RELG 265 Final Exam Study Guide
advertisement
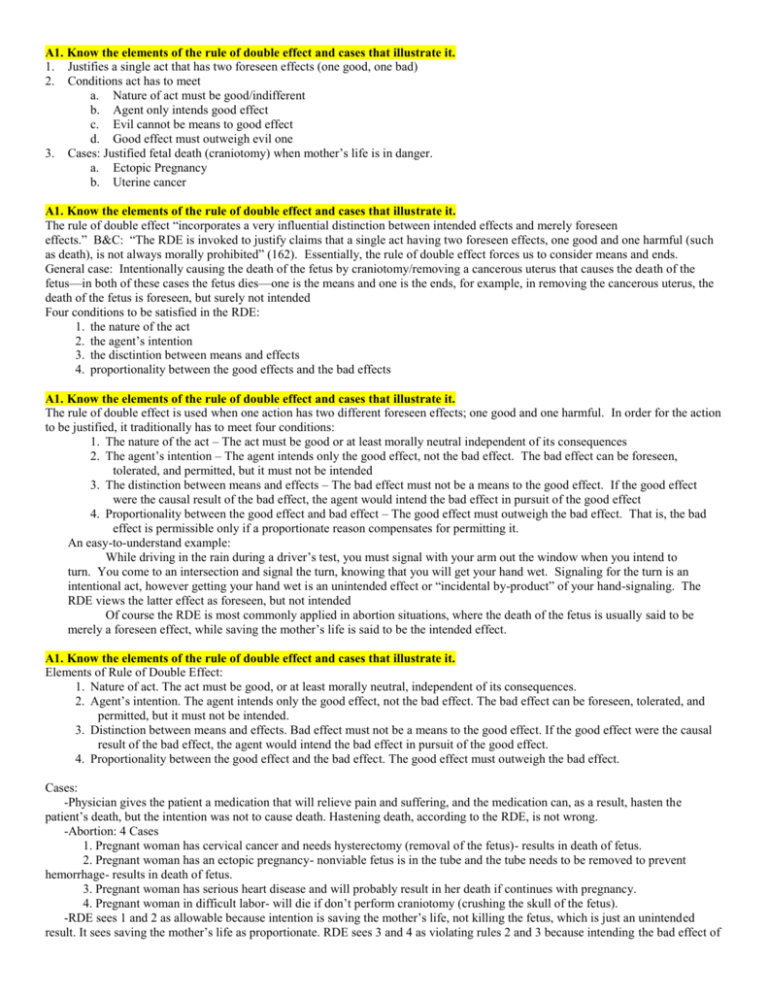
A1. Know the elements of the rule of double effect and cases that illustrate it. 1. Justifies a single act that has two foreseen effects (one good, one bad) 2. Conditions act has to meet a. Nature of act must be good/indifferent b. Agent only intends good effect c. Evil cannot be means to good effect d. Good effect must outweigh evil one 3. Cases: Justified fetal death (craniotomy) when mother’s life is in danger. a. Ectopic Pregnancy b. Uterine cancer A1. Know the elements of the rule of double effect and cases that illustrate it. The rule of double effect “incorporates a very influential distinction between intended effects and merely foreseen effects.” B&C: “The RDE is invoked to justify claims that a single act having two foreseen effects, one good and one harmful (such as death), is not always morally prohibited” (162). Essentially, the rule of double effect forces us to consider means and ends. General case: Intentionally causing the death of the fetus by craniotomy/removing a cancerous uterus that causes the death of the fetus—in both of these cases the fetus dies—one is the means and one is the ends, for example, in removing the cancerous uterus, the death of the fetus is foreseen, but surely not intended Four conditions to be satisfied in the RDE: 1. the nature of the act 2. the agent’s intention 3. the disctintion between means and effects 4. proportionality between the good effects and the bad effects A1. Know the elements of the rule of double effect and cases that illustrate it. The rule of double effect is used when one action has two different foreseen effects; one good and one harmful. In order for the action to be justified, it traditionally has to meet four conditions: 1. The nature of the act – The act must be good or at least morally neutral independent of its consequences 2. The agent’s intention – The agent intends only the good effect, not the bad effect. The bad effect can be foreseen, tolerated, and permitted, but it must not be intended 3. The distinction between means and effects – The bad effect must not be a means to the good effect. If the good effect were the causal result of the bad effect, the agent would intend the bad effect in pursuit of the good effect 4. Proportionality between the good effect and bad effect – The good effect must outweigh the bad effect. That is, the bad effect is permissible only if a proportionate reason compensates for permitting it. An easy-to-understand example: While driving in the rain during a driver’s test, you must signal with your arm out the window when you intend to turn. You come to an intersection and signal the turn, knowing that you will get your hand wet. Signaling for the turn is an intentional act, however getting your hand wet is an unintended effect or “incidental by-product” of your hand-signaling. The RDE views the latter effect as foreseen, but not intended Of course the RDE is most commonly applied in abortion situations, where the death of the fetus is usually said to be merely a foreseen effect, while saving the mother’s life is said to be the intended effect. A1. Know the elements of the rule of double effect and cases that illustrate it. Elements of Rule of Double Effect: 1. Nature of act. The act must be good, or at least morally neutral, independent of its consequences. 2. Agent’s intention. The agent intends only the good effect, not the bad effect. The bad effect can be foreseen, tolerated, and permitted, but it must not be intended. 3. Distinction between means and effects. Bad effect must not be a means to the good effect. If the good effect were the causal result of the bad effect, the agent would intend the bad effect in pursuit of the good effect. 4. Proportionality between the good effect and the bad effect. The good effect must outweigh the bad effect. Cases: -Physician gives the patient a medication that will relieve pain and suffering, and the medication can, as a result, hasten the patient’s death, but the intention was not to cause death. Hastening death, according to the RDE, is not wrong. -Abortion: 4 Cases 1. Pregnant woman has cervical cancer and needs hysterectomy (removal of the fetus)- results in death of fetus. 2. Pregnant woman has an ectopic pregnancy- nonviable fetus is in the tube and the tube needs to be removed to prevent hemorrhage- results in death of fetus. 3. Pregnant woman has serious heart disease and will probably result in her death if continues with pregnancy. 4. Pregnant woman in difficult labor- will die if don’t perform craniotomy (crushing the skull of the fetus). -RDE sees 1 and 2 as allowable because intention is saving the mother’s life, not killing the fetus, which is just an unintended result. It sees saving the mother’s life as proportionate. RDE sees 3 and 4 as violating rules 2 and 3 because intending the bad effect of the fetus’s death and the death of the fetus is the means of saving the mother’s life. In turn, it is not justified by proportionality, as saving the mother’s life does not outweigh killing a fetus. -Childress thinks a morally relevant difference between hysterectomy and craniotomy can’t be made because both don’t intend or want to kill the fetus and these acts do not show the difference between intending and foreseeing. One can say that crushing the head is the intended act, with the foreseen effect of the fetus’s death. RDE needs to make a clearer difference between intended and foreseen effects. A1. Know the elements of the rule of double effect and cases that illustrate it. Formulation of the RDE (EACH condition MUST be met): o The nature of the act must be good, or at least morally neutral, independent of its consequences. o The agent intends only the good effect, not the bad. The bad effect can be foreseen, tolerated, and permitted, but it must not be intended. o The bad effect must not be a means to the good. If the good effect were the causal result of the bad, the agent would then intend the bad effect in pursuit of the good effect. o The good effect must outweigh the bad effect. That is, the bad effect is permissible only if a proportionate reason compensates for permitting the foreseen bad effect. Four cases are addressed in B&C. They are as follows: (p.162-166) o Cancerous Uterus All four are satisfied. The removal of the uterus is the action undertaken. This does result in the death of the fetus, but the intention is to eliminate the cancer. The survival of the mother outweighs the destruction of the fetus. o Ectopic Pregnancy Nonviable fetus is in the fallopian tube. The tube is removed to prevent hemorrhage. All four are satisfied under the same logic as the cancerous uterus. o Serious Heart Condition (will result in death if pregnancy is carried to term) NOT justified. The action of terminating the fetus is what must be undertaken in order to save the mother, which violates condition 3. Thus the fetus’s death is intended. Violates 2. Cannot be justified by proportionality. Violates 4. o Difficult Labor (in which craniotomy is the only thing that will save the mother) When craniotomy is considered to be the killing of the fetus, it has the same problems as in the case above. But craniotomy COULD be considered the crushing of the fetal skull with the unintended result that the fetus dies. A more thorough discussion of intention and distinctions in the RDE (and its validity as a whole) is in B&C from 164-166. I felt as if that would be a bit extensive for this study guide (which will be like a million pages long already). A2. Explain the different religious perspectives on the status of the embryo/fetus. Roman Catholic- see Callahan (A4) The RC perspective: life begins at the moment of conception Judaism- presumption against abortion, but the fetus lacks full human status until head or greater part emerges in delivery, though some moral status through the pregnancy, beginning at 40 days and moral status increasing; abortion justifiable to protect life and health of pregnant woman Protestant (Mainline and Evangelical)- wide range of views, see chart in packet (27). Variety of Positions: 1. No moral issue 2. Abortion is morally problematic 3. Abortion is equivalent to homicide A2. Explain the different religious perspectives on the status of the embryo/fetus. Jewishà “Pregnancy Reduction in Jewish Law” by Fred Rosner 2. The unborn fetus is not considered a person until it is born and does not receive the same rights as a human being a. The fertilized egg is regarded as “mere fluid” until 40 days after conception 3. Instead, the fetus is treated a part of the mother’s body meaning that it doesn’t have its own identity and it’s life is dependent upon the mother 4. An analogy is given that a fetus is like the thigh of the mother and if the mother’s thigh turns gangrene, it must and shall be removed to protect the physical or mental health of the mother a. It is allowed to destroy the fetus to save the mother because the status and health of the mother comes first since the fetus is not a person and has no rights b. Only when the fetus is a threat to the mother’s life/health is it permissible to allow abortion of the fetus because… i. ii. iii. A potential human being is otherwise wasted, along with the wasteful use of human semen After 40 days, the fetus has “sufficient status” Under Jewish law, people are not allowed to harm themselves, and abortion is seen as harming oneself since the fetus is “a part of” the mother iv. Under Jewish law, people are not allowed to intentionally place themselves in danger and the act of abortion is seen as a dangerous act v. The Talmud states that abortion is only allowed when the mother’s life is threatened 5. Some Rabbi find it permissible to allow abortion for reasons like rape or incest because of concern for the well-being of the mother à the birth could negatively affect the mother’s mental/physical health 6. Abortion for the sake of the fetus is not allowed Catholicà “The Roman Catholic Position” Callahan / Congregation for the Doctrine of the Faith 2. The status of the embryo/fetus is equal to that of a human and must be treated as such, with the same respect and protection 3. The zygote must be treated as a human at the moment of conception and must receive the same rights as a person 4. Once conception occurs, the “life” must be protected with care 5. Prenatal testing is allowed as long as it doesn’t lead to abortion if abnormalities are found 6. Therapeutic procedures are allowed as long as they are used to benefit the embryo and promote life 7. Embryos obtained from in vitro fertilization are viewed as humans with rights and it is immoral to dispose any unused embryos that were produced via in vitro 8. Abortion is only allowed in the case of… a. An ectopic pregnancy b. A cancerous uterus 9. An innocent life is taken indirectly, meaning by an action that is designed and intended solely to achieve some other purpose even though death is a foreseen result a. Double Effectà The medical procedure is used to save the mother’s life with the direct intention of saving the mother and the foreseen but unintended/indirect result of the death of the fetus A2. Explain the different religious perspectives on the status of the embryo/fetus. Catholic position: the embryo/fetus is human life from conception Jewish position: the embryo/fetus is not “nefesh” (see below) until birth. Protestant positions: there are several conflicting positions, however for the most part, mainline Protestants place the embryo/fetus in the “potential for human life” category, while evangelical Protestants place an emphasis on individual conscience in determining the moral status. [The Catholic and Jewish positions are described with much greater detail in later questions; see below] A2. Explain the different religious perspectives on the status of the embryo/fetus. 2. Roman Catholic a. “Human life begins at the second of conception” b. Every unborn child must be regarded as a human person, with all the rights of a human person, from the moment of conception 3. Jewish Position a. An unborn fetus is not considered to be a person until it is born i. It is regarded as a part of the mother’s body b. The fetus is viewed as mere fluid until forty days where it gains some, but no significant rights 4. Protestants a. Many different religions b. Ultimately abortion is worng and should not be carried out c. Fetus has right to life A2. Explain the different religious perspectives on the status of the embryo/fetus. Judaism: o The fetus is not considered a full person (nefesh) until it is being born. o For the first forty days, the zygote is no more than “mere fluid”. o Between forty days and birth, the fetus has some status; its death requires cleaning processes, etc. Catholicism: o Human life begins at conception. o The fetus has full human rights and eliminating it is equivalent to murder. Protestant: WIDE range across denominations, etc o Mainline Generally pro-choice and do not consider the fetus to have full human status. o Evangelical Tend to be more aligned with Catholics A3. Define nefesh; explain Rosner’s position on the use of the “pursuer” metaphor in the context of maternal-fetal relations, and his position regarding when pregnancy reduction is allowed in Jewish law. Nefesh: a person— (literally means “soul”) not considered to be such until “egressed from the womb into the air of the world.” *Pregnancy reduction is allowed in Jewish law when it will save the mother’s life: “The permissibility to kill the unborn fetus to save the mother’s life rests upon the fact that an embryo is not considered a person until it is born.” *Pregnancy reduction is also allowed (abortion or embryotomy—where the life of the mother is endangered) because of “the argument of pursuit, whereby the fetus is pursuing (or endangering) the mother.” Essentially, taking the life of the fetus to protect “one’s fellow man,” the woman, is allowed. In this metaphor, the fetus is the “assailant.” A3. Define nefesh; explain Rosner’s position on the use of the “pursuer” metaphor in the context of maternal-fetal relations, and his position regarding when pregnancy reduction is allowed in Jewish law. Nefesh: in Hebrew it literally means “soul” The argument of “pursuit’ is used to justify abortion because it claims that the mother’s life is at risk because the fetus is “pursuing” the mother and therefore endangering her health à if the mother’s health is at risk, due to the “pursuing” fetus, then abortion should be allowed Rosner claims that this argument is incorrect because if the fetus is endangering the health/life of the mother, the child isn’t doing so intentionally because this is an act of God and is therefore a case of “heavenly pursuit” 2. Heavenly pursuit is a contradiction itself because the argument of pursuit is used to justify abortions but then the argument is overruled because the child is not held responsible for pursing the mother a. This problem is solved by the conclusion that the “nonperson” status of the fetus before birth doesn’t justify the embryos destruction which means that the embryo can’t be destroyed In Jewish law, a person cannot sacrifice one human life to save another human life 2. Rosner claims that pregnancy reduction is allowed in Jewish law ONLY in the case of “pursuit” when the pursuer is risking the life of another and must be stopped even if that means the pursuer must die 3. For example, in the case of sextuplets, pregnancy reduction cannot be justified because… a. it is unknown which 3 of the 6 fetuses are causing endangerment to the others b. even if 3 fetuses have an incurable disease, it cannot be said that their disease is directly harming the others A3. Define nefesh; explain Rosner’s position on the use of the “pursuer” metaphor in the context of maternal-fetal relations, and his position regarding when pregnancy reduction is allowed in Jewish law. Nefesh in Hebrew literally means soul, it is more or less the idea of “personhood.” In Jewish law, an unborn fetus is not considered to be a person/nefesh until it is born. The “pursuit” metaphor: The only exception to the principle that one may not sacrifice one life to save the life of another is the situation of “pursuit” (vide supra) where the pursuer who is threatening the life of his fellow man must be stopped even at the cost of the pursuer’s life. Abortion of one or more fetuses is never allowed in Judaism for the sake of the fetus. Abortion is permissible and even mandated only where the pregnancy is posing a serious danger to the mother’s health. The destruction of fetuses is usually permissible even without a health threat if it within 40 days of conception, however. Grounds for permissibility for “pregnancy reduction” must rest on the consideration that continuation of a multiple pregnancy constitutes a health risk for the mother. A3. Define nefesh; explain Rosner’s position on the use of the “pursuer” metaphor in the context of maternal-fetal relations, and his position regarding when pregnancy reduction is allowed in Jewish law. 3. Nefesh: Literally means “soul” or “person;” refers to when the person egresses from the womb or comes into the world. 4. Pursuer metaphor: Argument to abort the fetus when the fetus is endangering the mother’s life. They argue that the fetus is “pursuing” the mother and should be eliminated. a. Rosner feels this is inappropriate as the child never intended to kill the mother 5. Rosner on pregnancy reduction: a. Jewish law states that one may not sacrifice one human life to save another… but does this apply to the fetus that is not human? b. Abortion is permissible and even mandated when the pregnancy (single or multiple) poses a serious danger (physical or mental) to the mother c. Grounds for pregnancy reduction must rest on the fact that the fetus(es) pose a significant risk to the mother i. Rabbis are more lenient before the 40 days have passed, however, and since the fetuses are “mere fluid” they do not have to pose a serious risk to the mother A3. Define nefesh; explain Rosner’s position on the use of the “pursuer” metaphor in the context of maternal-fetal relations, and his position regarding when pregnancy reduction is allowed in Jewish law. Nefesh- In Hebrew, this literally means “soul”. A nefesh is considered a person with regular rights under Jewish law. Under Jewish law, the fetus is regarded as part of its mother’s body until it is born, and until forty days after conception, the zygote is “mere fluid.” So it is not a nefesh, and may be destroyed in order to save the mother’s life. The Pursuer Metaphor States that “it is one’s duty to disable or even take the life of [an] assailant to protect the life of one’s fellow man.” Some attempt to apply this logic to fetuses or babies as they are born, saying that in trying to be born, they may threaten their mother’s life. o However, the baby itself did not decide to endanger its mother’s life; this is an act of God. The child does not intend to kill the mother, so this would be a case of heavenly pursuit, and to defy heaven is to defy God and cannot be permitted. o The argument of pursuit is permissible as a weak justification for abortion when the fetus is not yet a nefesh. Once the baby is being born, however, it is considered a person and the pursuit is heavenly, so one life may not be traded for another. Pregnancy Reduction o A few documented arguments (presented, not endorsed, by Rosen): The principle of not sacrificing one life for another should not be extended to fetuses, so some can be eliminated. Contrary to above. Cannot surrender one for death to avoid all dying, because that requires choosing one to die. Siamese twins… can you separate them and let one die? Yes, because one is “chosen” to die… metaphor: two men with parachutes. One doesn’t open, so he clings to his friend’s foot. The friend may kick him off to save himself. (But this may not apply to multiple pregnancies, because one isn’t “chosen”.) If some are diseased and others are not, you cannot choose because of the disease. It is not the disease that is endangering the others, but simply their existence, which they share in common with all of the fetuses. o Is pursuit valid justification for pregnancy reduction? Can some fetuses be pursuing others, in that if all were to coexist none would survive? No. This is still heavenly pursuit, and anyway, it is unclear which fetuses are the pursuers and which are the pursued. o Abortion is never allowed for the sake of the fetus. Only for the sake of the mother. Multiple pregnancies are often associated with serious maternal complications. Ergo, it may be permissible to destroy one or more to reduce or eliminate these risks to the mother. But everything else… getting rid of fetuses because they are diseased or because they cause danger to each other, is for the sake of the fetus and cannot be allowed. o o A4. Know Callahan’s assessment of the traditional Catholic approach to abortion. Callahan: 1. God alone is the Lord of Life 2. Human beings do not have the right to take the lives of other (innocent) human beings 3. Human life begins at the moment of conception 4. Abortion, at whatever stage of development of the conceptus, is the taking of innocent human life Abortion is wrong in the eyes of the Roman Catholic position. “The only exception to this conclusion is in the case of an abortion that is the indirect result of an otherwise moral and legitimate medical procedure,” such as removing a cancerous uterus, thus satisfying the rule of double effect. A4. Know Callahan’s assessment of the traditional Catholic approach to abortion. Claim 1: God alone is the lord of life 2. Callahan is critical of the Catholic’s use of God’s lordship as a basis for determining the morality of abortion because it downplays the necessity of humans to make decisions/rules/mandates and saying that God alone is the lord of life and the source of the right to life doesn’t help people know how to deal with/respect that right Claim 2: Human don’t have the right to take the lives of other innocent humans 2. Callahan agrees with this view and recognizes two exceptions a. When the life to be taken is NOT innocent human life b. When it is innocent life but the taking of life is indirect i. Ex: removing a cancerous uterus to save directly save the mother but indirectly kill the fetus Claim 3: Human life begins at the moment of conception 2. Purpose is to provide protection to the earliest reaches of individual human life 3. The right to life is a human right and it is important to determine what qualifies an embryo or fetus as “human life” when discussing abortion to know whether or not abortion is morally allowed 4. In the Catholic perspective, the question of whether a fetus can be regarded as human life is the overarching question in whether or not abortion is allowed and in Callahan’s view, this prevents people from considering other values or asking other questions Claim 4: Abortion, at whatever stage of development of the conceptus, is the taking of innocent human life 2. Once it is determined that human life begins at conception, it is clear that abortion is the taking of human life 3. Callahan disagrees with the premises of the Catholic argument that define abortion as killing innocent life Claim 5: Double Effect 2. Abortion can only be justified when it is an indirect result of another procedure a. When an innocent life is taken indirectly, meaning by an action that is designed and intended solely to achieve some other purpose even though death is a foreseen result, then abortion is allowed b. Double Effectà The medical procedure is used to save the mother’s life with the direct intention of saving the mother and the foreseen but unintended/indirect result of the death of the fetus A4. Know Callahan’s assessment of the traditional Catholic approach to abortion. According to Callahan, life begins at the moment of conception. Abortion is taking an innocent human life, no matter what stage of development it is performed in. No abortions are permitted, except in extremely rare cases where the rule of double effect is applied. The rule of double effect is only applicable to cases of ectopic pregnancy or a cancerous uterus. As pointed out before, the RDE holds that you cannot intend the evil act, you may merely foresee it, however. A4. Know Callahan’s assessment of the traditional Catholic approach to abortion. o Overall thought: if there is life, abortion is morally wrong o Ideas this theory is based upon God alone is the Lord of life Normally, the right to life takes primacy over other rights, since without life no other rights can be exercised Human beings do not have the right to take the lives of other, innocent human beings Exceptions: o When the life to be taken is not innocent human life o When the taking of life is indirect Human life begins at the moment of conception Every unborn child must be regarded as a human person with all the rights of a human person Abortion, at whatever the stage of development of the conceptus, is the taking of innocent human life o Only exception: aborting a child as an indirect result of an otherwise moral and legitimate medical procedure o Callahan first formulates his argument by stating Catholic axioms and then refuting them. o God Alone is the Lord of Life. To use this in evaluating abortion presupposes God intervenes directly in cases of life and death, which obscures the role of free will in life. Even if you just say that God is the ultimate source of the right to life, it doesn’t address how we are supposed to respect that right or resolve conflicts with other rights. The right to life should not be the only question raised in an abortion case, but this is often what Catholic moralists do. o Human Beings Do Not Have the Right to Take the Lives of Other Innocent Human Beings. The justification for taking innocent lives has been governed by the rule of double effect (see the Crusades, etc). This is a huge loophole. Innocent lives can be taken when that action is indirect and serves to bring about a weightier positive outcome. o Human Life Begins at the Moment of Conception. This assertion comes from the Catholic wish to protect life as wholly as possible. Although they have no specific reasoning for choosing this as the beginning of life and no proof thereof, defining life as such is the safest way to do so. However, defining it as such often means that this is the only question asked. The abortion debate becomes onedimensional, hinging only on this question. The above point means that other issues are virtually ignored, when perhaps they should be more fully addressed. o Abortion, at Whatever the Stage of Development of the Conceptus, Is the Taking of Innocent Human Life. When the other premises are accepted, this one is inevitable. o Callahan then addresses the argument as a whole: Catholics often claim that justifying abortion would justify treating all human beings as expendable. This seems a ridiculous extrapolation except when you realize you have to accept abortion as taking a human life, in which case these concerns seem legitimate. o Callahan then addresses the principle of double effect (see #1 for a full discussion thereof) as perhaps a way to dispute the Catholic doctrine. The only cases in which abortion may be permissible are ectopic pregnancy and a cancerous uterus. In both, the justification is that the procedure has as its direct intention saving the mother’s life. The death of the fetus is foreseen but unintended and inevitable. Thus it doesn’t violate the principle of not killing innocent life. However, this line of logic is sometimes resented as simply going around the technical rules and disregarding the spirit of theology. “Do good and avoid evil” is not upheld when you’re just avoiding evil. Callahan says, however, that not acting in the face of the mother’s potential death is a moral choice, and when only physical life is considered, it would be irresponsible (wrong?) not to save her. A5. Describe Dresser’s 5 models for addressing conscientious objection & their strengths & weaknesses Conscientious objection: the ability to refuse an action or provide a procedure/ “treatment” if a physician believes it to be a morally objectionable decision Model 1: Contract Model 2. 3. 4. Before beginning treatment, the doctor tells the patient what they are willing to do and any treatment limits PRO: everything is up front and the patient is informed before anything begins CON: doesn’t work in emergency care when the patient needs care quickly OR when there is no other doctor to do the procedure Model 2: 2. The doctor who doesn’t want to perform the treatment MUST refer/transfer the patient to another doctor who will do the procedure 3. PRO: patient will hopefully find a new doctor 4. CON: won’t work if another doctor isn’t available AND doctors who are against a procedure may not want to recommend the patient to another doctor who will Model 3: 2. eliminates the chance of conscientious objection because when people decide to become doctors they must agree to conform to its basic standards and give up the freedom to avoid certain duties, ultimately if you decide to become a doctor, you must put your own ideas aside and assist the patient in their wishes/best interest, even if you do not agree with their decisions 3. PRO: patient gets what they want 4. CON: duties of a profession are never really clearly given and doctors could claim that they never understood/agreed to these requirements Model 4: The Draft Board Approach 2. Doctors who object to a procedure must explain/defend their opposition 3. The purpose of this model is to separate a doctor’s sincere beliefs from other less genuine motivations 4. CON: damaging to morale, good liars go undetected Model 5: 2. Advises doctors to reach a comprise between their own beliefs and the interest/desires of the patients A5. Describe Dresser’s 5 models for addressing conscientious objection & their strengths & weaknesses 1. Contract model where the professional discloses any treatment limits to the patients so that they may seek it from another professional if they so desire…but, not useful if the patient needs care quickly or there is no one else who can perform the desired treatment besides the objecting doctor 2. The objecting professional has a duty to refer or transfer patients to another professional. Can be objectionable if there is no one else to meet the patient’s need or if the professional objects to giving any assistance in obtaining the objectionable service. 3. Ruling out conscientious objection where the individual enters the profession, he or she agrees to give up the freedom to avoid certain core duties…but professionals may claim that such duties are never explicitly stated and doctors never agreed to such a contract. 4. Draft board to review objecting professionals…objectors must explain and defend their oppositions…but could be damaging to morale and cannot necessarily detect skilled liars 5. Compromise between personal beliefs and the patient’s interests…wrong to impose restrictions not supported by most professionals but also wrong for the professional to have to violate his or her moral views A5. Describe Dresser’s 5 models for addressing conscientious objection & their strengths & weaknesses Contract Model o At outset, professional discloses any limits of treatments. o If a patient requires a service that is excluded, they can then go elsewhere. o Weakness: does not work when patient needs quick care or no one else can take over and provide the service. Reference/Tranfer Model o If the professional objects and will not provide a service, they have an obligation to refer or transfer patients to another professional that will provide that service. o Weakness: fails when the contract model fails. o Weakness: some professionals will feel as if they are still committing wrong in facilitating the service. Standard Service Model o Conscientious objection is not allowed. o If you enter into a profession, you have to conform to its basic standards. Thus you must perform certain services. o Weakness: “basic standards” are hard to define, and professionals may not feel as if they have truly understood and assented to them. Draft Board Model o Requires objectors to explain and defend their opposition to performing a certain service. o Tries to separate sincere beliefs from those that have other motivations for avoiding a service. o Weakness: damaging to morale of professionals. o Weakness: cannot necessarily detect skilled liars. o Weakness: such a detection process is hard to formulate and may be corrupt. Compromise Model o o o o Professional should try to find a compromise between their beliefs and the patient’s interests. Depends in large part on the hope that other alternatives will arise that keep both professional and patient happy. Weakness: sometimes an option is not available. Weakness: compromise can leave both sides unsatisfied. A5. Describe Dresser’s 5 models for addressing conscientious objection & their strengths & weaknesses 1. The Contract Model—At the outset of the encounter, the professional should disclose to patients any treatment objections i. People in need of an excluded service may then seek that service from another professional ii. Works in some contexts iii. Doesn’t work when patients need care quickly or when no one else can take over the task of the objecting individual b. Refer/Transfer Model- the objecting professional must refer or transfer patients to another professional willing to provide the contested service i. Fails to meet patients’ interests when no one else is available ii. Model may be unacceptable to professionals who see any assistance in securing the service as complicity in immoral behavior c. Model ruling out the possibility of conscientious objection—people entering a profession agree to conform to its basic standards i. By deciding to become a particular kind of professional, the individual gives up the freedom to avoid certain core duties ii. Weakness: core duties are often not explicitly disclosed, unclear duties d. Model drawing on the military’s approach to handling conscientious objection i. Similar to a draft board—objectors must explain and defend their opposition to performing a particular medical procedure ii. Approach seeks to separate sincere beliefs from the other motivations that can underlie conscience claims iii. Weaknesses: damaging to morale, can’t detect skilled liars, the review process may be incompetent/ corrupt e. Model urging professionals to seek a compromise between personal beliefs and the patient’s interests in obtaining the disputed service i. Closer examination of the problem produces options that allow professionals to maintain their ethical integrity while meeting patients’ needs A6. List and explain Rhoden’s arguments regarding non-consensual Cesarean sections and her assessment of interpersonal risk-benefit comparisons. Question: Should courts have the power to authorize doctors to perform C-sections deliveries against the woman’s will? Rhoden is arguing that the courts should NOT order competent women to have Cesarean deliveries, even if other options (such as vaginal delivery) pose harm to the fetus for 3 primary reasons… 2. Performing a C-section against the woman’s will is an intrusion on the pregnant woman 3. It undermines the concept of “informed consent” which state that only the person that is subjected to a procedure can assess its risks and benefits 4. The action is a slippery slope that can lead to the seizure of more choices that women have during pregnancy Argument 1: Roe vs. Wade 2. Court-ordered C-sections go against the Roe v. Wade decision b/c it states that even after the fetus is viable, the woman’s life and health still come first so doctors shouldn’t force a C-section on a woman just to benefit the fetus b/c the woman’s life/interests come first Argument 2: Colautti vs. Franklin 2. This supreme court decision once again places the interests of the woman before the fetus 3. It states that doctors who are performing post-viability abortion MUST use the technique that is least harmful to the fetus UNLESS another technique is necessary for the woman’s health 4. It is NOT allowed for abortions after viability to be done using a procedure that is safest for the fetus b/c this technique is less safe for the woman Argument 3: Child Neglect/Fetal Neglect Analogy 2. Some people argue that the woman is neglecting the fetus because just as parent cannot deny care to their child, neither can a pregnant woman dent care to a fetus that is fully formed/viable a. This is a weak argument because “fetal neglect” implies legally enforceable duties and not until now in the present day have woman been expected to perform such duties b. The analogy is flawed because in terms of child neglect, the child can be treated on its own but in fetal neglect, the fetus cannot be treated without invading the woman Argument 4: Except in extreme cases, a C-section benefits the fetus not the woman and typically places the woman at greater risk for medical complications 2. Therefore, how can it be okay for the state to ignore the request of the woman to NOT have a C-section and impose a risk on the woman in able to preserve the life of the fetus Interpersonal Risk-Benefit Comparisons 2. All nonconsensual risks imposed on one person to save another are equally illegitimate 3. In decisions ordering C-sections, courts find that the potential harm to the fetus overrides the woman’s right to privacy/autonomy/bodily integrity and justifies imposing a physical harm on the woman 4. a. “the probably severe harm to X warrants imposing a lesser physical harm on Y” Courts cannot truly assess the potential risks they are placing on the pregnant woman because… a. The inability to assess statistical statements of risk b. The court doesn’t know the exact risk it is planning to impose on the woman c. Different circumstances yield different results d. A judge cannot know the woman’s subjective response to the possible risks A6. List and explain Rhoden’s arguments regarding non-consensual Cesarean sections and her assessment of interpersonal risk-benefit comparisons. 1. They impose an unparalleled intrusion upon pregnant women à just because the state has an interest in ensuring the health of the child does not mean that they can take any and all actions to prevent its harm…a woman’s life and health come first 2. They undermine the teachings of informed consent doctrine that only the individual being subjected to the procedure can assess its risks and benefits à the mother’s health is threatened by surgical delivery 3. They contain within them the seeds of widespread and pernicious usurpation of women’s choices during obstetrical care à doesn’t respect her autonomy, treats her as a “fetal container” Probable severe harm to X warrants imposing lesser physical harm on Y o People should be able to make their own decisions even if they’re harmful o Treats the woman as a vehicle for rescuing and imperiled fetus not as an end in herself o Authorizes an act of violence against the woman A6. List and explain Rhoden’s arguments regarding non-consensual Cesarean sections and her assessment of interpersonal risk-benefit comparisons. 1) Court ordered Cesareans impose an unparalleled intrusion upon pregnant women 2) Court ordered Cesareans undermine the teachings of the informed consent doctrine that only the individual being subjected to a procedure can assess its risk and benefits 3) They contain within them the seeds of widespread and pernicious usurpation of women's choices during obstetrical care 4) Proponents point to the Roe decision as justification to protect a fetus once it is capable of independent life outside the womb, but just because the state has an interest in preventing certain consequences doesn't mean that taking any and all action is constitutional, as there is a big jump in logic between prohibiting destruction and requiring surgical preservation 5) Supreme Court precedents have dictated that a state could not require a woman to undertake a more dangerous procedure in the interest of a child, and maternal death is 4 times higher with Cesarean sections than vaginal delivery 6) The claim that fetal neglect is legally parallel to child neglect is wrong because children can be treated in opposition to parental demands, but fetal care necessitates restraining and invading the woman as if she were simply a fetal container 7) Cesareans benefit the fetus and increase risk for the woman, and there is no other such case where the state can override treatment refusal and impose a risk upon one person in order to preserve the life of another. It is illegal and immoral to force a parent to donate a kidney to a child to save their life. 8) Interpersonal risk-benefit comparison says that if courts can order Cesareans, then the potential harm to the fetus overrides the woman's rights to privacy, autonomy, and bodily integrity; ordering harm upon one person for the lesser harm of another requires a third party to make this assessment about the utility of two bodies, and such an act has never had a place in US law 9) "while cowardice may not be admired, it is too human a quality to be formally punished by law." 10) The ability of a court, as a third party bystander, to truly understand the situation is radically limited 11) In ordering surgery, the court is thus rendering objective a determination that cannot rightfully be anything but subjective 12) All these cases assume that the physicians' predictions of harm to the infant are correct, when in reality, diagnostic technologies are only so good and would lead to unneeded surgery ordered, meaning unneeded risk enforced by a court to the woman A6. List and explain Rhoden’s arguments regarding non-consensual Cesarean sections and her assessment of interpersonal risk-benefit comparisons. Overall topic of article: She courts have the power to authorize doctors to perform Cesarean deliveries against the woman’s will? (C-section vs natural birth—each have risks) Rhoden argues that courts should not order competent women to have C-sections Abortion law—ex- Roe v. Wade Women can choose whether or not to even continue with pregnancy to a certain point State can prohibit intentional fetal destruction, but this doesn’t necessarily mean that it can go even farther by mandating major surgery to protect and preserve the fetus’ life Major difference between prohibiting destruction of a fetus and requiring surgical preservation Court-ordered C-sections violate Roe’s constitutional plan (that once the fetus is viable, the woman’s life and health come first) – surgery threatens woman’s life Child neglect/ Fetal neglect analogy Women don’t have legally enforceable duties to fetuses Child is inside woman. Women’s rights come first Women are more than just “fetal containers”—people often overlook this Should approach the issue by asking if the woman’s privacy can be violated The State’s interests in the well-being of third parties Patients’ privacy rights trump the state’s interests Parenthood should not obliterate personal autonomy There is no duty to undertake risky rescues in our country Parents have a duty to rescue their children, but they have no duty to rescue them by ricking their own life or health Interpersonal Risk-Benefit Comparisons All nonconsensual risks imposed on one person to save another are equally illegitimate Emotional responses should be regarded The most significant feature of decisions ordering C-sections is that the court finds out that the potential harm to the fetus overrides the woman’s rights to privacy, autonomy, and bodily integrity, and justifies imposing a physical harm upon her Which consequences are heavier? Cowardice may deter people from wanting to have a Cesarean Court can compare risks of the woman to benefits of the fetus (limited understanding—decisions cannot be rendered objective) In ordering surgery, court is rendering objective a determination that cannot rightfully be anything but subjective (denies the woman’s uniqueness and individuality) Although the chances of maternal injury are low, the moral risk is high, and this possibility should make courts thing twice before mandating surgery A7. Explain Annas’ perspective on fetal neglect laws. Annas says it is morally unacceptable to treat a pregnant woman as a fetal container while valuing the life of her fetus as more significant than hers…medical advice should remain advice not law and should not require the pregnant woman to give up her basic rights of bodily integrity and privacy A7. Explain Annas’ perspective on fetal neglect laws. 7. Main point of view:: laws on fetal neglect laws are hypocritical and silly 8. Medical advice is still advice and dangerous because it has such a vague meaning 9. Monitoring compliance would require confining pregnant women to an environment in which eating, exercise, drug use, and sexual intercourse could be controlled 10. Many quandaries arise if child neglect statutes are applied to fetuses a. Unlike a child, a fetus is absolutely dependent on its mom and can’t be treated without invading the mother b. Treating fetus and mom separately before birth can only be done by favoring one over the other c. Favoring the fetus means devaluing the mom and treats her like an inert incubator, or a culture medium for the fetus d. Thus, women are viewed as unequal citizens, since only them can bear children, and relegates them to performing 1 main func:: childbearing e. It is unfair to assume that the fetus’s interests are in opposition to its mom, and to require the mom to be the fetus’s servant f. If women must “consent” to such “care” of their fetuses, they are relegated to the role of containers g. Attempts to define fetal neglect, and to establish a prenatal police force to protect fetuses from their mothers, are steps backwards in terms of both women’s rights and fetal protection 11. The best chance the state has to protect fetuses is through actions to enhance the status of all women by fostering reasonable pay for the work they do and equal employment opportunities A7. Explain Annas’ perspective on fetal neglect laws. 'fetal neglect' laws would lawfully require a woman to live for her fetus, legally required to stay off her feet, eat unhealthy foods, smokes, drinks, or has intercourse Such laws change it so that the doctors' patients are the fetuses, and not the mothers Laws suggest that medical advice becomes laws that are grounds for criminal action, which is silly and dangerous, as physicians are neither lawmakers nor seers After the fact prosecutions wouldn't help the individual fetuses Such laws are dangerous because medical advice is a vague term that can cover almost anything, and to effectively monitor this would require confining pregnant women to a controlled, supervised environment, reducing women to simply fetal containers whose only job is to have the healthiest baby we can make them have Treating mothers and fetuses as two spate individuals with separate rights would require favoring one over the other in disputes, and favoring the fetus radically devalues the woman Child neglect laws cover don't require parents to provide optimal clothing, food, housing etc. and don't forbid taking risks with children, but fetal neglect laws do Some claim that when women get pregnant, they waive their right to abortion and take on obligations to the future child; this is flawed because such a 'waiver' never takes place and it is a woman's constitutional right to terminate the pregnancy; also if women have a right to bear children and there are no restrictions on a decision to have an abortion, but fetal neglect laws would say that a woman who elects childbirth surrenders her basic rights of bodily integrity and privacy, which is in effect a state-erected penalty on her exercise of the right to bear a child Fetal neglect laws would be a step backwards in women's rights and fetal protection A7. Explain Annas’ perspective on fetal neglect laws. The best chance the state has to protest fetuses is through actions to enhance the status of all women by fostering reasonable pay for the work they do and equal employment opportunities, and providing a reasonable social safety net, quality prenatal series, and day care programs Best way to protect fetuses—state should improve the welfare of pregnant women (helping to prevent child neglect) A8. Describe Asch’s position on the acceptability of abortion and prenatal genetic diagnosis. Asch believes that women’s rights to full social and sexual equality with men are compromised without the option of abortion because their bodily integrity is violated by involuntary pregnancy. Pregnancy compromises a woman’s opportunity for equality and is a form of involuntary servitude so abortion is acceptable. Asch disagrees with selective abortion because sex selection and selection against disabilities sends the wrong message to actual boys and girl and disabled children about their worth. It is differentiated from other abortions where women do not consent to carrying a child in the first place, but once a woman consents to carrying that child, Asch believes that she cannot abort it if she finds something about it that she doesn’t like. A8. Describe Asch’s position on the acceptability of abortion and prenatal genetic diagnosis. 