HERE - The Therapy Center for Physical Rehabilitation and Wellness

WHAT IS PHYSICAL THERAPY? phys·i·cal ther·a·py
noun
US
noun: physical therapy ; plural noun: physical therapies
1. the treatment of disease, injury, or deformity by physical methods such as massage, heat treatment, and exercise rather than by drugs or surgery.
2. Physical Therapists can specialize in many areas, such as Pediatrics, Neuro Therapy, Geriatrics, Orthopedics, Vestibular disorders, Lymphedema,
Women’s issues/Incontinence, Manual Therapy, Craniosacral, and Sports Medicine.
3. phys·i·o·ther·a·pee
ˌfizēōˈTHerəpē/
noun
noun: physical therapy
1. British term for physical therapy .
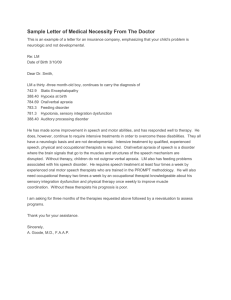
WHAT IS OCCUPATIONAL THERAPY? oc·cu·pa·tion·al ther·a·py
noun
1. a form of therapy for those recuperating from physical or mental illness that encourages rehabilitation through the performance of activities required in daily life. Focus of things such as dressing, bathing, eating, self care activities, including fine mot or skills of the hands. Some OT’s can specialize in hands, or Certified Hand Therapist.
WHAT IS SPEECH THERAPY? speech ther·a·py
noun
noun: speech therapy
1. training to help people with speech and language problems to speak more clearly
2. training people to improve their ability to comprehend and organize their thoughts and what they are seeing/hearing in their daily activities.
3. Training the oral-motor system, improving ability to swallow (dysphagia) There are many specialties of Speech Therapists.
PHYSICAL THERAPY
Overview
Physical therapy involves the interaction between therapist(s), patients or clients, other health care professionals, families, care givers, and communities in a process where movement potential is assessed and diagnosed and goals are agreed upon.
[1] Physical therapy is performed by a therapist and sometimes services are provided by a physical therapist assistant (PTA) acting under their direction. Physical therapists and occupational therapists often work together in conjunction to provide treatment for patients. In some cases, physical rehabilitation technicians may provide physiotherapy services.
[2]
PTs are healthcare professionals who diagnose and treat individuals of all ages, from newborns to the very oldest, who have medical problems or other health-related conditions, illnesses, or injuries that limit their abilities to move and perform functional activities as well as they would like in their daily lives.
[3] PTs use an individual's history and physical examination to arrive at a diagnosis and establish a management plan and, when necessary, incorporate the results of laboratory and imaging studies. Electrodiagnostic testing (e.g., electromyograms and nerve conduction velocity testing) may also be of assistance.
[4] PT management commonly includes prescription of or assistance with specific exercises, manual therapy, education, manipulation and other interventions. In addition, PTs work with individuals to prevent the loss of mobility before it occurs by developing fitness and wellness-oriented programs for healthier and more active lifestyles, providing services to individuals and populations to develop, maintain and restore maximum movement and functional ability throughout the lifespan. This includes providing therapeutic treatment in circumstances where movement and function are threatened by aging, injury, disease or environmental factors. Functional movement is central to what it means to be healthy .
Physical therapy is a professional career which has many specialties including sports , neurology , wound care , EMG , cardiopulmonary , geriatrics , orthopaedic and pediatrics .
Neurological rehabilitation is in particular a rapidly emerging field. PTs practice in many settings, such as outpatient clinics or offices, health and wellness clinics, rehabilitation hospitals facilities, skilled nursing facilities, extended care facilities, private homes, education and research centers, schools , hospices , industrial and this workplaces or other occupational environments, fitness centers and sports training facilities.
[5]
Physical therapists also practise in the non-patient care roles such as health policy, [6][7][8][9] health insurance, health care administration and as health care executives.
[10][11] Physical therapists are involved in the medical-legal field serving as experts, performing peer review and independent medical examinations .
[12]
Education qualifications vary greatly by country. The span of education ranges from some countries having little formal education to others having doctoral degrees and post doctoral residencies and fellowships.
History of physical therapy
Physicians like Hippocrates and later Galenus are believed to have been the first practitioners of physical therapy, advocating massage , manual therapy techniques and hydrotherapy to treat people in 460 BC.
[13] [ verification needed ]
After the development of orthopedics in the eighteenth century, machines like the Gymnasticon were
[14] developed to treat gout and similar diseases by systematic exercise of the joints, similar to later developments in physical therapy.
The earliest documented origins of actual physical therapy as a professional group date back to Per Henrik Ling , “Father of Swedish Gymnastics,” who founded the Royal Central Institute of Gymnastics
(RCIG) in 1813 for massage , manipulation , and exercise . The Swedish word for physical therapist is sjukgymnast = someone involved in gymnastics for those who are ill.
In 1887, PTs were given official registration by Sweden’s National Board of Health and Welfare. Other countries soon followed. In 1894, four nurses in Great Britain formed the Chartered Society of Physiotherapy .
[15] The School of Physiotherapy at the University of Otago in New Zealand in 1913, [16] and the United States' 1914 Reed
College in Portland, Oregon, which graduated "reconstruction aides." [17] Since the profession's inception, spinal manipulative therapy has been a component of the physical therapist practice.
[18]
Modern physical therapy was established towards the end of the 19th century due to events that had an effect on a global scale, which called for rapid advances in physical therapy. Soon following American orthopedic surgeons began treating children with disabilities and began employing women trained in physical education, massage, and remedial exercise. These treatments were applied and promoted further during the Polio outbreak of 1916. During the First World War women were recruited to work with and restore physical function to injured soldiers, and the field of physical therapy was institutionalized. In 1918 the term "Reconstruction Aide" was used to refer to individuals practicing physical therapy. The first school of physical therapy was established at Walter Reed Army Hospital in Washington, D.C., following the outbreak of World War I.
[19]
Research catalyzed the physical therapy movement. The first physical therapy research was published in the United States in March 1921 in "The PT Review." In the same year, Mary McMillan organized the Physical Therapy Association (now called the American Physical Therapy Association (APTA). In
1924, the Georgia Warm Springs Foundation promoted the field by touting physical therapy as a treatment for polio .
[20]
Treatment through the 1940s primarily consisted of exercise , massage, and traction . Manipulative procedures to the spine and extremity joints began to be practiced, especially in the British Commonwealth countries, in the early 1950s.
[21][22] Around this time when polio vaccines were developed, physical therapists have become a normal occurrence in hospitals throughout North America and Europe.
[23] In the late 1950s, physical therapists started to move beyond hospital-based practice to outpatient orthopedic clinics, public schools, colleges/universities health-centres, geriatric settings (skilled nursing facilities), rehabilitation centers and medical centers. Specialization for physical therapy in the U.S. occurred in 1974, with the Orthopaedic Section of the APTA being formed for those physical therapists specializing in orthopaedics. In the same year, the International Federation of
Orthopaedic Manipulative Physical Therapists was formed, [24] which has ever since played an important role in advancing manual therapy worldwide.
Education
Main article: Physical therapy education
Educational criteria for physical therapy providers vary from state to state and from country to country, and among various levels of professional responsibility. Most U.S. states have physical therapy practice acts that recognize both physical therapists (PT) and physical therapist assistants (PTA) and some jurisdictions also recognize physical therapy technicians (PT Techs) or aides. Most countries have licensing bodies that require physical therapists to be a member of before they can start practising as independent professionals.
