expect to see 2 of each – contrasting colors make the presence of a translocation obvious. Downfall- requires amplification -FISH- no amp needed, use probes directed towards a particular chromosomal region- can id changes in chromosome copy number, if 2 probes from diff chromosomes co-localize = translocation. Should verify with full karyotyping -PCR- amplifies a specific genetic sequence which is further studied for characteristics of size or sequence and this amplified sequence is targeted by designing unique DNA primers that flank the region of interest thermocycling PCR reaction amplifies the number of copies of target sequence -Gel electrophoresis- separates DNA fragments by size by pulling negatively charged DNA particles towards the anode and the mobility of the DNA fragments depends on their size, smallest move fastest -Southern blotting- Alternative technique used to detect large-scale changes that can’t be amplified by PCR= ex. Triplet expansions in noncoding regions that have size changes larger than those found in the coding region. Southern blotting—genomic DNA is digested with restriction enzymes and run on a gel restriction enzymes cut the DNA at periodic intervals produces a collection of DNA fragments put on nylon membrane labeled probe is hybridized to the unique complementary sequences on the membrane and visualized using x-ray film -Dideoxy Sanger sequencing- Detect single basepair changes; most widely used method for sequencing genes directly; id single base pair sequence changes. A DNA sequencing method using a mixture of both deoxynucleotide triphosphates (dNTPs) and dideocynucleotide triphosphates (ddNTPs) in a rxn that is related to the PCR rxn. If a dNTP is added to the growing DNA chain, then a 3’OH is present to continue addn of nucleotides; if a ddNTP is added, it is missing 3’OH and addition is not possible.= Forms characteristic sized molecules and ddNTPs are colored, separated by electrophoretic techniques= converted into linear DNA sequence. - Allele specific hybridization- Method used to detect single basepair changes, similar to Southern blot, but doesn’t separate DNA by size; instead, complete genomic DNA is hybridized to a spot on nylon membrane spot is probed with a labeled oligonucleotide which only hybridizes to normal or mutant allele membrane exposed to x-ray film presence/absence of signal will indicate which alleles are present (SKIP electrophoresis) Genetic changes on the nucleotide or gene level -Combination of PCR and gel electrophoresis detect deletions and insertions large enough to cause a chance in DNA migration (less than 10100s of basepairs) -PCR/gel electro- Used to detect Huntington CAG repeat- can predict with high accuracy, the likelihood of an ind. Developing Huntington’s based on the CAG repeats -Southern blotting used to detect large-scale deletions and insertions- detect non-coding triplet repeat expansions and also able to detect methylation status of a gene -Southern blotting- used for Fragile X -Both dideoxy-sequencing and allele specific hybridization are good at detecting single basepair changes; also designed to id mutations in small regions of genes but most disorders have some level of allelic heterogeneity – aka a condition that can be caused by multiple mutations (PKU, CF) ALTERNATIVES -Complete exon sequencing- So, typical genetic test for a disease with a high level of allelic heterogeneity = sequence only the exons= where the most predictable mutations are. -Panel of mutations- testing strategy is further focused by testing for a panel of mutations that represent the majority of mutations present in a given population -Focus mutation= if a particular mutation is identified in a patient by a broader sequencing method, family members can immediately focus on Genetic testing: Linkage testing Test specific for disease -Linkage testing is used if a patient exhibits disease that is suggestive of a particular disorder but no mutations can be identified by exonic sequencing. -Linkage tests take advantage of the same principles that guide linkage ANALYSIS in id-ing a disease gene -Use markers that lie close to the disease-gene because they are often inherited with the disease gene RFLPs can be detected by Southern analysis or amp by PCR SSLPs differ in length of repeat tracts and these differences can be detected by PCR and gel electrophoresis SNPs- identified by DNA sequencing, by restriction digest, by allele specific hybridization Markers for test are generally chosen based on 2 criteria: proximity to the gene and heterozygosity in the population -marker based genetic tests are useful in detecting Uniparental Disomy (UPD). Compare the haplotypes