MENNONITE COLLEGE OF NURSING
advertisement

MENNONITE COLLEGE OF NURSING at Illinois State University
Maternal Infant Nursing - 316
LECTURE GUIDE
Complications of the Neonate-- Unit VI--D
UNIT IV-D COMPLICATIONS OF THE NEONATE
Hyperbilirubinemia in the Neonate
Clinically evident jaundice in the 1st 24 hours of life.
A.
Causes of neonatal jaundice--OVERPRODUCTION
a. Immune hemolysis--Rh or ABO Incompatibility
b. Non-immune hemolysis—
c. red cell mass or fragility
d. Extravascular blood—vacuum extractor, cephalhematoma
e. Ethnicity—Asian, African-American, Mediterranean
B. Causes of neonatal jaundice—UNDER EXCRETION
a. Suboptimal breast feeding
C. Causes of neonatal jaundice—Prematurity
a. Hypoxia, asphyxia, hypothermia, acidosis, hypoglycemia
b. Immature liver function—
c. Polycythemia of the newborn (Hct > 65% at birth)
d. Enclosed hemorrhage (cephalhematoma, large bruises)
e. UTI, sepsis
D. Causes of neonatal jaundice—bood type
a. Rh Incompatibility
b. ABO Incompatibility
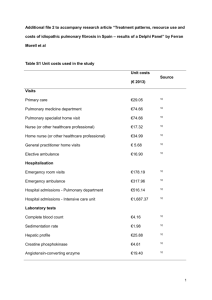
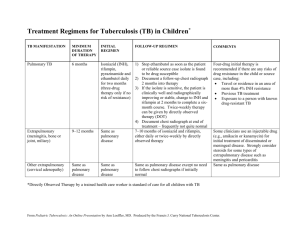
E. Treatment options— AAP changed the criteria in 2004 and added new criteria with nomogram based on
the age of the neonate in hours and the level of bilirubin
a.
b.
c.
d.
e.
Phototherapy—review nursing interventions in first module on neonate.
Exchange Transfusion
IVIG
Change what is fed—interrupt breastfeeding temporarily if indicated
“Hydration”
F. Severe complications: Kernicterus—SB > 20mg/dl—may lead to mental retardation and possible death.
May also cause 8th cranial nerve injury leading to hearing loss.
G. Prevention—
a. Careful TcB assessment within 1st 24 hours to identify pathologic jaundice.
b. Starting phototherapy at the appropriate time
c. Re-check in the office on day 3-5 without fail to re-assess TcB or SB.
d. Give all families specific information on jaundice before discharge including how to assess for
jaundice, sx of jaundice r/t poor feeding, lethargic behavior
H. Two levels of bilirubin evaluated:
a. Conjugated bilirubin-- the water-soluble form. also called "Direct". Increase in the direct bili is
usually caused by an obstruction or absence of liver bile ducts (ie. biliary atresia or serious
hepatic problems).
b. Unconjugated bilirubin-- the fat-soluble form also called “Indirect:. Produced when hemoglobin
is broken down, usually in the liver. This is the most common which we discussed earlier in the
semester
C. Medical Treatment-1. Prenatal-a.
Serial amniocentesis with OD450 evaluation followed by
b.
Possible intrauterine exchange transfusion: a small amount of fetus' blood (10-20 ml) is
removed and replaced with compatible unsensitized blood (in Rh incompatibility,
group O, Rh-neg.is used or packed RBC's reconstituted with fresh frozen plasma.
In ABO incompatibility, group O with Rh-specific cells and low titers of anti-A and anti-B
donor blood is used.
c.
Calcium gluconate is often given to prevent hypocalcemia in the fetus. Every 4-8 hours after the
transfusion, serum bili levels are checked. Repeat exchange transfusions may be necessary.
2. Neonatal-- Photo therapy
a. NSG GOALS:
1) Maintain a WARM, safe environment
2) Prevent injury to neonate
3) Adequate hydration
b. INTERVENTIONS:
1) Monitor incubator & babe's temp at least q 3-4hrs to prevent hyperthermia.
2) Ensure eye patches are in place to prevent eye damage or obstruction of nose.
3) Remove eye patches for feedings to assess eyes for sx of infection, and foster bonding.
4) Monitor I & O to identify neg. fluid balance and dehydration. Note green stools.
5) Shield genitalia with facemask or small diaper to prevent exposure of skin over gonads and
genitalia to beam of light.
6) Observe skin color in natural light to identify early sx of "bronzing" so tx can be D/C'd in a
timely manner. Do NOT use lotion while under lights as it can cause > bronzing of skin.
7) Ensure that lock of isolette doors are engaged to prevent infant from falling.
8) Maintain skin integrity with frequent diaper changes.