Physical Therapists
[ edit ]
The primary physical therapy practitioner is the Physical Therapist (PT) who is trained and licensed to examine, evaluate, diagnose and treat impairment, functional limitations and disabilities in patients or clients. Currently, most Physical Therapist education curricula in the United States culminate in a Doctor of Physical
Therapy (DPT) degree,
[25]
but many currently practising PTs hold a Master of Physical Therapy degree and some hold a Bachelor's degree . The World Confederation of
Physical Therapy (WCPT) recognizes there is considerable diversity in the social, economic, cultural, and political environments in which physical therapist education is conducted throughout the world. WCPT recommends physical therapist entry-level educational programs be based on university or university-level studies, of a minimum of four years, independently validated and accredited as being at a standard that accords graduates full statutory and professional recognition.
[2] WCPT acknowledges there is innovation and variation in program delivery and in entry-level qualifications, including first university degrees (Bachelors/Baccalaureate/Licensed or equivalent),
Masters and Doctorate entry qualifications. What is expected is that any program should deliver a curriculum that will enable physical therapists to attain the knowledge, skills, and attributes described in these guidelines. Professional education prepares physical therapists to be autonomous practitioners, that may work in collaboration with other members of the health care team.
[ citation needed ] Curricula in the United States are accredited by the Commission on Accreditation in Physical Therapy
Education (CAPTE). As of 2011, APTA reports that 222 out of 227 entry-level professional degree programs accredited in the United States are at the doctoral level.
[25] According to CAPTE, as of 2012 there are 25,660 students currently enrolled in 210 accredited PT programs in the United States .
[26]
The physical therapist professional curriculum is as rigorous as the traditional medical curricula and includes content and learning experiences in the clinical sciences
(e.g., content about the cardiovascular, pulmonary, endocrine, metabolic, gastrointestinal, genitourinary, integumentary, musculoskeletal, and neuromuscular systems and the medical and surgical conditions frequently seen by physical therapists).
Curricula for the Physical Therapist professional degree include:
Screening to determine when patients/clients need further examination or consultation by a physical therapist or referral to another health care professional.
Examination: Examine patients/clients by obtaining a history from them and from other sources. Examine patients/clients by performing systems reviews. Examine patients/clients by selecting and administering culturally appropriate and age related tests and measures. Tests and measures include, but are not limited to, those that assess: a. Aerobic Capacity/Endurance, b. Anthropometric Characteristics, c. Arousal, Attention, and Cognition, d. Assistive and Adaptive Devices, e. Circulation (Arterial,
Venous, Lymphatic), f. Cranial and Peripheral Nerve Integrity, g. Environmental, Home, and Work (Job/School/Play) Barriers, h. Ergonomics and Body Mechanics, i. Gait,
Locomotion, and Balance, j. Integumentary Integrity, k. Joint Integrity and Mobility, l. Motor Function (Motor Control and Motor Learning), m. Muscle Performance
(including Strength, Power, and Endurance), n. Neuromotor Development and Sensory Integration, o. Orthotic, Protective, and Supportive Devices, p. Pain, q. Posture, r.
Prosthetic Requirements, s. Range of Motion (including Muscle Length), t. Reflex Integrity, u. Self-Care and Home Management (including activities of daily living [ADL] and instrumental activities of daily living [IADL]), v. Sensory Integrity, w. Ventilation and Respiration/Gas Exchange, x. Work (Job/School/Play), Community, and Leisure
Integration or Reintegration (including IADL)
Evaluation: Evaluate data from the examination (history, systems review, and tests and measures) to make clinical judgments regarding patients/clients.
Diagnosis: Determine a diagnosis that guides future patient/client management.
Prognosis: Determine patient/client prognoses.
Plan of Care: Collaborate with patients/clients, family members, payers, other professionals, and other individuals to determine a plan of care that is acceptable, realistic, culturally competent, and patient-centered.
Intervention:Provide physical therapy interventions to achieve patient/client goals and outcomes. Interventions include: a. Therapeutic Exercise, b. Functional Training in
Self-Care and Home Management, c. Functional Training in Work (Job/School/Play), Community, and Leisure Integration or Reintegration, d. Manual Therapy
Techniques (including Mobilization/Manipulation Thrust and Nonthrust Techniques), e. Prescription, Application, and, as Appropriate, Fabrication of Devices and
Equipment, f. Airway Clearance Techniques, g. Integumentary Repair and Protection Techniques, h. Electrotherapeutic Modalities,
Provide effective culturally competent instruction to patients/clients and others to achieve goals and outcomes.
Prevention, Health Promotion, Fitness, and Wellness: Provide culturally competent physical therapy services for prevention, health promotion, fitness, and wellness to individuals, groups, and communities. Apply principles of prevention to defined population groups.
Students completing a Doctor of Physical Therapy program are also required to successfully complete clinical internships prior to graduation.
In Canada
In the province of Quebec, prospective physiotherapists are required to have completed a college diploma in either health sciences, which lasts on average two years, or physical rehabilitation technology, which lasts at least three years, to apply to a physiotherapy program or program in university. Following admission, physical therapy students work on a bachelor of science with a major in physical therapy and rehabilitation. The B.Sc. usually requires three years to complete. Students must then enter graduate school to complete a master's degree in physical therapy, which normally requires one and a half to two years of study. Graduates who obtain their M.Sc. must successfully pass the membership examination to become member of the Ordre p rofessionnel de la physiothérapie du Québec (OPPQ). Physiotherapists can pursue their education in such fields as rehabilitation sciences, sports medicine, kinesiology, and physiology.
Many provinces in Canada have changed their Bachelors in Physiotherapy degree program with the 3 years of college / university pre-requisite into a Masters in
Physiotherapy with the requirement of a Bachelors Degree including certain pre-requisite courses.
Physical Therapist Assistants
Physical therapist assistants may deliver treatment and physical interventions for patients and clients under a care plan established by and under the supervision of a physical therapist. Physical therapist assistants in the United States are currently trained under associate of applied sciences curricula specific to the profession, as outlined and accredited by CAPTE. As of August 2011, there were 276 accredited two-year ( Associate degree ) programs for physical therapist assistants In the United
States of America.
[27] According to CAPTE, as of 2012 there are 10,598 students currently enrolled in 280 accredited PTA programs in the United States.
[26]
Curricula for the physical therapist assistant associate degree include: [28]
Anatomy & physiology
Exercise physiology
Human biology
Physics
Biomechanics
Kinesiology
Neuroscience
Clinical pathology
Behavioral sciences
Communication
Ethics
Research
Other coursework as required by individual programs.
Physical Therapy Technicians or Aides
Some jurisdictions allow physical therapists to employ technicians or aides or therapy assistants to perform designated routine tasks related to physical therapy under the direct supervision of a physical therapist. Some jurisdictions require physical therapy technicians or aides to be certified, and education and certification requirements vary among jurisdictions.
In Canada
In the province of Quebec, physical rehabilitation technicians (also known as physical therapy technicians) are health care professionals who are required to complete a three year college diploma program in physical rehabilitation technology and successfully pass the membership examinations of the Ordre professionnel de la physiothérapie du Québec (OPPQ) in order to practise legally in the country.
Most physical rehabilitation technicians complete their college diploma at Collège Montmorency , Dawson College , or Cégep Marie-Victorin , all situated in and around the Montreal area.
After completing their technical college diploma, graduates have the opportunity to pursue their studies at the university level to perhaps obtain a bachelor's degree in physiotherapy , kinesiology , exercise science , or occupational therapy . The Université de Montréal and the Université de Sherbrooke are among the Québécois universities that admit physical rehabilitation technicians in their programs of study related to health sciences and rehabilitation in order to credit courses that were completed in college .
In the United States of America
Job duties and education requirements for Physical Therapy Technicians or Aides may vary according to employer, but education requirements range from high school diploma or equivalent to completion of a 2-year degree program.
[29] O-Net reports that 64% of PT Aides/Techs have a high school diploma or equivalent, 21% have completed some college but hold no degree, and 10% hold an Associate's Degree.