of both the suspected UPD chromosome and a control chromosome in the affected patient and his/her parents -CF sweat test- detect elevated levels of ions present in the sweat of individuals with defective chloride channels -PKU biochemical test- measure the blood concentration of Phe in newborns --Problem1. elevated levels may not show for a few days after birth and may go undetected) this wouldn’t happen with a genetic test which would thoroughly evaluate the gene 2. Biochemical tests do not yield insight about carrier status -Hemoglobinopathy- biochemical testing that can provide info about carrier status—two main types of testing used to screen for sickle cell anemia and various thalassemias 1. Isoelectric Focusing (IEF)- specialized form of protein electrophoresis that separates hemoglobin subunits within the gradient, the mutation present in the family rather than complete exonic sequencing -Linkage testing used for a family with a history of Duchenne’s muscular dystrophy (DMD) – gene is HUGE= 2.5 megabases (10x size of CFTR gene)so complete sequencing is less practical. -Linkage testing is carried out using 2 markers flanking the dystrophin gene. Although markers are chosen close to the disease gene, this doesn’t completely rule out the possibility of recombination skewing the results of this type of genetic test -UPD- chromosomes present are the same copy from the same parent= can lead to appearance of recessive disorders for which the parent is a carrier -Genotyping of markers on the suspected UPD chromosome can determine if both copies of a particular chromosome are derived from a single parent’s chromosome - If a UPD chromosome exists, the marker loci would all be expected to be homozygous for one parent’s alleles -One caveat- linkage genetic tests and marker tests for UPD require multiple heterozyg. Family members and at least 1 affected member or marker can be separated from disease gene by recomb. but relative quantities of the variant hb are more difficult to determine 2. High performance liquid chromatography (HPLC)- More accurately estimates quantities of hb variants, but more expensive Conclusion: The decision between biochemical and genetic testing comes down to a cost-benefit analysis. Generally, testing is recommended for individuals where medical decisions and treatments would be informed by test results (i.e. not adult-onset disorders). In terms of cost benefit, FULL GENE SEQUENCING would be the most informative but it is extremely costly making it inaccessible to most. Instead, goal is to offer MUTATION PANEL TESTING or COMPLETE EXON SEQUENCING, depending on the disorder/circumstances. Where there is a case of a known affected individual in a family, this individual should be tested first to id which mutation is travelling within a given family. Lecture 9: Genetic Frontiers Method Description -Thousands of DNA substrates bound to a solid surface in a highly ordered configuration. Each spot on the array corresponds to a Microarray technology aka gene known, unique DNA sequcnce. Once the DNA is bound, it can be probed using labeled DNA. The DNA probes are derived from experimental samples and are labeled with fluorophores. When the DNAs find a complementary sequence on the chip, they bind to that chips/ DNA chips sequence. The whole chip is scanned for fluorescent signal and any spot where signal is detected can be traced back to the original key of spots to determine which unique genomic locus has been detected. -Used for SNP genotyping detection of a signal indiciates presence of a particular SNP allele. Makes using a large collection of SNPs more feasible in linkage analysis -This type of high-throughput genotyping has allowed for the trend of using large genome wide association studies (GWAS) = vast catalogue of genes associated with disease helpful for complex diseases like obesity and diabetes -Microarrays used in direct-to-consumer tests -Microarrays used to id a novel coronavirus (SARS-CoV) which was the cause of SATS Direct-to-consumer -Private interests saw the profit potential and moved quickly to commercialize this info into genome-wide DIRECT-TO-CONSUMER tests tests which have positive benefits such as extending preventative testing to people who might not otherwise be identified until seeing a (An application of specialist Microarray test) -Problem- worry that patients will seek out genome-wide scans and not know what to do with the info after. A professional should be involved in interpretation of results. Comparative -A comparison is made between 2 diff signals which is useful for detecting polymorphic copy number variations or abnormal copy Genomic numbers of genes