7. Feminist case can be summarized:: a. Women have a substantial right to bodily integrity that is violated by involuntary pregnancy; as long as a fetus resides in within her body, a woman may decide about whether she wishes her body to be used to support new life b. Women have a right to autonomy and choice in matters of responsibility c. The value of fetal life is contingent upon the decision of the woman in whose body it resides d. Women should not feel compelled to create new life e. Women’s rights to full social and sexual equality with men are compromised w/o the option of abortion 8. Until a foolproof method of birth control exists, and as long as the only way for human life to develop is within women’s bodies, women need the option of abortion in order to avoid being fettered by biology 9. Birth control and abortion offer women the opportunity to separate sexuality from parenthood, and thus enable us to undertake parenthood only when we feel it makes sense for our lives 10. Pregnancy can impose financial, psychological, vocational, and social hardships; to require women to undertake these hardships constitutes a form of involuntary servitude 11. A chance pregnancy punishes a woman for sexuality in a way that men escape and threatens their equality in all spheres 12. Involuntariness of a pregnancy is a sufficient criterion to justify an abortion 13. Pregnancy is itself so complex that any moral or social order compelling women to undertake it unwillingly violates any claim to promoting their full social and sexual equality with men 14. People with disabilities have grown up in an unwelcoming society that often failed to provide them and their families with the financial support, social services, and educational opportunities needed to maximize their potential 15. Many people who themselves use prenatal diagnosis also support disability rights but argue that the world is too unwelcoming toward disabled people for them to want to see their own child live through what is waiting 16. Many people say they can’t face being parents of a child with serious problems that will cause them pain, grief, frustration, disruption of other life commitments, or hardships to siblings or other family members 17. The woman who aborts a fetus diagnosed as having spina bifida is sparing her child and herself untold misery that reaps only pain and no reward 18. The woman who aborts for reasons of disability may be signaling an unwillingness or incapacity to recognize that not everything in life can be controlled and that parenthood is one of those things we should not undertake unless we are willing to face what we cannot control and to seek the resources in ourselves and the world to master it 19. Should we really allow people who are not capable of raising a child, especially one with disabilities, to raise one? A8. Describe Asch’s position on the acceptability of abortion and prenatal genetic diagnosis. The feminist argument uses the following tenants; 1) women have a substantial right to bodily integrity that is violated by involuntary pregnancy, so she has the right to decide about whether she wishes her body to be used to support a new life, 2) women have a right to autonomy and choice in matters of responsibility, 3) the value of fetal life is contingent upon the decision of the woman in whose body it resides, 4) women should not feel compelled to create new life, 5) women's rights to full social and sexual equality with men are compromised without the option of abortion · If women are to be equal in life, especially sexually, they must feel their bodies and lives will not be altered by involuntary pregnancy; so until a 100% foolproof birth control exists, abortion must be allowed in order for women to separate sexuality from parenthood as men are able to do · Those who don't favor abortion because of adoption overlook the compromises and sacrifices the process of pregnancy itself imposes on women's equality, as pregnancy imposes financial, psychological, vocational, and social hardships · When dealing with planned, but later become unwanted, pregnancies, women should still be able to caringly and responsibly decide about the circumstances of her own life that no longer enable her to be the parent she wishes to be · Asch condemns selective abortion for sex selection because that sends the message that gender alone is reason enough to make life-death decisions about one's value · The same argument applies for disabilities, excluding those that result in protracted physical pain or death in infancy or early childhood, as people with disabilities such as Down's syndrome are able to interact with people, learn skills, and live as adults, so selective abortion to prevent Down's syndrome would send the message that all people with Down's syndrome born, because of faulty prenatal diagnosis or were born before the technologies existed, aren't as valuable to society and if we had it the way we wanted wouldn't be here · Selective abortion differs from the decision to end a pregnancy because one's adult life has radically changed because selective abortion assigns value to potential life we dislike as opposed to a decision regarding a woman's own life and ability to carry a baby and raise a child A8. Describe Asch’s position on the acceptability of abortion and prenatal genetic diagnosis. Abortion is allowed if the situation is not right to raise a child A chance pregnancy punishes women for sexuality in a way that men escape, and threatens their equality in all spheres Abortion is not ok if a woman is not happy with the child’s gender, health issues, etc. Ex- terminating a once-wanted pregnancy (selective abortion) A9. Analyze the holding and rationale of Roe v. Wade and the changes brought about by the Casey decision. Roe v Wade intends to protect the right of personal privacy and respect the rights and autonomy of the mother in making decisions regarding her own body. However the Casey decision gives the State the freedom to take steps to ensure that the woman makes an informed and thoughtful decision. Rules and regulations may be enacted to encourage her to carry the fetus to term. A9. Analyze the holding and rationale of Roe v. Wade and the changes brought about by the Casey decision. 7. ROE v. WADE a. It has been argued that abortion laws were the product of a Victorian social concern to discourage illicit sexual conduct b. 2nd reason is concerned with abortion as a medical procedure, thus a state’s real concern in enacting a criminal abortion law was to protect the pregnant woman, that is, to restrain her from submitting to a procedure that placed her life in serious jeopardy c. Abortion in early pregnancy is now relatively safe d. The right of privacy is broad enough to encompass a woman’s decision whether or not to terminate her pregnancy e. Appellants and some amici argue that the woman’s right is absolute and that she is entitled to terminate her pregnancy at whatever time, in whatever way, and for whatever reason she alone chooses f. Most of these courts have agreed that the right of privacy, however based, is broad enough to cover the abortion decision; that the right, nonetheless, is not absolute and is subject to some limitations g. There has always been strong support for the view that life does not begin until live birth h. A state criminal abortion statue of the current TX type, that excepts from criminality only a life saving procedure on behalf of the mother, without regard to pregnancy stage and without recognition of the other interests involved, is violative of the Due Process Clause of the 14th Amendment 8. CHANGES BROUGHT ABOUT BY THE CASEY DECISION a. The Roe v. Wade position was overturned; it is recognized as sui generis, different in kind from the others that the Court has protected under the rubric of personal or family privacy and autonomy b. Instead of claiming that Roe was correct as a matter of original constitutional interpretation, the opinion therefore contains and elaborate discussion of stare decisis c. Thus, authentic principles of stare decisis don’t require that any portion of the reasoning in Roe be kept intact d. The end result of the joint opinion’s paeans of praise for legitimacy is the enunciation of a brand new standard for evaluating state regulation of a woman’s right to abortion—the “undue burden” standard e. Reduced Roe to a dead letter A9. Analyze the holding and rationale of Roe v. Wade and the changes brought about by the Casey decision. Roe v. Wade Decision: -the historical reasons behind criminal abortion laws are not valid, they are 1) abortion laws were to discourage illicit sexual conduct, but this doesn't come into play in present case and no court would take that argument seriously 2) concern about the safety of abortion as a medical procedure, but today the techniques are advanced enough that early pregnancy abortions have a maternal mortality rate equal or less than delivery rate 3) the state's interest in protecting prenatal life, the reason that is most often used and most contested -when the court looks at legislative history, it finds that most state abortion laws were strictly to protect the women, and the issue of protecting prenatal life was never a concern -in previous decisions, the court has recognized that a right of personal privacy does exist under the constitution -some would argue that the woman's right is absolute and is entitled to terminate pregnancy at whatever time she wants for whatever reason, but the court disagrees, they assert that a state may properly assert important interests in safeguarding health, medical standards, and potential life, but at some point in pregnancy, these respective interests become sufficiently compelling to sustain regulation of abortion -pro-life advocates would life to argue the fetus is a person within language and meaning of 14th amendment, and if this were the case then the fetus's right to life would certainly be guaranteed, but previous decisions regarding abortion (such as United States v. Vuitch) upheld some instances of abortion and thus inherently did not see the fetus as a person protected fully by the 14th amendment -since experts in medicine, philosophy, and theology don't have any consensus about when life begins, the Court is in no position to make such judgment, and doesn't claim to do so, but it does note the wide divergence of thinking and that there has always been strong support for the view that life does not begin until live birth -many who have taken a formal position on the abortion issue have generally regarded it as a matter for the conscience of the individual and her family -physicians and scientists tend to focus upon conception, live birth, or the point at which the fetus becomes 'viable' outside of the womb -in areas other than criminal abortion law, the unborn have never been recognized in the law as persons in the full sense, so it doesn't make sense to do so in this once -considering everything, the court finds no reason that because of one theory of life, Texas may override the rights of the pregnant women that are at stake -the court does have an interest in preserving the health of the pregnant woman and the potential human life, but they are separate and each grows substantially as the pregnancy advances -the court finds the end of the first trimester to be when the fetus's health becomes compelling, as that is when a fetus would be viable outside of the womb -state regulation protective of fetal life after viability has both logical and biological justifications; if the state is interested in protecting life after viability than it may go so far as to proscribe abortion, except when health of the mother is a concern -Roe decision leaves the state free to place increasing regulations on abortion as the period of pregnancy lengthens, so long as those restrictions are tailored to the recognized state interests The Casey decision -the Supreme Court upheld provisions that said women seeking abortions must receive counseling on alternatives, wait 24 hours, minors must get a parent or judge permission, no abortions after 24 weeks except for medical reasons, and doctors need to keep detailed records; Supreme Court struck down provision that married women must notify their husbands -decision claimed that it was their "obligation to define liberty for all not to mandate our own moral code -though the woman has a right to choose to terminate or continue her pregnancy before viability, it does not at all follow that the State is prohibited from taking steps to ensure that this choice is thoughtful and informed -this decision says the states aren't allowed to have regulations that have the purpose and effect of placing a substantial obstacle in the path of a woman seeking an abortion for a nonviable fetus, but allows regulations that do no more than create a structural mechanism by which the State may express profound respect for the life of the unborn; so waiting 24 hours and giving counseling are allowed since they do not stop a woman from getting an abortion but allow for good decision making A9. Analyze the holding and rationale of Roe v. Wade and the changes brought about by the Casey decision. 1. The original Roe v. Wade case established abortion, or the woman’s right to choose, as a fundamental right protected in the 14th Amendment. a. The decision also set out a rigid standard of no state interference during the first trimester, yet acknowledged a state interest in protecting the life of the fetus after the first trimester as long as the health and the life of the mother were protected. b. This decision divided the nation even further than before. 2. In 1992, there was a lesser known case about the same issue: Planned Parenthood of Southern Pennsylvania v. Casey. a. In this case, five provision of the Pennsylvania Abortion Control Act were being challenged: i. Informed Consent ii. Spousal Notification iii. Parental Consent iv. 24-hour waiting period before obtaining an abortion v. Reporting Requirements of facilities providing abortion services b. The court decided to uphold the 3 essential parts of Roe: i. A woman’s right to choose an abortion ii. A confirmation of the state’s power to restrict abortion after viability iii. The State has a legitimate interest in the health of the mother and the life of the fetus at the outset of the pregnancy. c. Casey dropped those requirements that were too much of an obstacle to abortion, as they would then be considered unconstitutional. 3. Casey, while affirming Roe, actually weakened it. It now allows for more state regulation during the entire pregnancy and lowers the standard of review for other abortion statutes. A10. How would different ethical principles apply to the above discussions? 7. Theological premise -- God's sovereignty as giver of human life. 8. Moral principle -- it is morally wrong (i.e., murder) directly to take the life of an innocent human being. 9. Factual premise -- human life begins at the moment of conception. 10. Rational-deductive method leading to conclusion: abortion is morally wrong. 11. Possible ways to avoid conclusion: a. Show that fetus is not human, that the fetus is not innocent, or that fetal death is indirect rather than direct. 12. Is abortion killing the fetus or withdrawing bodily life support from the fetus? 13. Under what circumstances and how far is the pregnant woman obligated to provide bodily life support to the fetus? 14. Analogical reasoning and the feminist suspicions -- compare and contrast the provision of bodily life support in other settings, such as organ donation. 15. Debates about actual reasons and about morally acceptable reasons for abortions a. Protection of maternal life and health b. Abortion following rape and incest c. Abortion for the fetus' own sake in the case of severe genetic anomalies d. Multi-fetal pregnancy: Selective reduction of pregnancy? e. Interests of others, including father (i.e., impregnator) f. Other reasons 16. Societal laws, policies, and conflicts a. Moral rhetoric in the abortion debate -- is it possible to find a “common” or “middle” ground? b. Supreme Court cases and state laws: where abortion now stands. i. Problems with the framework of Roe v. Wade ii. The significance of the Casey decision iii. Developments in the states iv. Political and legal, as well as moral, debates about so-called “partial-birth abortions” (Gonzales v. Carhart decision in 2007) 17. Debates about maternal-fetal relations and conflicts a. Major types of conflicts i. Charges of prenatal child abuse for use during pregnancy of illicit drugs, etc ii. Recommendations of fetal therapy, including surgery iii. Court-ordered cesarean deliveries b. Ethical issues in maternal-fetal conflicts i. Extent of beneficence-based actions that can be morally required of pregnant women -- balancing risks, degree of intrusiveness, etc. “Good Samaritanism.” ii. Pregnant woman's autonomy and privacy: Does the pregnant woman's decision not to abort morally reduce her freedom and increase her obligation to the fetus? iii. Comparability of pregnant women's obligations and other parental (including paternal) obligations to children -issues of justice and fairness. iv. Should moral obligations to the fetus be enforced as legal obligations? 1. Further issues of autonomy and privacy in legal enforcement 2. Further issues of justice in legally requiring more of pregnant women than of others in the society and in imposing burdens on vulnerable women (e.g., poor women) 3. Medical uncertainties 4. Which strategies are likely to reduce harm to fetuses? c. Debate about testing pregnant women for HIV infection and treating them with anti-retroviral drugs to reduce the risk of transmission of HIV infection to their offspring A10. How would different ethical principles apply to the above discussions? -the rule of double effect is often invoked with regards to abortion, where some take the stance that abortion is ok to save a woman's health as long as the death is not the intended effect, but merely the foreseen effect; for example a cancerous uterus can be removed with the intended effect of preventing death in the woman from cancer, though death of the fetus is indirect, but foreseen, consequence; this view holds that cases such as a fetal craniotomy, in which crushing of the fetus's skull is the intended effect as a means to save the woman, are immoral -for the rule of double effect to be valid, 1) the action in itself must be good or at least indifferent, 2) the agent must only intend the good effect and not the evil, though foreseen, effect, 3) the evil effect cannot be a means to the good effect, and 4) there must be proportionality between the good and evil effects -many invoke the principles of beneficence and nonmaleficence or justice as cause for abortion being immoral, but that all depends on the view of when a fetus becomes a life or potential life to be protected by these principles -different phrasing causes different views, as some see abortion as killing the fetus while others see it as withdrawing bodily life support A10. How would different ethical principles apply to the above discussions? 4. Extent of beneficence –based actions that can be morally required of pregnant women – balancing risks, degree of intrusiveness, etc. a. Being a “Good Samaritan” 5. Pregnant woman’s autonomy and privacy: does the pregnant woman’s decision not to abort morally reduce her freedom and increase her obligation to the fetus? 6. Comparability of pregnant woman’s obligation s and other parental (including paternal) obligations to children – issues of justice and fairness 7. Should moral obligations to the fetus be enforced as legal obligations? a. Further issues of autonomy and privacy in legal enforcement b. Further issues of justice in legally requiring more of pregnant women than others in the society and in imposing burdens on vulnerable women (i.e., poor women) c. Medical uncertainties d. Which strategies are likely to reduce harm to fetuses? B1. Describe the views of family and of religion in BNW. Family and religion are seen as unnecessary in BNW. Such attachments pose a threat to the stability of the state because emotional attachments cause unpredictability and complications that are unnecessary. The state advocates simply using soma and other people without any commitment because religion and familial relationships create too much passion and endanger stability. B1. Describe the views of family and of religion in BNW. The concept of “family” is basically nonexistent in BNW because its establishment would be a threat to World State’s motto of Community, Identity, and Stability. In a world that denounces individual freedom, women do not even have the right to reproduce freely. Rather, every citizen of the World State is genetically created, destined to work in one of five different castes. However, citizens do have the right in the pursuit of happiness, which can be achieved by engaging in sexual pleasures with whoever he or she desires. This promiscuous environment would also create an unstable society for families to exist in. In the BNW, there is no such thing as marriage, monogamy, or family. The words “mother” and “father” are even considered extremely offensive. Technology can be seen as religion. The world revolves around their advanced genetic reproductive technologies, and they are fascinated with the creation of Henry Ford’s Model T. Just like we date time according to the death of Christ (A.D.), the people of BNW, refer to time based on Ford’s death (A.F.). Christ is paralleled with Henry Ford. The Director could be compared to God. He controls which castes each baby is born into and the characteristics (how strong, smart, etc) the person is. Everyone accepts their role in life, never second guessing the Directors decisions. B1. Describe the views of family and of religion in BNW. 1. Family a. Absence of the family in order to create a utopian society where happiness is not dependent on other beings, but can be achieved through materials such as soma b. BNW is filled with references to sex, yet sex and sexual reproduction is controlled by the government. i. The World State’s control of the population comes from its control over sexual desire and reproductive rights. ii. Reproductive rights are controlled through a system that sterilizes two-thirds of the women, requires the rest to use contraceptives, and removes ovaries when it needs to produce new human beings. iii. Sexual desire is controlled by social rewards for promiscuity and lack of commitment. c. The idea of having a mother or a father is laughable by the population of the World State > John, the outsider, does not understand the absence of family d. The World State does not want people to depend on one another for their happiness, thus, families cannot be prevalent in a successful utopian society. 2. Religion a. In the novel, human beings are taking on the work of God by creating humans and controlling their lives. b. Use of “our Ford” as a replacement to God c. Different religious positions: (to human reproductive cloning) i. Roman Catholicism: strong opposition ii. Protestantism: various positions, mostly opposed iii. Orthodox and Conservative Jewish rabbis: approval in some scenarios iv. Important point: child created by cloning would still be created in God’s image: child’s dignity violated but not diminished B2. Explain the function of soma and the image of Ford in BNW. 1. Soma is an example of a technology in BNW that provides for the World State’s consistent stability. This is due to the constant happiness that this type of drug creates for those people who consume it. a. Soma symbolizes the use of instant gratification to control the World State’s population b. It also symbolizes the powerful influence of science and technology on society c. As a kind of “sacrament”, it represents the use of religion to control society 2. The citizens of the World State substitute the name Henry Ford for God a. This displays how religion has been replaced with technology b. Shakespeare provides a contrast in that it represents the time “before Ford.” i. Shakespeare’s plays provide examples of emotional human relationship that the World State wants to eliminate. c. In stated of the “sign of the cross” they use a signal for Ford, again allowing for the image of Ford to replace all religions. B2. Explain the function of soma and the image of Ford in BNW. Function of soma: o Soma is a drug used to control the population of BNW o Whenever anyone experiences anything unpleasant, they take soma as a way of avoiding or escaping their troubles o Soma allows people to never experiences pain or suffering o because people can so easily escape pain/suffering without consequences, soma is a central part of BNW- it replaces methods formerly used to deal with issues (such as religion, alcohol, emotional connections with others, etc.) Image of Ford: o Replaces religion in the BNW- demonstrates how the society has eliminated emotional connections o Ford is worshiped in the same way God was: There are services involving soma and rhymes that replace church services People “cross” themselves but in references to Ford’s T rather than the cross that Jesus was crucified on Tops of crosses are cut off to make Ts o Used as a frame of reference for time (years After Ford = A.F.) o Technology has replaced religion: rather than looking to God, they look to Henry Ford because of the technology that he produced- society strives for similar efficiency B2. Explain the function of soma and the image of Ford in BNW. The Function of Somna - Taken by the characters in the book to feel nothing but happiness. “And do remember that a gramme is better than a damn.” -“that second dose of somna had raised a quite impenetrable wall between the actual universe and their minds” -Hug me, honey, snuggly bunny, Loves as good as somna.” -Somna shows that the people do not believe they can have truth and happiness. They have chosen to sacrifice truth for happiness. -Somna actually shortens life by years if taken excessively (society encourages its excessive use.)Yet it is believed by the doctor life is actually lengthened because the people are not suffering and so happy when taking somna. B2. Explain the function of soma and the image of Ford in BNW. A society can be stable when all of its citizens are happy. The drug, soma, can help create the World State’s ideal environment. Soma allows its users to escape all negative emotions and receive instant gratification. In a world where everyone is happy and satisfied with life, there is no need to rebel and create unnecessary problems. The image of Ford is parallel to Christ in Christianity. Faith is Christ has been replaced by Faith in Ford. Time is based on Ford’s death – all dates are preceded by A.F. (After Ford). There is a fascination with the development of Ford’s Model T car. He started the whole technology movement, which is central in BNW. B3. Discuss the relationship of technology and culture in BNW. In a Brave New World, technology is central. No one except the Controller fully understands more than a small part of the technology that actually rules all parts of BNW Use of technology to control BNW actually eliminates all emotions and culture in BNW. Individuals are eliminated and people are conditioned to act in certain ways so they fall into the correct group that they were selected to be part of. In addition, because technology is worshipped in BNW, anything that is “old” is eliminated and forbidden, including great books (Shakespeare, etc.), works of art, religion, languages, and other cultural traditions. The conditioning performed on each person in the BNW prevents him/her from appreciating or understanding the older culture because crucial elements such as family, mother/father relationships, and emotional connections are not in existence in BNW. Furthermore, in order to encourage use of new technologies and advancements, the controllers do not want people to have access to anything “old.” Instead, they focus carefully on only “new.” B3. Discuss the relationship of technology and culture in BNW. Technology is culture. Technology rules all citizens’ everyday lives, even down to the type of movies they watch. For example, citizens of the World State watch “Feelies,” which allow the watchers to experience good feelings that during the movie. These shows usually involve sexual situations, which bring happiness and pleasure to the watchers as well. The advanced genetic engineering technology determines what kind of life each person will lead. Each person is born into certain castes, which also determines their level of intelligence and strength. B3. Discuss the relationship of technology and culture in BNW. Ford is viewed like a god, the characters use expressions like “Thank Ford!” “Year of our Ford” “my Ford” Crosses have been turned into Ts. -The name Ford refers to Henry Ford the founder of the Ford Motor company and the maker of the model T. -Instead of respect for religion the society only has respect for technology which consumes their life a. b. c. d. e. In the novel, technology is used in order to control society. BNW demonstrates the dangers of giving the state control over technologies, and what type of culture would result from this. For example, the control of reproduction through technological and medical intervention i. The surgical removal of ovaries and all types of conditioning are controlled by the government Entertainment machines were created that generate harmless leisure along with high levels of consumption and production to provide the World State’s stability. The State uses technology to create a happy, superficial world through things such as “feelies.” ii. However, the State censors and limits technology, as it does not allow others to search for the truth – a fundamental part of science. C1. Explain Lauritzen’s feminist critique of reproductive technologies. Lauritzen, himself, experienced difficulties with infertility. He and his wife decided to hold off on having children until they had established their careers, never expecting/planning on having these difficulties. He presents 4 arguments about NRTs i. The Tyranny of Technology. 2 types of coercion 1. coercive offers advocates of NRT claim that these techniques were created to help infertile couples, expanding the range of choices open to them. Feminist argument: choice to participate in NRTs is illusory. Society and culture defines a woman’s identity in terms of motherhood. So developing NRTs is not about increasing choice because they are not available to single women (infertile or not) or lesbian women. 2. coercive threats the potential for a loss of control over one’s reproductive destiny is increased with the development of NRTs. Ultrasounds, amniocentesis, genetic testing, C-sections all have increased the medical community’s control over the process of birth. If trying to increase choice and decrease infertile women’s suffering, then doctors would put more effort in educated all women on causes of infertility. Also, NRTs would be open to single and lesbian women. The existence of infertility treatments leads people to view infertility as an individual problem, but in reality, the couple, together, suffers from infertility. ii. Dismemberment of Motherhood NRTs question the meaning of motherhood The maternal experience might become a discontinuous process The intimacy of pregnancy, labor, and childbirth is absent, which may lead to a loss of connection between the mother and child. Alienate women from the process of procreation, which removes an experience important for women’s identity and power. Importance of genetic and social parenthood is at stake Lauritzen believes that there should be a unity between genetic, gestational, and social parenthood. iii. The Commodification of Reproduction NRTs treat human beings as products Divides person into parts; also divides motherhood. NRT process does not treat the whole patient, just parts Like “living laboratories” à some women were not fully informed of experimental nature of procedures Children would be treated as products à women pay for embryos or eggs Because children would be considered property, then can demand for certain standards or else demand compensation or return the product. Lauritzen’s experience: difficult to maintain intimacy in clinic environment designed to achieve results. Procreation is separated from sexual intercourse. This would lead to sex being viewed as simply the production of an object. iv. Reproductive Technologies and Genetic Engineering General acceptance of NRTs is an inevitable route to widespread use of genetic engineering. Once the embryo is treated as a product that can be bought and sold, there will be pressure to create the perfect product. If genetic abnormalities can be detected and/or treated, much human suffering might either be avoided or alleviated. But this raises questions how we should distinguish attempts to alleviate suffering and attempts at eugenics? Increase in effort to create the perfect child. But who decides what is perfect? NRT techniques involves placing an extraordinary amount of control in the hands of the doctor, who for example, picks one sperm out of a million to inseminate the egg. A majority of the medical field are male. Thus, NRTs put power in the males’ hands. Lauritzen does not believe that this is a problem. His doctors are not acting in bad faith in developing new reproductive technologies. There is no conspiracy to gain control of the process of reproduction, but there is an increase in control C1. Explain Lauritzen’s feminist critique of reproductive technologies. If new reproductive technologies (NTRs) are not regulated- children will become products, women breeders, men will gain more control than ever A balance of rules and abstract principles with individual situations – necessary to understand both moral decisions and compassionate actions in moral situations Individuals should resort to NTRs only after extensive soul searching; society should resist expansion of NTRs—NTRs should remain only a last resort Issues: o Loss of intimacy in sex life o Existence/availability of technologies = coercive offer/threatens women’s future reproductive choices Choice to use technologies is an illusion because society defines woman’s identity by motherhood Women who agree to participate in IVF programs are not always free not to participate Not available to single or lesbian women – only increase choice of women who are married Future- what was originally an optional technology could become the norm Once technology of control (such as NTRs) exist, it is nearly impossible to not make us of them; societal expectation that the technology will be used simply because it exists o Dismemberment of motherhood: NTRs create three different mothers- genetic mother, gestational mother, social mother Also gives men power to reproduce in a way Confuses family relationships o Commodification of reproduction: treat human beings as products Language of reproductive medicine can be dehumanizing (eggs are harvested, etc.) Women are objectified Buyers can place demands on eggs, etc., children will inevitably be treated as property to be bought and sold (different price tags/worth) Does not encourage of facilitate intimacy o Slippery slope- genetic engineering, etc. Use of NTRs will lead to widespread use of genetic engineering Gradual acceptance of NTRs will lead to the acceptance of more and more technologies involving genetics (more casually, etc.) Child = product—customer satisfaction ensured Abnormalities can be detected and eliminated- how does one draw the line between eliminating suffering and attempts at eugenics Who can determine “suffering” and “disabilities” Every person has a right to bear a child- should every person have the right to bear a perfect child? C1. Explain Lauritzen’s feminist critique of reproductive technologies. Lauritzen’s feminist critique of reproductive technologies: -An account of a husband’s experience with reproductive technologies -He takes up feminist objections to reproductive technologies after the experience him and his wife have when trying to have children. -He explains feminist’s opponents to reproductive technology that it makes women and children products, and opens the door to wide spread genetic engineering. -Coercive because: 1. They very existence. (expanding their choices makes it hard to choose to accept infertility) 2. Future will include threats to women’s reproductive choices -If you decide to not pursue reproductive technologies you have chosen infertility. -Women are not adequately prepared for the fact these technologies are very experiments and very expensive. -In his experience him and his wife were dehumanized. He has a problem with the language of “harvesting eggs”. He was only valued for his sperm, and his wife her eggs. C2. Know the Roman Catholic lines of reasoning about reproductive technologies, including the position of the Congregation for the Doctrine of the Faith (SCDF) and the responses by Cahill and McCormick. God has shared with man and woman in marriage the power of creation in their act of procreation. The fundamental values connected with the techniques of artificial human procreation o The life of the human being called into existence o The special nature of the transmission of human life in marriage. Advancement of technologies removes procreation from sexual relations. Gift of life must be actualized in marriage through the specific and exclusive acts of husband and wife. Experimentation and scientific research o Human life begins at conception, therefore the zygote demands unconditional respect that is morally due to the human being in his bodily and spiritual totality. o Experimentation should not be allowed on human embryos for the purpose of scientific research Prenatal Diagnosis o If prenatal diagnosis respects the life and integrity of the embryo and the human fetus and is directed towards its safeguarding or healing as an individual, then the answer is affirmative. o Prenatal diagnosis is permitted if it makes it easier to prepare for certain therapeutic, medical and surgical procedures. Medical interventions o As with medical interventions on patients, one must uphold as licit procedures carried out on the human embryo which respect the life and integrity of the embryo and do not involve disproportionate risks for it but are directed towards its healing, the improvement of its condition of health, or its individual survival. o Must have free and informed consent of the mother o The mother should be aware of all the possible risks Experimentation on embryos o Medical research should refrain from operating on live embryos, unless there is absolute certainty that there will be no harm o If the embryos or living, whether viable or not, they must be respected like any other human person o Experimentation on embryos which is not directly therapeutic is illicit. o Corpses of human embryos and fetuses must be respected like the remains of any other human being. It is immoral to produce human embryos destined to be exploited as disposable “biological material” Embryos obtained through in vitro should be considered humans with rights Cryptopreservation offends respect for human beings. It exposes the embryo to risks of death and deprives them of maternal shelter and gestation for some time. Heterologous Artificial Fertilization: techniques used to obtain a human conception artificially by the use of gametes coming from at least one donor other thant he spouses who are joined in marriageà unacceptable o Every human being is always to be accepted as a gift and blessing from God. However, from the moral point of view a truly responsible procreation vis-à-vis/with regards to the unborn child must be the fruit of marriage. o Heterologous artificial fertilization is contrary to the unity of marriage, to the dignity of the spouses, to the vocation proper to parents, and to the child’s right to be conceived and brought into the world in marriage and from marriage. o Surrogacy is morally illicit because it is contrary to the unity of marriage and dignity of procreation Homologous Artificial Fertilization o Within marriage cannot be admitted except for those cases in which the technical means is not a substitute for the conjugal act but serves to facilitate and to help so that the act attains its natural purpose. CAHILL Vatican statement represents a missed opportunity Talked about inseparability of committed love, sexual expression and child bearing of sexual intercourse, failed to state that sex and procreation are best carried out within marriage. Fails to be reflect on objective and universal human values Fails to uphold Roman Catholic tradition of social justice and its emerging awareness that personal and social ethics are 2 sides of the same coin Fails to address the questions of health-care justice that are raised because expensive techniques are only available to a few Fails to affirm equality for women aggressively because it focuses on the physical integrity of sex acts and on rights of the embryos It is a defensive reaction against the possibility that not all traditional articulations of the unity of sex, love, and parenthood measure up to the experience of people whose lives are sexual, marital, and parental and also Catholic Christian. McCORMICK The document deserves careful study o Issues are profoundly important: touches on marriage, parenthood, etc o Likely that a fair # of people will dismiss what the Vatican has to say on sex, which is a mistake. o Many people are likely to draw conclusions on the basis of the dominance of a single value – the provision of a child to a couple who cannot otherwise have one. o Reproductive technology is a runaway poster and is all but unregulated. Appropriate restraints are required. Situation the document o Many people think that Roman statements are final, but they are not. They represent ongoing reflections. “Precise Indications” o Absolute inviolability of germinating life from the moment of fertilization o Rejects surrogate mothers, donated embryos, ova, and sperm, any form of IVF with embryo transfer o Risk of precise indications is that if the congregation wants to insist on procreation worthy of human beings, it should give no support to such moralistic nit-picking because it is contributing to casuistry unworthy of human beings. Congregation is rightly worried about the dehumanizing potential of technology Most controversial à exclusion of in vitro fertilization and embryo transfer in the “simple case” (between husband and wife) o When a child is “conceived as the product of an intervention of medical or biological techniques,” he cannot be “the fruit of his parents’ love.” C2. Know the Roman Catholic lines of reasoning about reproductive technologies, including the position of the Congregation for the Doctrine of the Faith (SCDF) and the responses by Cahill and McCormick. Position of the Congregation for the Doctrine of the Faith o Background: Require: the respect, defence and promotion of man, his “primary and fundamental right” to life, his dignity as a person who is endowed with a spiritual soul and with moral responsibility Basic scientific research and applied research constitute a significant expression of this dominion of man over creation Require unconditional respect for the fundamental criteria of the moral law Morally acceptable use of artificial human procreation involves 2 values: 1) life of human being called into existence; 2) the special nature of the transmission of human life in marriage “gift of human life must be actualized in marriage through the specific and exclusive acts of husband and wife, in accordance with the laws inscribed in their persons and their union” o Status of human embryo Human being must be respected as a person from the first instant of existence Embryo demands the unconditional respect that is morally due to the human being in his bodily and spiritual totality o Prenatal Diagnosis Permitted when parents consent and are informed and methods are safe Opposed when abortion will be considered depending on the results of the tests o Therapeutic procedure used on human embryos Allowed if there are no disproportionate risks and the procedure is directed towards healing, the improvement of health, or survival o Research/Experimentation of Human Embryos Medical research must refrain from operations on live embryos unless there is a moral certainty of not causing harm to life/integrity of mother/child Embryos = people- experimentation that is not directly therapeutic is illicit (includes embryos that are not used after in vitro fertilizations, etc.) Corpses of embryos must also be respected just like the remains of other human beings o Embryos in vitro Disposing of extras- researcher usurps the place of god, sets himself up as the master of destiny because he chooses who lives/dies o Manipulation of embryos in human reproduction Freezing embryos- not allowed because it goes against respect for human beings Cloning is not allowed because it opposes human procreation/conjugal union Genetic engineering is not therapeutic o Interventions upon human procreation IVF: destruction of human embryos- not allowed Must take place in marriage: Child has the right to be conceived, carried in the womb, brought into the word, and brought up within marriage Heterologous artificial fertilization Not ok because it involves a third party (if married couple is involved) or a person who will not be part of the child’s life (if a single person is involved) Surrogate motherhood: Contrary to the unity of marriage and to the dignity of the procreation of the human person Creates a division between the physical, psychological, and moral elements of a family Homologous artificial fertilization o Contraception is not allowed because it deliberately deprives the conjugal act of its openness to procreation Fertilization outside bodies is deprived of the meanings and values which are expressed in the language of the body and the union of human persons Morally illicit? o Unnatural o Illicit even when extra embryos are not discarded and masturbation is not involved because it deprives human procreation of the dignity which is proper and connatural to it If procedure does not replace conjugal act but simply facilitates it—OK Marriage does not = right to have a child; sterile couples have options of adoption, etc. Important rights: Right to life and physical integrity Right of the family and of marriage Child’s right to be conceived, brought into the world, brought up by his parents Cahill o o Vatican’s statement represents a missed opportunityBy tightly tying the inseparability of committed love, sexual expression and child-bearing to the natural biological structure of sexual intercourse, Vatican undercuts potential consensus on the message that sex/procreation should be in a loving marriage o Marks artificial reproduction in all cases as “illicit” o Focuses too much on human “nature,” “dignity,” and “rights” o Fails to uphold the RC tradition of social justice and its emerging awareness that personal and social ethics are the same instead calls for prudent public policy (still bases restrictions on individual acts) McCormick o Document deserves careful study o Argues that Roman statements are not the final word- actually represent contributions to ongoing reflection, not closure of it o Document focuses on precise indications Rejects everything