[30]
Employment
Physical therapy-related jobs in North America have shown rapid growth in recent years, but employment rates and average wages may vary significantly between different countries, states, provinces or regions.
In the United States of America
According to the United States Department of Labor 's Bureau of Labor Statistics , there were approximately 198,600 Physical Therapists employed in the United States in
2010, earning an average $76,310 annually, or $36.69 per hour, with 39% growth in employment projected by the year 2020.
[31] The Bureau of Labor Statistics also reports that there were approximately 114,400 Physical Therapist Assistants and Aides employed in the United States in 2010, earning an average $37,710 annually, or
$18.13 per hour, with 45% growth in employment projected by the year 2020. To meet their needs, many healthcare and physical therapy facilities hire "Travel physical therapists", who work temporary assignments between 8 and 26 weeks for much higher wages; about $113,500 a year.
[32] Bureau of Labor Statistics data on PTAs and
Techs can be difficult to decipher, due to their tendency to report data on these job fields collectively rather than separately. O-Net reports that in 2011, PTAs in the United
States earned a median wage of $51,040 annually or $24.54 hourly, and that Aides/Techs earned a median wage of $23,680 annually or $11.39 hourly in 2011.
[30][33]
Specialty areas
Because the body of knowledge of physical therapy is extremely large, PTs usually specialize in a specific clinical area. While there are many different types of physical therapy, [34] the American Board of Physical Therapy Specialties list eight specialist certifications. Most Physical Therapists practicing under a specialism will have undergone further training.
Cardiovascular & pulmonary
Cardiovascular and pulmonary rehabilitation respiratory practitioners and physical therapists treat a wide variety of cardiopulmonary disorders or pre and post cardiac or pulmonary surgery. An example of cardiac surgery is cabg . Primary goals of this specialty include increasing endurance and functional independence. Manual therapy is used in this field to assist in clearing lung secretions experienced with cystic fibrosis . Disorders, including heart attacks , post coronary bypass surgery , chronic obstructive pulmonary disease , and pulmonary fibrosis , treatments can benefit [ citation needed ] from cardiovascular and pulmonary specialized physical therapists.
[35] [ verification needed ]
Clinical electrophysiology
This specialty area encompasses electrotherapy/physical agents, electrophysiological evaluation (EMG/NCV) , physical agents, and wound management.
Geriatric
Geriatric physical therapy covers a wide area of issues concerning people as they go through normal adult aging but is usually focused on the older adult. There are many conditions that affect many people as they grow older and include but are not limited to the following: arthritis , osteoporosis , cancer , Alzheimer's disease , hip and joint replacement, balance disorders, incontinence , etc. Geriatric physical therapists specialize in treating conditions in older adults.
Integumentary
Integumentary (treatment of conditions involving the skin and all its related organs). Common conditions managed include wounds and burns. Physical therapists may utilize surgical instruments, mechanical lavage, dressings and topical agents to debride necrotic tissue and promote tissue healing. Other commonly used interventions include exercise, edema control, splinting, and compression garments.
Neurological
Neurological physical therapy is a field focused on working with individuals who have a neurological disorder or disease. These can include stroke , chronic back pain,
Alzheimer's disease, Charcot-Marie-Tooth disease (CMT) , ALS , brain injury, cerebral palsy ,l.g.b.syndrome, multiple sclerosis , Parkinson's disease , facial palsy and spinal cord injury. Common impairments associated with neurologic conditions include impairments of vision, balance, ambulation, activities of daily living , movement, muscle strength and loss of functional independence.
[35] Physiotherapy can address many of these impairments and aid in restoring and maintaining function, slowing disease progression, and improving quality of life. The techniques involve in neurological physical therapy are wide ranging and often require specialized training.
Neurological physiotherapy is also called neurophysiotherapy or neurological rehabilitation .
Orthopedic
Orthopedic physical therapists diagnose, manage, and treat disorders and injuries of the musculoskeletal system including rehabilitation after orthopedic surgery. This specialty of physical therapy is most often found in the out-patient clinical setting. Orthopedic therapists are trained in the treatment of post-operative orthopedic procedures, fractures, acute sports injuries, arthritis, sprains, strains, back and neck pain, spinal conditions, and amputations.
Joint and spine mobilization/manipulation, dry needling , therapeutic exercise , neuromuscular techniques, muscle reeducation, hot/cold packs, and electrical muscle stimulation (e.g., cryotherapy , iontophoresis , electrotherapy ) are modalities often used to expedite recovery in the orthopedic setting.
[36] [ verification needed ] Additionally, an emerging adjunct to diagnosis and treatment is the use of sonography for diagnosis and to guide treatments such as muscle retraining.
[37][38][39] Those who have suffered injury or disease affecting the muscles, bones, ligaments, or tendons will benefit from assessment by a physical therapist specialized in orthopedics.
Pediatric
Pediatric physical therapy assists in early detection of health problems and uses a wide variety of modalities to treat disorders in the pediatric population. These therapists are specialized in the diagnosis, treatment, and management of infants, children, and adolescents with a variety of congenital, developmental, neuromuscular, skeletal, or acquired disorders/diseases. Treatments focus on improving gross and fine motor skills , balance and coordination, strength and endurance as well as cognitive and sensory processing /integration. Children with developmental delays , cerebral palsy , spina bifida , or torticollis may be treated [ citation needed ] by pediatric physical therapists.
[35] [ verification needed ]
Sports
Physical therapists can be involved in the care and wellbeing of athletes including recreational, semi-professional (paid) and professional (full-time employment) participants. This area of practice encompasses complete athletic injury management under 5 main categories:
1. acute care - assessment and diagnosis of an initial injury;
2. treatment - application of specialist advice and techniques to encourage healing;
3. rehabilitation - progressive management for full return to sport;
4. prevention - identification and address of deficiencies known to directly result in, or act as precursors to injury
5. education - sharing of specialist knowledge to individual athletes, teams or clubs to assist in prevention or management of injury
Physical therapists who work for professional sport teams often have a specialized sports certification issued through their national registering organisation. Most Physical therapists who practice in a sporting environment are also active in sports medicine programs too.
Women's health
Women's health physical therapy addresses women's issues related to the female reproductive system, child birth, and post-partum. These conditions include lymphedema, osteoporosis, pelvic pain, prenatal and post partum periods, and urinary incontinence. It also addresses incontinence, pelvic pain, and other disorders associated with pelvic floor dysfunction.
[40]
Palliative care
Physiotherapy in the field of Oncology and Palliative care is a continuously evolving and developing specialty, both in Malignant and non-malignant diseases.
Rehabilitation for both groups of patients is now recognized as an essential part of the clinical pathway, as early diagnoses and new treatments are enabling patients to live longer. it is generally accepted that patients should have access to an appropriate level of rehabilitation, so that they can function at a minimum level of dependency and optimize their quality of life, regardless of their life expectancy.
Effectiveness
A 2012 systematic review found evidence to support the efficacy of spinal manipulation administered by physical therapists to patients.
[41] The same review found that physical therapy spinal manipulation seems to be safe and improves the outcome for individuals with low back pain .
[41]
SAMPLE ARTICLE:
How Exercise Works for Rheumatoid Arthritis
Exercise is one of the best things you can do for your body, even if you have RA.
The benefits include:
1.
2.
Better flexibility . Although it may seem more comfortable now to sit on the sidelines, moving your joints helps relieve stiffness and keeps them flexible.
Stronger muscles . Exercise strengthens muscles, and strong muscles better support and protect your joints.
Denser bones . Arthritis-related inflammation, and some of the drugs that treat it, can make your bones more fragile and more likely to break. Exercise boosts bone density, which could mean fewer fractures.
A healthier heart . Exercise is good for everyone's heart. If you have RA, that's especially important, since RA makes you more likely to get heart disease.