9) Educate parents regarding all the above and include them in the plan of care.
10) Change infant's position q 2 hours or with each feeding to expose as much of the skin as
possible.
II. Complications Related to Gestational Age and Birth Weight
A. Preterm Infants
1. Respiratory Distress Syndrome(RDS) - previously referred to as Hyaline Membrane Dz (HMD).
a. Epidemiology: leading cause of death in premies weighing between 1000 and 1500gms.
approx. 7000 deaths/year in US.
*b. Definition: a disorder of the lungs characterized by pulmonary hypoperfusion, hypoxemia,
metabolic and respiratory acidosis, classic changes in lung tissue leading to decreased
lung compliance, capillary damage, and alveolar necrosis.
*c. Signs and Symptoms: Retractions, cyanosis, tachypnea (>60/minute), rales, expiratory
grunting, flaring nares, see-saw respirations, SaO2 < 90%.
(Review Silverman-Andersen Score, p. 947)
2. Problems in RDS: Diminished Pulmonary Compliance
Pulmonary compliance is the capacity of the lung to expand with inspiration. In RDS, the lungs
are "stiff" due to the lack of surfactant that leads to dyspnea and an increased workload
on the lungs.
3. Causes of RDS: 1)prematurity and 2) asphyxia-- both of these interfere with surfactant production.
*4. Infants at risk for RDS include: white (Caucasian), premature, low birth weight(LBW), or very LBW
males who are IDM (infants of diabetic mothers), have a hx of fetal asphyxia, a 2nd born twin, or
who have an older sibling with a hx of RDS.
in
5. Medical treatment
* a. Prenatal-- Betamethasone (Celestone)
Dose & admin: 12mg IM to mother q 24h X 2 or 5mg q 24h X 2.
Peak effect is 48h after 1st dose and lasts 7 days. {fetus must be 28-34 wks gest. & delivery
delayed 24-48 hrs. to be effective
Action: binds with glucocorticoid receptors in alveolar cell to increase production of surfactant
fetus. Helps to decrease incidence of RDS, IVH, and NEC
Risk: watch use with betamimetic therapy (Ritodrine or Brethine) for PTL as there is increased
risk of pulmonary edema.
b. Neonatal-a. Maintain adequate OXYGENATION: oxyhood with humidified O2 or ventilator with ETTube if
PaO2 decreases or baby becomes tachypneic (>60-80 breaths/minute).
PEEP--positive end expiratory pressure
CPAP--continuous positive airway pressure
Jet ventilator or Oscillating ventilator- very high frequency at lower pressures help decrease
incidence of Chronic Lung Disease (CLD) formerly known as Bronchopulmonary
Dysplasia (BPD).
b. Correct acid/base imbalance--Na+bicarb IV (often via Umbilical Vein Catheter UVC),
--close monitoring of blood gasses via pulsoximetry and ABG's from Umbilical Artery
Catheter(UAC)
c. Chest x-rays-- show atelectasis, white opacities in lungs
d. Artificial surfactant via nebulizer through ETT--Exosurf / Surfanta, or other trade name has
been shown to effectively increase pulmonary compliance.
e. ECMO--extracorporeal membrane
oxygenation generally for emergencies only
f. Liquid oxygen may be administered via the ETT.
6. Complications of RDS and Prematurity
a. Retinopathy of Prematurity (ROP)—caused by severe vasoconstriction of the immature retinal
vasculature, followed by hypoxia in those areas. This may eventually lead to formation of fibrotic
tissue behind the lens; associated with retinal detachment and arrested eye growth. Recent studies
have shown that level of prematurity has greatest impact on the severity of ROP. Many other
causes may also contribute to this problem that is difficult to prevent .
b. Chronic Lung Disease (CLD) formerly called Bronchopulmonary Dysplasia (BPD)-- Chronic pulmonary
disease of multifactorial etiology characterized initially by alveolar and bronchial necrosis, which
results in bronchial metaplasia and interstitial fibrosis. Appears in x-ray as generalized small,
radiolucent cysts within the lungs. Often the result of long-term ventilator therapy in premies which
predisposes them to chronic lung problems.
c. Intraventricular hemorrhage (IVH)-- Hemorrhage occurs in tissue surrounding ventricles of the brain.
Blood enters brain cavities. It is the most common CNS hemorrhage secondary to hypoxia and
hypercapnia. Grades I - IV. Grade IV is the most severe with the poorest prognosis.
d. Pneumothorax-- an acute complication in which the alveoli rupture, air enters the pleural space, and
lung tissue collapses. Sx: Sudden tachypnea, nasal flaring, grunting, and severe retractions with
sudden drop in SaO2. Immediate intervention: Chest tube insertion to remove air and fluid and
allow lungs to expand normally.
e. Patent Ductus Arteriosus (PDA)--As a result of hypoxia, the pulmonary vasculature constricts,
pulmonary vascular resistance increases, and pulmonary blood flow in reduced which in turn may
cause a return to fetal circulation as the ductus opens and blood flow is shunted around the lungs.