except sexual intercourse Example of way around it- intercourse with a perforated condom so some sperm are imprisoned while others are not- finds casuistry debasing and repugnant, moral nit-picking o Sexual intercourse is not the only act of love in a marriage C3. Describe the Jewish position on reproductive technologies, as depicted by Mackler, and show how it compares to and contrasts with the Catholic position provided by the SCDF. Mackler dictates three clusters of values that are central in addressing the issues raised by reproductive technologies. o Procreation and the family Having children fulfills “mitzvah” (religious responsibility) IVF would satisfy this “mitzvah” However, reproductive technologies could have negative effects on communal values and on physical, personal, psychological and financial aspects o Responsibility of human stewardship Active partnership with God in completing “tikkun haolam” (completing works of creation and improving the world) “mandate to heal” o Humans created in God’s image Importance of respect for persons “K’vod habriyot” Jewish thinkers stressed connection of creation in God’s image with human free will Emphasizes responsibility to respect persons’ autonomous choices Some in Jewish world argue that reproductive technologies upset the “order of creation” o Make it impossible to view husband and wife as truly parents of offspring Procurement of sperm in IVF violates traditional prohibition of “emission of seed in vain” o But most halakhic authorities accept IVF IVF and reproductive technologies acceptable when considered a medical intervention Overall, in Jewish religion reproductive technologies can be used in certain circumstances In the SCDF, a much stronger argument is taken against reproductive technologies including IVF o Technologies contrary to the human dignity proper to the embryo o Contrary to right of every person to be conceived and to be born within marriage and from marriage o “twin fission” not permissible because contrary to moral law o Freezing of embryos not allowed because constitutes an offense against the respect due to human beings C3. Describe the Jewish position on reproductive technologies, as depicted by Mackler, and show how it compares to and contrasts with the Catholic position provided by the SCDF. - Talmud states that there are three partners in creating a human being: mother, father, and God. - IVF may pose certain medical risks; however, it is allowed according to Mackler in certain cases. - Infertile people can use own sperm and egg for IVF. - Should avoid having children with genetic disabilities. - Freezing embryos is fine as well; however, none should ever be thawed to be discarded. - Having donated sperm or eggs can be acceptable, but all the ethical concerns should always be considered by the couple. - The Jewish position contrasts with the Catholic position in that the Catholic position does not find reproductive technologies acceptable. These technologies take away the dignity of the human being and love between parents, and they ultimately bring up a great deal of moral concerns since they are not natural. C3. Describe the Jewish position on reproductive technologies, as depicted by Mackler, and show how it compares to and contrasts with the Catholic position provided by the SCDF. Guiding Values o Children = blessing for parents and broader community o In vitro = potential to bring new child into world, provide life to a child who would otherwise not be born, harmony/joy to family, strengthen community o People must have an active partnership with God in completing the works of creation and improving the world o Humans are created in God’s image- respect persons’ autonomous choices In Vitro Fertilization and Embryonic Development o Important to assess potential risk/benefits of various uses of the procedure (treatment of embryos outside the body, etc.) IVF using a couple’s own ova and sperm o Evaluate benefits/risks for couples, families, children, society, etc. o Some orthodox Jews reject- diverges too dramatically from natural reproduction, “upsets order of creation” Allowed when it is the only way the a couple can have children o Some see it as a way of assisting pregnancy: enable a couple to have a child reverent and active partnership with God o Other issues: IVF is objectionable if it entails risks for the embryo and increases the likelihood of a seriously impaired child Also destruction of embryos o Jewish law prohibits endangering one’s life and exposing one to excessive risk o OVERALL- Use of IVF in homologous cases = widely accepted in Conservative and Reform movements; never required, sometimes ill-advised, ethically acceptable Transferring In Vitro Embryos for Gestation o Some uses of IVF still require ethical evaluation o Pre-implantation genetic testing: Allowed because of status of fetus under Jewish law Genetic diagnosis and selective transfer of embryos is no more problematic than prenatal diagnosis and abortion of a fetus with severe genetic disease (also allowed) o Number of embryos transferred Multifetal pregnancy reduction = acceptable for Jewish ethics (health of mother, protection of remaining fetuses) Important to take reasonable steps to reduce possibility for need No more than three embryos should be transferred in a procedure Embryos not transferred o Creating extra/freezing embryos = acceptable in Jewish ethics Procedures both enhance likelihood of success and minimize medical risks/burdens faced by the woman o Embryos that are not intended to be transferred have no significant status and may be discarded o Thawing embryos in order to discard them- not ideal but acceptable o Allowing an embryo to be observed for scientific research (not more objectionable than discarding) o Further stages of development – NOT OK Donor Gametes and Embryos o Orthodox thinkers generally oppose the use of donor gametes- violates family bonds, parenthood, etc. o Otherwise- acceptable: Brings a child into the world Relieves suffering of parents who could not otherwise have children, etc Couples must not keep it a secret, especially within family Must also consider adoption o Donating Embryos Donor would be responsible for assuring that any biological offspring is likely to be well cared for o Medical risks must be evaluated as well If Judaism allows use of donated embryos- they also must allow for donations (repay society, etc.) Maternal identity Donor of eggs = genetic mother Pregnant/birth = birth/gestational mother Raises child = social mother Religion of child: woman’s status at time of birth determines the child’s identity C3. Describe the Jewish position on reproductive technologies, as depicted by Mackler, and show how it compares to and contrasts with the Catholic position provided by the SCDF. Jewish position is nearly opposite of Catholic position in moral standing of the technology. Both religions focus on the need for respect and the value of family but Judaism views reproductive technology as aiding in the creation of family while Catholicism sees it as destroying the sanctity of marriage, etc. C3. Describe the Jewish position on reproductive technologies, as depicted by Mackler, and show how it compares to and contrasts with the Catholic position provided by the SCDF. Jewish view of reproductive technologies: -It can be ok to use IVF if the couples own sperm and egg are used. -there are 3 partners in creation: husband, wife and God. - Offers child life and parents the ability to procreate and fulfill mutzavah. -Yet it reproductive technology can affect communal values. -do not approve of donor gametes because man must be created in the image of God out of a loving relationship. Cahil and McCormick-Cahil: Feels the church has missed an opportunity by grouping “artificial reproduction between couples in the same category as with donor gametes. -feels assertions are substituted for “nuance arguments” -also does not address personal and social ethics separately. C3. Describe the Jewish position on reproductive technologies, as depicted by Mackler, and show how it compares to and contrasts with the Catholic position provided by the SCDF. McCormick-Says the document deserves careful examination -It touches on some very important basic values (marriage, parenthood, good of children). -Says what the Vatican says should not just be dismissed as yet another similar Catholic position, rather it is an ongoing relfection. -Thinks they are rightly worried about the dehumanizing effect of technology. Comparing the documents (Jewish and Catholic) -Main difference is that the Jewish teaching allows the use IVF if the only partners are wife and husband. The Catholic tradition does not allow for any form of artificial insemination that takes out the conjugal act (more focus on the importance of the the conjugal act resulting in the creation of child) C4. Highlight the different religious perspectives on reproductive and research cloning. -Catholic: There is a general strong opposition. -The human being must be respected from the very first instant of his/her existence. -Just because technology is available for cloning does not make the cloning of humans morally acceptable. -“Attempts or hypotheses for obtaining a human being without any connection with sexuality through ‘twin fission’, cloning or parthenogenesis are to be considered contrary to moral law, since they are in opposition to the dignity both of human procreation and of the conjugal union.” -Human dignity is violated by the cloning of human beings because the foundation of this dignity is that each human being is created by a unique creative act of God. -Although identical twins are identical, neither one is the source or maker of the other. -According to Father Albert S. Moraczewski, cloning may be for helping endangered species or other animals, but not for human beings. -Jewish: Views vary, approved in some scenarios. -In summary, the theological and moral assessment of human cloning depends upon how it is used. -If choosing who is to be cloned based on social terms, it would violate the Jewish principle that we all have inherent worth as creatures created in the image of God. -Cloning cheapens life and makes human beings like inanimate objects on an assembly line when deciding the good and bad results of cloning. -An example of cloning for a bone marrow transplant can display what is justifiable and unjustifiable in reproductive and research cloning. It would be justifiable to produce a clone with the intent of transplanting bone marrow to an existing person with leukemia if the intention of those involved was to raise the clone as they would raise any other child. However, it would be unjustifiable to produce the clone, perform the transplant, and then destroy the clone. -Cloning must not be used to create “model” human beings. -There must be a balance between our actions and God’s. -An example: The Torah states that God imposes illness as punishment for sin, which may lead some to believe that medicine is not right to intervene in God’s decision to give illness, indeed, an act of human hubris. -Rabbis have also counteracted this position by stating that God authorizes and requires us to heal based on the written scripture of Exodus and Deuteronomy -If cloning humans is intended to advance medical research or cure infertility, it has a proper place in God’s scheme of things, according to Jewish tradition. -Cloning that supports human self-idolization and gives hope to a possibility of immortality is frowned upon. -Protestantism: There are various positions, but they are mostly opposed. C4. Highlight the different religious perspectives on reproductive and research cloning. Roman Catholicism o Strong opposition for both cloning and reproductive technologies o See SCDF section in C3 Judaism o More loose than in Roman Catholicism o Reform Judaism allows for the most technologies to be used o Orthodox Judaism is the most stringent for technologies to be used o See Mackler section in C3 Baptists and Evangelicals emphasize individual judgment C4. Highlight the different religious perspectives on reproductive and research cloning. - Cahill (Catholic) o NO to cloning Individuality potential loss of individuality is not too important Family loss of rules and social stability - Father Albert (Catholic) o NO to cloning Exceeds human limits Loss of human dignity Sex-procreation-marriage Eugenic intent Danger that child becomes an object - Meilander (Protestant) o NO to cloning Limits male and female parenthood People are begotten, not made - Dorff (Jewish) o Regulated cloning, but shouldn’t be banned Concern with cloning Exploitation Cheapens life Difficult to decide who is parent Increased inequality Should not be banned because there is a Jewish obligation to heal other humans in partnership with God. C5. Explain the position taken by the President’s Council on Bioethics with regard to reproductive and research cloning and the reasons the Council offered for its positions. -The Council on reproductive cloning: -Once the human embryo (child-to-be) is carefully considered, the arguments that overemphasize the freedom, desires, and control of parents are not sufficient to overcome the powerful case against engaging in reproductive cloning. -There seems to be no ethical way to try to discover whether reproductive cloning can become safe, now or in the future. -Five categories of concern for reproductive cloning: 1. Problems of identity and individuality -The cloned child will have expectations to live up to and comparisons being formed to the “original” child. 2. Concerns regarding manufacture -It could increase commercialization and industrialization of human procreation since these cloned children have been genetically chosen in advance and could then be seen as products rather than gifts. 3. The prospect of a new eugenics -If cloning were to be successful, it might end individualized eugenic enhancement by avoiding genetic defects or by preserving notable genetic traits. 4. Troubled family relations -It would transgress the natural boundaries between generations and strain the social ties between them. For example, mothers could give birth to their genetic twins. 5. Effects on society -It could affect how society views children and cause an intervention in novel forms of control by one generation over the next. *Conclusion: For some or all of these reasons, the Council is in full agreement that reproductive cloning is not only unsafe but also morally unacceptable, and ought not to be attempted. -The Council on research cloning: -The Council is divided on the ethics of cloning for research. -They agree that all parties to the debate have concerns vital to defend, vital not only to themselves but to all of us. They feel no human being and no society can afford to be callous to the needs of suffering humanity, or cavalier about the treatment of nascent human life, or indifferent to the social effects of adopting one course of action rather than another. -They present competing ethical cases for and against research cloning: -The moral case for research cloning: -Position One: Most council members have serious moral concerns. They feel these concerns can be addressed by setting proper boundaries. -Intermediate moral status: -The cloned human embryo has a developing and intermediate moral worth that requires respect, but it is morally permissible to use early-stage cloned human embryos in important research under strict regulation. -Deliberate creation for use: -The concerns for the problems of deliberate creation of cloned human embryos for use in research are termed to have merit, but don’t prevent research cloning. Cloned human embryos are not “created for destruction”, but instead are created for use in the service of life in medicine. Their destruction is in the service of a great good. -Going too far: -They approve only of research on cloned human embryos that is limited to the first fourteen days of development, not of research past the blastocyst stage. -Position Two: A few council members don’t share the above ethical qualm and feel that research cloning has no special moral problems and should be used for medical knowledge and benefits to humankind. -The moral case against research cloning: -Moral status of the cloned embryo: -It states that the position two (above) is mistaken about the equality between earlystage human embryo and all other human cells and that the position one (above) is unconvincing for biological and moral reasons. There should be continuous history and equal respect of human individuals from the embryonic to fetal to infant stages of existence. -The exploitation of developing human life: -Research cloning crosses the significant moral boundary of the creation of human life that is specifically for the sole purpose of research and is deliberately destroyed. Granting this research would be granting the view that nascent human life is only a resource or tool. -Moral harm to society: -It would risk significant moral harm to our society by approving the genetic manipulation and control of nascent human life, opening the option to reproductive cloning or research on later-stage human embryos and fetuses, and potentially putting the government in the position of mandating the destruction of nascent human life. Prudence requires us not to engage in cloning for research. -What we owe the suffering: -We all are patients or potential patients, but we are not just that, and easing suffering is not our only moral obligation. We owe our children a world that honors moral limits, that respects all life whether strong or weak, and that refuses to secure the good of some human beings by sacrificing the lives of others. -The Council’s Policy Recommendations: -Their ethical and policy analysis leads them to the conclusion that some deliberate pubic policy at the federal level is needed in the area of human cloning. -Majority Recommendation (10 members): -They recommend a ban on reproductive cloning combined with a four-year moratorium on cloning for research. They also call for a federal review of current and projected practices of human embryo research, pre-implantation genetic diagnosis, genetic modification of human embryos and gametes, and related matters, with a view to recommending and shaping ethically sound policies for the entire field. -They believe that our society should carefully address this decision by taking time to make a judgment that is well-informed, respectful of strongly held views, and representative of the priorities and principles of the American people. They believe the ban-plus-moratorium proposal offers the best available way to a wise and prudent policy. -Minority Recommendation (7 members): -They recommend a ban on reproductive cloning, with regulation of the use of cloned embryos for biomedical research. -They believe this approach will insure that abuses are prevented and that the concerns regarding human cloning displayed within this report are adequately addressed by their ban-plus-regulation proposal. They feel the nation should support this responsible effort of finding treatments and cures to aid those who are suffering. C5. Explain the position taken by the President’s Council on Bioethics with regard to reproductive and research cloning and the reasons the Council offered for its positions. Council developed 5 categories of concern regarding cloning to produce children o Problems of identity and individuality Cloned children will be genetically identical and therefore will face problems of identity Expectations of cloned may be shadowed by comparisons to “original” o Concerns regarding manufacture Might be considered more products of a manufacturing process than “gifts” whom their parents are prepared to accept as they are Increased commercialization and industrialization of human procreation o Prospect of a new eugenics Cloning may lead to individualized eugenic enhancement o Troubled family relations Cloning could strain social ties between generations Genetic relation to only one parent might produce special difficulties for family life o Effects on Society Affect the way society looks at children Position number one: Council Members favor cloning for biomedical research have serious moral concerns o Intermediate moral status o Deliberate Creation for use o Going to far o Other Moral hazards Position number 2: same as position number one but that research presents no special moral problems and therefore should be endorsed with enthusiasm C5. Explain the position taken by the President’s Council on Bioethics with regard to reproductive and research cloning and the reasons the Council offered for its positions. - Cloning of humans is not currently successful, but this may soon be possible; thus, this should be seriously considered. - Strict ban on all human cloning July 2001. - Other countries and the UN are working towards banning all human cloning. - Use of clones for obtaining stem cells is wrong because it exploits and destroys human life. - The meaning of individuality and having children would be blurred if cloning were allowed. - People may be manipulated and exploited. - Cloning to create children children become objects - All in all, cloning would degrade society and trouble families C5. Explain the position taken by the President’s Council on Bioethics with regard to reproductive and research cloning and the reasons the Council offered for its positions. Majority recommendation On reproductive cloning: ban Demonstrates strong ethics Unanimous in the Council (and in Congress) and widely supported by the American people Problems that could result of reproductive cloning is not banned: o Problems of identity and individuality “original” vs. clone o Concerns regarding manufacture Entire genetic make-up selected in advance?—children more like products? o Prospect of a new eugenics o Troubled family relations Generational mix-up o Effects on society Change the way society looks at children/non-therapuetic interventions On research cloning: four-year moratorium Demonstrates high regard for the value of biomedical research, but also establishes an additional safeguard not afforded by policies that would allow the production of cloned embryos to proceed without delay Calls for and provides time for further democratic deliberation Would afford time for scientific evidence that would give us a better sense of whether cloning for this purpose would work as promised Two views: 1) moratorium to enable us to make our case in a democratic way, 2) give time to develop a system of national regulation that might come into use C6. Describe Murray’s perspective on reproductive cloning. -As stated by Murray himself, “Life flows in one direction; science cannot reverse the stream or reincarnate the dead”. Murray strongly believes that there are four hard truths to reproductive cloning: -The first truth is that cloning does NOT produce healthy, normal offspring. -The second truth is that even if a healthy embryo were produced through cloning, that embryo would not be the same person as the one whose genetic material was used. -The third truth is that creating a child to replace another dead child is unfair. -The fourth truth is there is no real escape from grief. -Murray addresses these truths by discussing his own personal loss of a daughter and comparing it to a man’s written loss of a young child. According to Murray, the man who wrote the letter of his 11-month-old son’s loss of life to heart surgery forms false hope of successful cloning of his lost son due to other scientists’ claims that cloning is safe. It is through Murray’s past experiences that he forms a healthy perspective of the reality of reproductive cloning. C6. Describe Murray’s perspective on reproductive cloning. Murray comments on the position of another father. The other father lost his daughter, and he hopes that research on cloning will be allowed to continue to that one day she may be brought back. Murray has also lost a child and understands these emotions; however, he states that we are all much more than the sum of our genes. Cloning someone would not bring back their memories and experiences. In addition, this would not be fair to the clone since he/she would have to live up to the standards of the dead person (for example, a clone of Michael Jordon might not have any interest in playing basketball). C6. Describe Murray’s perspective on reproductive cloning. Murray who himself lost his child is overall against cloning o At the current stage the clone would not be healthy The only way to guarantee that the clone would be healthy would be to unlock the secrets behind every single cell to be cloned Thus, currently would be a blatant example of immoral human experimentation o Even if clone produced, would not be same as the original person Thus would not be viable to make a clone in order to replace a person Creating a child to stand in for another dead child is unfair C6. Describe Murray’s perspective on reproductive cloning. “Even If It Worked, Cloning Wouldn’t Bring Her Back” Murray had lost his 20 year old daughter (murder victim) and he responding to a letter by a father mourning over the death of his 11-month old son. The father wants to revive the memory of his son through cloning, though Murray entirely disagrees with reproductive cloning and states, “Cloning can neither change the fact of death nor deflect the pain of grief.” He supports his statement by also saying: 1. Cloning does not result in healthy, normal offspring (and thus, experimentation at this stage in the technology would be “immoral human experimentation.” “Even if cloning produced a healthy embryo, the result would not be the same person as the one whose genetic material was used.” 3. Cloning a child = reincarnation of someone else… parental expectations for the child, perverse? Essentially, Murray says that we should try to preserve their memory rather than attempting to bring them back through cloning. 2. C7. How would different ethical principles apply to the above discussions? -The ethical principles of freedom, equality, and human dignity would be quite notable in regard to reproductive and research cloning. Determining the importance and priority of these ethical principles is where the issue stands. The importance of these principles is varied in the views of the President’s Council on Bioethics, Murray, and the different religions. - Ethical principles such as nonmaleficience and beneficence apply to the above discussions. Cloning can lead to causing harm on not only the clone (by extraction of cells and experimentation), but to the person who was cloned due to his/her loss of identity. - Rule of double effect: o Killing a clone to save the life of another is not ethical since life is taken in the process. - Autonomy: o Who is responsible for the clone? Does a clone have equal rights? C7. How would different ethical principles apply to the above discussions? Ethical principles that apply to cloning o Respect for autonomy Respect for autonomy for both the people wanting to use reproductive technologies and the human developed/cloned through reproductive technologies o Right for individuality Cloning as said above in the President’s Council would greatly diminish the individuality of humans o Lack of proven safety As said above, cloning is not at the stage where the clone would be guaranteed healthy C7. How would different ethical principles apply to the above discussions? Respect for autonomy (procreative liberty) The respect to choose how to have a child—in vitro, artificial insemination, adoption, etc Beneficience Whether or not the benefits would override the costs for therapeutic cloning D1. Explain the distinction between germ-line and somatic-cell interventions and between therapeutic and enhancement interventions. What ethical significance do these distinctions have? Germ-line interventions: line of germ cells that include sex cells (sperm, egg); changes made to this kind of cell would not only affect patient but also offspring Somatic-cell interventions: non-reproductive cells; changes made to this kind of cell would only be limited to patient and not affect offspring Therapeutic interventions: meant to correct disease (ex: make symptoms non-existent or less harmful) Enhancement interventions: meant to improve qualities (ex: choose sex, hearing ability or lack of) Somatic cell gene therapy is least controversial/most widely accepted by society o Concerns about slippery slope from this kind of therapy to others, especially germ-line enhancement Germ-line gene therapy is second most accepted Somatic cell enhancement is third Germ-line enhancement is least Somatic-cell interventions have more ethical concerns than germ-line because of right of autonomy (unborn has no part in decision-making), unpredictability of consequences for unborn Enhancement interventions have more ethical concerns than therapeutic because can be viewed as futile and not medically necessary D1. Explain the distinction between germ-line and somatic-cell interventions and between therapeutic and enhancement interventions. What ethical significance do these distinctions have? Germ-line intervention The germ-line starts as the fertilized egg, or zygote. In the case of germ line gene therapy, germ cells, i.e., sperm or eggs, are modified by the introduction of functional genes, which are ordinarily integrated into their genomes. Therefore, the change due to therapy would be heritable and would be passed on to later generations. Somatic-cell intervention Somatic Cells make up the rest of the body. In the case of somatic gene therapy, therapeutic genes are transferred into the somatic cells of a patient. Any modifications and effects will be restricted to the individual patient only, and will not be inherited by the patient's offspring Somatic cell (non-repro cell) Germline (sperm, egg, embryo) Correct disease 1 2 Enhance qualities 3 4 There is concern about the slippage from #1 to the others (particularly #4) Therapeutic intervention As for therapeutic cloning, it allows for the growth and cloning of stem cells to grow into a piece of human tissue or a complete human organ for transplant—the end result would not be a human being, but a replacement organ, or piece of nerve tissue, or quantity of skin. Some ethical issues would include: 1) the moral status of the cloned embryo, 2) the exploitation of developing human life—in that the creation of human life is only for the purpose of its use in research, 3) moral harm to society—in that it would open the door to reproductive cloning, etc Enhancement intervention Examples: Athletes’ use of performance enhancing drugs and genetic intervention, sperm-sorting or pgd to choose sex of their children, etc Issues: safety, fairness and non-discrimination, respect for the human embryo, and “enhancement threatens our humanity by eroding human agency” D1. Explain the distinction between germ-line and somatic-cell interventions and between therapeutic and enhancement interventions. What ethical significance do these distinctions have? types of human genetic engineering o somatic only affects individual ethical issues discussion of research involving human subjects (see lecture 10) concern about slippage from 1 to the others (particularly 4) designed to correct a gene that is causing/will cause a disease acceptable however the difference b/t diseases and qualities is vague o germline will affect individual as well as future generations Somatic Cell Germline Correct Disease 1 2 Enhance Qualities 3 4 historical background o eugenics movement in the U.S. and elsewhere Nazi Germany Virginia’s role in the eugenics movement Lynchburg story images and metaphors o images from Brave New World o slippery slope argument from correction of diseases to enhancement of qualities. non-genetic intervention of HGH genetic enhancement in sports from somatic cell to germline interventions may occur if its more efficient o playing God 2 senses unlimited power to decide unlimited power to act, including creating new life forms theological support of human genetic engineering (at least w/in limits) discussion of “co-creation” criticisms o transgression of limits o failure in garden of Eden and failure to accept human responsibility creation of humans in the image of God concern about the unpredictability of consequences and uncertainty in their evaluation D2. Analyze Buck v. Bell, including Gould’s assessment and the connection between genetics and eugenics. Emma Buck was committed to an institution on the grounds of feeblemindedness of which there was little evidence she had a daughter, named Carrie (CB) who was also committed for the same reason o the true reason here was probably to hide the fact that she had been raped and become pregnant o no evidence of mental deficiency CB, in turn, had a daughter named Vivian (VB) who was also deemed mentally deficient o again, no real evidence o having 3 generations committed was enough, at the time, to prove a pattern (i.e. deficiency caused by genetics) vs coincidence CB was the 1st person to be selected fro sterilization under the new act o compulsory sterilization law, 1924 VA Buck v Bell o challenged the sterilization of CB o headed by VA Christians o Supreme Court upheld the law 8-1 o Holmes majority opinion: “Three generations of imbeciles are enough.” in 1980, Dr. Nelson uncovered 4000 sterilizations of mentally deficient patients o including CB and her sister Gould views this as a horrible mistake in history eugenics was based falsely on genetics o Laughlin’s list of “genetic” disorders blindness and serious visual impairment deafness and serious hearing impairment orphans ne’er do wells tramps paupers o most forms of mental deficiency are not genetic 1 of the 2 main arguments used in defense of the law said that most were genetic D2. Analyze Buck v. Bell, including Gould’s assessment and the connection between genetics and eugenics. Buck v. Bell (1927) was the United States Supreme Court ruling that upheld a statute instituting compulsory sterilization of the mentally retarded "for the protection and health of the state." It was largely seen as an endorsement of negative eugenics—the attempt to improve the human race by eliminating "defectives" from the gene pool. *Gould believes that the Supreme Court decision was based on falsehood and that Carrie Buck’s daughter was not mentally ill Americans eugenic movement at its peak in 1920s Harry Laughlin, superintendent of the Eugenics Record office proposed model sterilization law in 1922 to remove “the most worthless one-tenth” of population State of VA passed compulsory sterilization law in 1924 Carrie Buck’s daughter Vivian had decent food, upbringing, medical care, and education – so how could state of VA justify sterilizing her against her will? Laughlin’s testimony to Supreme Court based on 2 major points: 1. Carrie buck and Emma buck were feebleminded by Stanford-Binet IQ test (which was an unproven and new test at the time) 2. Most feeblemindedness resides in genes In 1980, Dr. K. Ray Nelson found Carrie Buck alive and well near Charlottesville, she was obviously a woman of normal intelligence. Paul Lombardo wrote “she was neither mentally ill nor retarded” Miss Wilhelm, who initially was said to have stated Vivian Buck had a mental deficiency later denied that she had ever examined Vivan or deemed her feebleminded *Gould believes her case was never about mental deficiency but that Carrie was prosecuted for supposed sexual immorality and social deviance D2. Analyze Buck v. Bell, including Gould’s assessment and the connection between genetics and eugenics. 1927 Supreme Court case that ruled in favor of compulsory sexual sterilization Believed it did NOT violate the 14th amendment which requires equal protection of the law Since they thought imbecility was inherited, had a right to protect the “greater good” from more feeble-minded people being reproduced (“three generations of imbeciles are enough”) Carrie Buck: poor, uneducated white woman; became committed to the State Colony for Epileptics and Feeble-Minded in Lynchburg for becoming pregnant at a young age and unmarried (result of rape) Carrie’s daughter, Vivian, was deemed feeble-minded from when she was a baby because it seemed “very apathetic and not responsive,” very biased and unreliable statement because no way to measure imbecility in babies Gould’s assessment o Compulsory sterilization became popular because of eugenics movement and safer operations (imposed on criminals, people with hereditary defects like alcoholism, “imbeciles”) o The fact that three generations of women were all imbeciles proved that imbecility was not an accident but a hereditary trait, even though Carrie actually had normal intelligencemethods to prove this fact were not scientifically sound nor legitimate o Real reason Carrie was stigmatized was for her sexual immorality, very looked down upon by society at this time for having premarital sex Genetics: scientific study of heredity Eugenics: purpose was to “create better humans through breeding,” movement to “improve” human race by preventing reproduction of those deemed biologically unfit and encouraging reproduction among the “worthy” D3. Know the story of Sharon and Candy, especially in relation to the pieces by Nance and Kilner. Sharon and Candy o lesbian, deaf couple o have a deaf daughter and want to have another deaf child o since deafness is not a “desired” trait, it is not selected for at sperm banks used sperm donated by a deaf friend o wanted a deaf child b/c: they were deaf and felt they’d be better able to cope w/ his struggles than those of a hearing child they believe the deaf community is very close and has a unique culture Nance o case of a couple, both w/ probable recessive deafness, who’ve come in for genetic counseling author assumes they want to have a hearing child and refers to deafness as a “defect” or “abnormality” this offends the couple and shows the author that deafness can be “a defining cultural characteristic rather than a handicap” this is parallel to the case of C and S b/c they also believe that deafness is not a disability but a feature to be embraced o “does adherence to the concept of nondirective counseling actually require that we assist …a (deaf) couple in terminating a pregnancy w/ a hearing child? “some draw analogy w/ Catholic physicians who refer pts to other drs when they require genetic counseling” argue that the advice is best given by a deaf person others say that selecting for deafness is “dysgenic (and) would constitute a perversion of the process of genetic counseling” others say that the most important thing is the welfare of the fetus if there is no danger to the fetus, there is no justification for termination o “educated members of the deaf community are themselves widely divided in their views about the appropriate use of genetic tech” o it is “critically important…to consider the cultural values of the target population and…any program that attempts to provide genetic services for the deaf will have to take these…divergent value systems into account” Kilner o “is it ethical for parents to force their children to have genetic traits that will be harmful to the child but beneficial to the parents?” o 2 responses “all ppl…should be free to pursue their desires but not in ways that prevent others from pursuing theirs” “we can more clearly see the harms of (this) when we consider how we would view the same harm w/o the genetics involved” o response 1 we expect even more from parents – they should be trying to enhance their child’s experiences, not hinder them but at the very least, “parents ought not to disadvantage their child so that (the parents) can benefit even members of the deaf community admit that options are limited for deaf ppl indicating that it is indeed a disability not deaf discrimination but a human rights case if this is allowed, we are saying that parents can do whatever they want to their children as long as they (the parents) benefit from it o response 2 “wouldn’t we condemn parents who took some tool and intentionally destroyed their child’s ability to hear?” this is what is happening, only using genetic tools o Sharon and Candy’s justifications their life as deaf ppl is fine, and their kid’s life will be too o response: while ppl are very resilient and can adjust and adapt to difficult situations, it doesn’t mean these situations should voluntarily be imposed upon them if it’s ok for black parents to select for a black child b/c they are black, its ok for deaf parents to select for a deaf child response: being black doesn’t “necessarily impose major limitations” society may limit ppl based on race but this can and should be removed “the limits of deafness, however, are not completely the product of human prejudice and are not all removable” new issue: “how ethical is it to impose characteristics on ppl that are not necessarily harmful, but which they may not want?” ex not everyone wants to be a man, be white, etc conclusion: “perhaps only genetic interventions all ppl would want can ethically be imposed on children” i.e. prevention of fatal diseases, etc D3. Know the story of Sharon and Candy, especially in relation to the pieces by Nance and Kilner. Sharon and Candy: deaf, lesbian couple trying to have second deaf baby through friend’s sperm donation Couple doesn’t see a problem with purposefully trying to have a deaf baby because for them, it would be easier to communicate, raise, and deafness isn’t a disability but an identity Others argue that it violates their duty of parenthood by placing limits on child’s potential and making their life more difficult than necessary Deaf children’s schools are paid by public funds which costs public more but increases diversity Nance: o To deaf couples, do not view their condition as a “defect” but just a “trait” and it is insensitive of society to maintain the opposing mindset o Genetic counseling could be applied to deaf couples in 2 ways: Should be used to remove deafness from offspring; selfish for deaf parents to want deaf babies because just because they can live freely with their condition doesn’t mean it should be forced upon their children Should be prohibited because not right to play “God” and also, sends a message to deaf people that they are deficient and no more of their people should exist Kilner: o Believes this is not a “deaf rights” case but a “human rights” case since it asks whether parents can impose limits on children ethically; it’s not saying that deaf people are not worthy but purposefully implementing a harmful trait is wrong o Parents would be condemn if they used a tool to intentionally damage children’s hearing, essentially what genetic counseling is o Not acceptable to cause deafness; completely unrelated to accepting deaf people D3. Know the story of Sharon and Candy, especially in relation to the pieces by Nance and Kilner. Sharon and Candy were a deaf lesbian couple who wanted a deaf child. Deaf community is pretty close knit and generally supports bringing in more deaf people to their group. Daughter Jehanne is deaf as well. New son Gauvin is born and after testing he is not as deaf as Jehanne but still has a significant amount of hearing loss. Sharon and Candy decide that if he wants a hearing aid later, they will let him, but won’t put him on one while he’s in infancy Nance agrees that deafness should not be treated as a deformity but simply an attribute. Deaf people often want their children to be deaf as well, so a genetic counselor should not try to approach deafness as an illness, but instead go with what couple wants. Kilner believes that there are ethical limits to what parents can impose on a child. Parents or anyone else should not be allowed to impose a harmful characteristic on their child. Deafness imposes a limitation on the child and should not be justified. D4. Explain Behar’s & Sandel’s respective positions on genetic enhancement in sports & the ethical norms to which they appeal. Behar o the World Anti-Doping Agency has defined gene doping as “the non-therapeutic use of genes, genetic elements and/or cells that have the capacity to enhance athletic performance” o gene doping is very difficult to detect only way to prove it is to “biopsy a suspicious muscle and look for signs of DNA tampering” obviously not desirable for athletes o gene doping would significantly increase the strength and durability of athletes’ muscles – very desirable o a poll of American athletes showed that most would “take any drug that would help them win even if they knew (it) would eventually kill them” evidence for the need for parentalism o there are not clear lines b/t using gene therapy to repair injuries vs for enhancement o he seems to believe that it is a dangerous science for several reasons its virtually undetectable it could have severe long term effects but that probably wouldn’t deter athletes it would provide an unfair advantage to certain athletes Sandel safety objection seeks improvements at the cost of incurring medical risk o least controversial and least interesting objection o leaves unanswered whether the practices of genetic enhancement/selection are troubling in and of themselves arguments re means o fairness and non-discrimination o respect for the human embryo o ex skewed gender ratio in China some worry about the gender discrimination some worry about the discarded female embryos both are troubling, but they aren’t the only reasons why sex selection is morally troubling usually doesn’t involved killing embryos or discrimination argument re free will o ex steroids are safe and available to all so none have an unfair advantage what, if anything, would be wrong w/ them?? o still troubling – resides in not only the means, but also the ends being aimed at o threatens human capacity to act freely and for ourselves o sporting achievements wont be as impressive if accomplished w/ aid of steroids “as the role of enhancement increases, our admiration for the achievement fades” “this suggests that our moral response to enhancement is a response to the diminished agency of the person whose achievement is enhanced” this is not the biggest problem; it is the danger of trying “to remake nature…to serve our purposes and fulfill our desires” o “the drive to mastery (misses) and may even destroy is an appreciation of the gifted character of human powers and achievements” o appreciation for giftedness of life gives humility o its is in part religious, but not wholly hubris objection o “moral problem w/ enhancement lies less in the perfection it seeks than in the human disposition it expresses and promotes” o ex we would find severe genetic alterations of animals to be troubling if we are not causing suffering, whats the problem? “represents ultimate human dominion” troubling b/c all life “is a gift not subject w/o limit o our mastery or dominion” analgous distinction is beholding and molding the world conclusion: problem w/ genetic “enhancement is that it represents the triumph of willfulness over giftedness, dominion over reverence, molding over beholding” D4. Explain Behar’s & Sandel’s respective positions on genetic enhancement in sports & the ethical norms to which they appeal. Gene doping – non-therapeutic use of genes, genetic elements, and/or cells that have the capacity to enhance athletic performance. Behar believes gene therapy is on the rise and more and more athletes who will do anything to win will be using it. IGF-I gene drives muscle growth and repair. Gene doping is hard to spot. The only way to prove someone has had gene doping is to biopsy suspicious muscle and look for signs of DNA tampering. Most athletes obviously would not let doctors take bits of flesh from the muscles they worked so hard to develop. Sandel believes what is troubling about enhancement is that it represents the focus on human will rather than what was naturally gifted. It is morally troubling and diminishes humanity. With genetic enhancement, an athlete’s performance does not represent his achievement, but instead his pharmacist’s drugs. Genetic enhancement causes the “erosion of human agency.” D4. Explain Behar’s & Sandel’s respective positions on genetic enhancement in sports & the ethical norms to which they appeal. Behar: o New technology that can create genes that have the ability to repair weak or damaged muscles, bones, etc. and increase strength and size of normal muscles in a short period of time o enticing to athletes to perform better and be stronger o o o o International Olympic Committee and most professional sports organizations prohibit gene doping “nontherapeutic use of genes, genetic elements and/or cells that have the capacity to enhance athletic performance” Gene doping is different from steroids because it cannot be easily detected since gene doping becomes a part of the DNA Effects of gene doping are uncertain Possibly make precancerous cells grow faster and stronger The virus that serves as carrier could be deadly Will be hard to distinguish between healing injuries and enhancing performance Athletes cannot succumb to temptation of unnaturally altering bodies (ethical norm) Sandel: o Genetic enhancement is troubling because athletes are seeking improvement at cost of medical risk o Our capacity to act freely and to consider ourselves responsible for our actions is being threatened Achievements cannot be admired when they’ve been aided by enhancement because performance was not a result of hard work and dedication o will cause people to change human nature to serve our purposes and satisfy our desires people have to be able to recognize that not everything in the world is open to any use we may desire (ethical norm) D5. According to Parker & Lucassen, what are the advantages of viewing genetic information as a joint account? joint account model genetic info is shared by more than one person advantages: o favored by justice/reciprocity o benefits gained and harms avoided o consistent w/ clinical genetic practice justice/reciprocity o “strongest ethical principle in favor of the joint account” o genetic info is familial by very nature o benefits>harms o when you go to counseling, you provide a detailed family history, often w/o the consent of the other family members o b/c of this, there is no reason why 1 member should be able to benefit while excluding others from the benefits benefits gained and harms avoided o ppl who may benefit from knowing their genetic history are unaware of their need to be tested o when ppl develop a genetic disorder and find out that a family member knew about it, they may lose trust in their drs consistent w/ nature of practice in clinical genetics o b/c genetic counselors often work w/ families, allowing them access to everyone’s info would make it easier for them o offers possibilty o in order for geneticists to benefit patients the most, need to know familial information to provide most comprehensive care (when there is no risk of serious harm to patient and family) D5. According to Parker & Lucassen, what are the advantages of viewing genetic information as a joint account? -assumed that info should be available to all account holders unless there are good reasons to do otherwise -storage of genetic information of relevance to other family members in account can help construct family histories. -reciprocity: genetic info is unavoidably familial in nature -families can benefit from genetic testing and diagnosis -consistent with nature of practice in clinical genetics...geneticists work with families. D5. According to Parker & Lucassen, what are the advantages of viewing genetic information as a joint account? Joint account: one type of model over genetic information; genetic information as essentially familial; presumption for disclosures, unless major harms to individual which then, individual has right to withhold information from other family members o based on justice/reciprocity no reason why one family member should be able to benefit and also be allowed to exclude others from access to benefits o based on benefits to be gained and harms to be avoided strict confidentiality doesn’t allow for all possibilities and options to be explored if patients were to find out physicians were withholding information, loss of trust to medical community o consistent with clinical genetics in order for geneticists to benefit patients the most, need to know familial information to provide most comprehensive care (when there is no risk of serious harm to patient and family) D6. Differentiate the uses of pre-implantation genetic diagnosis (PGD) and Robertson’s assessment of them. Preimplantation genetic testing is a technique used to identify genetic defects in embryos created through in vitro fertilization (IVF) before pregnancy. Preimplantation genetic diagnosis (PGD) refers specifically to when one or both genetic parents have a known genetic abnormality and testing is performed on an embryo to see if it also carries a genetic abnormality. In contrast, preimplantation genetic screening (PGS) refers to techniques where embryos from presumed chromosomally normal genetic parents are screened for aneuploidy. Preimplantation genetic diagnosis (PGD) is recommended when couples are at risk of transmitting a known genetic abnormality to their children. Only healthy and normal embryos are transferred into the mother's uterus, thus diminishing the risk of inheriting a genetic abnormality and decreasing the risk for adverse outcomes such as early and late miscarriage and late pregnancy termination (after positive prenatal diagnosis). The ethical acceptability by Robertson is consistent in most cases, when the ultimate decision is carefully balanced against personal bias. Whereas the article proposes to analyze the ethical controversy of embryo selection, Robertson presumes that embryos do not have rights, but protective value. Robertson includes speculative scenarios, including selection based upon possible sexual orientation and hearing ability. The author concludes that except for sex selection of the first child, most current uses and extensions of PGD are ethically acceptable, and believe that future nonmedical purposes could be reasonable. Even in situations where the child is screened to provide medical benefit of a sibling, he proposes that this situation doesn’t preclude the child from having a happy life and the knowledge that he/she was responsible for saving their sibling’s life. The ethical issue of discarding embryos and the topic of selection are addressed early in the article, but the author easily dismisses these concerns, believing that medical diagnosis is primary in importance. The concern for future abuse through the selection process and the possibility of designer children is noted as a concern for future regulation and public policy. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) Testing modalities include diagnostic testing (e.g., confirmatory tests for Huntington's Disease); pre-symptomatic testing for individuals (e.g., BRCA1); pre-natal testing (e.g., amniocentesis to detect trisomy 21); pre- implantation testing of embryos; and population screening (e.g., for Tay-Sachs). Persons being tested (or, in the case of an embryo, fetus or child, the parents) aren't the only people with an interest in the test results. Family members and potential mates, employers, insurers, the press (in the case of a celebrity) and the government all may desire information about a person's genetic endowment, and their interests may have nothing to do with -- or be antithetical to -- the welfare of the patient. One issue that arises is whether a physician or other health professional providing genetic testing services should be permitted without the patient's consent or over their objection to reveal test results (or even the fact that a patient has sought genetic counseling or testing) to third parties. The rule is no different than for medical information in general: confidential information that can be linked to an identifiable patient should be disclosed without the patient's authorization only when necessary to protect third parties from harm or when disclosure is compelled by law (e.g., reporting HIV test results to public health officials). When is disclosure of genetic information permitted in order to protect third parties from harm? For example, can a physician over the patient's objection reveal a positive test result for an inherited disorder to the patient's children, on the ground that disclosure is necessary to enable the children to protect themselves (e.g., by prophylactic treatment or more frequent diagnostic screening) or to prevent the disorder from being passed on to others (e.g., by not conceiving or by testing and aborting an affected fetus)? This is the subject of significant debate within the bioethics community, but the consensus at this time seems to be that the information should not be disclosed over the patient's objection and that the exception to protect third parties should be interpreted narrowly to extend only to a situation in which disclosure would enable third parties to obtain treatment or prevention to avoid fairly immediate, serious health consequences. Privacy is the ability of an individual to have control over access to him/herself. In the case of genetics and genetic testing, the individual has the right to privacy over information relating to the results of genetic testing (informational privacy) because the information has the ability to be stigmatizing and can create an atmosphere of discrimination. Confidentiality is a surrender of privacy by granting access to personal information, but we usually retain some control over the information. This information is not accessible to “others” without authorization of release by the individual. Confidentiality infers a special relationship. Medical confidentiality provides that when a person discloses information to their physician, the information is private and cannot be revealed because of it would be a violation of their rights to privacy. The exceptions are generally never genetic in nature, but related to a crime (gunshot wound) or a communicable disease, such as a venereal disease. However, when genetic information involves an at-risk circumstance that can be fatal to a family member or can prevent harm, then the physician must assess if there is a reasonable way to avert the harm. Nevertheless, the default is non-disclosure without permission. D6. Differentiate the uses of pre-implantation genetic diagnosis (PGD) and Robertson’s assessment of them. PGD used to screen embryos in assisted reproduction for chromosomal abnormalities before transfer o Should consult with ethics and research committees Direct examination of specific sections of the genome for mutations o No ethical issues in this, should be allowed To avoid the birth of children who are healthy at birth but face a higher than average risk of having cancer or other serious disease For late onset conditions such as Alzheimer’s disease, to free child of that condition o Ethics question is whether physicians act properly when they enable a woman/couple to have a child knowing that the child may soon lose one parent to disease o Believes it is mostly acceptable because they don’t want to cause unnecessary suffering to child Nonmedical sex selection, to serve parent interests in having a healthy child of a particular gender o sex selection justified if for example in a society where child would be aborted if it was not a male For other nonmedical traits such as hearing, sexual orientation, height, beauty, intelligence, or other factors o Too soon to reach definitive judgments about whether these uses would or should be permitted D6. Differentiate the uses of pre-implantation genetic diagnosis (PGD) and Robertson’s assessment of them. Uses: -screen embryos for aneuploidy (abnormal number of chromosomes) and genetic diseases Possible future uses: -susceptibility to cancer, late-onset disease screening, HLA-matching for existing children (tissue testing for blood transfusions, organ donation, blood marrow donation), gender testing Assessment: -current use of PGD to screen for aneuploidy and serious Medelian disorders is ethically and legally acceptable when performed according to applicable regulatory guidelines -PGD is acceptable to prevent having offspring with serious genetic disorders -controversial issue: PGD for gender selection, hearing, sexual orientation and other non-medical traits D6. Differentiate the uses of pre-implantation genetic diagnosis (PGD) and Robertson’s assessment of them. Pre-implantation genetic diagnosis (PGD) – technique by which early human embryos are genetically screened and then discarded or placed in the uterus – as a reproductive practice that needs close ethical, legal, and social scrutiny Uses of PGD: o Traditional: screening for aneuploidy and genetic disease o New: susceptibility to cancer or other conditions, late-onset diseases, HLA-matching for existing children, and for gender The most common use of PGD is to screen embryos in assisted reproduction for chromosomal abnormalities before transfer. PGD offers the alternative of screening embryos rather than fetuses, thus avoiding the need to terminate a pregnancy in order to ensure an unaffected child Ethical issues in current and expanded uses of PGD Objection #1: effect on embryos (creating, selecting, discarding) – does it sufficiently benefit important human interests to meet the demands of special respect for embryos that supporters of PGD may require Objection #2: selection itself (risks of greatly expanding future selection of embryos and children) o Deontological concern - Wrong to choose traits of offspring, no matter how was intentioned (reproduction is a gift and any form of selection or manipulation turns the child into manufacture; impairs human flourishing) o Consequentialist concern – fear that increasing the frequency and scope of genetic screening will move us toward a eugenic world in which children are valued more for their genotype than for their inherent characteristics --- world of “designer” children where engineering is routine Robertson: while recognizing the strong objections of some people to PGD on these grounds, he believes the use of PGD to screen for aneuploidy and serious Mendelian disorders is ethically and legally acceptable when performed according to applicable regulatory guidelines. He concentrates on new indications for PGD, questioning ethical standards. Aneuploidy – a cause of spontaneous abortions; PGD looks for chromosomal abnormalities via karyotyping; only ethical concerns arise if programs/institutions are unequipped to do these procedures properly while offering them to patients. Need for careful patient selection and consultation. Mendelian Diseases – PGD allows for direct examination of specific sections of the genome for mutations which lead to diseases such as Tay Sachs, cystic fibrosis, sickle cell anemia, Duchenne muscular dystrophy, and hemophilia. At-risk couples (carriers of these mutations) would go childless, adopt, or use donor gametes. Or, they would have prenatal testing once pregnant and then abort if the results were not good. PGD offers alternate of screening embryos rather than fetuses, thus avoiding the need to terminate a pregnancy in order to ensure an unaffected child. PGD to screen out embryos affected by these serious diseases raises no ethical issues beyond those that arise with prenatal diagnosis and selective termination of pregnancy. Some may find PGD preferable b/c of the undeveloped state of the embryo vs. the fetus. PGD for susceptibility conditions Extension beyond Mendelian disorders to avoid births of children who have higher risk of having cancer or some other serious disease. (Examples include screening of p53 and BRCA1 and 2 mutations). Are the burdens to the parents and child that great to justify these means? Robertson says if one accepts that embryos lack rights and interests but deserve special respect, then a plausible case for permitting PGD for this purpose exists. Creating and destroying embryos to have a healthy child is not treating embryos frivolously. o The fact that the disease state does not occur until much later in life, unlike other Mendelian disorders, should not be morally significant. A child susceptible to cancer or other disease could be a major source of suffering for parents and child. o PGD for susceptibility conditions is legal in the United States. Chief legal restriction on susceptibility testing at present may come from patent holding (ex. BRCA1 gene screening for breast cancer only done by Myriad Corp. in Utah) PGD for late-onset conditions Alzeimer’s Disease or Huntington’s Disease Woman w/ Alzheimer’s Disease – used PGD to have child free of that condition o Justifiable to screen out gene, especially when it is not preventable o Ethical twist – ability of the affected parent to raise the child; child will lose parent while it is still dependent on it for support/upbringing o Did physicians act properly? If they deny to her, then have to deny to HIV or cystic fibrosis or cancer candidates as well. Even if the child loses one parent, another parent is almost certain to be present to take care of the child. The child could not otherwise be born but with the risk… psychological trauma of dealing with death of parent doesn’t make life so full of suffering or w/out clear benefit that one is harming the child by enabling its birth. PDG for HLA matching for an existing child Hematopoietic stem cells from umbilical cord of new child used for stem cell transplant of previous child. PDG advantageous b/c can transfer to uterus disease free and of HLA type match o Different from others b/c done wholly or in part to choose embryos that will enable the resulting child to serve as an HLA-donor for an existing child. o Distinction should not matter morally b/c child will not be any less loved; its birth might save the life of an existing, loved child; if the transplant fails, the parents will have another child to love. HFEA: Only ethically acceptable to use if screening b/c known genetic link to second child (not, for example, leukemia/lymphoma that can come about on its own.) o Prudent step to ensure that expanded uses of PGD occur slowly, but should reconsider ruling since screening for closeness of HLA match serves a substantial family need and is not abusive or commodifying of resulting children. PGD for gender selection Serves parental interests in having a healthy child of particular gender o Select for 1st child of specific sex (usually male), OR o Select for an additional child of different sex Highly controversial, but since PGD isn’t likely to be highly/widely used, the first child scenario is only marginally likely to contribute to those disparities in the sex ration of the species. Use for 1 st child is likely to reflect culturally-founded sexist notions. 2nd case is much less susceptible to sexism charges if used to have opposite-gendered child. Couple seeks a balance in the gender of offspring. Feminist arguments – o Any attention to gender in inherently sexist, particularly when social attitudes and expectations play such an important role in constructing sex role expectations and behaviors. o Some find it defensible as long as the intention and consequences of the practice are not sexist Just b/c parents want to rear a child of another sex, doesn’t mean they are inherently sexist or devalue one gender over the other. They just want the different experience. Verdict: Case not strong for allowing PGD for first child cases, but may be acceptable for gender variety in families (where risk of sexism is lessened). Even so, is there a strong enough reason for creating and discarding embryos for this reason? o Depends on how strong the interest is o Only have another child if they could control what sex that child would be (opposite of existing) o Legitimacy of wanting to raise children of both genders… need outweighs symbolic cost of creating and destroying embryos for that purpose o Countries such as India where it’s so culturally important to have male heir; would have aborted fetus if it was a girl, even though this is illegal. o Overall, creating baby that would have not otherwise been born. PGD for nonmedical traits Hearing, sexual orientation, height, beauty, intelligence, or other factors became available… but have strong influence of environment and learning, so probably low chance to really know for sure. Deafness mutations – o screen out deafness gene; ethical concern with prejudice to deaf community. o Screen FOR deafness; ethical issue is whether having a deaf instead of a hearing child would have hurt that child; acceptable when strong commitment to well-being of child and the rich culture now available to deaf people (ex. lesbian couple story) Sexual orientation – similar concerns Lead to more drastic efforts at selection and alteration of offspring traits? Most of these tests are too far off in the future, if ever feasible… until more of a reality, shouldn’t be important issue of accepting PGD Making public policy for PGD No effective oversight in many countries --- potential for misuse of embryo screening and selection HFEA exists in UK to tightly regulate PGD and draw up guidelines based on public consultation process US – much different. No agency exists at the state or federal level comparable to HFEA. Congress exercises some control by refusing to fund research or use of PGD…. How PGD is used and for what indications is left largely to the discretion of providers offering those services and the patients who seek it. CONCLUSION PGD is increasingly available for aneuploidy in low prognosis IVF patients and for single gene mutations that cause genetic disease, susceptibility to cancer, and late-onset disorders. If PGD is acceptable to prevent offspring with serious genetic disease, then these additional uses should be acceptable as well. There is also ethical support for using PGD to assure that a child is an HLA match with an existing child. More controversial is the use of PGD for gender selection, particularly for the first child. Equally controversial would be its use to screen embryos for hearing, sexual orientation, and other nonmedical traits – uses that are highly speculative. Need for careful ethical analysis and open public debate when considering new uses of PGD. D6. Differentiate the uses of pre-implantation genetic diagnosis (PGD) and Robertson’s assessment of them. Pre-implantation genetic diagnosis (PGD) is a method to screen embryos for aneuploidy and genetic diseases, and more recently to screen for susceptibility to cancer, for late-onset diseases, and for gender, prior to implantation. It is beneficial in that it helps to avoid the practice of selective pregnancy termination, because after screening it is highly likely that the baby will be free of the tested diseases. PGD is mainly used for two groups of people; those couples with a high risk of transmitting and inherited condition, and those couples who undergo IVF and whose embryos are screened for aneuploidies. Robertson, in "Extending pre-implantation genetic diagnosis: the ethical debate", reveals ethical issues that arise from PGD and its current extensions. Robertson first raises two main concerns; the issue of the status of the embryo (referring to concerns of discarding the unwanted embryos) and the issue of the risks of future selection of embryos and how it maybe be "wrong" to choose traits and how it might lead to a eugenic world. He moves past these issues to discuss several innovative uses of PGD and the ethical concerns associated with them. The first use of PGD he discusses is for assisted reproduction, for screening embryos for chromosomal abnormalities before transfer. He believes that this is a beneficial practice and believes that is raises "few ethical concerns" (467). He also delves into the examination of specific sections of the genome for mutations. He argues for this use, on the grounds that it screens embryos rather than fetuses, thus avoiding the need to terminate a pregnancy in order to ensure an unaffected child. Many prefer this, because of the undeveloped state of the embryo compared to the fetus. Another use of PGD he brings up is the ability to screen for risks of late-onset diseases. He believes the "ethical twist" in this situation is not the fact that the child may develop these diseases in their 30s and 40s, but the issue of the parent's ability to raise the child. But he concludes that we cannot condemn parents who use PGD in this situation, because they are trying to avoid unnecessary and undo suffering in their offspring. PGD for matching for an existing child is another use. Parents may have a child to provide stem cells to another child, and PGD allows for the transfer to the uterus of only embryos free of the disease in the existing child. He sees two benefits in this use; one, the new child may be able to save the life of the existing child and two, even if the existing child doesn't survive, they will have a new child to love. A controversial use of PGD is gender selection. This is less of a compelling argument, because it is less medical procedure. It has received criticism for being a sexist practice, and has conjured worries about the potential imbalance of genders if this were to become a norm. Robertson condones the practice if the use is for providing gender variety in the family. The final use that Robertson brings up is PGD for nonmedical traits (hearing, sexual orientation, height, beauty, intelligence, etc). Robertson believes it is too soon to reach definitive judgments for these uses. D6. Differentiate the uses of pre-implantation genetic diagnosis (PGD) and Robertson’s assessment of them. o PGD – the technique by which early human embryos are genetically screened and then discarded or placed in the uterus (has been available since 1990) Successful, but intrusive, expensive and raises serious ethical concerns and therefore only sought if there is sufficient reason to do so (advanced maternal age; special risk for genetic disease – want to have child without risking an affected pregnancy or later abortion) Might lead to use for sex selection (but demand will remain a small percentage of people using it) o Two Ethical Issues: o o 1. People who think fetus is a person will object to creating and destroying embryos (oppose PGD); (also those who thing fetus deserves special respect as first stage toward a new person) 2. Fact of selection itself; ethical judgment that it is wrong to choose traits of offspring. Human reproduction is a gift and any form of selection turns child into manufacture (designer children) Expanded uses of PGD and assessment of them Screen embryos in assisted reproduction for chromosomal abnormalities before transfer (most common use) – exclude aneuploid embryos from transfer Raises few special ethical issues beyond use of IVF itself and discard of embryos PGD for Mendelian Disease: screening embryos rather than fetuses (avoiding need to terminate pregnancy) for Tay Sachs, sickle cell, cystic fibrosis and other serious diseases No ethical concern issues beyond those that arise with prenatal diagnosis and selective termination of pregnancy PGD for Susceptibility Conditions: use to avoid the birth of children who are healty at birth but face a higher than average risk of having cancer or some other serious disease If one accepts that embryos lack rights and interests, but deserve special respect than this is morally permissible. Creating/destroying embryos to have healthy child is not using embryos in frivolous way and shows respect for embryos. Fact that disease doesn’t occur later in life does not matter – still could be major source of suffering for parents and child PGD for susceptibility conditions is legal in US PGD for Late-Onset Conditions: Parent who has condition that sets in late in life wants to make sure child will not inherit disease (Alzheimer’s disease) Ethical issue is whether physicians act properly when they enable a couple to have a child knowing that the child may soon lose one parent Fact of shortened life span makes reproduction all the more pressing – denying reproductive services would require denying services to individual (or individual’s partner) who has other issues that might shorten life span (HIV, cystic fibrosis, cancer) Not fair to condemn parents or (doctors who help them) who reproduce when one parent might die soon. Though death of a parent causes trauma it does not make a life so terrible that one is harming child by enabling his/her birth. PGD for HLA Matching for an Existing Child: Used by parents who have one sick child and wish to have another whose umbilical cord blood would serve as a source of stem cells; screening assures that child born will be free of the disease first child has and be HLA match to existing child. Although having sick existing child is motivating factor to have additional child, it is not likely to make the parents ignore the needs of new child Birth would save life of existing child which would increase its specialness (if stem cell transplant fails then parents will have new child to love) Whether or not the embryo is at risk for disease which stem cells are sough, screening for closeness of HLA match for an existing sick child serves a substantial family need and is not abusive to resulting child (should be allowed) PGD for Gender Selection: two uses (1) by parents who want to select gender of first child (2) by parents who already have a child of one gender and wish to have another of the opposite gender. (1) use for selection of first child is likely to reflect culturally founded sexist notions (2) use to select sex of second or subsequent children is much less susceptible to charge or sexism (if use to select gender opposite to that of existing child) some feminist might argue that any attention paid to gender is sexist; some say it is okay as long as intention is not sexist Supreme Court view – desiring different rearing experience that comes with boys and girls does not make parents sexist Case 1 not strong case for using PGD; promotes sexist social mores Case 2 may be acceptable for gender variety in family (selection would enable a couple to have a child they would not otherwise had – goal served in other cases of embryo screening) PGD for Non-medical Traits: ex. hearing, sexual orientation, height, beauty, intelligence etc Too soon to reach definitive judgments about whether these uses, if ever feasible, would or should be permitted tests are too far off in the future to make informed judgments Public Policy: In US congress has some control and a few states have laws but mainly how PGD is used and for what is left largely to discretion of providers offering those services and the patients who seek it D7. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) Arguments for genetic testing: Genetic testing situations considered: screening for late-onset conditions, for HLA-matching for tissue donation to existing child, and for gender selection. Only a small number of people using assisted reproduction, and thus a much smaller of people aoverall who reproduce, are likely to use PGD (preimplantation genetic diagnosis) to screen embryos. Under view that embryos are to rudimentary to have rights but deserve respect, PGD would be justifiable in most respects except for gender selection of a first child. Parents have a strong, interest in having children who will be healthy and not face the burdens for continued monitoring, prophylactic surgery, or other preventive actions. For late onset patients: ethical implication of late onset is negligible – ethical twist is that the parents’ ability to raise the child will be impaired since the parent now has a late-onset disease. In the case of allowing PGD for sex selection of second or subsequent children: it is less susceptible to a charge of sexism since the parents seek balance and variety. On the basis of deafness: deafness is considered as distinct from most disabilities because there is a strong deaf community which demands respect and perceives deafness not as something negative, but as a positive, inherent trait of its community. Parents feel they can raise and connect with a deaf child better and, through personal experience, do not see deafness as being universally inhibitory. D7. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) Arguments against genetic testing: Against the need to create and select embryos on chromosomal or genetic grounds with the deselected embryos usually discarded. Against the fact of selection itself Argue that human reproduction is a gift and that any form of selection or manipulation turns the child into a manufacture and thus impairs human flourishing. Increasing the frequency and scope of genetic screening of prospective children will move us toward a eugenic world in which children are valued more for their genotype than for their inherent characteristics. In the case of allowing PGD for sex selection, sex selection of the first child would heavily under the criticism of sexism. In the case of allowing PGD for sex selection of second or subsequent children: When social attitudes and expectations play such an important role in constructing sex role expectations and behaviors, selecting on the basis of gender is inherently sexist since parents expect something of the child because of its sex. On the basis of deafness: it is a case of human rights not deaf rights. Deafness imposes a limitation on the child that is irreversible, unlike race. Parents do not have the right to make a child deaf on the basis of their interests. General arguments against genetic testing: It represents a drive to mastery which negates the view of life as a gift and begins to remove the human willingness to behold instead of to mold. The problem lies in the hubris of the designing parents which disfigures the relation of parent and child. Genetic testing approaches eugenics in that in demonstrating the willingness to eliminate individuals with unwanted diseases, we create a mind-set that justifies the process of human selection. We move into the questionable arena of human worth, and to some degree eugenic thought. Other factors in genetic testing: Balancing benefits and harms, costs and burdens Providing equitable access Preventing various forms of genetic discriminations in health insurance or in employement Privacy vs. Confidentiality: The difference between privacy and confidentiality is that privacy involves information which the individual has the right to choose not to disclose and confidentiality involves information which has been disclosed to a third party which then commits to only disclosing that information with the individual’s consent. There are calls for genetic privacy in which genetic information which could be susceptible to common stigmatizations is rightfully the patient’s to disclose. The problematic metaphor of as genetics as a “future diary” increases the worries of public genetic information. – B &C conclusion: since other medical information provides information similar to what would be gained by genetic tests and may also be stigmatizing, public policies should address the privacy of medical and health information in general, and then add protections for genetic information only if needed. Justified infringements of rules of confidentiality: Assessing and reducing risks to others is essential to understanding when to disclose information and break with rules of confidentiality. Criteria for assessing risks to others include the magnitude of the harm and the probability of the harm. EX: Disclosure of HIV infection to third parties D7. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) PROS -vast increase in knowledge of human biology – improve and create cures to, or even prevent, genetic diseases -Pharmacogenetics: (the study of genetic variation that affects response to medicines) people have variable responses to the same drug, and some of this variation stems from their genetic differences – improving safety and efficacy CONS - Playing God -Two senses: unlimited power to decide and unlimited power to act, including creating new life forms (prenatal testing might lead to abortion, etc.) -Theological ideas in support of human genetic engineering (at least within limits). E.g., creation of humans in the image of God, etc. -Concern about the unpredictability of consequences and uncertainty in their evaluation - slippery slope arguments (Brave New World) -From correction of diseases to enhancement of qualities. -non-genetic intervention of human growth hormone. -Genetic enhancement in sports—major concern -From somatic cell to germline interventions -Loss of control: Nazi Germany, the Lynchburg story - Reprogenetics - Pre-implantation Genetic Diagnosis (Specialists analyze for chromosomal abnormalities, clients can select embryos free of certain diagnosable genetic conditions/diseases) -Selection of embryos free of diseases—but which diseases? What about late-onset diseases? -Selection of embryos who could be a matched source of cord blood or bone marrow for transplantation to a sibling -Sex selection -"reification" of racial/ethnic categories as genetic? - use of race as genetic criterion is scientifically problematic & ethically problematic, genetic variation w/in racial groups overlaps w/ other groups - gene transfer & therapy experiments – not complete success and has led to test patient deaths - Other ethical issues in genetic testing & screening Balancing benefits and harms, costs, and burdens, Providing equitable access Preventing various forms of genetic discrimination (e.g., in health insurance or in employment). Parental decisions to test children – how would we set limits? Privacy: state of limited access to a person Different meanings and kinds of privacy – informational, decisional, etc. Privacy as a state distinguished from a right to privacy – emergence of legal right to privacy in U.S. constitutional law (contraception & abortion decisions) Confidentiality: Definition: Relationship in which the source of information controls access, by third parties, to that information When is a breach of confidentiality ethically justifiable? conditions for overriding prima facie obligations: if one person's genetic information will help or even save another's life, is it ethical for them to request to keep that information private? (i.e. hereditary disease, organ and tissue transplant compatibility, etc.) D7. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) Genetic testing is directed at individuals after problems have arisen, while genetic screening is directed at populations. TYPES of genetic testing/screening o VOLUNTARY – most genetic testing (prenatal – problem of abortion) o MANDATORY – newborn screening (within limits) – calls for expanse but debate regarding conditions for screening – parental right to opt out? Reprogenetics – the case of pre-implantation genetic diagnosis (PGD) – See Robertson in packet Advocates main arguments FOR PGD (and the Counterarguments) – From Kilner Avoids need to abort children later who are not well-matched or suited to parent’s liking. o PGD offers the alternative of screening embryos rather than fetuses, thus avoiding the need to terminate a pregnancy in order to ensure an unaffected child. o Counter: either way, the same human being dies… shouldn’t matter, no improvement. Various risks of the procedure to the child (physical and psychological) can be mitigated (monitor procedures and offer counseling) o Counter: But, allowing PGD to go forward constitutes experimentation on children (unacceptable) The “public” “supports” the process o Counter: 60% support doesn’t make the process right… if it did, ethics is nothing more than determination by public opinion w/out respect for fundamental truths and rights Main Arguments AGAINST PGD – from Kilner Using PGD as method of weeding out undesirable offspring is unethical by its very nature o Most of the time the goal is to avoid passing on genetic disease, though PGD is sometimes used for gender selection or selecting children with other traits as well. But even if for admirable goals (avoid diseased baby), end up creating humans and throwing away those that don’t measure up… they don’t have enough value to justify their existence. o Kid is only loved b/c they don’t have some unwanted problem; what about when a problem pops up in life? Will parents be willing to deal? o What about those who are disabled in our society? Embryos are entire beings, not merely cells, and human embryos are accordingly human beings. o Scientific basis of genetics – beings will a full human genetic code o Biblical basis – image of God is present in living beings o Status is still debatable and uncertain, so we should protect them anyhow ***Should not engage in behavior that could be harmful to those who might be human beings. o PRIVACY – state or condition of limited access to a person Different meanings and kinds: informational, decisional, etc. Privacy as a state distinguished from a right to privacy o Emergence of legal right to privacy is US constitutional law (contraception and abortion decisions) o Debates about this right – should it be extended to death and dying? CONFIDENTIALITY – relationship in which source of information controls access, by third parties, to that information Widespread across cultures in medical ethics – more so than other principles When is breach of confidentiality ethically justifiable? Look at conditions for overriding prima facie obligations o Competing principle or rule is stronger in the situation Ex. Woman with AIDS won’t tell husband; doctors wants to prevent severe harm to male, but also has duty of confidentiality (Nonmaleficience takes priority over confidentiality) o Infringement of one principle will probably protect the other o This infringement is necessary to protect the other principle o The infringement is the least possible in the circumstances to protect the other principle o The agent must seek to minimize the negative effects of the infringement o The agent must act impartially with regard to all affected parties Control over information: bank account analogy (see Parker and Lucassen in packet) o Personal vs. joint account o Privacy concerns: access and uses of genetic information o In cases where foreseeable harms of disclosure or non-disclosure are serious, the two models agree. D7. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) Genetic testing is a controversial issue and has a great deal of support as well as opposition. Genetic testing allows for the genetic diagnosis of vulnerabilities to inherited diseases. Many critics believe that genetic engineering is the "mortal man's feeble attempt to play God in order to create the perfect child" (256). They fear the future of eugenics and 'designer babies'. Others view this technology as a blessing as to prevent avoidable suffering and harm to offspring. Confidentiality is fundamentally an issue of who is to control the dissemination of certain information. Typically the physician promises not to reveal information about the client without consent, yet issues arise when protecting this confidence infringes on the rights of others or would cause general social harm. Privacy focuses on an agent's control over access to himself, but this definition confuses the concept of privacy and an agent's control over privacy. In B & C, 4 types of privacy are defined; informational privacy, physical privacy, decisional privacy, and proprietary privacy. Loss of privacy can stem from the kind and extent of access to something private, or who, through what means, has access. The issue of privacy and confidentiality arises in Parker and Lucassen's artcle, Genetic Information: a joint account?". The case involved Helen Cross, an individual whose 4 year old son was just diagnosed with Duchenne's muscular dystrophy, and Helen's sister Penelope who was ten weeks pregnant and worried about implications. Helen wanted her information to be private and confidential, yet the doctor was torn due to the fact that this would potentially harm Penelope's child. The article suggests a "joint account" model, in which the information of genetic testing becomes open to the entire family. In this system, the patient would have to be at risk of serious harm to not share information, and it would extend the benefits of testing when there was no serious harm to index patients or their relatives. D7. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) o Pro Genetic Testing: can help identify genetic disorders early on and thus lead to preventative measures for individuals who might be at high risk, can help families make difficult decisions about child birth (know chances child has of inheriting disease) o Con Genetic Testing: fear that it might lead to social stigmatization if information is leaked, lead to practice that only those with good genes should reproduce (eugenics), promotes genetic determinism (George Annas and genetic diary greatly oversimplified) o Privacy: state or condition of limited access to a person; it is a state (distinguished from a right to privacy) o Confidentiality: branch/subset of informational privacy (prevents re-disclosure of information originally disclosed within a confidential relationship); relationship in which source of information controls access by third parties to that information. Only the person or institution who obtains information in a confidential relationship can be charged with violating rights of confidentiality. Note that there has been a general decline of confidentiality due to need for quick and efficient access to information o Genetic Testing: practice brings up issue of privacy and confidentiality and who should have/be given access to genetic information and when Confidentiality should be breached and relative informed about genetic risks when (1) attempts to elicit voluntary disclosure fail (2) there is high probability of fatal harm to relative (3) disclosure of info will prevent harm (4) disclosure is limited to information necessary (5) there is no other way to avert the harm Person/Individual Account vs. Joint Account Personal account: genetic information as personal, based on respect for autonomy and trust, consistent with medical practice, sometimes right to breach confidentiality (see above 5 conditions). B&C support this view o Ethical justification arises out of respect for patient choice Joint Account: genetic information as essentially familial, based on justice or reciprocity ad benefits to be gained, consistent with clinical genetics, presumption for disclosure (unless major harms to individual) o Ethical justification arise out of respect for justice or reciprocity D7. Explain the reasons for and against genetic testing, as well as the distinction between privacy and confidentiality, and how these norms relate to genetic information. (Also discussed under Public Health) Testing modalities include diagnostic testing (e.g., confirmatory tests for Huntington's Disease); pre-symptomatic testing for individuals (e.g., BRCA1); pre-natal testing (e.g., amniocentesis to detect trisomy 21); pre- implantation testing of embryos; and population screening (e.g., for Tay-Sachs). Persons being tested (or, in the case of an embryo, fetus or child, the parents) aren't the only people with an interest in the test results. Family members and potential mates, employers, insurers, the press (in the case of a celebrity) and the government all may desire information about a person's genetic endowment, and their interests may have nothing to do with -- or be antithetical to -- the welfare of the patient. One issue that arises is whether a physician or other health professional providing genetic testing services should be permitted without the patient's consent or over their objection to reveal test results (or even the fact that a patient has sought genetic counseling or testing) to third parties. The rule is no different than for medical information in general: confidential information that can be linked to an identifiable patient should be disclosed without the patient's authorization only when necessary to protect third parties from harm or when disclosure is compelled by law (e.g., reporting HIV test results to public health officials). When is disclosure of genetic information permitted in order to protect third parties from harm? For example, can a physician over the patient's objection reveal a positive test result for an inherited disorder to the patient's children, on the ground that disclosure is necessary to enable the children to protect themselves (e.g., by prophylactic treatment or more frequent diagnostic screening) or to prevent the disorder from being passed on to others (e.g., by not conceiving or by testing and aborting an affected fetus)? This is the subject of significant debate within the bioethics community, but the consensus at this time seems to be that the information should not be disclosed over the patient's objection and that the exception to protect third parties should be interpreted narrowly to extend only to a situation in which disclosure would enable third parties to obtain treatment or prevention to avoid fairly immediate, serious health consequences. Privacy is the ability of an individual to have control over access to him/herself. In the case of genetics and genetic testing, the individual has the right to privacy over information relating to the results of genetic testing (informational privacy) because the information has the ability to be stigmatizing and can create an atmosphere of discrimination. Confidentiality is a surrender of privacy by granting access to personal information, but we usually retain some control over the information. This information is not accessible to “others” without authorization of release by the individual. Confidentiality infers a special relationship. Medical confidentiality provides that when a person discloses information to their physician, the information is private and cannot be revealed because of it would be a violation of their rights to privacy. The exceptions are generally never genetic in nature, but related to a crime (gunshot wound) or a communicable disease, such as a venereal disease. However, when genetic information involves an at-risk circumstance that can be fatal to a family member or can prevent harm, then the physician must assess if there is a reasonable way to avert the harm. Nevertheless, the default is non-disclosure without permission. D8. Distinguish embryonic, pluripotent, totipotent, & adult stem cells. - embryonic stem cells – stem cells derived from an embryo that has been created through in vitro fertilization and donated for research. - pluripotent stem cells – stem cells which can give rise to all the various type of cells which can be found in the body. These stem cells are particularly valuable to scientists. - totipotent stem cells – stem cells which can give rise to all the cells which are found in the body and all the cells which are found in the placenta. - adult stem cells – undifferentiated cells which are derived from differentiated adult tissue and can develop into any type of cell that occurs within the differentiated tissue that it was derived from. D8. Distinguish embryonic, pluripotent, totipotent, & adult stem cells. Embryonic stem cells—Primitive (undifferentiated) cells derived from a 5-day preimplantation embryo that have the potential to become a wide variety of specialized cell types. Pluripotent—Ability of a single stem cell to give rise to all of the various cell types that make up the body. Pluripotent cells cannot make so-called "extra-embryonic" tissues such as the amnion, chorion, and other components of the placenta. Scientists demonstrate pluripotency by providing evidence of stable developmental potential, even after prolonged culture, to form derivatives of all three embryonic germ layers from the progeny of a single cell and to generate a teratoma after injection into an immunosuppressed mouse. Totipotent—A totipotent stem cell can give rise to all the cell types that make up the body plus all of the cell types that make up the extraembryonic tissues such as the placenta. Adult (or somatic) stem cell—An undifferentiated cell found in a differentiated tissue that can renew itself and differentiate (with certain limitations) to give rise to all the specialized cell types of the tissue from which it originated. It is important to note that scientists do not agree about whether or not adult stem cells may give rise to cell types other than those of the tissue from which they originate. D8. Distinguish embryonic, pluripotent, totipotent, & adult stem cells. Embryonic stem cells: as their name suggests, are derived from embryos. Specifically, embryonic stem cells are derived from embryos that develop from eggs that have been fertilized in vitro—in an in vitro fertilization clinic and then donated research purposes with informed consent of the donors. They are not derived from eggs fertilized in a woman's body. The embryos which human embryonic stem cells are derived are typically four or five days old and are a hollow microscopic ball of cells called the blastocyst. Adult stem cells: an undifferentiated cell found among differentiated cells in a tissue or organ, can renew itself, and can differentiate to yield the major cell types of the tissue or organ. The primary roles of the adult stem cells in a living organism are to maintain and repair the tissue in which they are found. Unlike embryonic stem cells, which are defined by their origin, the origin of the adult stem cells in mature tissues is unknown. Totipotent (aka omnipotent) stem cells can differentiate into embryonic and extraembryonic cell types. Such cells can construct a complete, viable, organism. These cells are produced from the fusion of an egg and sperm cell. Cells produced by the first few divisions of the fertilized egg are also totipotent Pluripotent: embryonic stem cells originate as inner mass cells within a blastocyst. The stem cells can become any tissue in the body, excluding a placenta. These stem cells are the descendants of totipotent cells and can differentiate into nearly all cells, i.e. cells derived from any of the three germ layers. D8. Distinguish embryonic, pluripotent, totipotent, & adult stem cells. Stem cells—Cells with the ability to divide for indefinite periods in culture and to give rise to specialized cells. o unspecialized cells that renew themselves for long periods through cell division. o under certain physiologic or experimental conditions, they can be induced to become cells with special functions such as the beating cells of the heart muscle or the insulin-producing cells of the pancreas. Embryonic stem cells—Primitive (undifferentiated) cells derived from a 5-day preimplantation embryo that have the potential to become a wide variety of specialized cell types. Embryonic germ cells—Pluripotent stem cells that are derived from early germ cells (those that would become sperm and eggs). Embryonic germ cells (EG cells) are thought to have properties similar to embryonic stem cells. Embryonic stem cell line—Embryonic stem cells, which have been cultured under in vitro conditions that allow proliferation without differentiation for months to years. Pluripotent—Ability of a single stem cell to give rise to all of the various cell types that make up the body. Pluripotent cells cannot make so-called "extra-embryonic" tissues such as the amnion, chorion, and other components of the placenta. Scientists demonstrate pluripotency by providing evidence of stable developmental potential, even after prolonged culture, to form derivatives of all three embryonic germ layers from the progeny of a single cell and to generate a teratoma after injection into an immunosuppressed mouse. Totipotent—A totipotent stem cell can give rise to all the cell types that make up the body plus all of the cell types that make up the extraembryonic tissues such as the placenta. Adult (or somatic) stem cell—An undifferentiated cell found in a differentiated tissue that can renew itself and differentiate (with certain limitations) to give rise to all the specialized cell types of the tissue from which it originated. It is important to note that scientists do not agree about whether or not adult stem cells may give rise to cell types other than those of the tissue from which they originate. D8. Distinguish embryonic, pluripotent, totipotent, & adult stem cells. Embryonic stem cells are stem cells derived from the inner mass of an early stage embryo known as the blastocyst. Embryos reach this stage 4-5 days after fertilization and are a mere 50-150 cells at this point. Embryonic stem cells are pluripotent. This means they have the ability to differentiate into any derivative of three different germ layers (ectoderm, endoderm, and mesoderm). These stem cells have amazing plasticity and potentially unlimited capacity for self-renewal, which is why these stem cells have been studies for regenerative medicine and tissue replacement. Totipotentcy is the ability of a single cell to divide and reproduce all the differentiated cells in an organism. These cells are produced during sexual reproduction, when two gametes fuse to form a zygote. This cell divides into totipotents cells, and after four days these cells begin to specialize. Adult stem cells are undifferentiated cells found throughout the body, which multiply by cell division and replenish dying cells and regenerate damaged tissue. They are also known as somatic cells. The use of these stem cells in research is much less controversial them embryonic stem cells, but don't have all the benefits that embryonic stem cells do. D8. Distinguish embryonic, pluripotent, totipotent, & adult stem cells. o Embryonic Stem Cells - pluripotent and give rise during development to all derivatives of the three primary germ layers; they can develop into each of the more than 200 cell types of the adult body when given sufficient and necessary stimulation for a specific cell type. o Pluripotent Stem Cells - stem cells are the descendants of totipotent cells and can differentiate into nearly all cells except those needed to develop a fetus. o Totipotent Stem Cells - stem cells can differentiate into embryonic and extraembryonic cell types. Such cells can construct a complete, viable, organism. A fertilized egg ( fusion of egg and sperm cell) is considered totipotent, meaning that its potential is total; it gives rise to all the different types of cells in the body. o Adult Stem Cells - undifferentiated cell found among differentiated cells in a tissue or organ, can renew itself, and can differentiate to yield the major specialized cell types of the tissue or organ. The primary roles of adult stem cells in a living organism are to maintain and repair the tissue in which they are found. (origin in mature tissues is unknown) D9. Compare and contrast the different religious perspectives on human embryonic stem cell research. Rabbi Elliot N. Dorff – Judaism does not consider the embryo to be of full human worth. As a result embryos taken from the body and used for the benefit of others or they can be culture by mixing eggs and sperm in a petri dish. Outside the body embryos have no worth. They can be discarded as well as the stem cells. Access to the technology must be balanced. Applications of research must be used for cure and not for enhancement. Edmund D. Pellegrino M.D. – First Roman Catholic Position – the fetus and embryo are treated with human worth. The Catholic position is opposed to the creation and destruction of embryos for research. It is opposed to the use of embryos taken from aborted fetuses if the act of termination life Is completely separate from the use of harvested cells because it views using the embryos would be like using data from an unethical human experiment since Catholicism is against abortion. It is opposed to using spares of in vitro fertilization because it argues that not all the spare embryos would be destroyed. It is against the conception of respect for the embryo on the basis of the value of the research conducted with the embryo since the respect is based on a condition other than its intrinsic value. It supports the funding and development of alternate sources of stem cells. Margaret A. Farley – Second Roman Catholic Position – Offers a new catholic perspective which interprets embryos in the earliest stages of development as deserving respect, but not entirely human. On this basis, stem cell research would be permitted on stem cells taken from embryos that are not entirely human. Gilbert C. Meilaender, Jr., Ph.D. – A protestant perspective – Communicates first the primacy of the belief that a society is not strong if it does not carry it weakest members. Interprets the embryo to be the weakest of living human beings. States that only by declining to use embryos for this research do we awaken our imagination and force ourselves to seek other sources for stem cells. He objects to stem cell research on aborted fetuses (which were not spontaneously aborted) because it is a case of the strong using the weak that other solutions should be pursued. Abdulaziz Sachedina, Ph.D – Islam has “little problem in endorsing ethically regulated research on the stem cells that promises potential therapeutic value, provided that the expected therapeutic benefits are not simply speculative. Islam sees equal human value in the embryo at later stages of its biological development. Makes a distinction between the biological and moral person , placing the latter stage after, at least, the first trimester. D9. Compare and contrast the different religious perspectives on human embryonic stem cell research. Jewish views of the use of genetic materials are conflicted. Within Judaism, abortion is forbidden, which is the source of embryonic stem cells. However, it is permissible if it saves the life of the mother. Recent sources have included that abortion is permissible when genetic testing indicates that the fetus will suffer from a terminal disease or from serious malformations. Therefore, if a fetus is aborted for legitimate reasons, may be used to advance efforts to preserve the life and health of others. Stem cells can be procured for research from donated sperm and eggs that are cultured in a Petri dish. Genetic material outside the uterus has no legal status in Jewish law. The recommendation is to advance stem cell research and its applications in an effort to take advantage of its potential for good. Online Jewish Opinion Jewish views hold that a fetus outside the mother's body does not have the same value as a fetus within her body. Traditionally, a fetus was 'water' for the first 40 days.8 'Genetic materials outside the uterus have no legal status in Jewish law, for they are not even part of a human being until implanted in a woman's womb'.9 Most commentators speak of a 'mandate to heal' and a 'mandate to be partners with God in creation,' and some would allow creation of embryos in a petri dish solely for research. Catholic views are based upon church doctrine regarding the sanctity of life, including clear opposition to abortion and the embryonic stem cells derived from aborted fetuses. However, the two articles represent divided opinions regarding the moral status of the embryo. In the first article, written by the physician, he states that the teachings of the Roman Catholic Church provide that all embryos have the same status as a fetus and the utilitarian argument for stem cell research does not justify destruction or disposal of embryos. He further notes that Catholics recognize the potential for human therapeutics in stem cell research, as long as the source of cells is derived from adults. Nevertheless, he is unbending in his opinion of the Roman Catholic view that human life is a continuum from the one-cell stage to death. At every stage, human life has dignity and merits protection. It should be noted that the medical author also believes in the protection of humans in a vegetative state. This perspective defies the understanding that brain death is the legal definition of death, allowing the use of organs in transplantation. He is totally opposed to the use of “spare embryos” from in vitro fertilization clinics and challenges the accepted understanding of the potential of pluripotential cells. The second opinion, written by an academic scholar of religious studies contradicts the first opinion, stating that Catholics disagree on the use of fetal and embryonic stem cells. The basis of her argument is centered upon the belief that the human embryo in its earliest stages deserves respect and protection; however, the centuries-old Catholic position that a certain amount of development is necessary in for a conceptus to warrant a personal status. Fertilization is a process and not a “moment.” The authors are consistent in the concept of complicity when using cells from aborted tissues. The second author approves the use of embryonic stem cells, and therefore, stands in opposition to the first opinion. If both authors are deemed credible, then the “Catholic” opinion is divided and inconsistent. Online Catholic Opinion Catholic doctrine holds that embryos have intrinsic value. The National Conference of Catholic Bishops is much in the news as the most vocal opponent of stem cell research, even after Bush's decision. However, this conservative body does not represent all American Catholics or all Catholic moral theologians. Polls suggest that the majority of Catholic laypeople approve stem cell research. There is some latitude in moral theology. Although the Pope publicly expressed his disapproval to President Bush before 9 August, he did not speak ex cathedra, which could have made the statement 'infallible' according to Catholic doctrine. A growing number of Catholic moral theologians do not regard very early human embryos as individualized human entities and would allow research before the development of the 'primitive streak' at 14 days, which marks the point at which some cells are destined to become the embryo and others to become the placenta. 6 This dividing line is widely recognized as having enough symbolic significance to permit research beforehand and prohibit it afterwards. This view is analogous to a centuries-old tradition of 'ensoulment'. According to Thomas Aquinas (following Aristotle and St Augustine), rational souls entered males at 40 days and females at 90 days, thereby establishing personal existence and completing the process of conception. Embryos in the earliest stages had only a 'vegetative' life-force. However, nineteenth-century scientific discoveries about the timing of conception pushed ensoulment into the background. In July 2000 the Pope listed cloning and stem cell research as among 'the evils of Western culture'. Protestant viewpoint provides that stem cells are not themselves and cannot develop into embryos; however, embryos deserve protection from destruction because of its moral status as the weakest member of the community. The author believes that the embryo has “individuality” and only through the refusal to give in to the temptation of its possible therapeutic value will we force ourselves to discover other methods of achieving desirable ends. He opposes the use of embryos from aborted fetuses because of his objection to abortion. The article proposes that harvesting stem cells encourages the improper development and use of these cells and lose the ability to respect human life in the form of an embryo. The author does not take a concrete position on the correctness of use of embryonic stem cells, but encourages the search for “truthfulness” in our understanding and regulate future use. Online Protestant Opinion Protestant views vary. Historically, Protestantism supported science, believing that nature was faulty and that God intended us to discover its inner workings and repair it. In the seventeenth century, Boston's Puritan ministers preached the virtues of inoculation for smallpox from the pulpit and even administered it themselves, while the medical establishment held back.7 This crusading spirit, originally religious, continues to affect American medical practice and scientific research. Some denominations have expressed support for embryonic stem cell research, including the General Assembly of the Presbyterian Church (http://www.eurekalert.org/pub_releases/2001-06/SaRN-Pvif-1406101.php) and the United Church of Christ. Others have taken the intrinsic value position, including the conservative Missouri Synod Lutheran Church (http://www.islet.org/forum/messages.19166.htm), the United Methodist Church (http://www.umc-gbcs.org/bbpr118a.htm) and the Southern Baptist Convention (http://www.sbcannualmeeting.org/sbc99/res7.htm), all three of which oppose embryonic stem cell research and hope that adult stem cells will suffice. In view of their overall support for medicine and technology, some denominations that now oppose may change their minds if embryonic stem cell research succeeds. Islamic viewpoint and tradition, research uses of Pluripotent stem cells derived from human embryos can be inferentially deduced from the rulings of the Shari’a Islamic law regarding the sanctity of the embryo. Specifically, these cells come from a second source, similar to a cadaver, and suitable for donation in order to save the lives of others. Personhood development occurs over time and endorsement of the use of embryonic stem cells is consensual with all sects. The Koran does not provide any definition or recognition of the embryo, but a crime against a fetus is the same as a crime committed against any human being. As a result, the distinction between a biological and a moral person occurs after the first trimester of pregnancy. Online Islamic Opinion Islamic views generally place ensoulment at the 120th day, after three 40-day periods of development, and hold that a very early embryo has no moral status. According to one interpreter, 'research on stem cells made possible by biotechnical intervention is regarded as an act of faith in the ultimate will of God as the Giver of all life, as long as such an intervention is undertaken with the purpose of improving human health'. D9. Compare and contrast the different religious perspectives on human embryonic stem cell research. The conservative Christian view that human life is created at conception contrasts with the view common among Jews that an embryo doesn't become human until 40 days after conception, and the similar Muslim view that human life begins when the soul enters the developing baby sometime between 40 days and 120 days after conception. The different beliefs in the timing of when a developing embryo becomes a human likely accounts for different levels of acceptance for embryonic stem cell research, which is supported in the Jewish community, is accepted in many Muslim countries, yet is opposed by the Roman Catholic Church and some Protestant denominations. D9. Compare and contrast the different religious perspectives on human embryonic stem cell research. JEWISH Perspective: Rabbi Elliot N. Dorff, Ph.D. A. Fundamental Theological Convictions Our bodies belong to God; God wants us to seek to preserve our lives and our health Physicians are agents and partners of God; Jewish tradition accepts both natural and artificial means for overcoming illness. Must use any therapies which aid us in taking care of our bodies (which ultimately belong to God). All humans (regardless of level of ability or disability) are created in the image of God, and must be valued as such. Epistemological humility – we are not God, so we must do what we can to “work the world and preserve it”; achievement of that balance which is our divine duty. B. Jewish Views of Genetic Materials Status of abortion is main concern (b/c embryonic stem cells involves procuring them from aborted fetuses) o By and large, in Judaism, abortion is forbidden. (Cannot destroy a part of the body, unless that part becomes dangerous to the mother.) o So, if a pregnancy endangers a woman’s life or health, an abortion must be performed to save her life or protect her physical or mental health. o If only elevated risk, abortion is permitted but not required. o Some accept abortion in cases where fetus will suffer from a terminal disease (ex. Tay-Sachs) or serious malformations. IF a fetus was aborted for legitimate reasons under Jewish law, it may be used to advance our efforts to preserve the life and health of others. Another way to procure stem cells is from mixing donated sperm and eggs. o Genetic materials outside the uterus have no legal status in Jewish law, b/c they are not even part of the human body until implanted… even then, during the first 40 days, their status is “simply water”. Abortion is prohibited during that time except for therapeutic purposes. o Outside the womb, no special potential of growing into a human being. o Frozen embryos can therefore be discarded or used for reasonable purposes and so may the stem cells which are produced by them. C. Other Factors in This Decision If materials for SCR are produced in permissible ways, the technology itself is morally neutral. It gains moral valence on the basis of what we do with it. Risk-benefit analysis of SCR: look at Hastings Center Report o Justice arguments (provision of health care as a communal responsibility) vs. our capitalistic system of economics: must balance access to applications of the new technology with the legitimate right of a private company to make a profit on its efforts to develop and market applications. o Potential for SCR to create organs for transplant and cures for disease is both awesome and hopeful. Some may argue (from a Jewish perspective) we have a DUTY to proceed with that research. However, must draw line b/w uses for cures and uses for enhancement. Jews are especially sensitive to creating a model human being that is to be replicated though the kind of genetic engineering that SCR application swill involve. o Thus, in light of the Jewish view that all human beings are created in the image of God, regardless of their level of ability or disability, it is imperative from a Jewish perspective that the applications of SCR be used for cure and not for enhancement. D. Recommendation (SUMMARY) Take steps necessary to advance SCR and its applications in effort to take advantage of its great potential for good. However, do so in such a way that we provide access to its applications to all Americans who need them and at the same time prohibit the development of applications intended to make all human beings fit any particular model of human excellence. Seek to cure disease while appreciating the variety in God’s creatures. ROMAN CATHOLIC: Edmund D. Pellegrino, M.D Argues against moral acceptability of research involving (1) embryonic stem cells obtained from in vitro-fertilized blastocysts and (2) embryonic primordial germline cells obtained from aborted fetuses. o Teachings of the Roman Catholic Church about moral status of the fetus and embryo: both involve direct interruption and termination of a human life. (RC have moral claim of protection from first moments of conception.) o Insufficiency of the utilitarian arguments that would justify destruction or discarding of embryos: o The practical difficulties of effectively regulating the practice even if it were morally defensible. (1) Moral Status of Embryo o Life is a continuum from one-cell stage to death… at every stage life has dignity and merits protection. o Cannot use life (at any stage) as means to another end, no matter how noble. o RCC rejects idea that full moral status is conferred by degrees or is achieved at some arbitrary point in development. o Also rejects socially constructed models that leave moral status to definition by social convention, where moral status can be conferred or taken away depending on social norms. (ex. Cases of genocide; cases of fetus, embryo, mentally retarded, or permanent vegetative state.) o However, is difference of using cells from aborted fetuses if act of abortion is separated from needing those cells. Moral problem is that abortion is wrong. Moral gravity of tissues (fetus or embryo) is different, but both still have rights so act is still wrong. (2) Moral arguments for permitting ESCR are faulty o One argument: spares (fertilized ova) from IVF will be discarded anyway, no why not use them? o However, many spares are frozen; all have not been destroyed. Even if consent to use of extras, moral status of embryo has not changed. Ones created for research are no different than ones created for reproduction. Embryos still treated as a means to an end. o Inherent moral status violated b/c still killed to obtain stem cells. Cannot subject anyone to harm, even on prediction death will come anyway. o Governmental funding of research is also a problem, since it forces compliancy through taxation. (3) Cannot promise to control abuses through appropriate legal regulation o Temptation to make “spares” for research; cannot (and should not) post monitors in all labs. o Still uncertain whether pluripotent cells are not totipotential and capable of developing into a complete human embryo o Obvious complications of profits and patents when ethics boards are appointed by biotechnological corporate elites. CONCLUSION o Must reject any attempt to legitimize embryonic stem cell research from in vitro fertilized-blastocysts or from aborted fetuses, the moral, legal, and practical impediments of which are of such great magnitude and complexity. o Instead, should strongly encourage the funding and development of alternate sources of stem cells – those that do not depend on the destruction of living human embryos or make use of cells from induced abortions. ROMAN CATHOLIC: Margaret A. Farley, Ph.D. No simple or single voice from the Catholic Community Disagreements regarding human embryonic stem cell research dependent on the moral status of the human embryo and the aborted human fetus, from which the cells come from. AGAINST o Human embryos must be protected as human persons, at least so that they may not be created or destroyed merely for research purposes. o Use of aborted fetuses as a source for stem cells should be prohibited b/c it is complicit with an offers a possible incentive for elective abortion o Need to identify other alternatives (use of adult stem cells, dedifferentiated, redifferentiated, etc.) FOR o Many theologians do not consider the human embryo in its earliest stages (prior to development of the primitive streak or to implantation) to constitute an individualized human entity with the settled inherent potential to become a human person. o Moral status of the embryo is not that of a person, and its use for certain kinds of research can be justified. Though it is a form of human life, it does deserve respect, such as not to be bought or sold. o Return to idea that we need a certain amount of development in order for a conceptus to warrant personal status. Embryological studies show that fertilization is a process, and not a moment. At the blastocyst stage where stem cells would be extracted, the embryo is not sufficiently individualized. o Also, may use spontaneous abortions, and rule out any donated fetuses. o Ensure absolute barrier b/w cloning for research and cloning for reproductive purposes. Farley stands with the FOR case PROTESTANT: Gilbert C. Meilaender, Ph.D. No simple or single voice from the Protestant Community (1) STATUS of the HUMAN EMBRYO o Procuring ESCs requires destruction of the embryo, so look to moral status o Look to abortion, which focuses of claims of fetus and claims of the pregnant woman, taking the women’s claims over the fetus’. However, in research, no such direct conflict. The embryo is the “weakest and least advantaged of our fellow human beings”, and no community can really be strong unless it carries its weakest members. o What does it mean to be an individual? To have personhood? Must refuse to think of a person as someone with a certain set of capacities, but as someone who carries a personal history, whether or not they are aware of it. o So, we must honor the dignity of even the weakest of living human beings, and come to appreciate their history. (2a) SCR as a SAVING SOLUTION o SCR can be developed as a saving solution, but promises and possibilities of SCR could easily be oversold o Suffering, and even death, are not the greatest evils of human life. o Even though research sees a desirably good end, the means of destroying embryos do not justify this. Only by declining to exercise our will in this way, do we force ourselves to look for other possible ways to achieve admittedly desirable ends. (3) Must not derive stem cells from aborted fetuses. o Even though this can be seen as simply another form of tissue or organ donation, it threatens to take us back to the abortion debate. o We could ensure safeguards that do not encourage abortion, and only use spontaneous abortions, but then why couldn’t we used fetuses aborted for permissible reasons, though induced and intended? Slippery slope. o Since the life of the fetus has been forfeited through abortion for the good of someone else, no matter the method or means, “a moral intuition insists that being used once is enough”. (3) Language: Must speak truly and straightforwardly o Must avoid euphemism and equivocation o ISLAM TRADITION: Abdulaziz Sachedina, Ph.D. Speaks for the Islam tradition in general, a textual tradition, taking into account two major schools of thought: the Sunni, and the Shiite, both “orthodox”. STATUS of the HUMAN EMBRYO The use of cells from embryos following abortion is analogous to cadaveric donation, so it is permissible Question of inception of embryonic life: Life inside the womb occurs in stages; Koran suggests the embryo’s development and ensoulment occurs over time, where moral personhood is an achievement at the later stage in biological development. o Allows for possible distinction between a biological and moral person. Look to collaborate with scientific research and evidence. (has changed over time) o First was looking for palpable movements in womb (4th month of pregnancy) o Many today still make distinction between pre- and post-ensoulment stages in pregnancy, at the 120 day (or 4 month) mark, where there is a well-defined form and evidence of voluntary movement o But many still regard the embryo in the pre-ensoulment stages as alive and its eradication a sin. As participants in the act of creating and curing with God, human beings can actively engage in furthering the overall good of humanity by intervening in the works of nature, including the early stages of embryonic development, to improve human life. CONCLUSIONS The Koran and Tradition regard perceivable human life as possible at the later stages of the biological development of the embryo, thus the fetus is accorded a legal status of a person at this later stage when perceptible form and voluntary movement are demonstrated. o Distinction b/w a biological and moral person at the ensoulment stage. Biotechnical intervention in the early stages of life is regarded as an act of faith in the ultimate will of God (not as an interference with the will of God) as long as such intervention is undertaken with the purpose of improving human health. D9. Compare and contrast the different religious perspectives on human embryonic stem cell research. Jewish View The Jewish tradition legitimizes the use of stem cells research IF the fetus was aborted for legitimate reasons, it may be used in research to benefit the lives of others. Also, stem cells may be used in research if they came form donated embryos and sperm that were cultured in a Petri dish (genetic material outside the womb has no status in the Jewish religion). Roman Catholic View The Catholic tradition argues against the moral acceptability of research involving stem cells obtained though IVF blastocytes, and germ line cells obtained from aborted fetuses. They view human life as a "continuum from the one cell stage to death" and at every stage, human life has dignity. Embryos should be treated with respect, so to use their cells in research is morally wrong. This is summed up by Meilander who uses the argument that "no community…is strong if it will not carry its weakest member". They believe that we may sometimes need to deny ourselves the "handiest means" to an undeniably good end, and suggest looking to new solutions to this stem cell issue. Islamic Perspective The use of pluripotent stem cells derived from the human embryo, in Islam can be deduced from the laws of fetal viability and the sanctity of the embryo. The moral considerations stem from the issue of when the fetus attains human personhood and full moral and legal status. Most make this distinction at the end of the fourth month when "ensoulment" takes place. Others argue that life begins in the very second of conception and the embryo must be protected. The proposal has been made that the fetus attains human status only in later stages of development, so research on stem cells is made possible in the early stages of life, on the grounds of improving human health. D9. Compare and contrast the different religious perspectives on human embryonic stem cell research. o Elliot (Judism): Fetus is thought of as “the thigh of the mother” – only gotten rid of if it threatens the mother in some way (it does not have status of full human being. Abortion is permitted if there is elevated risk to woman beyond that of normal pregnancy; therefore if the fetus is aborted for legitimate reasons it may be used to advance efforts to preserve life and health of others Genetic materials outside uterus have no legal status in Jewish law; frozen embryos may be discarded or used for reasonable purposes and so may the stem cells that are produced for them Technology is morally neutral – gains moral valence on basis of what we do with it Healthcare is communal responsibility potential for stem cell research in creating organs for transplants and cures for disease is awesome Technology to cure is good but technology for enhancement must be approached with caution (cure = good, enhancement = bad because everyone is created in the image of god and there is no one human model of excellence) o Pellegrino (Roman Catholic) Okay to use cells form humans, miscarriages and placental blood NEVER okay to (1) destroy human embryos or (2) harvest germ cells from aborted fetuses Life is a continuum from 1 cell death and therefore human life always deserves respect and protection Cannot treat embryo as a means to an end (killed to get stem cells) Need legal regulation to combat the temptation to make spares Reject any attempt to legitimize embryonic stem cell research from in vitro fertilized blastocysts of from aborted fetuses Instead encourage funding and development of alternative sources of stem cells (those that do not depend on destruction of living human embryos or make use of cells from abortions) o Farely (Roman Catholic) Disagreements; conflicting assessments of the moral status of the human embryo and the use of aborted fetuses as sources of stem cells Against – embryos must be protected on a par with humans – they should not be created or destroyed merely for research purposes. Alternative methods should be used For – growing number do not consider the human embryo in its earliest stages to constitute an individualized human entity with inherent potential to become a human person (still due to some respect – can’t be bought or sold). They insist on barrier between cloning for research and therapeutic purposes and cloning for reproductive purposes Authors View (For) – research can be made without sacrificing the tradition’s commitments to respect human life, promote human well being and honor the sacred o Meilaender (Protestant) Three main points (1) No community is really strong if it will not carry its weakest members embryo is weakest member and strong community and in honoring its dignity we come to appreciate the mystery of human person (2) we many sometimes need to deny ourselves the handiest mean to an undeniable good end we must force ourselves to look for other possible ways to achieve desirable ends – saying no stimulates us to think creatively about other, better possibilities should not use stem cells from aborted fetuses or embryos because this is example of strong using the weak (life of embryo sacrificed to help someone else; being used once is enough) (3) use language necessary to form lives in truthful manner should not deceive ourselves by using fancy language (saying we will use only “excess” embryos from infertility treatments when these treatments create far more embryos then are actually needed) o Sachedina (Islamic) Many different views within religion (below is most common views held) Cell derived from fetal tissue following abortion are analogically similar to cadaver donation for organ transplantation in order to save other lives therefore cell from that source are permissible Majority make distinction between two stages in pregnancy divided by end of the fourth month (120 days); abortion is okay before end of fourth month Most common view – perceivable human life as possible at later stages of biological development of embryo Fetus given same status of legal person at later stages in development (when form and voluntary movement develop); embryo possesses no moral status before this Research on stem cells made in early stages of life is regarded as act of faith in ultimate will of God – as long as intervention is undertaken with purpose of improving human health D10. Describe President Bush’s decision (& its justification) on funding human embryonic stem cell research. The decision: to provide funding for stem cell research on lines already derived and not provide funding on the procurement of the cells from embryos. The justification is that the government acts morally in providing funds for research which has the potential to help people and avoids acting immorally by possibly funding the destruction of embryos. The moral lines it draws have been criticized as superficial solutions. D10. Describe President Bush’s decision (& its justification) on funding human embryonic stem cell research. President Bush believed in not funding the part of the research where the embryonic stem cells would have to be destroyed, but rather using the already available (destroyed) stem cell line and funding research using those cell lines. His justification is that the state is not supporting the actual destruction of embryonic cells, but supporting the fruitful results that may come from such research D10. Describe President Bush’s decision (& its justification) on funding human embryonic stem cell research. President Bush’s policy Private funds for derivation, but federal funds for use on cell lines derived by 9:00 PM EDT, August 9, 2001 President’s Council on Bioethics Agreed for a ban on reproductive cloning but differed on whether to regulate or temporarily suspend therapeutic cloning o Majority (10) Ban on cloning-to-produce-children 4-year moratorium on cloning-for-biomedical-research o Minority (7) Ban on cloning-to-produce-children Regulation of the use of cloned embryos for biomedical research Justification o Bush, argues that research on the cells, which can be derived from human embryos created during in-vitro fertilization treatments, effectively destroys a human life o Bush said he took heart from studies released that suggested it may be possible to grow stem cells from sources other than human embryos such as human adults President Bush has praised new research and claimed some credit for the breakthrough: His ban on the use of federal funds for human embryonic stem cell research helped to stimulate the search for ethically acceptable alternatives D10. Describe President Bush’s decision (& its justification) on funding human embryonic stem cell research. Bush believes we should not perform research on embryonic stem cells because o It is a slippery slope and it could lead to unethical research (scientists made embryonic stem cells in test tubes specifically for the purpose of research not as a result of IVF) o Human life is a “sacred gift from our Creator” and will be devalued by research o Worries it won’t live up to its hope Bush says there are already 60 lines of genetically diverse stem cells made from already destroyed embryos and they can reproduce indefinitely by themselves. Federal funds should be used for these and more should not be created. Federal funds can be used for umbilical stem cell research which do not have the same moral dilemma. D11. How would different ethical principles apply to the above discussions? Principles – Nonmaleficence, Beneficence, Autonomy, Justice, and Utility With regards to stem cell research, utility, balancing the good and the bad effects, is a priority in that part of the ethical justification for stem cell research is that can be beneficial to individuals with currently incurable diseases. This good effect must be certain or justification for stem cell research, regardless of position on the moral status of the embryo, is void. The autonomy of individual moral beliefs must be considered when making public policy considerations since the money funding stem cell research is taken from tax payers, some of which may be morally opposed to stem cell research. In an opposite scenario, respect for the autonomy of individuals who hope for a cure to their disease and who stand to benefit from stem cell research must be taken into account. Justice is key in genetic testing. The practice of genetic testing must be made available to all. Distribution of the resources must be a primary goal if genetic testing is to be ethical. Also, from a different perspective, for genetic testing to be ethical, it must not promote eugenic thought which could fortify injustices against disabled members by placing on them a stigma. D11. How would different ethical principles apply to the above discussions? In terms of beneficence President's Bush's stance on the matter is somewhat incomplete. His use of already dead germ line is beneficial to society, but funding all types of stem cell research would be most beneficial to society. President Bush's lack of support in the actual destruction of the embryonic cells supports the nonmaleficence argument, since he refuses to support any sort of ending of a life and destructing the possible chance of a human life. Lastly, the president's use of the already destroyed cells illustrates a utilitarian argument as well, in that he is putting the already destroyed cells to good use, however a complete utilitarian argument would be using all potential embryonic cell lines that are frozen but not yet destroyed in use for research. D11. How would different ethical principles apply to the above discussions? 1. Slippery slope a. From correcting genetic diseases in somatic cells to enhancing qualities of the germline 2. Justice and equity a. FDA approval of Bidil, an anti-heart failure drug, for use by self-identified black patients b. selection of research subjects needs to be scrutinized in order to determine whether some classes are being systematically selected simply because of their easy availability, their compromised position, or their manipulability, rather than for reasons directly related to the problem being studied i. (e.g., welfare patients, particular racial and ethnic minorities, or persons confined to institutions) c. research supported by public funds leads to the development of therapeutic devices and procedures i. not provide advantages only to those who can afford them and that such research should not unduly involve persons from groups unlikely to be among the beneficiaries of subsequent applications of the research 3. Confidentiality a. Genetic privacy i. Genetic information is uniquely personal and powerful ii. Problematic metaphor of a “future diary” 4. Respect for Persons a. individuals should be treated as autonomous agents i. subjects enter into the research voluntarily and with adequate information b. not every human being is capable of self-determination i. because of illness, mental disability, or circumstances that severely restrict liberty c. persons with diminished autonomy are entitled to protection 5. Beneficence a. research involving children i. research that presents more than minimal risk without immediate prospect of direct benefit to the children involved 1. would rule out much research promising great benefit to children in the future E1. List and explain Emanuel et al’s ethical requirements for clinical research. Informed consent is not sufficient for ethical clinical research However there are 7 requirements that make up the proper framework for ethical clinical research: o 1. There must be value- enhancements of health of knowledge must be derived from the research. o 2. There must be scientific validity- the research must be methodologically rigorous. o 3. There must be fair subject selection- scientific objectives, not vulnerability or privilege, and the potential for and distribution of risks and benefits, should determine communities selected as the study sites and the inclusion criteria for individual subjects. o 4. There must be a favorable risk-benefit ratio- risks must be minimized, potential benefits enhanced, and the potential benefits for individuals and society must outweigh the risks. o 5. There must be independent review- unaffiliated individuals must review the project and approve, amend, or terminate it. o 6. There must be informed consent- individuals should be informed about the research and give their voluntary consent. o 7. There must be respect for enrolled subjects- subjects will have their privacy protected and the ability to withdraw from the experiment. All 7 requirements must be met in order to have and ethical clinical study. The requirements are universal and they must be adapted to the health, economic, cultural, and technological conditions in which the research is being conducted. E1. List and explain Emanuel et al’s ethical requirements for clinical research. 