You feel better . Exercise boosts your mood, gives you more energy, helps you sleep better, and can make you feel better about yourself. If you work out with a friend, it's also an opportunity to socialize.
Exercise and RA
If you're not active now, check with your doctor to see if you have any limitations. Once you get the green light, think about ways you can make these four types of exercise a habit:
Flexibility: Gentle flexibility exercises help your joints work normally. It can also be relaxing. You should do gentle flexibility exercises every day. Listen to your body, and never stretch to the point of pain.
Strengthening: Use weights, resistance bands, or your own body weight to make your muscles work harder. Stronger muscles are are better able to support your joints.
To improve strength, you should gradually increase the amount or form of resistance. Do strengthening exercises every other day. Working with a physical therapist or trainer can help you get started.
Aerobic: Anything that gets your heart rate up -- such as walking, dancing, bicycling, swimming, running, or rowing -- counts as aerobic exercise. It's good for your heart, lungs, weight, and bones. It can also be a good way to release stress and improve your mood. Get some aerobic exercise most days of the week, working up to 30 minutes each session.
Body awareness: Body awareness exercises, such as tai chi and yoga, work on posture, balance, coordination, and relaxation.
As you get into your exercise program, these two strategies should help you:
Set goals. Break big goals down to smaller ones. Reward yourself for meeting them.
Make it fun.
Choose enjoyable activities that you can fit into your daily routine, such as going for a walk or meeting a friend for water aerobics.
Occupational therapy , often called OT , is the use of treatments to develop, recover, or maintain the daily living and work skills of people with a physical, mental or developmental condition.
[1]
Occupational therapy is a clientcentered practice that places a premium on the progress towards the client’s goals.
[2]
Occupational therapy interventions focus on adapting the environment, modifying the task, teaching the skill, and educating the client/family in order to increase participation in and performance of daily activities, particularly those that are meaningful to the client.
History of occupational therapy
See also: History of OT in America , History of OT in New Zealand , Occupational Therapy in the Seychelles
Early therapy
The earliest evidence of using occupations as a method of therapy can be found in ancient times. In c. 100 BCE, Greek physician Asclepiades initiated humane treatment of patients with mental illness using therapeutic baths, massage, exercise, and music. Later, the Roman Celsus prescribed music, travel, conversation and exercise to his patients. However by medieval times the use of these strategies with people considered to be insane was rare, if not nonexistent.
[3]
In 18th-century Europe, revolutionaries such as Philippe Pinel and Johann Christian Reil reformed the hospital system. Instead of the use of metal chains and restraints, their institutions utilized rigorous work and leisure activities in the late 18th century. This was the era of Moral Treatment, developed in Europe during the Age of
Enlightenment , where the roots of occupational therapy lie.
[4] Although it was thriving abroad, interest in the reform movement waxed and waned in the United States throughout the 19th century. It re-emerged in the early decades of the 20th century as Occupational Therapy.
The Arts and Crafts movement that flourished between 1860 and 1910 also impacted occupational therapy. In a recently industrialized society, the arts and crafts societies emerged against the monotony and lost autonomy of factory work .
[4] Arts and crafts were utilized as a way of promoting learning through doing and provided an outlet for creative energy and a way of avoiding the boredom that was associated with long hospital stays, both for mental illness and for tuberculosis.
Although only a small percentage of occupational therapists continue to work in the field of mental health, many universities place a strong emphasis on training students in psycho-social occupational therapy.
Health profession
The health profession of occupational therapy was conceived in the early 1910s as a reflection of the Progressive Era . Early professionals merged highly valued ideals, such as having a strong work ethic and the importance of crafting with one’s own hands with scientific and medical principles.
[3] The National Society for the Promotion of
Occupational Therapy, now called the American Occupational Therapy Association (AOTA), was founded in 1917 and the profession of Occupational Therapy was officially named in 1920.
The emergence of occupational therapy challenged the views of mainstream scientific medicine. Instead of focusing on purely physical etiologies, occupational therapists argued that a complex combination of social, economic, and biological reasons cause dysfunction. Principles and techniques were borrowed from many disciplines — including but not limited to nursing , psychiatry , rehabilitation , self-help , orthopedics , and social work —to enrich the profession’s scope. Between 1900 and 1930, the founders defined the realm of practice and developed supporting theories. By the early 1930s, AOTA had established educational guidelines and accreditation procedures [5] In a short 20-year span, they successfully convinced the public and medical world of the value of occupational therapy and established standards for the profession.
[3]
World War I forced the new profession to clarify its role in the medical domain and to standardize training and practice. In addition to clarifying its public image, occupational therapy also established clinics, work shops, and training schools nationwide. Due to the overwhelming number of wartime injuries, “reconstruction aides” (an umbrella term for occupational therapy aides and physiotherapy aides, now known as physical therapists) were recruited by the Surgeon General. Between 1917 and
1920, nearly 148,000 wounded men were placed in hospitals upon their return to the states. This number does not account for those wounded abroad. The success of the reconstruction aides, largely made up of women trying to “do their bit” to help with the war effort, was a great accomplishment. Post-war, however, there was a struggle to keep people in the profession. Emphasis shifted from the altruistic war-time mentality to the financial, professional, and personal satisfaction that comes with being a therapist. To make the profession more appealing, practice was standardized, as was the curriculum. Entry and exit criteria were established, and the American
Occupational Therapy Association advocated for steady employment, decent wages, and fair working conditions. Via these methods, occupational therapy sought and obtained medical legitimacy in the 1920s.
[3]
Occupational therapy. Toy making in psychiatric hospital. World War 1 era.
The profession has continued to grow and expand its scope and settings of practice. Occupational science, the study of occupation, was created in 1989 as a tool for providing evidence-based research to support and advance the practice of occupational therapy, as well as offer a basic science to study topics surrounding
"occupation".
[6]
Evolution of the philosophy of occupational therapy
The philosophy of occupational therapy has changed over the history of the profession. The philosophy articulated by the founders owed much to the ideals of romanticism ,
[7] pragmatism
[8]
and humanism which are collectively considered the fundamental ideologies of the past century.
[9][10][11]
One of the most widely cited early papers about the philosophy of occupational therapy was presented by Adolf Meyer , a psychiatrist who had emigrated to the United
States from Switzerland in the late 19th century and who was invited to present his views to a gathering of the new Occupational Therapy Society in 1922. At the time, Dr.
Meyer was one of the leading psychiatrists in the United States and head of the new psychiatry department and Phipps Clinic at Johns Hopkins University in Baltimore,
Maryland.
[12][13]
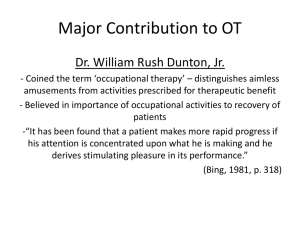
William Rush Dunton , a supporter of the National Society for the Promotion of Occupational Therapy, now the American Occupational Therapy Association, sought to promote the ideas that occupation is a basic human need, and that occupation is therapeutic. From his statements came some of the basic assumptions of occupational therapy, which include:
Occupation has a positive effect on health and well-being.
Occupation creates structure and organizes time.
Occupation brings meaning to life, culturally and personally.
Occupations are individual. People value different occupations.
[14]
These philosophies have been elaborated on over time in order to form the values that underpin the Codes of Ethics issued by each national association. However, the relevance of occupation to health and well-being remains the central theme. Influenced by criticism from medicine and the multitude of physical disabilities resulting from World War II , occupational therapy adopted a more reductionistic philosophy for a time. While this approach led to developments in technical knowledge about occupational performance, clinicians became increasingly disillusioned and re-considered these beliefs.
[15][16] As a result, client centeredness and occupation have reemerged as dominant themes in the profession.