such as deletions or amplifications, freq associated with tumorigenesis. Hybridization -Control = green and experimental sample = red two DNA samples are mixed and hybridized to a chip locus amplified in the tumor (An application of = red and deleted locus = green Microarray testing) -When used in conjunction with comparative genomic hybridization, can detect microdeltions probes loci spaced every 35 basepairs High density along chromosomes. microarray Conclusion: Microarray-based technologies help the id of loci associated with particular disease and id of the disease gene itself. Expression profiling (application of microarray test) Gene Therapy 1) REPLACE gene -Act. Paralogs -Wild type copy of gene -Viral machinery to deliver genes -Expression profiling- id patterns of gene expression associated with particular disorders. Understand the interplay of numerous genes in promoting a disorder. Highly objective and precise, esp in determining tumor subtypes, prognosis, progressiveness related to treatment strategies and id of biomarkers. -Technique of gene therapy is to make use of an individual’s own genes to supply functional copies of genes that are mutated. -Sickle cell anemia and Beta-thalassemia- Ex. Used in sickle cell anemia by using a functional paralog (homologous gene within the same organism) of the B-subunit that normally acts during the fetal period. This subunit (with butyrate treatment) can displace the mutant HbS protein. Also used in B-thalassemias - When paralogs are not available, wild type copies of gene from outside source is used through safe and effective gene delivery, including the use of naked DNA or of liposomes which are synthetic lipid bilayers that can be made to carry specific DNA molecules. TWO DRAWBACKS to this method- nonspecific and inefficient -Developed replication deficient viruses which could carry and deliver recombinant DNA to certain target cells; the modified viral genome itself doesn’t have copies of key genes needed for the viral life cycle. All the genes needed to produce an infectious viral particle are present but once these particles are used to infect normal human cells, the viral genome is incomplete and cannot produce addl viral particles. Over 60% of these trials are used for cancer therapeutics. -SCID- The most promising trial involved severe combined immunodeficiency (SCID). Gene was delivered to allow expression of T and NK cells which are mutant in the disease. However, after 30 months, 2/11 patients developed acute lymphoblastic leukemia (ALL) bc the viral genome integrated with the patient’s LMO2 locus, activating the oncogenes. -Before gene therapies can be widely accepted, issues of safety and efficacy need to be addressed. It is advised to use bone marrow transplants before gene therapy for SCID. 2) Use of RNAi -Small interfering RNAs (siRNA) and an RNA-induced silencing complex (RISC) target homologous mRNA for cleavage. If engineered siRNA molecules could be delivered by viral mechanisms, this could allow for sequence-targeted inact. Of genes -HIV- Ex- Proposed that this technique could be used to inactivate expression of CCR5, the HIV coreceptor to prevent HIV infection of CD4 + cells. -Cancer – RNAi could be used to inactivate cancer genes such as bcr-abl by engineering siRNA molecules that bridge the fusion junction 3) Stem Cell therapy (cell-based delivery of genes) -Two main forms: treatment with embryos (advantage = cells are totipotent- potential to become any cell type but problem might be difficult to find an HLA match) and treatment with adult stem cells derived from the patient himself (pluripotent- potential to become many but not all cell types, HLA will match). -Induced pluripotent stem cells (iPS)- using tissue derived from adult mouse or human in which these differentiated adult cells were reprogrammed with the introduction of a combo of TFs normally expressed in embryonic stem cells and these modified cells were able to behave as pluripotent stem cells after reprogramming Corrected cells. -Sickle cell disease and Hemophilia B- genetically altered cells used in methods to treat these two conditions -Study of individual responses to drugs- aim to determine the factors that influence drug specificity, metabolism, and toxicity. Pharmacogenetics -ALL- childhood leukemia which is treated with 6-mercaptopurine (6-MP), a fraction of which is inactivated by the TPMT enzyme. 1/300 have a low activity TPMT prevents inactivation of 6-MP accumulation of 6MP toxic byproduct that inhibits DNA replication. -Detect low activity by simple genetic test and can be treated by reducing the concentration of 6MP given to patients with reduced TPMT activity