1. Social or scientific value o Evaluates a diagnostic or therapeutic intervention that could lead to improvements in health or well-being o Increase knowledge o Requirement so that it ensures responsible use of finite resources and avoidance of exploitation 2. Scientific validity o Must be conducted in a methodologically rigorous manner o Must have a clear, scientific objective, be designed using accepted principles, methods, and reliable practices, have sufficient power to definitively test the objective and offer a plausible data analysis plan o There must be an equipoise – controversy within the scientific community about which is better o Requirement so that it ensures responsible use of finite resources and avoidance of exploitation 3. Fair subject selection o The scientific goals of the study, not vulnerability, privilege, or other factors unrelated to the purposes of the research, be the primary basis for determining the groups and individuals that will be recruited and enrolled o Efficiency cannot override fairness in recruiting subjects o Required to ensure justice 4. Favorable risk-benefit ratio o To minimize risk and maximize benefits; risks must be at least proportionate to the benefits to the subject and society o Required for beneficence, nonmaleficence, and to ensure exploitation does not happen 5. Independent review o Important for social accountability o Assures members of society that people who enroll in trials will be treated ethically and that some segments of society will not benefit from the misuse of other human beings o Ensures the trial is ethically designed and the risk-benefit ratio is favorable o Occurs through multiple groups o Required for public accountability and minimizing potential conflicts of interest 6. Informed consent o Individuals must be accurately informed of the purpose, methods, risks, benefits, and alternatives to the research o They must understand this info and its bearing on their own clinical situation o Must make a voluntary and uncoerced decision whether to participate o Embodies the need to respect persons and their autonomous decisions 7. Respect for potential and enrolled subjects o Privacy must be respected by managing the info in accordance with confidentiality rules o Must permit subjects to change their mind and to withdraw without penalty o Welfare of subjects must be monitored throughout study o Justified by multiple principles including beneficence, nonmaleficence, and respect for persons E1. List and explain Emanuel et al’s ethical requirements for clinical research. 1. Social or Scientific Value a. clinical research must lead to improvements in health or advancement in knowledge b. Valueless research includes vague studies, “me too” studies, and non-disseminated research 2. Scientific Validity a. Research must be conducted in a methodologically rigorous manner that is practically feasible b. must produce reliable and valid data that can be interpreted c. Invalid research includes underpowered studies, studies with biased endpoints, instruments, or statistical tests, and studies that cannot enroll sufficient subjects 3. Fair subject selection a. Convenient groups should not be selected b. Groups cannot be excluded without scientific reasons c. Higher risk is a reason to exclude certain groups d. scientific objectives of the study—not vulnerability or privilege—should guide inclusion criteria and targeted Populations e. Lowering risk and enhancing generalizability can then be considered f. Should not select rich, politically powerful or otherwise well connected people for “promising research” studies 4. Favorable risk-benefit ratio a. Risks must include: i. Physical —death, disability, infection ii. Psychological —depression and anxiety iii. Social —discrimination iv. Economic —job loss b. If potential benefits to the individual outweigh risks to the individual then proceed c. If risks outweigh benefits to the individual, then evaluate risks against social benefit of knowledge gained 5. Independent review a. Because investigators have multiple legitimate interests, they have potential conflicts of interest b. Independent review of the research minimizes these conflicts Independent review also assures society it will not benefit from abuse of subjects 6. Informed consent a. 7. For those who cannot consent—such as children and mentally impaired—must be sure research fits with their interests b. Informed consent consists in 4 elements i. Competence of the subject ii. Disclosure of information to the subject iii. Understanding or comprehension by the Subject iv. Voluntariness of the decision c. The Federal regulations require 8 elements be included in each informed consent form. i. Purpose and duration of participation ii. Risks iii. Alternatives iv. Benefits v. Confidentiality of records vi. Compensation for injuries vii. Person to contact for answers to questions viii. Voluntariness and right to withdraw Respect for potential and enrolled human subjects a. Protecting confidentiality b. Permitting withdrawal c. Providing new information d. Monitoring welfare e. Informing them of what was learned from the research, and newly discovered risks or benefits E1. List and explain Emanuel et al’s ethical requirements for clinical research. The 7 ethical requirements for clinical research: Value—which means that ethical, clinical research must be valuable --- that the intervention could lead to improvements in health or well-being, also it could generate important knowledge abt structure/ function of human biological systems, even if the knowledge may not lead to immediate benefits. This includes sharing of the information, whether positive or negative. Reasons why this requirement is necessary: "use of finite resources and avoidance of exploitation." Scientific Validity --to be ethical valuable research it must be conducted in a methodical manner – the methods should be valid and practically possible. The research should have defined scientific objectives, designed using correct, acceptable, usable pactices, have enough power to definitely test the objective, and thre should be a real plausible data analysis plan. Fair Subject Selection- subjects should be selected fairly in that scientific goals of the study be used as primary basis for determining which groups and/or individuals should be recruited. Also, groups or individuals shouldn't be excluded unless for a good scientific reason, such as risks, (groups such as women). More importantly, subject selection can affect the risks and benefits of study, and subjects should always be chosesn to minimize risks and enhance benefits to the subjects and society. Favorable Risk –Benefit Ratio - clinical research can only be justified if it is consistent with the scientific goals, but mainly the potential risk must be minimized, the benefits enhanced, and thus the potential benefits to the individual and/or society must be proportionate to or outweigh the risks. Independent Review- research done by various individuals will portray a variety of interests that may conflict and skew the good willed intentions of a study, thus an independent review by individuals not associated with the clinical research helps minimize the potential impact of such conflicts of interest. Informed Consent- purpose of informed consent is that the individual controls whether or not he/she wants to participate in the study, and to ensure that the research is consistent with their personal values and choices. Also to provide informed consent, individuals must be accurately informed about all aspects of the study to make a voluntary, uncoerced decision. Respect for Potential and Enrolled Subjects – basically, individuals must be respected at all times since they were approached to participate in the study—even during study if enrolled, and even if they decided not to enroll in study. This respect includes: respecting their privacy, allowing them to change their mind without penalties, given any new information obtained, monitoring welfare of subjects at all times, and lastly informing them of what was learned from the study. E2. Describe Rothman’s explanation of research abuses around the time of WWII. WWII was the turning point in human experimentation. For the first time, clinical investigations became well-coordinated; extensive, and centrally funded team efforts. Experiments were now frequently designed to benefit not the research subjects but others- namely soldiers vulnerable to the disease in question. o This occurred during a time when the wartime conditions were affecting the soldiers’’ ability to consent. He Committee on Medical Research was created to conduct medical research and its primary concerns were to create antidotes to dysentery, influenza, venereal diseases, and malaria, in which all would require extensive research with human subjects. o The battlefield proved to not be a good control for the experiments so researchers turned to asylums to do their tests. Serious side-effects were felt by many of the patients. o Because malaria was so rare in the U.S, researchers infected the subjects with malaria and then attempted to cure it. o CMR also sought to find a cure for influenza because it was the disease most drastically affecting the soldiers. o WWII eventually turned into the war against disease. E2. Describe Rothman’s explanation of research abuses around the time of WWII. Informed consent was not required because during war, the draft had no consent so scientists felt they did not need to do informed consent if it was benefiting society Performed research on people with impaired inmates of asylums and prisoners and mentally retarded people Purposefully injected people with viruses “when research promised to buttress the war effort (as did research on influenza, malaria, and dysentery), considerations of consent and voluntariness disappeared” More about the utilitarianism of the war, than about each individual so they did not have a hard time justifying using mentally retarded, mentally ill, or institutionalized people for research Society did not revolt against this until the late 1960’s E2. Describe Rothman’s explanation of research abuses around the time of WWII. 1. Practices established during these years profoundly influenced researchers’ behavior in the postwar era a. Clinical investigations became well-coordinated extensive, and centrally funded team efforts b. Experiments were now frequently designed to benefit not the research subjects but others, namely soldiers vulnerable to the disease in question 2. Investigators sought suitable research sites for researching antidotes to dysentery a. Research on the battlefield was out of the question b. Instead asylum wards where dysentery was endemic and no one objected to experiments on impaired inmates c. Trials were also carried out on retarded residents i. Using mentally incompetent inmates as research subjects also accorded closely with popular ideas about eh sacrifices appropriate to the home front 3. Malaria was rarely found n the united States a. Researchers infected subjects and then measured the effectiveness of their antidotes b. Relied heavily on prisoners in state penitentiaries 4. The Committee on medical research convened a special committee to review protocol decisions about the prisoners ineligible to volunteer and a consent form a. Although an intuitional review board today might object that the document exaggerates the potential benefit of the research to the subjects and is too aggressive I its recruitment , the form is notable accurate about the risks posed by the research 5. When research promised to buttress the war effort, considerations of consent and voluntariness disappeared a. A wartime environment also undercut the protection of human subjects, because of the power of the example of the draft. i. Researchers doing laboratory work were also engaged in a military activity, and they did not need to seek the permission of their subjects 6. Physicians apparently found Nuremberg irrelevant to their own work a. They believed that the bizarre and cruel experiments had been conducted not by scientists, and doctors but by sadistic Nazi officers and therefore that dedicated investigators had nothing to learn from the experience E2. Describe Rothman’s explanation of research abuses around the time of WWII. Turning point in human experimentation was WWII, when these experiments became well coordinated and centrally funded , and mainly they were carried out not to benefit the subjects but the rest of society (soldiers). They needed to make antidotes to dysentery, influenza, venereal disease, and malaria, which all would require research with humans. The ethical concerns discussed were the use of asylum wards (where dysentery was endemic) as a setting for research, and the fact that nobody objected to the use of impaired inmates as test subjects. Other horrid examples of such unethical practices was the experimentation on orphanage children for finding a cure for the shiglla bacteria, another example was the use of retarded residents at the New Jersey State Colony for the Feeble Minded for Malaria research. Out of all the studies, only one study conducted by the CMR prompted a complete discussion of ethics, and that was research in the area of gonorrhea, where actual consent of prisoners was taken. Also a lot of the research portfolios had claims of exaggerated potential benefits than actually possible. What was another upsetting point of these studies was that even if informed consent was considered and risk-benefit calculations were carried out wartime demands obscured such occurrences. Using such subjects such as mentally incompetent inmates was valued as a sacrifice appropriate to the home front. E3. Know the ethical considerations in the use of placebos, and the concept of ‘clinical equipoise’. How do these concepts apply to international clinical research? See B&C and Emanuel et al. B&C feel that there is no justification for not revealing to potential subjects the full set of methods, treatments, and placebos that will be used, their known risks and probable benefits and uncertainties. o The once a patient is selected they are randomized as to which treatment they will receive. o “Clinical equipoise”- the community of reasonable physicians who feel that randomized controlled trials are justifiable because prior to conducting the research they do not know if it is more advantageous to be in the control of experiment group. Many moral problems surround starting a placebo-controlled trial when a disease appears to be universally fatal and no promising alternative to the new treatment exists. There are related questions about when it is right to stop a trial. Surgery acting as a placebo can also be dangerous because there are dangers from the procedure and anesthesia. E3. Know the ethical considerations in the use of placebos, and the concept of ‘clinical equipoise’. How do these concepts apply to international clinical research? See B&C and Emanuel et al. 1. Controlled clinical trials are needed to establish or confirm that an observed effect, such as reduced mortality from a disease, results from a particular intervention rather than from an unknown variable in the patient population a. A control group receives either a standard therapy or a placebo so that investigators can determine whether an experimental therapy is more effective and sager than a standard therapy or placebo b. Commonly, subjects are randomly assigned to control and experimental groups to avoid intentional or unintentional bias c. Blinding certain persons to some information about the randomized controlled trial (RCT) provides additional protection against bias i. Single blind; the subject does not know whether he or she is in the control group or the experimental group ii. Double blind; neither the subject nor the investigator knows iii. Unblinded ; all parties know 2. “Clinical equipoise” (Benjamin Freedman): Lack of clinical consensus, in relevant community of experts, about the superiority of one treatment over others. a. Ethical concerns during a clinical trial arise in human trials when the investigator(s) begin to believe that one arm of the trial is more beneficial than another i. there is genuine uncertainty over whether or not the treatment will be beneficial E3. Know the ethical considerations in the use of placebos, and the concept of ‘clinical equipoise’. How do these concepts apply to international clinical research? See B&C and Emanuel et al. The use of placebos is controversial in that if there is incomplete disclosure or intentioinal deception involved. The placebo is a substance of intervention that the researchers believe to be inert for the condition being treated. Controversies arise against therapeutic use of placebos without full disclosure mainly due to possible negative consequences. It is also looked down upon due to the failure to respect patient autonomy through deceptive nondisclosure. In defending the use of placebos an appeal is that, a patient has given prior general consent to the goals of the treatment but this isn't necessarily informed consent and it would only be acceptable if the patient was informed of the possible use of the placebo sometime during the study. Sometimes the use of placebo can be instated even without nondiscloscure or deception and the placebo effect can occur if patients have been informed that the substance is inert and that the patient still consents to its use. In clinical trials there's usually an experimental group and a control group, which receives either a standard therapy or placebo so the researchers can determine whether the experimental treatment is more effective and safer than the current standard therapy or the placebo. The clinical equipoise is when researchers do not know prior to conducting the research whether it is more advantageous to be in the control group or in the experimental group. Thus it is okay for the expert medical community to provide treatments of either group because it is not known whether one will be more dangerous than the other. The problem with clinical equipoise is that once a physician knows that one group is more advantageous than the other it is not ethical to provide treatment to any test subjects of either groups. E4. List the elements of informed consent (B&C) & list and explain the standards of disclosure (B&C) Informed consent- no procedure can be performed until the patient or client o 1. Has been informed of the nature of the procedure, risks, alternatives, and the prognosis if the procedure is not done. o 2. Has been determined mentally competent to give or refuse consent. o 3. Has given a free and willing consent to having the procedure done. In emergency situations consent to life-saving treatment is presumed. Standards of Disclosureo Professional practice standard: a professional community’s customary practices determine disclosure. The professional custom establishes the amount and kinds of information to be disclosed. Disclosure is the responsibility of the physicians because they have professional expertise of the patients’ wellbeing. Many legal jurisdictions rely on this method. o The reasonable person standard: the information being disclosed should be determined to a reference to a hypothetical reasonable person. Gaining acceptance in more states. o The Subjective Standard: Judges the adequacy of the information by reference to the specific informational needs of a person. People with different beliefs may require a different informational base than the “reasonable” person. E4. List the elements of informed consent (B&C) & list and explain the standards of disclosure (B&C) a. (Threshold) i. Competence ii. Voluntariness b. (information) i. Disclosure ii. Understanding iii. Recommendation c. (Consent) i. Decision ii. authorization - disclosure o some see this as the only major condition of informed consent o from moral viewpoint, informed consent has less to do with liability of professionals, and more to do with the autonomous choices of the patients/subjects o professionals obligated to disclose core set of info facts/descriptions that patients usually consider material in deciding whether to consent/refuse info that professional believes to be matieral professional’s recommendation purpose of seeking consent nature and limits of consent as an act of authorization o if research is involved, disclosures should cover aims/methods of research, anticipated risks & benefits, any anticipated discomforts, subjects’ right to withdraw at any point without penalty - standards of disclosure o which norms should govern standards of disclosure? a. Professional practice standard i. Professional custom establishes what info is disclosed ii. Responsibility of the physicians iii. Difficulties: 1. Will lead to only expert testimony of physicians to count as evidence of a violation of patients’ right to info a. Abuse! 2. ‘reasonable doctor standard’ a. Does this exist? 3. Subjective measures of what is ‘good’ for the patient 4. Subverts autonomous choice b. Reasonable person standard i. Info to be disclosed determined by reference to a hypothetical ‘reasonable’ person ii. Physicians may be guilty of negligent disclosure if their behavior even if conforms to recognized professional practice iii. Difficulties: 1. How do you define a “reasonable person” and what “material info” they should get? 2. Do patients really use their disclosed info to reach decisions? a. Empirical studies say that only 12% really did, even though 93% believed they did b. Other studies say that patients often accept physician’s advice without carefully doing benefitcost analysis c. Subjective standard i. Reference to the specific info needs of individual 1. Physician must give info if they believe/know that they might want it 2. Preferable moral standard, but it doesn’t work for law/ethics because it doesn’t translate too well practically. 2. o o o o o E4. List the elements of informed consent (B&C) & list and explain the standards of disclosure (B&C) I. Threshold Elements 1) Competence (to understand & decide) 2) Voluntariness (in deciding) II. Information Elements 3) Disclosure (of material information) Professionals are obligated to disclose a set of information containing: 1) Facts or descriptions that patients or subjects usually consider material in deciding whether to refuse or consent to intervention or research 2) Information professional considers to be informational 3) Professional’s recommendation 4) Purpose of seeking consent 5) The nature and limits of consent as an act of authorization Standards of Disclosure: o o o o o Professional Practice Standard (Reasonable Doctor Standard) Holds that the professional community’s customary practices determine adequate disclosure (professional custom determines what type of information is to be disclosed) Difficulties Affecting Standard: 1) Uncertain whether a customary standard exists for the communication of information in medicine 2) If custom, alone, were definite, persistent negligence could be continued with exemption from punishment 3) It is questionable whether many physicians have developed the skills to determine the information that serves their patients’ best interest *Legal jurisdictions rely on this standard Reasonable Person Standard The information to be disclosed should be determined by reference to a hypothetical reasonable person (whether information is important is to be measured by the significance a reasonable person would attach to it Authoritative determination of informational needs shifts from physician to patient. Physicians may still be found guilty of negligent disclosures even if their behavior conforms to this standard Difficulties Affecting Standard: 1) No one has clearly defined the concepts of “material information” or “reasonable person” Study indicated that patients usually make their decisions prior to and independent of the process of receiving information Other studies indicate that patients often accept physicians’ recommendations without carefully weighing the risks and benefits *This standard has gained acceptance in over half of the states in the United States Subjective Standard Judges adequacy of information by reference to the specific informational needs of the individual person, rather than by the hypothetical “reasonable person” Individual needs may differ: Person may have unconventional beliefs, unusual health problems, or unique family histories that require a different informational base than the reasonable person needs If a physician knows or has reason to believe that a person wants such information, to withhold it may undermine autonomy Standard requires the physician to disclose the information a particular patient needs to know, if it is reasonable to expect the physician to know that patient’s informational needs Difficulties Affecting Standard: Patients often do not know what information is relevant for their deliberations, and we cannot reasonable expect a doctor to do an exhaustive background and character analysis of each patient to determine the relevant information Preferable moral standard of disclosure because it alone, meets a person’s specific informational needs 4) Recommendation (of a plan) 5) Understanding (of 3 & 4) III. Consent Elements 6) Decision (in favor of a plan) 7) Authorization (of the chosen plan) E5. Distinguish among the special classes of research subjects and the relevant ethical considerations for each. 1. Prisoners: The question arises if it is fair to use prisoners in experimentation as they already have a bias against them in society, as they are seen as wrong doers. Therefore it is hard to ascertain that they gave informed and voluntary consent for experimentation or were forced into it due to their social position. 2. Children: Firstly the question arises if children are fully competent to make their own decisions. Should they be given the full right to autonomy and at what age? Getting past this issue, another dilemma is should parents have the ability to enroll their child into some sort of research, and is such an act morally justified? How do we know for sure that the parents have the best interests of the child at heart when enrolling their child into research. 3. Patients in emergency treatment: Since the patient in an emergency situation is not able to give consent as he/she may be in a coma etc. the question arises as to whether a decision made without the explicit consent of the patient is valid and justified. Two forms of such consent include “deferred consent” which allows that because the patient is in an emergency situation there is not enough time to contact the family members of the patient so treatment is started, and the family is later contacted after the first dosage to obtain consent for continued study participation. It is also a consideration if community consent is morally valid and acceptable in this situation (the informed consent given by someone other than the patient of research subject), does the community truly have the interests of the patient at heard? 4. Decisionally-impaired subjects: Similar questions arise as the class above. As the patient is unable to make their own informed decision is it justified to obtain consent indirectly from other individuals, and does this violate the patient’s rights to autonomy? 5. Citizens of other countries: Two main issues arise, one regarding the exploitation of the citizens, and the other regarding the image of the United States as an imperialistic state for imposing its own standards. The first point concerns whether justified informed consent will be obtained from the patients, and whether the consent will be voluntarily given. As other countries may have lower economic prosperity and lower education they may be taken advantage of and placed into studies that they do not fully comprehend and do not seek to participate in. Examples of this class include AIDS vaccine trials in Africa. 6. Embryos: The embryo issue is most prevalent in stem cell research studies. A large number of issues arise in this class, for example is the embryo considered alive? Should it be granted the same protection and respect of autonomy as other individuals? Is it justifiable to involve embryos in studies when their consent is not obtained? 7. Animals: While animal testing is much more prevalent, considerations concerning its ethical nature still arise. The issue of morality for example is quite prevalent. Is the study humane? Are the animals being subjected to unfair and harsh conditions? E5. Distinguish among the special classes of research subjects and the relevant ethical considerations for each. Therapeutic privilege i. Physician believes that giving the info would damage the patient – ie depressed/suicidal patient 1. need to consider what the limit is – can you withhold any info at all on the grounds that it will be detrimental to the patient? 2. Other formulations: permit physician to withhold info only if there are serious detriments – ie patient’s decisionmaking process jeopardized 3. Narrowest formulation appeals to incompetence scenario: a. Only can invoke therapeutic privilege if they have sufficient reason to believe that it’ll make someone incompetent to consent, or will make them refuse treatment altogether ii. Respect for autonomy apparently not violated because patient wouldn’t be autonomous if they’re incompetent b. Therapeutic use of placebos i. Arguments against: negative consequences like the decrease in trust of physician ii. Failure to respect patient’s autonomy (respect for autonomy principle) iii. Violates informed consent principle 1. Resolve this by informing them that a placebo might be used on them c. Withholding information from research subjects i. Need to conduct research that probably no one would agree to 1. Ie: epidemiology study – investigation to determine whether a need exists to trace and contact particular individuals who are at risk of disease, and obtain permission for further research 2. Will then notify person, tell them how their data will be used, give them opportunity to refuse/consent 3. Ie: Emory study, participants of STD study didn’t know about the piggy-back study of recent cocaine use, deceived over aims and purposes of the research, but they needed accurate information, and they were pretty sure it’s not something that people would report ii. Problems: violates respect for autonomy and privacy, maybe even nonmaleficence? iii. Can this be justified under the idea that we’re fighting a war on disease and they’re drafted to take risks?’ iv. In general, deception in research that requires people to take significant risks cannot be justified v. Nonmaleficence standard: Permit deception if information is vital, and there’s no substantial risk, must debrief subject \E5. Distinguish among the special classes of research subjects and the relevant ethical considerations for each. o Prisoners: Can they give voluntary, informed consent? Is it fair to use them in nontherapeutic research? o Children: If they cannot give valid consent, is it morally justifiable for parents to enroll them in low- or minimal-risk nontherapeutic research? Debate about use of foster children in AIDS drug trial o Patients in emergency treatment: is community consent or “deferred consent” a moral possibility? o Decisionally-impaired subjects—e.g., psychiatric research o Citizens of other countries—e.g., AIDS vaccine trial in Africa & placebo-controlled trial of reduced dose of AZT to prevent perinatal HIV transmission i. Concerns about exploitation, personal voluntary and informed consent, etc. ii. But also concerns about imperialistic imposition of U.S. standards o Controversy about the use of embryos—particularly in stem cell research o Animals: moral, social, and political conflicts. Animal rights? Animal interests? E6. How would different ethical principles apply to the above discussions? The different ethical principles would apply to the discussions in determining whether or not the research subjects should be part of the experiment despite each of their respective conditions. The ethical principles would be used to justify or condemn research done on particular subjects. Essentially the principles would serve as a screening test for particular cases to determine if it is ethically justified to conduct research on the subject. For example the Nuremberg code could be used to analyze if research conducted on citizens of other countries is valid. Do the citizens give voluntary concent? Will the experiment yield fruitful results? Etc ec. E6. How would different ethical principles apply to the above discussions? 1. Is there a value in the research being done? 2. Is there scientific validity in the facts drawn? 3. Has a fair subject selection been made? 4. Have the favorable risk-benefit ratios been considered? 5. Has an independent review been established? 6. Has the participant given informed consent on the research at hand? 7. Has a respect for enrolled subjects (e.g. privacy) been demonstrated? F1. Explain the difference between formal and material principles of justice. Formal: All theories of justice say that equals must be treated equally, and unequals must be treated unequally. Formal principles do not identify specific requirements as to how equals should be treated and whether or not individuals are in fact equals. The Formal theory essentially lacks substance and defines justice in very vague terms leaving it open to various arguments. For example: Which differences should be compared when assessing the similarities between individuals or groups as equals? And how far should equality extend. Material: Material principles specifically define the relevant characteristics for equal treatment. They are called material because they identify the substantive properties for distribution. Example of a material principle of justice: principle of need – says social resources should be distributed according to need. Other proposed material principles of distributive justice: a) to each person an equal share b) to each person according to need c) to each person according to effort d) to each person according to contribution e) to each person according to merit f) to each person according to free-market exchanges. F1. Explain the difference between formal and material principles of justice. o Formal Principle of Justice (Principle of Formal Equality) o Equals must be treated equally and unequals must be treated unequally Identifies no particular respects in which equals ought to be treated equally and provides no criteria for determining whether two or more individuals are in fact equals o This principle lacks all substance How shall we express equality and which differences are relevant in comparing individuals or groups? How far should equality go although all citizens should have equal political rights, equal access to public services, and equal treatment under the law? To deny benefits to some when others in the same class receive benefits is unjust o Material Principle of Justice o Specifies characteristics that constitute relevant similarities and differences and that a person must possess to qualify for a particular distribution. Examples include: Medical need Ability to pay Age Social value o The following principles have been proposed as a valid, general material principle of distributive justice: To each person an equal share To each person according to need To each person according to effort To each person according to contribution To each person according to merit To each person according to free-market exchanges *A plausible moral thesis is that each of these material principles identify a prima facie obligation F1. Explain the difference between formal and material principles of justice. 1. Formal principle of justice: a. Equals must be treated equally; unequals unequally. b. Identifies no particular respects that helps you discern which between equal and unequal, neither does it give you criteria for determining whether two or more individuals are in fact equals i. What it does: assert that people equal in whatever respects should be treated equally. 2. ii. Lacks substance -> everyone can agree with this sort of logic, but it doesn’t help us figure anything out iii. How do we express equality? How do we define classes that won’t omit anyone who is truly needy? Material principle of justice: a. Principles that specify the relevant characteristics for equal treatment, unlike formal principles, they identify the substantive properties for distribution i. Ie: principle of need: social resources should be distributed according to need, given that it’s a fundamental need – if this need isn’t met, the person will be harmed ii. If we were to analyze the notion of fundamental needs, we could progressively specify and shape the material principle of need into public policy in order to distribute resources 1. Therefore, we have “material principles of distributive justice:” a. To each person an equal share b. To each person according to need c. To each person according to contribution d. To each person according to effort e. To each person according to merit f. To each person according to free-market exchanges 2. Problems : conflicts amongst trying to meet all these principles. F2. Explain the four major theories of justice and their relevance for access to health care. (Arras & B&C) These theories were designed by philosophers to figure out how to distribute social burdens including healthcare. A. Utilitarian Theories: -seek to maximize public utility -regard distributive justice as a problem of maximizing value -utilitarians want rights to be strictly for maximizing net social utility -It is disputed among members of this theory whether or not rights have a meaningful place in moral theory, but if rights were to have an existence that would maximize social utility utalitarians could not object to rights. -agruments against utilitarian theory include that rights such as the right to health care does not have a strong foundation if it is based on utility maximization because social utility can change at any time. -Utalitarian moral theories have helped in forming just health policies, and it presents problems for theory of justice. B. Libertarian Theories -Libertarian theories emphasize rights to social and economic liberty. -Health care in this model is not a right and the ideal health care system is private. -Liberterian model focus on ensures the operation of fair procedures under conditions of the law. -Justice is seen in the operation of just procedures not just outcomes. -Distribution of any good is only justified if the individuals in the relevant group do so out of free will and choice. -They support a health care system in which healthcare is private and voluntarily purchased. -It is relevant because it resembles the modern health care system in the United States C. Communitarian Theory -Stress the principles of and practices of justice that evolve through tradition and practice in a community. -Do not support attempts to make a single theory of justice, but rather believe justice comes from many different conceptions of good. -Emphasize the responsibility of the community to the individual and vice versa. -For example in the Netherlands solidarity is viewed as a collective obligation. -Justice resides in the guarantee that services will be provided to fulfill community goals. D. Egalitarian Theories -Emphasize equal access to the goods that in life that every rational person values. -Hold that persons should receive equal distribution of healthcare. -Qualified egalitarianism allows inequalities along with some basic equalities among individuals, that benefit the least advantaged. -The most celebrated theory of egalitarian justice by John Rawl states that each person be permitted the maximum amount of liberty so that everyone else receives the same. Once this equal liberty is assured additional, inequalities are allowed only if they benefit everyone and they are attached to positions open to all based on fair and equal opportunity. -This theory has been applied to healthcare to argue that barriers should be removed that prevent fair equality of opportunity for healthcare. Diseases are viewed as restrictions on a persons opportunities to realize basic goals. -Allocation of health care resources is designed to make sure everyone has fair and equal opportunity. And each person would have in this model access to adequate levels of healthcare. F3. Explain the fair opportunity rule and its implications for access to health care. No person should receive social benefits on the basis of undeserved advantageous properties, and similarly no person should be denied social benefits on the basis of undeserved disadvantages. An example of such a property is an individuals IQ. Essentially if one is disadvantaged, such as a student with difficulty reading, the system proposes the creation of special schooling that teaches at the same level as the schooling other children are receiving, even if it costs more to run specialized schools. The rule applies to health care in that it allows that individuals with disabilities etc (who have undeserved disadvantageous properties) should be entitled to higher health care services which gives them an equal chance at living. F4. List and explain Emanuel’s seven goals of healthcare reform in Healthcare, Guaranteed. 1. Guaranteed Coverage- 100 % of Americans covered by the new health care plan. Health care is given to unemployed as well as employed. Everyone receives standard benefits without exception—anything else is unacceptable. 2. Effective Cost Controls- Healthcare in the current system is grossly overpriced and many Americans can not afford to pay for it. The price is continually rising as well making it even less likely that Americans can afford it The plan is to make it more efficient by eliminating fraud and expensive administrative fees. In addition we must eliminate the inflation of health care to keep it affordable for all Americans. 3. High Quality Coordinated Care- The extremely high price for health care does not accurately represent the care we actually receive. Patients continually are over treated, undertreated, or treated with unproven drugs. In addition errors are often made and expensive treatments are used which are not medically useful or cost effective. Quality care is a must as many mistakes and failures are made. 4. Choice- Choice is very important for the plan. Choice of physician insurance plan and hospitals are a must for the plan. In addition Americans have the choice to upgrade their plan and pay extra for more expansive coverage as long as everyone has the standard coverage. 