[17][18][19] Over the past century, the underlying philosophy of occupational therapy has evolved from being a diversion from illness, to treatment, to enablement through meaningful occupation.
[14] This became evident through the development and widespread adoption of the Canadian Model of
Occupational Performance .
The two most commonly mentioned values are that occupation is essential for health and the concept of holism . However, there have been some dissenting voices.
Mocellin in particular advocated abandoning the notion of health through occupation as obsolete in the modern world and questioned the appropriateness of advocating holism when practice rarely supports it.
[20][21][22]
The values formulated by the American Occupational Therapy Association have also been critiqued as being therapist centred and not reflecting the modern reality of multicultural practice.
[23][24]
Central to the philosophy of occupational therapy is the concept of occupational performance. In considering occupational performance the therapist must consider the many factors that comprise overall performance. This concept is made more tangible using models such as the person-environment-occupation model proposed by Law et al. (1996) and the Person-Environment-Occupation-Performance (PEOP) model developed at the same time by Christiansen and Baum in the United States.
[25][26] This approach highlights the importance of satisfactions in one's occupations, broadening the aim of occupational therapy beyond the mere completion of tasks to the holistic achievement of personal well-being.
In recent times occupational therapy practitioners have challenged themselves to think more broadly about the potential scope of the profession, and expanded it to include working with groups experiencing occupational deprivation which stems from sources other than disability.
[27] Examples of new and emerging practice areas would include therapists working with refugees , [28] and with people experiencing homelessness .
[29]
The expanded version of the Canadian model of occupational performance and engagement (CMOP-E) encourages occupational therapists to think beyond just occupational performance and address other modes of occupational interaction such as occupational deprivation, competence, and justice. The broader notion of occupational engagement encompasses all that we do to become occupied and is congruent with how occupational therapists address issues of occupational enablement today.
[14]
Enabling occupation
Best practice in occupational therapy seeks to offer effective, client-centred services that enable people to engage in occupations of life. The Canadian Model of Client
Centered Enablement (CMCE) embraces occupational enablement as the core competency of occupational therapy [14] and the Canadian Practice Process Framework
(CPPF)
[14]
as the core process of occupational enablement.
Occupational therapy process
An occupational therapist works systematically through a sequence of actions known as the occupational therapy process. There are several versions of this process as described by numerous writers, although all include the basic components of evaluation, intervention, and outcomes. Creek
[30]
has sought to provide a comprehensive version based on extensive research which has 11 stages.
The Canadian Practice Process Framework (CPPF), [14] has eight action points and three contextual elements.
Fearing, Law, and Clark [31] suggested a 7 stage process. A central element of this process model is the focus on identifying both client and therapists strengths and resources prior to beginning to develop the outcomes and action plan.
The Occupational Therapy Practice Framework: Domain and Process (2nd edition) (AOTA, 2008) presents a 3 stage process, and includes interrelated constructs that define and guide practice.
Areas of practice in occupational therapy
The role of occupational therapy allows occupational therapists to work in many different settings, work with many different populations and acquire many different specialties. This broad spectrum of practice lends itself to difficulty categorizing the areas of practice that exist, especially considering the many countries and different health care systems. In this section, the categorization from the American Occupational Therapy Association is used. However, there are other ways to categorize areas of practice in OT, such as physical, mental, and community practice (AOTA, 2009). These divisions occur when the setting is defined by the population it serves. For example, acute physical or mental health settings (e.g.: hospitals), sub-acute settings (e.g.: aged care facilities), outpatient clinics and community settings.
In each area of practice below, an OT can work with different populations, diagnosis, specialities, and in different settings.
Occupational therapy during WWI: bedridden wounded are knitting.
Children and youth
Occupational therapists work with infants, toddlers, children, and youth and their families in a variety of settings including schools, clinics, and homes.
[32] Occupational therapists assist children and their caregivers to build skills that enable them to participate in meaningful occupations. Occupational therapists also address the psychosocial needs of children and youth to enable them to participate in meaningful life events. These occupations may include: normal growth and development, feeding, play, social skills, and education.
[33]
Occupational therapy with Children and Youth may take a variety of forms: [32][33]
Promoting a wellness program in schools to prevent childhood obesity
Facilitating hand writing development in school-aged children
Promoting functional skills for children with developmental disabilities
Providing individualized treatment for sensory processing difficulties
Addressing psychosocial needs of a child and teaching effective coping strategies
Health and wellness
The practice area of Health and Wellness is emerging steadily due to the increasing need for wellness-related services in occupational therapy. A connection between wellness and physical health, as well as mental health, has been found; consequently, helping to improve the physical and mental health of clients can lead to a general increase in wellness.
[34]
As a practice area, health and wellness can include a focus on the following:
[34][35]
Prevention of disease and injury
Prevention of secondary conditions
Promotion of the well-being of those with chronic illnesses
Reduction of health care disparities
Enhancement of factors that impact quality of life
Promotion of healthy living practices, social participation, and occupational justice
Mental health
According to the World Health Organization, mental illness is one of the fastest growing forms of disability.
[36]
There is a focus on prevention and treatment of mental illness in populations including children, youth, the aging, and those with severe and persistent mental health issues.
[37]
Occupational therapists provide mental health services in a variety of settings including hospitals, day programs, and long-term-care facilities.
[38]
Occupational therapists help individuals with mental illness acquire the skills to care for themselves or others including the following: [39]
schedule maintenance
routine building coping skills medication management employment education
community access and participation social skills development
leisure pursuits money management
childcare
Productive aging
Occupational therapists work with older adults to maintain independence, participate in meaningful activities, and live fulfilling lives. Some examples of areas that occupational therapists address with older adults are driving, continuing to live at home, low vision, and dementia or Alzheimer’s Disease (AD).
[40] When addressing driving, driver evaluations are administered to determine if drivers are safe behind the wheel. To enable independence of older adults at home, occupational therapists perform fall screens and evaluate older adults functioning in their homes and recommend specific home modifications. When addressing low vision, occupational therapists modify tasks and the environment.
[41] While working with individuals with AD, occupational therapists focus on maintaining quality of life, ensure safety, promote independence, and utilize retained abilities.
[42]
Rehabilitation
Occupational therapists address the needs of rehabilitation, disability, and participation. Occupational therapists provide treatment for adults with disabilities in a variety of settings including hospitals (acute rehabilitation, in-patient rehabilitation, and out-patient rehabilitation), home health, skilled nursing facilities, and day rehabilitation programs. When planning treatment, occupational therapists address the physical, cognitive, psychosocial, and environmental needs involved in adult populations across a variety of settings.
Occupational therapy with adult rehabilitation, disability, and participation may take a variety of forms:
Working with adults with autism at day rehabilitation programs to promote successful relationships and involvement in the community [43]
Increasing the quality of life for a cancer survivor or individual with cancer by engaging them in occupations that are meaningful, providing therapy for lymphedema management, implementing anxiety and stress reduction methods, and fatigue management [44]
Training individuals with hand amputations how to put on and take off a myoelectrically controlled limb as well as training for functional use of the limb [44]
Using and implementing new technology such as speech to text software and Nintendo Wii video games [45]
Communicating via telehealth methods as a service delivery model for clients who live in rural areas [46]
Providing services for those in the armed forces such as cognitive treatment for traumatic brain injury, training and education towards the use of prosthetic devices for amputations, and treatment for psychological distress as a result of post-traumatic stress disorder [47]
Travel occupational therapy
Because of the rising need for occupational therapists, [48] many facilities are opting for travel occupational therapists —who are willing to travel, often out of state, to work temporarily in a facility. Assignments may run as short as 8 weeks or as long as 9 months, but typically last 13 –26 weeks in length.