Tx includes ventilatory support, fluid restriction, and diuretics and Indomethacin (Indocin) which is a
prostaglandin inhibitor that causes the PDA to constrict in ~85% of cases.
f.
Necrotizing Enterocolitis (NEC)--necrosis of the bowel in preterm infants associated with mucosal
injury from asphyxia and ischemia. Hypoxia leads to "gut shunting" allowing entrance of bacteria
into mucosal lining. Surgical intervention often necessary with temporary colostomy resulting in
"short gut syndrome". Mortality rate is often high--30-40%.
B. Post-Term Infants
1. Birth asphyxia--the inability to make the transition to extrauterine life which leads to a return to fetal
circulatory patterns. Many of the manifestations seen in an apneic infant are similar to those seen in
RDS: Hypoxia, hypercarbia, acidosis (pH < 7.20).
Etiology: 1. Uteroplacental insufficiency
2. Impaired fetal circulation (trauma)
3. Impaired blood flow through umbilical cord
4. Impaired respiratory effort i.e., Meconium Aspiration, severe neonatal narcosis
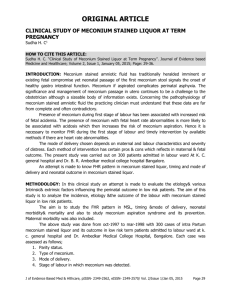
2. Meconium Aspiration Syndrome (MAS)
Definition: when aspirated meconium adheres to airways and alveoli in a ball-valve action uneven
obstruction and inhibits airflow to and from gasexchanging surfaces hyperinflation and
hypoxemia and acidemia increased pulmonary vascular resistance R to L shunting. Alveoli
become overdistended and rupture pneumothorax. Meconium also causes a chemical pneumonitis.
Etiology: meconium stained fluid in utero
Treatment: Prevention of aspiration is key to management. MD. or midwife should aspirate mouth and
nares when head is delivered and still on the perineum. If the meconium is thick, the glottis is visualized
and suctioning of meconium from the trachea is done. High ambient O2 and controlled ventilation,
possibly ECMO, prophylactic antibiotics.
3. Persistent Pulmonary Hypertension of the Newborn (PPHN)—
Definition: Also called persistent fetal circulation because there is right-to-left shunting of blood away
from the lungs and through the fetal ductus arteriosus and patent foramen ovale.
Etiology: often associated with postmaturity syndrome, RDS, MAS, intrapartal asphyxia, pneumonia, &
diaphragmatic hernia. Leads to hypoxemia and acidosis.
Treatment: The goal is to Pulmonary Vascular Resistance (PVR) & reverse the R L Shunting while
maintaining adequate tissue oxygenation. Hyperventilation will achieve respiratory alkalosis (pH > 7.55)
which will cause pulmonary vasodilatation and PVR .
Nursing Care: Close monitoring of VS & blood gasses is essential along with critical observation of the
ventilator therapy and the infant’s response to it and any meds administered. Care & support of parents
is essential with PPHN because of the serious nature of this disease.
C. Small for Gestational Age Infants (SGA
1. Hypoglycemia
Definition: Blood glucose below 30mg/dL in the first 72 hrs and below 40mg/dL after the first 3 days OR
Dextrostix result below 45mg/dL. **REMEMBER < 40mg/dL is worthy of notification of MD>
Sx: jitteriness, tremors, twitches, weak or high-pitched cry, lethargy, limpness, convulsions, cyanosis,
apnea, irreg. resp, diaphoresis, refusal to feed.
Treatment: RN can assess blood sugar before calling MD, but must have order to supplement with any
glucose whether orally or IV. If there are no other associated sx, D5W solution may be given orally and
the blood sugar rechecked approx. 1hr later. If other complications ie. cong heart dz, CNS dz, sepsis, etc,
then IV infusions of 5%-10% dextrose solutions are usually indicated with close monitoring of blood
sugar levels.
2. Cold Stress-- review thermoregulation and how it stresses preemie greatly. (Figure 33-11)
Goal: create a neutral thermal environment (NTE)
Factors that put preterm infants at > risk for cold stress:
a. Large body surface area in relation to weight
b. Minimal insulating subcutaneous fat
c. Limited stores of brown fat (an internal source for the generation of heat present in normal term
infants)
d. Decreased or absent reflex control of skin capillaries (shiver response)
e. Inadequate muscle mass activity (rendering the premie unable to produce its own heat)
f. Friable (easily damaged) capillaries
g. An immature temperature regulation center in the brain.