5. Fair Funding- Lower-income Americans should not bear the burden for subsidizing the rich. Those who can afford to pay ore for healthcare should prove the social safety net for retired or poor individuals 6. Reasonable Dispute Resolution- Physicians who continue to injure people should not be able to practice anymore. In addition there should be a focus on ensuring that the system protects patients from needless harm rather then compensating them after they are hurt. 7. Economic Revitalization- In the new plan jobs would no longer have to pay for health care so it would allow them to hire based off qualifications not fear of health care costs. By breaking the union between work and health care our economy can benefit by having a more effective work force. In addition it would allow both workers to leave jobs without fear or loosing benefits as well as the ability for couples to divorce without fear of loosing health care. F5. Distinguish between medical utility and social utility. Medical utility- The two components of medical utility are the medical need and probability of success. That means that if a procedure or treatment is necessary for a patient’s health and is very likely to succeed the doctor should proceed. The likelier the success and the more necessary it is the more medical utility the procedure has. Medical utility is reflected in the medical criteria in patient selection. In this case medical utility is the maximization of welfare among patients suffering from end-stage organ failure. Social utility- There are two views of social utility, narrow and broad. The narrow view of social utility is that everything has specific roles and functions within society. The broad view does not simply focus on the on the individual and instead looks at the overall utility for the society. Social utility can be summarized as the maximization of social welfare. F6. What is the concept of triage? How does it illuminate health care distribution? o Triage- emergency treatment concept where you categorize patients according to the severity of the problem… typically people w most life-threatening problems get priority for care. o If you have to ration care, you ideally you would be rationing resources and time, but for health care distribution you are more concerned with resource distribution… you would think severity of the problem would be high on the list of factors to be considered but other factors are involved such as the cost of the care/how you can best martial the cost of the care to help the most number of people. To a degree, health care dist is dependent on triage to a degree, but there are still other things to consider, such as how many people you could help with the dollars that would be spent on expensive procedures for the elderly, for instance. F6. What is the concept of triage? How does it illuminate health care distribution? Triage is a French term meaning “sorting”, “picking”, or “choosing” and can be applied to sorting items. In health care triage is a process of developing and using criteria for prioritization. The objective is to use available medical resources as effectively and as efficiently as possible, appealing to medical utility. In triage you would sort patients based off medical need and the likelihood of the procedure being successful. It is okay under triage to use social worth as long as they have specific qualities that are essential to the community’s immediate protection. An example of this would be vaccinating doctors and nurses first during an epidemic to allow them to help patients with the disease. F7. Explain reasons for and against using age as a criterion for access to health care. (Several articles & B&C) Reasons for and against using age as a criterion in health care: Reasons for using age as a criterion in health care The majority of the American health care expenditures are made by a minority number of elderly people (by 2040 the elderly will represent 21% of the population and consume 45% of the expenditures) An increasingly large share of health care is going to the ederly in comparison with benefits for children- the federal government spends 6 times as much on people over 65 then they do on people under 18 The elderly dying consume a disproportionate share of health care costs Limits on health care would be justifiable because each citizen, through out a life time, would benefit if funds now used to extend life at its end were redirected to earlier stages of life Health care has to be limited because of the limited resources available so that means we must institute rationing. It is morally permissible because there is a limited supply so we must best distribute it. Procedures on elderly often have a much lower medical utility because the success rate is much lower Against using age as a criterion Elderly need the help more so they are obviously going to consume a larger portion of the budget Discrimination is not good- by having health care rationed and using age as a criterion we would be discriminating against the elderly. In addition it would go against fundamental democratic principles The actual savings might not be very large- high cost hospital admissions account for not more then 3.5 percent of Medicare. Only if routine medical care were withheld would the savings be substantial It would increase tensions between generations and devalue the elderly F7. Explain reasons for and against using age as a criterion for access to health care. (Several articles & B&C) o PRO Callahan- elderly people have value according to what role they have/needing to fulfill obligation to society/taking care of young (communitarian view). Once people have fulfilled their purpose, they should be treated with palliative care. Wants to shift societal expectations of healthcare to improving the quality of the lives of the elderly rather than just trying to prolong life. Economic problems: o Elderly dying consume a disproportionate share of healthcare costs o Increasingly large share of health care is going to the elderly in comparison with benefits for children Moral problems: o Shifting the views of health care (from keeping them alive to keeping them happy) o CON Levinsky- correlation between age and the likelihood that the patient will benefit from treatment is not deterministic… if rationing is instituted, resources should be allocated according to the probability that a patient will benefit rather than his/her age. Economic: o Not enough money would be saved by withholding high-cost hospital admissions (only account for 3.5% of medicare).. to make a dent you would have to withhold regular/routine medical care. Moral: o Shift in societal view would decrease the value of the elderly. Thinks that the value of the old is determined by their own accomplishments in their own lives (individualistic/utilitarian view…depends on individual). Using age as a criteria would decrease the value of the elderly… like saying they are worthless Boyle (criticizes Callahan)- again, age correlates with many factors that might make it reasonable to deny health care, but its those factors, not age, that matter. Callahan’s argument doesn’t take into account the fairness of rationing based on age or allocation of scarce resources… he tries to apply his argument regardless of possible scarcities. The use of age as a criterion for rationing is not necessary.. when things need to be rationed, it should be based on medical grounds not age. Allocation vs rationing Allocation- complex, allocate resources on a large scale… determines which sources will be available and what we should use money for/to do. Rationing- simple, who will get the available resources (ie vaccines/treatments). F7. Explain reasons for and against using age as a criterion for access to health care. (Several articles & B&C) o FOR Age is a universal category and concrete enough to be employed for policy purposes. Usually, the very young and very old are most susceptible to disease and have more medical needs. May be an indicator of the probability of surviving a major operation Daniel Callahan: medical care should be used to mitigate suffering, NOT used to resist death and extend life beyond a normal life span Using age as a meter for “fair” lifetime Norman Daniels o o impartial persons would choose (assuming the conditions of scarcity) to distribute health care over a lifetime in a way that improved the chance of attaining at least a normal life span o we would reject a pattern that reduced our chances of reaching a normal life span but increased our chances of living beyond normal life span o An impartial person would choose to shift resources that might otherwise be consumed in prolonging the lives of the elderly to the treatment of younger persons—in this way, we would maximize each person’s chances of living at least a normal life span The “fair innings” argument o Considers a person’s whole lifetime experience and seeks equality o Alan Williams: Intergenerational equality would require, not merely permit, “greater discrimination against the elderly than would be dictated simply by efficiency objectives.” (denying elderly patients treatment when they are in competition with younger patients and resources are scarce) Expected quality and length of life— who will benefit more? Theoretically, a young person will benefit more from a transplant than an elderly person and have a longer time of use of the organ. Ageism: using the judgment that a person is too old as a ground for denying benefits Robert Veatch: the relatively greater opportunity for wellbeing which the elderly have had over the course of their lives weakens their claims on health care in relation to other classes of persons (However, does this devalue the status of the elderly?) AGAINST Risk of perpetuating injustice by stereotyping the elderly treating the elderly as scapegoats because of increased health care costs creating unnecessary conflicts between generations certain age groups complain that they do not have as much access to new technologies that were developed, often using their taxes for funding so the limited resources are “fairly” distributed amongst all age groups with no discrimination may lead to just focusing solely of the health of children, setting a threshold age beyond which funding for various conditions would not be publicly available Usually we are just extending the lives of the elderly but not the quality of those lives Are we focusing too much on the elderly? Unfair allocation of funds? Skewed priority will impose on younger age groups. “Aging and the Ends of Medicine” by Daniel Callahan o In 1980, the 11% of the population over age 65 consumed some 29% of the total American health care expenditures of 219.4 billion; by 1986, percentage of consumption by the elderly had increased to 31% and total expenditures to $450 billion o Medicare costs are projected to rise from $75 billion in 1986 to $114 billion in the year 2000, and in real not inflated dollars. o By the year 2040, it has been projected that the elderly will represent 21% of the population and will consume 45% of all health care expenditures. o YET the present Medicare and Medicaid programs are grossly inadequate in meeting the real and full needs of the elderly—failing in providing decent, long-term care and medical care that does not constitute a heavy out-of-pocket drain. o The federal government spends six times as much on health care for those over 65 as for those under 18. can be unjust in the way that have been implemented in many countries age and social obligation do not correlate not ALL elderly people are in huge medical need also, (Joseph Boyle) rejecting age as a basis for rationing does not imply that, in making allocation decisions, we should give any settled, definite priority to the health needs of the elderly as a group—one can address the complexities instead F7. Explain reasons for and against using age as a criterion for access to health care. (Several articles & B&C) FOR B&C Probability of successful treatment, i.e. medical utility Age may be an indicator of the probability of, say, surviving a major operation o Judgments of the probability of success can also include the length of time that the recipient of an organ is expected to survive Usually shorter for older patients than younger patients Norman Daniels’ argument: Age should be viewed differently from race and gender for purposes of healthcare allocation o Consider the perspective of an entire lifetime o Each age group represents a stage in a person’s life span o Goal: to allocate resources prudently throughout the stages of life within a social system that provides a fair lifetime share of healthcare for each citizen o Assuming conditions of scarcity, an impartial person would choose to distribute healthcare over a lifetime in a way that improved the chance of attaining at least a normal life span o We would reject a pattern that Reduced our chances of reaching a normal life span but Increased our chances of living beyond a normal life span if we did become elderly o An impartial person would choose to shift resources that might otherwise be consumed in prolonging the lives of the elderly to the treatment of younger persons To maximize each person’s chances of living at least a normal life span “Fair innings” argument o Considers a person’s whole lifetime experience o Seeks equality o Alan Williams (proponent) This conception would require “greater discrimination against the elderly than would be dictated simply by efficiency objectives.” “Aging and the Ends of Medicine” by Daniel Callahan Providing equal or more access to healthcare for the elderly will o Impose great economic burdens on younger age groups This is a huge burden because the elderly are likely to require more healthcare than the young o Suggest to both the young and the old that they key to a happy old age is good health care This may not be true An increasingly large share of health care is going to the elderly in comparison with benefits for children o The federal government spends 6 times as much on healthcare for those over 65 as for those under 18 o Demographer Samuel Preston, in a presidential address to the Population Association of America in 1984 “… the transfers from the working-age population to the elderly are also transfers away from children, since the working ages bear far more responsibility for childrearing than do the elderly.” o The elderly dying consume a disproportionate share of healthcare costs Stanford economist Victor Fuchs: “At present, the United States spends about 1 percent of the gross national product on health care for elderly persons who are in their last year of life…” o Jerome L. Avorn, M.D. of the Harvard Medical School “With the exception of the birth-control pill, each of the medical-technology interventions developed since the 1950s has its most widespread impact on people who are past their fifties – the further past their fifties, the greater the impact.” Future goal of medicine in the care of the aged should be that of improving the quality of their life, not in seeking ways to extend that life o This, however, would be equivalent to asking medicine to restrain itself in the face of aging and death o In order for the public to accept this, two conditions must be met and understood It is possible to live out a meaningful old age that is limited in time, one that does not require a compulsive effort to turn to medicine for more life to make it bearable As a culture, we need a more supportive context for aging and death One that cherishes and respects the elderly while at the same time recognizing that their primary orientation should be to the young and the generations to come, not to their own age group Recognize that in the passing of the generations lies the constant reinvigoration of biological life o One should also consider what it means to live a decently long and adequate life – a natural life span Modern medicine and technology have conditioned us to think that the average life span is not a natural fact but is instead dependent upon the state of medical knowledge and skill Hence, the average life expectancy continues to increase, with no end in sight o Longer life does not guarantee better life Death due to old age, though sad, is just part of life itself Medical “need” can no longer work as an allocation principle o Too elastic a concept A person of 100 dying from congestive heart failure “needs” a heart transplant no less than someone who is 30 Are we to treat both needs as equal? Not economically feasible to do so Age is a meaningful and universal category o It can be understood at the level of common sense o Concrete enough to be employed for policy purposes o It can be of value to the aged themselves if combined with an ideal of old age that focuses on its quality rather than its indefinite extension Example: the British health care system o Tacit allocation policy that emphasizes improving the quality of life through primary care and home care rather than life-extending acute care medicine o Well-known difficulty in getting dialysis after 55, restrictions on access to open heart surgery and other forms of expensive technology o As a result, the British spend a significantly smaller proportion of their GNP (6.2%) on health care than Americans (10.8%) for an almost identical outcome in health status AGAINST B&C Using age as a criterion for access to healthcare may cause society to run the risk of perpetuating injustice by o Stereotyping the elderly o Treating them as scapegoats because of increased health care costs o Creating unnecessary conflicts between generations Elderly persons in each generation will complain that They did not have access to new technologies that were developed, although these technologies were funded by them through tax Unfair to deny them those technologies now “Aging and the Ends of Medicine” by Daniel Callahan Although proponents argue that the elderly receive a disproportionate share of resources, what helps the elderly helps every other age group o The young will eventually face the same problems and require treatment when they age o Guarantees them treatment if they need it There is no guarantee that any cutback in healthcare for the elderly would result in a transfer of the savings directly to the young Why should we contemplate restricting care for the elderly when we wastefully spend hundreds of millions of dollars on an inflated defense budget? The charge that the elderly dying receive a large share of funds hardly proves that it is an unjust or unreasonable amount o The elderly are, after all, the most in need “Age as a Criterion for Rationing Health Care” by Norman G. Levinsky Why is it acceptable to propose limits on health care for the elderly, in contrast to the obvious unacceptability of such a proposal applied to other groups and classes of citizens such as blacks or women? Only if routine medical care were withheld would the savings be substantial o Medicare data by Scitovsky indicates that high-cost hospital admissions account for no more than 3.5 percent of Medicare expenditures This saving is achieved at the cost of lives o Even this overstates the proportion of medical care costs for the elderly that are devoted to intensive, high-priced hospital care The noneconomic costs of a national policy to restrict routine care for the elderly would be high Medical care that extends life devoid of human qualities should not be undertaken, but this principle should apply equally to patients of all ages, not only to the elderly o Should we continue to treat younger patients vigorously, even though their prognosis is worse than that of otherwise healthy elderly persons with pneumonia? To achieve acceptance of such intuitively distasteful measures would require a societal reeducation effort that would exacerbate tensions among the generations and further devalue the status of the elderly o American attitudes: emphasis on youth and devaluation of the aged in American society Restrictions would not, in practice, be applied equitably o Were lifesaving medical care to be denied to Americans beyond a certain age, some citizens would nevertheless obtain care by dint of wealth, social standing, personal connections, etc. o The intent might be equitable, but the outcome would not be fair o Eg. Although for many years informal policy in Great Britain discouraged dialysis or transplantation for patients over 55, older persons who could “work for the system” were nevertheless accepted for treatment o Eg. Before 1973, patients who managed to obtain dialysis were disproportionately white, middle-class men with relatively high educational status STRIKING A BALANCE? B&C Need to set a threshold age beyond which funding for various conditions would not be publicly available But we still need to proceed with caution o Although it is fair, the implementation of age-based criteria for access to healthcare has been unjust in many countries. “Aging and the Ends of Medicine” by Daniel Callahan The proper question is not whether we are succeeding in giving a longer life to the aged It is whether we are making of old age a decent and honorable time of life This can be done by changing society’s perspectives, expectations, attitudes towards the elderly, etc. F8. Explain reasons for and against using alcoholism as a criterion for access to liver transplantation. FOR “Should Alcoholics Compete Equally for Liver Transplantation?” by Alvin H. Moss and Mark Siegler Alcoholism is a chronic disease o Treatment is available and effective High success rates of some alcoholism treatment programs Therefore, patients can accept responsibility for their treatment o Patients with alcohol-related end-stage liver disease (ARESLD) develop the disease only after 10 to 20 years of heavy alcohol consumption In view of the number of years of heavy alcohol consumption required, as well as the availability and effectiveness of alcohol treatment, attributing personal responsibility for ARESLD to the patient seems all the more justified ARESLD is different from other critical diseases because of the scarcity of the resource needed to treat it o This difference permits us to make some discriminating choices – or to establish priorities – in selecting candidates for liver transplantation based on notions of fairness AGAINST “Should Alcoholics Compete Equally for Liver Transplantation?” by Alvin H. Moss and Mark Siegler Why should patients with ARESLD be singled out when a large number of patients have health problems that can be attributed to so-called voluntary health-risk behavior? o E.g. smokers with chronic lung disease; obese people who develop type II diabetes; etc. We could rightly preclude alcoholics from transplantation only if we assume that qualification for a new organ requires some level of moral virtue or is canceled by some level of moral vice o But there is absolutely no agreement as to what constitutes moral virtue and vice and what rewards and penalties they deserve o Even if we could agree upon the kind of misconduct we would be looking for, the fair weighting of such a consideration would entail highly intrusive investigations into patients’ moral habits Some drinkers have a greater predisposition for alcohol abuse than others o For some who drink in excess, the predisposition to cirrhosis is also greater o Penalizing cirrhotics by denying then transplant candidacy would have the effect of holding some groups arbitrarily to a higher standard than others and would probably hold women to a higher standard of conduct than men Medical argument o The premise that the outcome for alcoholics will invariable be poor relative to other groups is at least doubtful and probably false o Even if the premise were true, it could serve as a good reason to exclude alcoholics only if it were an equally good reason to exclude other groups having a prognosis equally bad or worse F8. Explain reasons for and against using alcoholism as a criterion for access to liver transplantation. Reasons for and against using alcoholism as a criterion for access to liver transplant: For using alcoholism as a criterion Livers are very scarce and so they must be subject to a much more rigorous standard Alcoholism is a disease, but one that is easily and effectively cured Individuals should bear some responsibility for their actions In the issue of fairness people who by no fault of their own contract ESLD (end-stage liver disease) should have a higher priority then those whose liver disease results from failure to obtain treatment for alcoholism. Against using alcoholism as a criterion Alcoholism is a disease so it should not be used as a discriminatory criterion Why should alcoholism be singled out when the medical profession treats many patients who engage in behavior that causes their diseases Everybody deserves in equal share of treatment F8. Explain reasons for and against using alcoholism as a criterion for access to liver transplantation. b. PRO i. since the health care resources are so scarce, patients with ARESLD should not compete equally with other candidates for liver transplantation because they engaged in behavior that caused their own diseases… a priority ranking should be established. ii. This pertains mostly to patients who have made no effort to correct their problem/receive treatment. alcoholics who have done so would be higher on the priority list. c. CON i. Cant not allow them to have the transplant based on moral/medical reasons… ii. otherwise all other medical problems caused by the individual should not be allowed to have treatment iii. Just because the transplants might not be as successful for the alcoholics does not mean they should be excluded from transplants because that rule does not apply to other treatments F8. Explain reasons for and against using alcoholism as a criterion for access to liver transplantation. o FOR Liver donations are SCARCE and nonrenewable, and transplantations are very expensive; no therapies to treat and cure Alcoholics are much more morally blameworthy of their condition. Moss & Siegler: patients who develop end-stage liver disease through no fault of their own should have higher priority for receiving a liver transplant than those whose end-stage liver disease results from failure to obtain treatment for alcoholism if using a first-come, first-serve approach, patients with alcohol-related end-stage liver disease receive more than half the available donor livers Moral argument of fairness; principles To each, an equal share of treatment o Ex: child dying of biliary atresia has priority over ARESLD patient born with a normal liver and needing a second one this is the moral intuition of the public To each, similar treatment for similar cases o Using the example above, the child’s case was less preventable; therefore, it is acceptable to treat them differently To each, treatment according to personal effort o Although alcoholism is a disease, while alcoholics may not be held responsible for their disease, they can still be held responsible for seeking and obtaining treatment that could prevent the development of late-stage complications such as ARESLD. ex: Alcoholics Anonymous To each, treatment according to ability to pay o Distributive justice o Poor ARESLD patients are less able than rich patients to pay for alcohol treatment programs; therefore, the poor patients hold greater claim for a donor liver. Less public support for ARESLD patients receiving transplants Medicare coverage for liver transplantation be offered to patients with alcoholic cirrhosis who are abstinent However, how long should abstinence necessary to qualify for transplantation? Alcoholics have a high recidivism rate (tendency to relapse) and, according to a 1988 report, usually have a lower survival rate after transplantation than nonalcoholic patients. o AGAINST Criterion should be NEED Survival rate between patients with ARESLD (alcohol-related end-stage liver disease) and patients with ESLD (endstage liver disease) are comparable Patients with ARESLD represent more than 50% of the patients with ESLD, they account for less than 10% of those receiving transplants (1990) Since alcoholism is a disease, ARESLD patients should be considered equally Influenced genetically, environmentally, etc. Weakness of will Because it is a disease, it is legitimized that it requires medical treatment Also, because it is a chronic disease, it is hard for people to just stop drinking Why are ARESLD patients singled out for discrimination, when the medical profession treats many patients who engage in behavior that causes their disease? Smokers = chronic lung disease Obese people = type II diabetes Sex = HIV, STDs, etc. Sports = injuries No seat beats = vehicular accidents We do not use moral evaluation in deciding treatments to patients Don’t base on whether a person is abusive, routinely lies or cheats, etc. How accurate was the representations of the 1988 report? Even if alcoholics have a little more difficulty recovering after the transplant, other groups who have harder chances of recovering are NOT excluded from transplants. Is this fair? Cohen & Benjamin: You should not refuse a liver because of alcoholism, but if you are to judge on the basis of drinking, you must have the following guidelines because they are more reliable predictors: Refined diagnosis by those trained in the treatment of alcoholism Acknowledgement by the patient of a serious drinking problem Social and familial stability Other factors experimentally associated with long-term sobriety F9. Describe how Emanuel & Wertheimer would allocate influenza vaccine in a pandemic & their reasons Rationing o Inescapable because of its current uncertainty of its value o Demand greatly exceeds supply o Rationed according to… Life-Cycle Principle o Save-the-most-lives principle may be justified in some emergencies when decision urgency makes it infeasible to deliberate about priority rankings and impractical to categorize individuals into priority groups o Each person should have an opportunity to live through all the stages of life is more appropriate for a pandemic Great value in being able to pass through each life stage o Most people would endorse this principle for themselves o People strongly prefer maximizing the chance of living until a ripe old age, rather than being struck down as a young person The Investment Refinement o Emphasizes gradations within a life span o Gives priority to people between early adolescence and middle age on the basis of the amount the person invested in his or her life balanced by the amount left to live Public Order o Focuses on the value of ensuring safety and the provision of necessities such as food and fuel o The investment refinement combined with the public-order principle (IRPOP) should be the ultimate objective of all pandemic response measures, including priority ranking for vaccines and interventions to limit the course of the pandemic, such as closing schools and confining people to homes F9. Describe how Emanuel & Wertheimer would allocate influenza vaccine in a pandemic & their reasons o Rather than thinking only about saving the most lives when considering vaccine rationing strategies, a better approach would be to maximize individuals’ life span and opportunity to reach life goals. o Priority should be given to vaccine production and distribution workers as well as health care and public health workers with direct patient contact o Investment refinement combined with the public-order principle (IRPOP) should be the ultimate objective of all pandemic response measures, including priority ranking for vaccines and interventions to limit the course of the pandemic o Priority should be given to vaccine production and distribution workers as well as health care and public health workers with direct patient contact. Also emphasize people between early and adolescence and middle age… the basis of the amount the person invested in his/her life balanced by the amount left to live. o IRPOP: Investment refinement of life-cycle principle (LCP) including public order Life-Cycle Principle: based on the idea that each person should have an opportunity to live through all the stages of life is more appropriate for a pandemic Most people support this principle for themselves; we prioritize our own resources to ensure we could live past the illnesses of childhood and young adulthood and would allocate fewer resources to living even longer once we reached old age. People strongly prefer maximizing the chances of living until a ripe old age, rather than being struck down as a young person egalitarian The Investment Refinement: Gives priority to people between early adolescence and middle age on the basis of the amount the person invested in his or her life balanced by the amount left to live (13-40 year olds) Public Order: focuses on the value of ensuring safety and the provision of necessities, such as food and fuel IRPOP: Top priority: 13-40 year olds with less than two high-risk conditions with priority to key government leaders; vaccine production and distribution workers, public health workers; military, police, and fire workers; telecommunications and IT workers; funeral directors Next priority: 7-12 year olds and 41-50 years old with less than two high-risk conditions with priority as above Next priority: 6 months to 6 year olds and 51-64 year olds with less than two high-risk conditions with priority as above Next priority: 65 and older with less than two high-risk conditions Is meant to apply to the situation in the United States Depending on patterns of flu spread, some mathematical models suggest that following IRPOP priority ranking could save the most lives overall. F9. Describe how Emanuel & Wertheimer would allocate influenza vaccine in a pandemic & their reasons Emanuel and Wertheimer would allocate influenza vaccine based on a life-cycle allocation principle. They argue that each person should have an equal right of living a long and healthy life and they should all be given an equal opportunity to live through all the stages of life. Their point is that they would refrain from giving medicine to a 65 years old versus a 7 year old, only because that child has not had a chance to live yet. "Death seems more tragic when a child or young adults dies than an elderly person – not because the lives of older people are less valuable but because the younger person has not had the opportunity to live and develop through all stages of life." F10. How would different ethical principles apply to the above discussions? Doctors have the obligation to prevent harm as well (Beneficence) and from preventing the elderly from getting the medication they are pretty much letting them die. One could also argue discrimination against a certain age group. Though elderly have lived a longer life, who is to say that it has been a fulfilling one and who has the right to tell them that a child's life is more important than theirs'. F10. How would different ethical principles apply to the above discussions? Age as a criterion for access to healthcare Equity o Medical care that extends life devoid of human qualities should not be undertaken But this principle should apply equally to patients of all ages, not only to the elderly o Even if access to healthcare is restricted by age, people can still find ways to work around the system Evidenced by the British healthcare system This gives an unfair advantage to those with financial resources, social status, personal connections and the like. Alcoholism as a criterion for access to liver transplantation Fairness o To each, an equal share of treatment Liver transplantation: impossible to give patients “equal share” because a liver cannot be shared o To each, similar treatment for similar cases Patients with ARESLD are unequal in a relevant respect to others with ESLD since their liver failure was preventable; therefore it is acceptable to treat them differently o To each, treatment according to personal effort Although alcoholics cannot be held responsible for their disease, once their condition has been diagnosed they can be held responsible for seeking treatment and for preventing the complication of ARESLD o To each, treatment according to ability to pay Since alcoholism is prevalent in all socioeconomic strata, it is not discrimination against the poor to deny liver transplantation to patients with alcoholic liver disease In fact, poor patients with ARESLD have a stronger claim for a donor liver than rich patients because they have less financial resources to seek treatment for alcoholism Allocation of influenza vaccine in a pandemic “Save the most lives” o Common in emergencies “Women and children first” o Used on the Titanic “First come first served” o Operates in other emergencies and in ICUs when admitted patients retain beds despite the presentation of another patient who is equally or even more sick “Save the most quality life years” o Central to cost-effective rationing “Save the worst-off” o Plays a role in allocating organs for transplantation “Reciprocity” o Giving priority to people willing to donate their own organs o Proposed but probably not practiced yet “Save those most likely to fully recover” o Guided priorities for giving penicillin to soldiers with syphilis in World War II “Save those instrumental in making society flourish” o Through economic productivity or by “contributing to the well-being of others” F10. How would different ethical principles apply to the above discussions? life-cycle allocation principle: o Great value in being able to pass through each life stage and enjoy range of opportunities o Most people would endorse this principle for themselves—people prefer to maximize their chance of living until a ripe old age (death seems more tragic when a child dies) Fair to all because everyone will live to be older unless life is cut short Gradations within a life span: o priority to people between early adolescence and middle age based on investment in life left to live Public Order: ensuring safety and provision of necessities o Highest ranking to vaccine production and distribution workers and people with direct patient contact Groups at risk F10. How would different ethical principles apply to the above discussions? 3. Justice: a. All of the above discussions (F) deal with justice. Justice is interpreted as what is “fair, equitable, and appropriate treatment in light of what is due or owed to persons.” However, what is justice is perceived differently by different people. There are also different kinds of justice: formal and material and certain other variations. 4. Respect: a. The above discussions do not really involve a lot of the respect principle, in regards of respected individual’s autonomy and decisions. In #4, in Emanuel’s plan, all people are provided with basic health care (egalitarian), but people also have the option of upgrading their health care by paying for it themselves if they desire it. 5. Beneficience: a. In all of the discussions, there is beneficience involved and utilitarianism is usually the popular concept applied; still, different groups of people benefit more than others in certain discussions, usually to comply with the fair-opportunity rule. For instance, in #7, the elderly people are the people benefiting the most out of the system, as opposed to the other age groups; however, we support this because we believe that the elderly are the most in need of medical attention, so it would be beneficial to give them more treatments. In concepts such as triage (#6), the situation is similar—the people in worse medical condition are given more treatments. However, in #9, it is the people who have most potential who are benefiting the most, and the lowest priority is given to the elderly. 6. Nonmaleficience: a. “Do no harm”—in the above discussions, they do not directly cause nonmaleficience, some only caused indirectly by not giving certain people treatment (such as in #8). 7. Utility/Proportionality: a. In the above discussions, although they are regarding justice, not all people benefit since you have to consider limited resources and services. Therefore, in many of the discussions, the utilitarian concept is applied—so there is maximum welfare among the whole population—and also the fair-opportunity rule (such as #6 and #7). However, people have different ideas of how to produce maximum welfare. In #4, Emanuel proposes a universal healthcare plan, which benefits everyone. However, in #8, people are divided by who gets priority because of the argument of “fairness”—alcoholics with ESLD (ARESLD) or nonalcoholics with ESLD, despite the ARESLD majority. Also, in #9, it is hypothesized that IRPOP plan would provide maximum welfare in the U.S. in the case of providing vaccinations although it depends of the patterns of disease spread (flu). G1. Know the arguments for & against voluntary/mandatory and universal/selective screening for HIV infection. Voluntary Universal screening is completely up to the individual without any incentives provided by another party. While, compulsory universal screening is forced on people. Both of these screenings were unjustified since universal screening of any type would require a lot of resources and may even prove to be unnecessary. Since HIV infections are more likely to be present in certain conditions/environment, universal screening is just a waste to resources and would also provide false results. However, B & C do say that no. 1 could be justified since HIV is more of a chronic disease now but the cost and the benefits from the results still make both of these screening methods unjustifiable. The second one cannot be justified since it takes away an individual's autonomy and freedom of choice. Voluntary selective screening is using only certain groups in a community and giving them the choice to be tested for HIV like newborns and pregnant women. It is justified since benefits outweigh the risks but there is debate about who should be responsible for the payment and what about those patients who are unable to pay. It should still be kept in mind that this is still voluntary and the test could be refused. However, concern is present for those who may be HIV positive since it would be a psychological, and social burden on those. However, it is justified since not telling individuals would risk those around them. Compulsory Selective screening is partly justified and this is the case where a group is forced to be tested. They can be needed in cases where there is risks to others without their knowing about it like in blood donations. G1. Know the arguments for & against voluntary/mandatory and universal/selective screening for HIV infection. Screening that identifies individual involves loss of privacy (if anonymous, no privacy loss) Voluntary rests on encouragement rather than coercion –doesn’t violate any moral rights of privacy and autonomy Universal screening not necessary to protect the public health o HIV only affects those engaged in “high-risk activities” If screen groups with low prevalence there will be a high rate of false positives o Universal screening very costly, not cost-effective Because various conditions can change (ie technologies created to reduce false positive at a low cost), position doesn’t oppose universal testing in principle Voluntary-selective screening justified because people engage in unsafe practices o Questions still remain of who should be encouraged to be tested, who should bare costs, pre- and post test counseling that should be offered, conditions that make the decision to undergo testing reasonable HIV screening has big benefits and risks including actions taken by person once results revealed o Psychological and social effects as well Compulsory-selective – only compulsory to a degree because patients choose whether or not to enter situation or institution where screening is mandatory o Justifiable when person engaged in actions that impose risks on others who can’t avoid risks (sperm donation, etc) o Issues when involving pregnant women or newborns G1. Know the arguments for & against voluntary/mandatory and universal/selective screening for HIV infection. Voluntary-universal screening For: It does not violate any moral rights of privacy or autonomy. It rests on encouragement and choice. Against: It is cost-ineffective because HIV infection is not widespread outside groups engaging in high-risk activities. Screening in groups with low prevalence of HIC infection is not necessary to protect the public health. Compulsory-universal screening According to B&C, it is impossible to justify compulsory universal HIV screening because (1) it rests on coercion, and thus violates moral rights of privacy or autonomy. (2) it fails in terms of cost-effectiveness and cost-benefit assessments as HIV infection is not widespread outside groups engaging in high-risk activities. Voluntary-selective screening For: it does not violate any moral rights of privacy, and the benefits of HIV testing outweigh the risks for individuals. It is especially justified in groups with high rate of unsafe sexual practices, needle sharing in intravenous drug use, and pregnant women and newborns. Against: It is difficult to determine who should be encouraged to be tested, who should bear the costs, which sorts of pre-and posttest counseling should be provided, and which conditions make the decision to undergo the test reasonable for individuals. Compulsory-selective screening For: it is justified on grounds that persons engage in actions or are involved in procedures that impose risks on others who cannot avoid those risks: donation of blood, organs, and sperm; employment (exposure to bodily fluids could transmit the virus); foreign service; institutional settings, such as the military, prisons (high rate of HIV infection), and schools; marriage licenses; insurance; hospital admissions; immigration; pregnancy (antiretroviral treatments can reduce the transmission of HIV infection to the child, but it might also discourage pregnant women from seeking prenatal care); etc. Against: since it is compulsory, it violates individuals’ moral right of privacy. It is selective so it encounters the same ethical difficulties as the voluntary-selective screening (who should be encouraged to be test…). B&C’s objection of voluntary/compulsory-universal screening is subject to reversal as more effective treatments for HIV became available and made HIV more of a chronic condition. G1. Know the arguments for & against voluntary/mandatory and universal/selective screening for HIV infection. a. For voluntary-universal screening: rests on encouragement and choice and does not violate in itself any moral rights of privacy or autonomy. b. Against universal screening: It is not necessary to protect the public health. It would be very costly and ineffective. HIV is not so common outside of groups of those engaging in high-risk activities and screening in groups or areas with low prevalence of HIV infection produces false positives, especially without confirmatory testing c. d. e. f. g. For voluntary-selective screening: can be justified for those who practice unsafe sex, share needles in intravenous drugs, and for pregnant women and newborns. Pro voluntary screening: It is the most respectful option of a person’s privacy and autonomy. Against voluntary-selective screening: Questions arise on who should be tested, who should pay the fees, what sort of pre and post counseling should be provided, and what conditions make the decision to undergo the test reasonable for individuals. For mandatory-selective screening: appears to be a good public health strategy to reduce spread of HIV infection. It can be justified in areas where persons engage in actions that impose risks on others who cannot avoid those risks. (Example: blood donation, organ donation…) Against mandatory screening (pro voluntary): The individual who is screened risks the possibility for some loss of privacy since others can gain access to that private information. Would probably be ineffective and counterproductive. (pg 299 C&S) G2. Distinguish between privacy and confidentiality, and know major arguments about rules of confidentiality in relation to HIV/AIDS. (See also Applied Human Genetics) Confidentiality is the safekeeping of information disclosed in a trusted relationship. With confidentiality the confider has willingly given information to a second party entrusting him/her with its safe keeping. The major difference between confidentiality and privacy is that a breach in confidentiality occurs when the second party deliberately discloses information to others without the individual's consent. Invasion of privacy can be done by a party completely uninvolved with the original trade of information and it could be someone who is trying to get information that they never (ever) had access to without consent. In favor of breaking confidentiality – when there is a chance that others in the HIV positive person's life could be prevented from harm or could be treated for harm. In the case where the husband has it and refuses to tell his wife, who later turns out to be HIV positive – the doctor has an obligation to prevent his patient from inflicting harm on to others in his life. Below are the steps that a physician should follow in such a case. 1: try and persuade his patient to let his loved ones know, 2; if he refuses and there is chance of harm, inform the authorities, 3: if authorities don't do anything then it is within physician's responsibilities to inform the third party (case about the psychologist and man wanting to kill). Even if the person promises to have safe sex but refuses to tell partner, physician has the duty to disclose. However, he should first try and get patient's permission to go ahead with disclosure but his refusal will not limit the physician. G2. Distinguish between privacy and confidentiality, and know major arguments about rules of confidentiality in relation to HIV/AIDS. (See also Applied Human Genetics) Privacyo obligations of privacy and confidentiality affect controversies over policies to control to spread of HIV Proposals to screen individuals to determine whether they are antibody positive tor HIV threaten loss of privacy Obligations of confidentiality questioned when HIV patients refuse to inform or allow physicians to inform their spouses of their condition Lose some privacy when grant others access to personal histories or bodies but can still retain confidentiality o Confidentiality is a branch of information privacy – prevents re-disclosure of information that was originally disclosed within a confidential relationship Difference: infringement of person’s right to confidentiality occurs when person to whom the info was disclosed in confidence fails to protect information o Only person who receives information in a confidential relationship can be charged with violating rights of confidentiality G2. Distinguish between privacy and confidentiality, and know major arguments about rules of confidentiality in relation to HIV/AIDS. (See also Applied Human Genetics) Privacy: state or condition of limited access to a person. It is not merely an agent’s control over or a right to. A person can have privacy without having any control over access by others. Privacy includes informational, proprietary, physical, decisional, and relational or associational privacy. Confidentiality: it is a branch of informational privacy that prevents redisclosure of information originally disclosed within a confidential relationship in which the source of information controls access, by third parties, to that information. The basic difference between privacy and confidentiality is: an infringement of a person’s right to confidentiality occurs only if the person to whom the information was disclosed in confidence fails to protect the information or deliberately discloses it to someone without first-party consent. (for example, you doctor discloses your medical record to insurance company without your consent) By contrast, a person who, without authorization, obtains information about another person violates rights of privacy of that person. Confidentiality of an HIV positive patient is prima facie and can be overridden on some conditions. For example, if people (spouses or lovers) are at risk of serious harms, and the disclosure is necessary to prevent and probably would prevent the harms, then disclosure that breaks confidentiality is justified. The patient’s permission is not a necessary condition for warning an endangered third party. However, controversy arises in terms of the nature, scope, and strength of the clinician’s ethical obligation to protect the third parties. In addition, one consequentialist argument suggests that people who have been exposed to the AIDS virus but do no yet have symptoms will be reluctant to seek testing unless confidentiality is protected. (Counterargument: HIV infection and AIDS are defined as chronic diseases, people will still seek testing and treatment if confidentiality is breached under limited conditions). In addition, values of the exercise of autonomy and the right to control one’s privacy support rules of confidentiality. G2. Distinguish between privacy and confidentiality, and know major arguments about rules of confidentiality in relation to HIV/AIDS. (See also Applied Human Genetics) 2. The main difference is that: “an infringement of a person’s right to confidentiality occurs only if the person (or institution) to whom the information was disclosed in confidence fails to protect the information or deliberately discloses it to someone without first party consent. In contrast, a person, who without authorization, enters a hospital record room violates privacy, although he/she may also obtain confidential information. Only the person who obtains info in a confidential relationship can be charged with violating rights of confidentiality” (303 C&S). a. In a way, confidentiality is a branch of informational privacy 3. The disclosure of information to a third party, that breaks confidentiality, can be justified if that party is at risk of being harmed by the person who is infected with HIV/AIDS. 4. According to the AMA’s council on ethical and judicial affairs: “A physician ‘who knows that a seropositive individual is endangering a third party…should, within the constraints of the law, (1) attempt to persuade the infected patient to cease endangering the third party; (2) if persuasion fails, notify authorities; and (3) if the authorities take no action, notify the endangered third party” (308 C&S). Disclosure can be justified because the primary concern of health professionals is to reduce the risk of death in certain cases that are under their control. 