[49]
Work and industry
Occupational therapists may also work with clients who have had an injury and are trying to get back to work. Testing may be completed to simulate work tasks in order to determine best matches for work, accommodations needed at work, or the level of disability. Work conditioning and hardening are approaches used to restore performance skills needed on the job that may have changed due to an illness or injury. Occupational therapists can also prevent work related injuries through ergonomics and on site work evaluations.
[50]
Occupational therapy approaches
Services typically include:
Teaching new ways of approaching tasks [51]
How to break down activities into achievable components e.g. sequencing a complex task like cooking a complex meal [51]
Comprehensive home and job site evaluations with adaptation recommendations.
Performance skills assessments and treatment.
Adaptive equipment recommendations and usage training.
Environmental adaptation including provision of equipment or designing adaptations to remove obstacles or make them manageable [51]
Guidance to family members and caregivers.
[52]
The use of creative media as therapeutic activity
Activity analysis
Activity analysis has been defined as a process of dissecting an activity into its component parts and task sequence in order to identify its inherent properties and the skills required for its performance, thus allowing the therapist to evaluate its therapeutic potential.
[53]
Theoretical frameworks
Occupational Therapists use a number of theoretical frameworks with which to frame their practices. Note that terminology has differed between scholars. Theoretical bases for framing a human and their occupation being include the following:
Frames of reference and generic models
Frames of reference or generic models are the overarching title given to a collation of compatible knowledge, research and theories that form conceptual practice.
[54] More generally they can be defined as "those aspects which influence our perceptions, decisions and practice".
[55]
Person Environment Occupation Performance Model
Occupational Therapy Intervention Process Model (OTIPM) (Anne Fisher and others)
Occupational Performance Process Model (OPPM)
Model of Human Occupation ( MOHO ) (Gary Kielhofner and others)
MOHO was first published in 1980. It explains how people select, organise and undertake occupations within their environment. The model is supported with evidence generated over thirty years and has been successfully applied throughout the world.
[56]
Canadian Model of Occupational Performance and Engagement (CMOP-E)
Occupational Performances Model - Australia (OPM-A) (Chris Chapparo & Judy Ranka)
The OPM(A) was conceptualized in 1986 with its current form launched in 2006. The OPM(A) illustrates the complexity of occupational performance, the scope of occupational therapy practice, and provides a framework for occupational therapy education.
[57]
Kawa (River) Model (Michael Iwama)
Functional Group Model
Functional Information-Processing Model
Biomechanical Frame of Reference
The Biomechanical Frame of Reference is primarily concerned with motion during occupation. It is used with individuals who experience limitations in movement,
inadequate muscle strength or loss of endurance in occupations. The Frame of Reference was not originally compiled by Occupational Therapists, and Therapists should translate it to the Occupational Therapy perspective, [58] to avoid the risk of movement or exercise becoming the main focus.
[59]
Rehabilitative (compensatory)
Neurofunctional ( Gordon Muir Giles and Clark-Wilson)
Cognitive Disabilities
Dynamic Systems Theory
Sensory Integration
Lifestyle Performance Model (Fidler)
Client-Centered Frame of Reference
This Frame of Reference is developed from the work of Carl Rogers . It views the client as the center of all therapeutic activity, and the client's needs and goals direct the delivery of the Occupational Therapy Process.
[60]
Cognitive-Behavioural Frame of Reference
Psychodynamic Frame of Reference
Ecology of Human Performance Model
Recovery Models & Self-Management Models
Curtin pARTicipation Model
Knowledge Translation of Self-Management Models [61]
Life-Skills Tree Model [62]
Occupational Therapy - Mahidol Clinical System (OT-MCS) Model [63]
Occupational therapy and ICF
The International Classification of Functioning, Disability and Health (ICF) i s a framework to measure health and ability by illustrating how these components impact one’s function. This relates very closely to the Occupational Therapy Practice Framework as it is stated, “The profession’s core beliefs are in the positive relationship between occupation and health and its view of people as occupational beings”.
[64]
The ICF is also built into the 2nd edition of the practice framework. Activities and participation examples from the ICF overlap Areas of Occupation, Performance Skills, and Performance Patterns in the framework. The ICF also includes contextual factors
(environmental and personal factors) that relate to the context in the framework. In addition, body functions and structures classified within the ICF help describe the client factors as described in the OT framework.
[65]
Further exploration of the relationship between occupational therapy and the components of the ICIDH-2 (revision of the original International Classification of
Impairments, Disabilities, and Handicaps (ICIDH); later becoming the ICF ) was conducted by McLaughlin Gray.
[66] First, the ICF is an international framework and provides an opportunity for the occupational therapy field to become better known across the globe. Second, the ICF provides occupational therapists with a global language to describe their expertise to the larger international health care community. The ICF uses a positive, holistic language emphasizing skills, capacities, and strengths of an individual rather than focusing on one’s deficits and disabilities. This is similar to the outlook of occupational therapists. Third, the ICF includes environmental and personal contextual factors which are incorporated into the theory behind occupational therapy. It is important to take into consideration an individual’s personal, environmental, and occupational factors to develop an effective intervention.
[13] The last notable application of the ICF to occupational therapy is the recognition of cultural patterns in occupation. Culture has significance on an individual’s activities and participation and it is important to keep this in mind when treating an individual.
Although the ICF can be very useful for occupational therapists, it is noted in the literature that occupational therapists should use specific occupational therapy vocabulary along with the ICF in order to ensure correct communication about specific concepts.
[67]
The ICF might lack certain categories to describe what occupational therapists need to communicate to clients and colleagues. It also may not be possible to exactly match the connotations of the ICF categories to occupational therapy
terms. The ICF is not an assessment and specialized occupational therapy vocabulary should not be replaced with ICF terminology [68] The ICF is an overarching framework for current therapy practices.
World Occupational Therapy Day
October 27 is World Occupational Therapy Day and celebrates the many different ways occupational therapists can change the lives of others.
[69] In honor of World
Occupational Therapy Day, occupational therapists from around the world participate in an Occupational Therapy Global Day of Service (OTGDS) [70] This event gives occupational therapy practitioners and students worldwide the opportunity to give back to their communities through service and to promote the profession through helping others. Through social media, participants were also able to communicate with the global occupational therapy community to discuss their OTGDS activities and learn about how others are celebrating World Occupational Therapy Day. Providing free treatment, volunteering at local organizations, and participating in community events are some of the ways occupational therapists celebrate OTGDS and World Occupational Therapy Day.
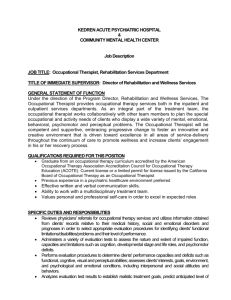
Occupational Therapy Professionals: Education and Salary
Certified Occupational Therapists typically hold Masters or Doctoral degrees in Occupational Therapy from an ACOTE accredited institution. To practice in the United
States, occupational therapists must receive a master's degree and pass a licensing examination to become certified by the National Board for Certification in
Occupational Therapy (NBCOT).
The average wages of a permanent occupational therapist in the United States are approximately $76,400/year.
[71] Traveling occupational therapists may have higher wages (approximately $113,600/year).
[72] They also enjoy benefits such as free housing, health/medical insurance, travel reimbursement, loyalty bonuses, and a 401k plan [ reference needed ]. Most commonly (43%), travel occupational therapists enter the industry between the ages of 21-30.
[72] The average annual income for occupational therapy assistants as of 2009 was $50,840. The middle 50% earned between $41,200 and $59,890. Salaries for the lowest 10% were around $33,350, while the highest 10% earned approximately $68,450, with top pay upwards of $105,000.
[73]
SAMPLE ARTICLE:
Complex Regional Pain Syndrome
Save This Article For Later
Share this:
Font size:
AAA
Complex regional pain syndrome (CRPS), also called reflex sympathetic dystrophy syndrome, is a chronic pain condition in which high levels of nerve impulses are sent to an affected site. Experts believe that CRPS occurs as a result of dysfunction in the central or peripheral nervous systems.
CRPS is most common in people aged 20-35. The syndrome also can occur in children; it affects women more often than men.
There is no cure for CRPS.
What Causes Complex Regional Pain Syndrome?
CRPS most likely does not have a single cause; rather, it results from multiple causes that produce similar symptoms. Some theories suggest that pain receptors in the affected part of the body become responsive to catecholamines , a group of nervous system messengers. In cases of injury-related CRPS, the syndrome may be caused by a triggering of the immune response which may lead to the inflammatory symptoms of redness, warmth, and swelling in the affected area. For this reason, it is believed that CRPS may represent a disruption of the healing process.
What Are the Symptoms of Complex Regional Pain Syndrome?
The symptoms of CRPS vary in their severity and length. One symptom of CRPS is continuous, intense pain that gets worse rather than better over time. If CRPS occurs after an injury, it may seem out of proportion to the severity of the injury. Even in cases involving an injury only to a finger or toe, pain can spread to include the entire arm or leg. In some cases, pain can even travel to the opposite extremity. Other symptoms of CRPS include:
"Burning" pain
Swelling and stiffness in affected joints
Motor disability, with decreased ability to move the affected body part
Changes in nail and hair growth patterns: There may be rapid hair growth or no hair growth.
Skin changes: CRPS can involve changes in skin temperature -- skin on one extremity can feel warmer or cooler compared to the opposite extremity. Skin color may become blotchy, pale, purple or red. The texture of skin also can change, becoming shiny and thin. People with CRPS may have skin that sometimes is excessively sweaty.
CRPS may be heightened by emotional stress.
How Is Complex Regional Pain Syndrome Diagnosed?
There is no specific diagnostic test for CRPS, but some testing can rule out other conditions. Triple-phase bone scans can be used to identify changes in the bone and in blood circulation. Some health care providers may apply a stimulus (for example, heat, touch, cold) to determine whether there is pain in a specific area.
Making a firm diagnosis of CRPS may be difficult early in the course of the disorder when symptoms are few or mild. CRPS is diagnosed primarily through observation of the following symptoms:
The presence of an initial injury
A higher-than-expected amount of pain from an injury
A change in appearance of an affected area
No other cause of pain or altered appearance
How Is Complex Regional Pain Syndrome Treated?
Because there is no cure for CRPS, the goal of treatment is to relieve painful symptoms associated with the disorder. Therapies used include psychotherapy , physical therapy , and drug treatment , such as topical analgesics, narcotics, corticosteroids, antidepressants and antiseizure drugs .
Other treatments include:
Sympathetic nerve blocks: These blocks, which are done in a variety of ways, can provide significant pain relief for some people. One kind of block involves placing an anesthetic next to the spine to directly block the sympathetic nerves.
Surgical sympathectomy: This controversial technique destroys the nerves involved in CRPS. Some experts believe it has a favorable outcome, while others feel it makes CRPS worse. The technique should be considered only for people whose pain is dramatically but temporarily relieved by selective sympathetic blocks.
Intrathecal drug pumps: Pumps and implanted catheters are used to send pain-relieving medication into the spinal fluid.
Spinal cord stimulation: This technique, in which electrodes are placed next to the spinal cord, offers relief for many people with the condition.
SPEECH THERAPY
National approaches to speech and language pathology
Speech-language pathology is known by a variety of names in different countries:
Speech-language pathology (SLP) in the United States [1] , Canada [2] , Malta [3] , Italy [4] , and in the Philippines
Speech and language therapy (SLT) in the United Kingdom, Ireland [5] , and South Africa [6] . Within the United Kingdom a Speech and Language Therapy team is sometimes referred to as the "SALT" team, to avoid confusion with Senior Leadership Team. S< is preferable however, and closer to the official abbreviation SLT used
by RCSLT (Royal College of Speech and Language Therapists) [7] .
Speech and language therapist (logopedist) are educated to give therapy in the Netherlands and Hungary.
Speech pathology in Australia [8] , and the Philippines
Speech-language therapy in New Zealand
Speech therapy in India [9] , Hong Kong [10] and other Asian countries.
Speech and language pathologist in the Netherlands, the title for graduates from University who can participate in research.
Prior to 2006, the practice of Speech-Language Pathology in the United States was regulated by the individual states. Since January 2006, the 2005 "Standards and
Implementation Procedures for the Certificate of Clinical Competence in Speech-Language Pathology" guidelines given by The American Speech-Language-Hearing
Association (ASHA) have determined the qualification requirements to obtain "Speech-Language Pathology Clinical Fellowship". First, individuals must obtain an undergraduate degree, which may be in a field related to speech-language-hearing sciences. Second, individuals must graduate from an accredited master's program in speech-language pathology. Many graduate programs will allow coursework absent in undergraduate study to be completed during graduate work. Some states licensure regulations differ. The Certificate of Clinical Competence (CCC) is granted after the clinical fellowship year (CFY), when the individual provides services under the supervision of an experienced and licensed SLP. After a CCC in Speech-Language Pathology is awarded, continuing education is required every three years to maintain certification.
[3] Post-master's graduate study for a Speech-Language Pathologist may consist of academic, research, and clinical practice. A doctoral degree (Ph.D or
Speech-Language Pathology Doctorate) is currently optional for clinicians wishing to serve the public. Speech-Language Pathology Competencies
The practice of speech-language pathology may include the following competencies (ASHA, 1996b):
Provide screening, identification, assessment, diagnosis, treatment, intervention, and follow-up services for people with speech and language disorders
Provide consultation and counseling, and make referrals when appropriate
Train and support family members and other communication partners of individuals with speech, voice, language, communication, and swallowing disabilities
Develop and establish effective augmentative and alternative communication techniques and strategies
Select, fit, and establish the effective use of appropriate prosthetic/adaptive devices for speaking and swallowing
Use instrumental technology to diagnose and treat disorders of communication and swallowing
Provide aural rehabilitation and related counseling services to individuals with hearing loss and to their families
Collaborate in the assessment of central auditory processing disorders in cases inwhich there is evidence of speech, language, and/or other cognitive-communication disorders
Conduct pure-tone air conduction hearing screening and screening typmanometry for the purpose of the initial identification and/or referral of individuals with other communication disorders or possible middle ear pathology
Enhance speech and language proficiency and communication effectiveness, including but not limited to accent reduction, collaboration with teachers of English as a second language, and improvement of voice, performance, and singing
Train and supervise support personnel
Develop and manage academic and clinical programs in communication sciences and disorders
Conduct, disseminate, and apply research in communication sciences and disorders
Measure outcomes of treatment and conduct continuous evaluation of the effectiveness of practices and programs to improve and maintain quality of services
- See more at: http://www.asha.org/Careers/job/slp_comp/#sthash.W5ULr4a0.dpuf
The Speech-Language Pathology vocation
Speech-Language Pathologists provide a wide range of services, mainly on an individual basis, but also as support for individuals, families, support groups, and providing information for the general public. Speech services begin with initial screening for communication and swallowing disorders and continue with assessment and diagnosis, consultation for the provision of advice regarding management, intervention and treatment, and provision counseling and other follow up services for these disorders.
cognitive aspects of communication (e.g., attention, memory, problem solving, executive functions).
speech ( phonation , articulation , fluency, resonance, and voice including aeromechanical components of respiration);
language ( phonology , morphology , syntax , semantics , and pragmatic/social aspects of communication) including comprehension and expression in oral, written, graphic, and manual modalities; language processing ; preliteracy and language-based literacy skills, phonological awareness.
swallowing or other upper aerodigestive functions such as infant feeding and aeromechanical events (evaluation of esophageal function is for the purpose of referral to medical professionals);
voice (hoarseness (dysphonia), poor vocal volume (hypophonia), abnormal (e.g. rough, breathy, strained) vocal quality). Research demonstrates voice therapy to be especially helpful with certain patient populations; individuals with Parkinson's Disease often develop voice issues as a result of their disease.
sensory awareness related to communication, swallowing, or other upper aerodigestive functions.
Multi-discipline collaboration
Speech-Language Pathologists collaborate with other health care professionals often working as part of a multidisciplinary team, providing referrals to audiologists and others; providing information to health care professionals (including doctors , nurses , occupational therapists , dietitians ), educators , behavior consultants ( applied behavior analysis ) and parents as dictated by the individual client's needs.
In relation to Auditory Processing Disorders [4] collaborating in the assessment and providing intervention where there is evidence of speech, language, and/or other cognitive-communication disorders.
The treatment for patients with cleft lip and palate has an obvious interdisciplinary character. The speech therapy outcome is even better when the surgical treatment is performed earlier.
[5]
Healthcare
Promote healthy lifestyle practices for the preservation of communication, hearing, or swallowing, or for the treatment of other upper aerodigestive disorders.
Recognizing the need to provide and appropriately accommodate diagnostic and treatment services to individuals from diverse cultural backgrounds and adjust treatment and assessment services accordingly.
Advocating for individuals through community awareness, education, and training programs to promote and facilitate access to full participation in communication, including the elimination of societal barriers.
Research
Conduct research related to communication sciences and disorders, swallowing disorders, or other upper aerodigestive functions.
Training
Education:
Speech Pathology is a Master's entry-level field. Clinicians may hold a Master's degree in Speech-Language Pathology (e.g. M.A., M.S., or M.Ed), a clinical doctorate in
Speech Language Pathology (e.g. CScD or SLP-D), or a Ph.D.
All clinicians are required to complete 400 clinical hours (25 observation hours during the undergraduate degree and 375 hours of graduate Clinical Practicum).
Must pass multiple Knowledge and Skills Acquisition (KASA) exams
Additional coursework at the undergraduate and graduate level as well as additional licensure is required if the SLP wishes to work in a K-12 school setting.
After all the above requirements have been met during the SLP’s path to earning the graduate degree:
Passing score on the National Speech-Language Pathology board exam (PRAXIS).
Successful completion of a clinical fellowship (CF). The CF is 36 weeks of full-time (35 hours per week) experience (or the equivalent part-time experience), totaling a minimum of 1260 hours).
[6]
American Speech and Hearing Association (ASHA) certificate of clinical competence (CCC) and full state licensure to practice, following successful completion of clinical fellowship (CF).
Continuing Education and Training Obligations:
Educate, supervise, and mentor future Speech-Language Pathologists.
[7]
Participate in continuing education.
Educate and provide in-service training to families, caregivers, and other professionals.
Train, supervise, and manage Speech-Language Pathology Assistants and other support personnel.
Educating and counseling individuals, families, co-workers, educators, and other persons in the community regarding acceptance, adaptation, and decisions about communication and swallowing.
[8]
Professional Suffix:
Credentials of a clinical fellow typically read as: M.A., CFY-SLP.
Credentials of a licensed SLP commonly read as: M.A., CCC-SLP, indicating a practitioner's graduate degree and successful completion of the fellowship year/board exams to obtain certification.
Salary by state or district
[ edit ]
Average salaries for speech-language pathologists vary somewhat throughout the United States, ranging on average between 40-90K depending on setting and years of experience.
Working environments
[ edit ]
Speech-Language Pathologists work in a variety of clinical and educational settings. SLPs work in public and private hospitals , skilled nursing facilities (SNFs), long-term acute care (LTAC) facilities, hospice , [9] and home healthcare. SLPs may also work as part of the support structure in the education system, working in both public and private schools , colleges , and universities.
[10] Some speech-language pathologists also work in community health, providing services at prisons and young offenders' institutions or providing expert testimony in applicable court cases.
[11]
Subsequent to ASHA's 2005 approval of the delivery of Speech-Language Pathology services via video conference, or telepractice,
[12]
SLPs have begun delivering services via this service delivery method.
Methods of assessment
[ edit ]
For more details on this topic, see Speech and language assessment .
Assessment of speech, language, cognition, and swallowing can consist of informal (non-standard or criterion based) assessments, formal standardized tests, instrumental measures, language sample analyses, and oral motor mechanism exam. Informal assessments rely on a clinician's knowledge and experience to evaluate an individual's abilities across areas of concern. Formal standardized testing is used to measure an individuals' abilities against peers. Instrumental measures (e.g., nasometer)utilizes equipment to measure physiological or anatomical impairments (e.g., Fiberoptic Endoscopic Evaluation of Swallowing (FEES) or Modified Barium
Swallow Study (MBS)). Oral motor assessments review the strength, co-ordination, range of movement, symmetry, and speed of cranial nerves V, VII, IX, X and XII.
Referrals to Speech and Language Pathologists should be made if there are any concerns regarding slow or limited communication development in children, cognition
(limited attention, disorganization etc. following by a Traumatic Brain Injury), difficulty with word-finding, errors in speech sound production, or for Augmentative Alternative
Communication needs.
Clients and patients requiring speech and language pathology services
[ edit ]
Speech-Language Pathologists work with clients and patients who can present a wide range of issues.
Infants and children
[ edit ]
Infants with injuries due to complications at birth, feeding and swallowing difficulties, including dysphagia
Children with mild, moderate or severe:
Genetic disorders that adversely affect speech, language and/or cognitive development including cleft palate , Down syndrome , DiGeorge syndrome
Attention deficit hyperactivity disorder [13][14]
Autism , [15] including Asperger syndrome [16]
Developmental delay
Feeding disorders- including oral motor deficits
Cranial nerve damage
Hearing loss
Craniofacial anomalies that adversely affect speech, language and/or cognitive development
Language delay
Specific language impairment
Specific difficulties in producing sounds, called articulation disorders , (including vocalic /r/ and lisps)
Pediatric traumatic brain injury
Developmental verbal dyspraxia
Some children are eligible to receive speech therapy services, including assessment and lessons through the public school system . If not, private therapy is readily available through personal lessons with a qualified Speech-Language Pathologist or the growing field of telepractice.
[17] Teleconferencing tools such as Skype are being used more commonly as a means to access remote locations in private therapy practice, such as in the geographically diverse southern New Zealand.
[18] More at-home or
combination treatments have become readily available to address specific types of articulation disorders. The use of mobile applications in speech therapy is also growing as an avenue to bring treatment into the home.
Children and adults
[ edit ]
Cerebral Palsy
Head Injury ( Traumatic brain injury )
Hearing Loss and Impairments
Learning Difficulties including
Dyslexia
[19][20]
Specific Language Impairment (SLI)
Auditory Processing Disorder [21]
Adults
[ edit ]
Physical Disabilities
Speech Disorders (like Cluttering )
Stammering , Stuttering ( disfluency )
Stroke
Voice Disorders ( dysphonia )
Language Delay
[22]
Motor speech disorders ( dysarthria or Developmental verbal dyspraxia )
Adults with mild, moderate, or severe eating, feeding and swallowing difficulties, including dysphagia
Adults with mild, moderate, or severe language difficulties as a result of:
Stroke
Progressive neurological conditions
Alzheimer's disease , dementia ,
Huntington's disease ,
Multiple Sclerosis ,
Motor Neuron Diseases ,
Parkinson's disease ,
cancer of the head, neck and throat (including laryngectomy ) mental health issues transgender voice therapy (usually for male-to-female individuals)
Naming difficulties (anomia)
Dysgraphia, agraphia
Cognitive communication disorders
Pragmatics
Laryngectomies
Tracheostomies
Oncology (Ear, nose or throat cancer)