5. A consequentialist argument in opposition to that above, is that those who have been exposed to AIDS virus but do not yet have symptoms will be less willing to agree to be tested unless they know that confidentiality will be protected. Therefore, they would not be receiving important information that could lead them to protect others from contracting the disease. 6. C&S also argue that it is important to notify the patient before disclosing information to a third party, but omitting to do so does not mean that such a disclosure of info is unjustified; the patient’s permission to notify a third party is not necessary. “Without prior notification, the physician breaches confidentiality but may be justified in doing so; with prior notification, the physician breaches privacy but not confidentiality” (308) 7. Klitzman and Bayer found in a study that, “many HIV-infected persons prefer to see confidentiality breached to prevent another person’s infection (309)” G3. Explain arguments for and against directly observed therapy in controlling TB (in B&C) Has been used to protect public until patient becomes non-contagious or cured Not just paternalistic rationale, but to protect others For directly observed: o To protect others over time o If patients don’t continue treatment, risk of developing multidrug-resistance forms—threat to others and themselves o Risk also of escalation of treatment cost Against: o Because the majority of TB patients comply, would be “wasteful, inefficient and gratuitously annoying” to mandate DOT o Most restrictive and intrusive intervention for some patients In some cases, DOT is justifiable, other cases must respect privacy and autonomy Effective strategy: to pay attention to conditions that cause TB and emphasize policies with privacy and freedom of choice Coercive measures justified to protect public health but give priority to least restrictive measure (induced DOT should be considered before mandatory) G3. Explain arguments for and against directly observed therapy in controlling TB (in B&C) 8. For: TB is spread by airborne emission and mandatory screening can be easily justified if others are put at risk to be contaminated. If directly observed therapy is not enforced, TB could continue to spread and treatment costs could rise. DOT is justified when its motive is to protect public health and it is issued in the least restrictive and intrusive manners. 9. Against: Critics argue that since most TB patients adhere to treatment, it would be wasteful to mandate DOT to all patients. Also, implementing DOT, would fail to implement the least restrictive and intrusive method for certain patients. G3. Explain arguments for and against directly observed therapy in controlling TB (in B&C) For: TB is spread by airborne transmission. Directly observed therapy is justified because it protects the public from people shown to have active TB and prevent further spread of TB, particularly its multidrug-resistant forms. Against: As the majority of TB patients comply with the treatment, it is wasteful and inefficient to make DOT for all patients with TB. Plus, it fails to select the least restrictive and most effective intervention for particular patients. It also violates both privacy and autonomy. G3. Explain arguments for and against directly observed therapy in controlling TB (in B&C) Because TB is spread by airborne transmission, easier to justify infringement of privacy and autonomy. Mandatory TB screening and directly observing patients take their medications is justifiable if substantial risk of transmission exists (like in crowded workplaces or prisons). For DOT: 1/3 of patients with TB fail to adhere to treatment, and when they do not continue prescribed TB treatment until they are cured, multidrug-resistant TB arises. Spread of TB and the rising costs also important reason for trying to prevent spread of TB. Against DOT: believe that since a majority of TB patients comply, this would be wasteful and inefficient. Also, DOT is not the least restrictive and intrusive intervention for particular patients. Childress: mandated DOT that intrudes privacy is justified when needed to protect public health, but priority must be assigned to least restrictive and least intrusive measures. G4. Identify and discuss the 4 key ethical issues in pandemic influenza raised by Stand on Guard for Thee 1. “Health Workers’ duty to provide care during a communicable disease outbreak: o Government and health care sector should ensure that care providers safety is detected and providers can discharge duties and receive support. Human resource strategy to be developed for communicable disease outbreaks 2. Restricting liberty in the interest of public health by measures such as quarantine o Governments should have a plan/protocol for restrictive measures in event of pandemic o Government should inform public of rationale for measure, and benefits/ consequences of [non]compliance. o Protect against stigmatization o Plan back up for those who are quarantined 3. priority setting, including allocation of resources, such as vaccines and antiviral meds o Governments should publicize clear rational for priority and initiate public discussion regarding allocation o Should engage stakeholders in allocation decisions o Keep stakeholders updated on information 4. global governance implications (ie travel accessories)” o WHO should be transparent about travel recommendations o Ensure relationships within country are adequate o Developed world invest in surveillance capacity of developed countries G4. Identify and discuss the 4 key ethical issues in pandemic influenza raised by Stand on Guard for Thee 1. Health workers’ duty to provide care during a communicable disease outbreak. i. Their ability to provide care is greater than that of the public. ii. Freely chose this profession and knew of its risks. iii. Social contract where they need to be available in times of emergencies. Codes should state what constitutes ethical conduct, and the rights and responsibilities of health professionals during times of crises. Need to define the extent of professional obligations. Ethical issue of reciprocity shows that society and its institutions need to support these workers and provide for their health and safety; one way is by providing an insurance funds. Government needs to make it transparent what the roles of individuals are in these crises and make it equitable to distribution of risk. Ethical values in this issue: duty to provide care, reciprocity, trust, and solidarity. 2. Restricting liberty in the interest of public health by measures such as quarantine. i. Needed to reduce spread of disease. ii. Reciprocity: since those who are affected lose some personal freedoms, society needs to make sure they get adequate care and don’t suffer unfair economic penalties, like loss of income and jobs. iii. State has right to override right to privacy if will help protect public health, but it must respect the value of privacy as much as possible and it should reveal accurate info. iv. Use the least restrictive methods and without discrimination, must be proportional and necessary. v. Public should be aware of the rationale for restrictive measures and the benefits and consequences of compliance and noncompliance. 3. Priority setting, including the allocation of scarce resources, such as vaccines and antiviral medicines. i. Effective communications strategy should be developed to ensure a transparent priority setting process, to know the necessity of the process, the degrees of freedom within, and roles of individuals, as well as the rationale behind the process. This way the process will be seen as reasonable and fair because stakeholders had a part in the discussion. Appeals should be allowed. 4. Global governance implications, such as travel advisories. i. Any decision by the WHO that can infringe on the sovereignty of a nation needs to be clearly justified and the process transparent. ii. WHO should remain aware of the impact of travel recommendations on affected countries because it could lead to economic losses if it isn’t necessary. It should also make sure that these recommendations are made in a timely manner to slow the spread of disease. iii. Responsibility of countries to have their governments organized enough to be able to retrieve info from throughout the country in order to make timely decisions. iv. Developed countries need to invest in surveillance in developing countries and to invest to improve public health of these countries G4. Identify and discuss the 4 key ethical issues in pandemic influenza raised by Stand on Guard for Thee 1. health workers’ duty to provide care during a communicable disease outbreak a. health workers have obligation to care for the sick because they have greater ability to provide care than that of the public; their profession assumes risk and requires the profession to be available in times of emergency. However, some believe that health workers should have some level of protection to themselves and their families, and it is unreasonable to demand extreme heroism from health care workers as the norm. 2. restricting liberty in the interest of public health by measures such as quarantine a. our highly prized individual liberties are limited especially when balanced against the common good of society. Health professional’s fear for personal safety is in conflict with the duty to treat the sick, and the economic losses must be weighted against the need to contain the spread of a deadly disease. Government should apply the least restrictive methods that are reasonably available to limit individual liberties. 3. priority setting, including the allocation of scarce resources, such as vaccines and antiviral medicines a. decision makers seek to maximize benefits for society while balancing obligations to individuals and individual needs. They will do so by using priority-setting processes or rationing. Some believe that health care workers and people in emergency services should have priority for the use of antivirals while others believe that children should be the last to be immunized as they have higher chance of surviving. Decision makers need to rely on a fair process and open communication to establish the legitimacy of priority setting decisions, that way stakeholders will feel engaged and understand 4. global governance implications, such as travel advisories a. in light of rapid spread of communicable diseases, the need for global solidarity such as travel advisories emerges. Travel advisory can help to slow the spread of the virus, but it also imposes severe penalties on both individuals and entire regions in terms of personal liberty and economic losses. Any decisions made by WHO can infringe upon the sovereignty of a nation and need to be justified and the process transparent. G4. Identify and discuss the 4 key ethical issues in pandemic influenza raised by Stand on Guard for Thee 10. Health workers’ duty to provide care during a communicable disease outbreak a. During the SARS outbreak, some medical workers feared that they would contract the virus and were torn between these fears yet also fulfilling their duty to care for their patients. i. The ability of the physicians and health care workers to provide care is greater than that of the public, thus increasing their obligation to provide care. ii. By freely choosing a profession devoted to care for the ill, they assume risks. iii. The profession has a social contract that calls on members to be available in times of emergency. 11. Restricting liberty in the interest of public health by measures such as a quarantine. a. During the SARS outbreak, a number of people were ordered to remain at home to prevent the spreading of the disease. People subject to restrictive measures will need to have their basic needs met, including some protection for their income and jobs. i. The protocol should be based on proportionality and least restrictive means. ii. The public should be explicitly told the rationale behind quarantine and the benefits or consequences of compliance or non-compliance. iii. The government should protect the community and individuals against stigmatization. iv. The government should provide support services to members affected by the restrictive measures. 12. Priority setting, including the allocation of scarce resources, such as vaccines and antiviral medicines a. During the SARS outbreak patients suffering for other illnesses had their care postponed since the medical workers’ attention was mainly focused on the emergency at hand. 13. Global governance implications, such as travel advisories a. The World Health Organization (WHO) and governments seek to control the spread of diseases through restrictions on travel. G4. Identify and discuss the 4 key ethical issues in pandemic influenza raised by Stand on Guard for Thee o 1. Health workers’ duty to provide care during a communicable disease outbreak afraid that they might be infected with SARS and subsequently infect their families/friends/co-workers. Following through with duty to patient care is the priority, bc workers are more able to provide care than the public choosing this profession assumes risks and comes with social contract to be available in emergencies Primary care and emergency service workers would bear a disproportionate risk compared to more specialized care providers Ethical codes should be clearly articulated in high-risk situations, defining How much risk workers are expected/obligated to take (is it unreasonable to demand extreme heroism from HC workers as the norm?) Duty to care for the sick and for themselves (so they can continue to provide care) o o o Duty not to harm others by transmitting diseases (is it unreasonable to demand that they put their families’ lives at high risk?) Issues of reciprocity and solidarity—duty of society to support and minimize the burdens on workers who take high risks (ie their health/life insurance and protection from financial hardship/job loss due to limitations imposed) Psychological, in addition to physical, risk—need to feel that they have support of superiors All 5 procedural values apply: reasonable (decisions based on reasons like evidence/principles/values that stakeholders agree are relevant to meeting health needs), open & transparent (open to public scrutiny), inclusive (decisions made with stakeholder views in mind/engaging stakeholders in the process), responsive (review/revision of decisions as new information emerges and ways to address disputes), and accountable (ensure decision makers are accountable) 2. Restricting liberty in the interest of public health by measures such as quarantine workers quarantined/isolated/detained to prevent spreading disease need protection for their income and jobs restrictive measures may be one of the most important ways to reduce spread of a communicable disease, but may limit basic personal liberties of mobility, assembly, and privacy. Puts a heavy burden on those affected; if decision makers expect full compliance, the affected need reciprocity (support/compensation for social environment, health care, food supplies, jobs/finances). Also, people need to be fully informed about the issues (rationale for restrictive measures, benefits of compliance, and consequences of non-compliance). government needs to respect privacy as much as possible to reduce stigmatization, but they can override individual’s right to privacy if it helps protect public health. (proportionality- restrictions to individual liberty and measures taken to protect the public from harm should not exceed what is necessary to address the actual level of risk/critical needs of the community). could use other measures like mandatory vaccination, surveillance cameras, monitoring devices, even imprisonment of those who fail to comply. All 5 procedural values apply 3. Priority setting, including the allocation of scarce resources, such as vaccines and antiviral medicines resources such as hospital beds, staff, and equipment could be redirected from important scheduled treatments to the public health emergency because there will be an extraordinarily high number of sick people around the world, straining and overwhelming medical systems. Medical resources will become scarce. (solidarity) Equity: decision makers will need to maximize benefits for society while balancing obligations to individual needs by setting priorities/rationing/allocating resources. Current societal expectations about access to health care will have to change. Government and health care sector should publicize a clear rationale for priority decisions. Public support of decisions should be strengthened by public discussion. Also, decision makers may have to rely on a fair process to establish the legitimacy of priority setting decisions, since there is often disagreement about what principles should be used to make fair allocation decisions . Stakeholders and public should be involved in decision-making. Decisions must be transparent (people need to know in advance what priorities to expect and why). (trust & stewardship) Stakeholders will feel engaged/understand the decision-making process, priorities will be justified / seen as reasonable, and process will seem fair All 5 procedural values apply 4. Global governance implications, such as travel advisories emergence and rapid spread of communicable diseases increases risk to global human security and shows global interdependence, need for global solidarity involving highly coordinated public health responses that involve cooperation of all levels of government. Governments and the WHO (World Health Organization) seek to control the spread of communicable diseases (protect the public from harm) through restrictions on travel, which can impose severe penalties on both individuals and regions (such as economic losses because of reduced travel and tourism) Federal states where powers are shared/allocated among national/state/provincial governments (ie Canada, US, Australia) can face organizational problems in responding to public health crises. Federal ability to obtain data from a province/state would be dependent on voluntary transfer, since the management of communicable disease outbreaks falls under their jurisdiction; this may lead to a delay in providing information to the WHO. Federal countries need to use mechanisms available to ensure that relationships within the country are adequate to ensure compliance with new IHR regulations. (solidarity & trust) Surveillance responsibilities may be beyond the capacities of many developing countries, but attempts to enhance surveillance must not occur at the expense of managing the multitude of ongoing public health threats. Developed countries must increase their investment in the surveillance capacity and in improving the overall public health infrastructure of developing countries to prevent this from happening. The WHO must do everything possible to prevent spread to other countries, but it must also respect national sovereignty. Nations, though, have responsibility as members of the global community to cooperate fully in the international pandemic response. (proportionality) Any decision by the WHO that can infringe on the sovereignty of a nation needs to be clearly justified and process must be transparent. If issued recommendations seem inappropriate to nations it could cause a lack of confidence in the WHO’s leadership and undermine support for the IHR (International Health Regulations). Conversely, failure of the WHO to institute travel advisories in a timely manner, perhaps due to political pressure, could lead to otherwise preventable spread of the pandemic. (proportionality) all 5 procedural values apply G5. How would different ethical principles apply to the above discussions? DOT: direct overseeing of therapy for TB- ethical principle of privacy applies and how it may be limited. Restrictive measures to prevent spread of disease: ethical principle of privacy and autonomy applies, for the affected persons are prevented from going places, taking part in certain activities, etc. Certain information about such persons are also compromised and provided to public in order to prevent harm to society. But the least restrictive methods are sought in order to protect the privacy and freedoms of individuals as much as possible. G5. How would different ethical principles apply to the above discussions? First issue: substantive values applicable to this issue are duty to provide care, reciprocity, trust, and solidarity; procedural values that apply are reasonable, open and transparent, inclusive, responsive, and accountable Second issue: substantive values most applicable here is liberty, protection of public from harm, proportionality, privacy, and reciprocity. Procedural values apply: reasonable, open and transparent, inclusive, responsive, and accountable. Third issue: substantive values are equity, trust, solidarity, and stewardship. Procedural values are reasonable, open and transparent, inclusive, responsive, and accountable. Fourth issue: substantive values: protection of the public from harm, proportionality, trust, and solidarity. Procedural values: reasonable, open and transparent, inclusive, responsive, and accountable. G5. How would different ethical principles apply to the above discussions? b. During the SARS outbreak, some medical workers feared that they would contract the virus and were torn between these fears yet also fulfilling their duty to care for their patients. Ethical Principles: Duty to provide care, reciprocity, trust, and solidarity c. Restricting liberty in the interest of public health by measures such as a quarantine. Ethical Principles: Liberty, protection of public from harm, proportionality, privacy, and reciprocity d. Priority setting, including the allocation of scarce resources, such as vaccines and antiviral medicines. Ethical Principles: Equity, trust, solidarity, and stewardship e. Global governance implications, such as travel advisories. Ethical Principles: Protection of the public from harm, proportionality, trust, and solidarity G5. How would different ethical principles apply to the above discussions? a. Principle of Autonomy: Right to confidentiality about AIDS screening i. Justice to others though about who has contracted it b. Justice: Fair distribution of vaccines to the nation H1. “Who’s My Mommy?” [Clemons VHS 13144] -What actually makes someone a parent? This is a question constantly addressed throughout the film when addressing the five people who had a role in the conception and birth of a young girl by the name of JayCee Buzzanca. JayCee, who is 2 years and 9 months old, is seen as an innocent, active, and normal child by those who look after her. However in truth, she is not very normal at all due to the complications of the modern fertility methods used to create her being, which has caused a custody battle to stir over her life. The process of having JayCee was started by Luanne and her husband John; a couple that was not able to have children. Beginning in 1989, Luann spent 6 years and $200,000 trying to get pregnant and failed until she found a way in which she could use a donated egg and sperm to produce a child. Luanne and John found a surrogate mother, Pamela Snell, who was willing to form a pregnancy for a stable couple that she approved to be loving and caring for the child she was to be bearing. With success, anonymous donors provided an egg and sperm to form an embryo, which was then implanted in Pamela Snell. However, the strong bond of love held between Luanne and her husband John began to unravel when the focus of Luanne’s life, according to John, was having a child. John filed for divorce in 1995, a month before JayCee was born, and refused Luanne’s request of child support because he claimed that he was not the father of JayCee. Luanne then got a lawyer and made an argument against John stating that although John was not the biological father, he was legally the father of JayCee because he signed the contract of consent to allow the embryo to be implanted in the surrogate, Pamela Snell. John stated that he only signed the contract because Luanne had begged him to help her have a child before he divorced her. Amidst this chaos was Pamela Snell’s act of suing for the custody of JayCee. Pamela felt she had been lied to and betrayed by Luanne, who prevented Pamela from knowing about the filing for divorce between her and John by stopping Pamela’s mail until after JayCee’s birth. Pamela felt that carrying JayCee through pregnancy made her the lawful mother. In the fall of 1997, John and Luanne went to court over the custody of JayCee and the judge ruled that neither John nor Luanne was the legal father or mother of JayCee. Luanne decided to appeal this ruling. Throughout the process of deciding who had legal custody of JayCee, Luanne had custody of JayCee. The option to adopt JayCee was out of the question to Luanne who felt that it wouldn’t make sense to adopt your own child and also knew that it would cause her to lose the battle of child support with John. Trouble continued to stir when the woman who provided the egg, Erin Davidson, had claimed that her egg had been used without her consent due to the disorganized fertility clinic. The sperm donor, who wished to remain anonymous, and his wife claimed that his sperm had been used without his consent. However, the sperm donor and his wife retracted the claim when they realized they had accidentally circled the choice to donate the remaining sperm of the sperm donor. The sperm donor and his wife did not sue or ask for custody of JayCee. The case, as it stands now, favors Luanne because in 1999 the state appeals court ruled that the custody of JayCee belonged to Luanne. John was then termed the legal father of JayCee and has been required to pay child support of approximately $400 a month. John attempted to appeal the ruling of this case with another lawyer, but his appeal was rejected and he legally is required to continue paying monthly child support. H2. “The Lynchburg Story” [Clemons VHS 7864] -between 1905-1972, over 70 000 Americans were forced to undergo sexual sterilization because the state judged them “defective and unable to reproduce” -more than 8 000 came from Virginia, the majority of which were sterilized at the Lynchburg Colony -Lynchburg was supposed to be for the feeble minded -Mary Donald was brought because she was poor and considered a burden…sterilized at age 11 -no one told her why she was brought -most of the Lynchburg Colony was deemed “feebleminded”…poor whites who were uneducated and who the state saw as a burden -one girl was operated on who was pregnant…fetus was killed -Judy Crocket (who worked for the ACLU in Richmond) thought this sterilization had violated the victim’s rights…prepared to sue the state of Virginia -Laughlin’s Law—mandatory sterilization for those who were deemed “unfit” -wanted to make sure the white race was kept as pure as possible -basis of law was for eugenics -politicians thought eugenics would increase the “vigor of the nation” as well as save millions of dollars in jails, welfare, etc. -sterilization was originally targeted those who had mental retardation in their family history, but turned into teenagers who were either raped, had children out of wedlock, stole, etc. -some states struck down the eugenics laws in the beginning because they thought it was unconstitutional -1927 Buck v. Bell—states became comfortable with sterilization -Supreme Court said it was ok to sterilize someone because they were feebleminded -Carrie Buck was raped by the nephew of her foster parents and became pregnant, gave birth -she was taken to Lynchburg and considered the second generation of feeblemindedness -Supreme Court case based off of this -main evidence given by Dr. Laughlin even though he had never met her (he was in charge of eugenics records office in New York) -said Carrie was a socially inadequate person and a moral delinquent because she had a child out of wedlock…these defects were attributed to the family and it was thought she would pass this on to her child -other evidence given by Red Cross nurse who examined Carrie’s child at 6 months…nurse said there was “something peculiar” about the child -Eugenics laws in America came right before Hitler’s sterilization laws -Lynchburg colony praised Hitler’s actions in 1933 -in 1936 the Nazis gave Laughlin an honorary doctorate because of his race purification -1934: one doctor said “the Germans are beating us at our own game” because of their eugenics program -At Lynchburg able-bodied individuals worked -boys worked on farms -girls served in dining halls/wards -some were sold to work outside of the colony -In an ironic turn, Dr. Laughlin was eventually diagnosed with epilepsy -Lynchburg colony had “social problems excised with the surgeons knife” H2. “The Lynchburg Story” [Clemons VHS 7864] o Virginia State Epileptic Colony in Lynchburg – the state put men, women, and children away in this institution o They sterilized 8,300 people (men, women, and children) o It was a compulsory sterilization of deaf, blind, alcoholic, feeble-minded, homeless, and criminals o It was meant to keep the white race as pure as possible, so that they don’t “drag down” the white race by reproducing o Eugenics – the proposed improvement of a race or simply the human species by only allowing those to reproduce that have the desired qualities o In 1924 Virginia law passed to allow sterilization to promote eugenics and the not healthy could not reproduce; wanted to promote survival of the fittest o Social reformers advocated eugenics because it promoted the success of the nation o Eugenics had strong political support o Ended in 1972 H2. “The Lynchburg Story” [Clemons VHS 7864] Followed the Eugenics Movement in the state of Virginia o While looking through old record files, the director of the Lynchburg Hospital determined that about 4000 patients were sterilized without consent o The Lynchburg State Colony for the Epileptics and Feebleminded opened in 1910 and became a home for those judged to be the state’s poorest residents, teens from broken homes, and those whom state officials considered socially inadequate or feebleminded Through genetic cleansing, they were sterilized for fear that their defects would contaminate the purity of the white race since their defect was ‘hereditary’ The Virginia Eugenic Sterilization Act called which called for sterilizations to promote an individual's health and protect the welfare of society made this possible Buck v. Bell Virginia wanted to test to see if the Sterilization Actwas constitutional and therefore brought the case to the United States Supreme Court 18 year old Carrie Buck, of Charlottesville, VA, who was born illegitimately to Emma Buck, was sent to the Lynchburg colony after becoming impregnated by her foster brother through rape The Supreme Court reached an agreement that Carrie’s family was feebleminded Both her and her mother carried children out of wedlock and it was feared that Carrie’s daughter, Vivian, would follow the same trend, since feebleminded was deemed to be hereditary The Supreme Court decision ruled that the three generations (Emma, Carrie, and Vivian) would all be sterilized Years later, investigators looked back at Vivian's elementary school report cards and discovered that she was a good child, an average student, and not an 'imbecile' after all Several Virginians were unaware that they had been sterilized until the Lynchburg story hit the press and lawyers from the American Civil Liberties Union (ACLU) filed a class action lawsuit on their behalf H2. “The Lynchburg Story” [Clemons VHS 7864] Beginning in the 1920s Many thousands of people in the US were sterilized against their will/without their consent to prevent undesirable breeding Between 1927 and 1972, over 8000 children and young teenagers were forcibly sterilized because they were “unfit” to reproduce Victims included: various degrees of mental retardation, the poor, ill-educated. “Since these people were, it was claimed, obviously the victims of ‘bad genes’, the law was overtly aimed at maintaining the ‘racial purity of the white race’ by preventing the further ‘breeding’ of those whose offspring would ‘drag down’ this race.” Based upon the notion of eugenics Dr. Harry Laughlin—responsible for most of the sterilizations in the town—thought what he was doing was for the ‘scientific good’ of society Sterilization law declared constitutional in the US in 1927 and became the basis of Hitler’s eugenics program 1. “The Lynchburg Story” [Clemons VHS 7864] H2. “The Lynchburg Story” [Clemons VHS 7864] This movie was an expose on the practice of eugenics in the United States in the 1930s and 1940s. Leading doctors at this time were trying to purify the white race, and were practicing "forced sterilization" on those who were deemed feeble-minded. They targeted those who seemed to be low class, 'feeble-minded' and 'trashy' including women who had children out of wedlock. They locked these chosen people in institutions and continued to sterilize them. This happened across the country, but the greatest number of people with forced sterilization was found in Lynchburg, Virginia. In 1980, Lynchburg was finally exposed and discovered to have had a victim count of 8,300. And it was later discovered that by 1935 some 20,000 forced sterilizations had been carried out in the United States. It was found to be a violation of the Constitution. Many see this as a small-scale version of the Holocaust, with the ultimate goal being to cleanse the American race. This is also the setting for the infamous Carrie Buck, who after giving birth out of wedlock (after being raped) was forced into the institution and sterilized, being deemed "feeble minded" and an "imbecile". H2. “The Lynchburg Story” [Clemons VHS 7864] This was the story of Carrie Buck, who was the first person to be sterilized under the 1924 compulsory sterilization law of Virginia. Carrie had been committed to the Lynchburg Colony (an institution for Epileptics and Feeble-Minded) after she was raped by her foster parents’ nephew. She was committed because she was pregnant, and the family wanted to send her away. However, once at the colony, Dr. Harry Laughlin (superintendent of the Eugenics Record Office) used Carrie, her daughter Vivian, and the knowledge of her mother Emma as evidence that feeblemindedness is hereditary, and the state should therefore enact sterilization laws to help curb this social problem. The case was brought to court in 1927, under Justice Holmes, who declared that “three generations of imbeciles are enough”, and ruled in favor of Dr. Laughlin and the Lynchburg Colony. (Dr. Laughlin had presented shaky evidence and testimony to prove that Carrie’s mother, who had been a prostitute, was feeble-minded and socially-inept, who then birthed Carrie who was also deemed an imbecile, who was pregnant and had Vivian. The only evidence of Vivian’s state of mind was from nurse Caroline Wilhelm, who basically only said there was something “not quite right” about the child. And that was that.) The movie went on to describe that Hitler and the German eugenics and sterilization movement of 1933 was based on Laughlin’s sterilization laws of 1924. Even after WWII, sterilization didn’t drop off, but only changed its language. Nearly fifty years later, Carrie’s sister Doris found out that she too had been covertly sterilized. She was so gravely offended that the state thought she was so incompetent and disgusting that she could not be allowed to have children. It was a deep blow to her personally identity, as it was to the thousands of others who had been sterilized. Later, Mary Bishop, a Roanoke Times reporter, had sought out sterilization victims such as Carrie Buck and Jesse Meadows. Mary found out that patients of the colony were made to work for 25 cents a week. There were horrible punishments for those who misbehaved, including beatings as well as solitary confinement in a “blind room”. Most people who were sterilized could not remember a hearing to let them know of the procedure. Many patients of the colony were kept until they agreed to be sterilized. Once someone had been deemed feeble-minded and worthy of sterilization by the state’s standards, there was really no choice for the victim. The courts and lawyers were all a charade on the state’s side. H2. “The Lynchburg Story” [Clemons VHS 7864] - thousands of children sterilized because they were deemed unfit to reproduce under the term feeble mindedness (many of these people were from Virginia) o 1980 Virginia Sterilization – 8,300 sterilized - Model Sterilization Law (Laflen Law) o Compulsory sterilization or blind, deaf, criminals, feeble minded, homeless, crippled, stds, TB, lepers, poor, mentally retarded etc. o Trying to make sure that we kept white race as pure as possible (stopped short of killing them, but made sure they wouldn’t reproduce); Many people put in insane intuitions had no mental problems but were poor and were put in for the sole purpose of being sterilized - 1924 law legalized Lynchberg Sterilization Program - Eugenic Sterilization o Eugenics – science of good breeding, having healthy productive people marry other healthy productive people and preventing those who were not healthy from having kids o History – survival of fitness; apply laws of science and plants to humans o Eugenics thought state has job of getting rid of unfit people; people believe eugenics would improve vigor of people and lower costs of healthcare etc. o Law was taken up as a practical way to limit reproduction among those that some thought should not reproduce o State fairs held “fittest families” contests to reward strong and smart families - 1927 Buck vs. Bill (when states became comfortable with using sterilization) o first time that supreme court said it was permissible under the constitution to sterilized someone because they were likely to have kids that were socially inadequate o Carrie Buck from Charlottesville was a young girl who was raped, committed of feeble-mindedness and taken to Lynchburg Colony (where her mother already was) o Ruling: Holmes (judge) said people could be sterilized: “three generations of imbeciles is enough” (Carrie was feeble minded mother of feeble minded daughter and daughter feeble minded woman) - After Buck vs. Bell states begin mass sterilization and compete to see who can sterilized the most people; who can save the most people - Hitler comes to power and creates sterilization act (beginning of Holocoust) o Lynchberg welcomed Hitler’s sterilization process (apply pruning knife with vigor) o “German’s are beating us at our own game”; Hitler’s law borrowed directly from US sterilization laws o Program US had, had influence on Germany - Conditions of Lynchberg Colony o People were made to work for slave wages, many were sold outside colony; Some people were beaten to death; Punishments were very, very harsh; They received very little education - ACLU found that there were trials beforehand but these cases were completely ridiculous o Person representing them didn’t know them and questions were misleading. (ask if they were okay with operations in general, if person said yes, judge said okay go ahead with sterilization) o “If it’s for my health I guess I’ll do it.” – Children were young and didn’t understand what was going on. o Children had to be sterilized in order to be released - Deep blow to who they were; state thought they were useless (their lives, relationships and marriages were ruined) - Virginia sterilization lasted 42 years, stopped in 1972 - ACLU Case o Judge was not going to declare something unconstitutional that Supreme Court had said was constitutional (was not going to say that sterilization that took place at Lynchburg was unconstitutional) o Announcement in paper and on radios – people that went though this were told to contact state so they could get counseling. State never would have agreed to pay for reversal processes. H3. “The Deadly Deception” [Clemons VHS7946] An unethical government sponsored scientific research project which for forty years tracked the effects of untreated syphilis on about 400 African American men living in Macon, Alabama in 1932. The documentary showed the testimony of two survivors: Herman Shaw and Charles Pollard. The study was titled "The Tuskegee Study of Untreated Syphilis in the Negro Male." The study began as a research project dedicated to the eradication of syphilis, but turned into a study on the long term effects of syphilis. The subjects believed they were receiving medical treatment for their syphilis but in reality they were only receiving placebos. In 1972 the Center for Disease Control exposed the experiment and officially ended it giving each of the surviving subjects a financial settlement. H3. “The Deadly Deception” [Clemons VHS7946] About unethical behavior in government sponsored scientific research Chronicles the forty year study of untreated syphilis in approximately 400 African-American men from Macon County, Alabama which began in 1932. The utilization of interviews with two survivors of the experiment, Herman Shaw and Charles Pollard, and experts in the fields of research, medicine, and civil rights, along with original film taken during the experiment, demonstrates the startling portrayal of the misuse of human subjects in scientific research. Infuses a play about the now infamous experiment entitled "Miss Evers' Boys" which helps the viewer to understand the lengths to which the United States Public Health Service (USPHS) went to keep the "experiment" in place and the deceit used against the men to retain their participation In the play, Miss Evers is intended to represent Eunice Rivers, who was the nurse who served as a liaison between the men and the public health service and was a key player in encouraging their continued participation. In addition to Nurse Rivers, the USPHS used social institutions that the men trusted, such as churches and schools, to keep them involved in the study. Different perspectives are done in order for a person to judge the experiment on the men of Tuskegee, Alabama which was titled "The Tuskegee Study of Untreated Syphilis in the Negro Male." Provides a chronological account of the government program that was sponsored by the U.S. Department of Public Health and was initially dedicated to the eradication of syphilis Program, begun in the late twenties, changed its focus due to economics and ultimately was transformed from a treatment program to one where the participants turned from being patients to subjects. When the USPHS discovered that 35 percent of the Macon County men were infected with Syphilis, this allegedly overwhelmed the service in terms of holding to the original program goal. Director of the USPHS, Talford Clark, saw an opportunity to study untreated Syphilis in African-American men within a "natural" experimental laboratory, Macon County, which also involved the Tuskegee Institute. Over the years, the program continued to be a scientific experiment using the poor black males of Macon County to determine the long term effects of syphilis. Subjects believed they were receiving medical treatment, yet they were actually getting placebos. In 1972 the Centers for Disease Control (CDC) finally publicly exposed the study and it ended, with the subjects each receiving a minimal financial settlement. While the public was not aware of the alleged research malfeasance committed in Macon County, the scientific community, especially some of those studying venereal disease and social epidemiology, were quite aware of the true nature of the study as the findings had been shared in mainstream medical journals over the years, thus the experiment, its procedures, and findings were well known and institutionalized within the medical community. H3. “The Deadly Deception” [Clemons VHS7946] Tuskegee experiments Alabama county – the health care debacle. Fooling poor black men about being able to cure their “bad blood” syphilis for free, when all they wanted was to study Syphilis The deep south. Old south. 80% of the people who live there – black. 2 or 3 generations from slavery Already oppressed by ravages of poor health Sharecroppers who couldn’t afford health care High instances of infant mortality, syphilis… etc. Mounting tension to health needs Lots of public health concerns: germs know no color boundary; help the black people in order to make sure it doesn’t spread to the white people The terrifying consequences of syphilis – phobia, stigmatized (with illicit sexual behavior, fear that it was everywhere Toxic mercury, arsenic, etc for a year -> prevent worst damage of s. Epitome of what modern medicine was about o Can find the cause o Can treat them effectively o Effective address, in other words How it all started: (Macon county) o At first they wanted to treat o Initial testing: epidemic rate of infection more than they could deal with o Not enough money to treat all the people, weren’t counting on the Great Depression, government doctors pulled out o Wanted to salvage this experiment o Clark : decided to use it as a laboratory, to see if there are any differences in the disease between blacks and whites (the focus is on genetics. Like black people are inherently immoral, couldn’t control lust, syphilis ..) o Depressed economic conditions o Promiscuous sexuality o Prevailing indifference to disease o Clark wanted to use that site for 6 months of s. research, prove that black people weren’t inherently different to gain more funds for that project (?) o Used the school! Used the church! That had gained the trust of Macon county o Patients to experimental subjects. o No questions asked about rights of the men o Greater part of 20th c: Assumed that what scientists and doctors were doing was humane and moral o 1930s sleeping sickness experiments – o No regulations! o Experimental subjects usually poor, socially disadvantaged o Macon patients were told that the spinal taps were TREATMENT. Omg. Omg omg. o Never informed of the real purpose of the research project o Never told of the dangers they faced o Government doctors were fascinated at the data o Contradictory data -> shows that syphilis affected blacks and whites in the same way o Pushed to extend study into long term open research project omg omg omg. o Rivers – nurse o Gather control experiments o Roundup experiment subjects They were given placebos, trusting those doctors. Expected to live in deference to white society; ordered to go for testing by white bosses, etc. o End point of the study => autopsy! o 50$ life insurance for bribery o Subjects – if they tried to get out and seek help, they got chased down o Denied penicillin because the government doctors were so determined to follow through the experiment o The nazi doctors and mass murders = gross examples of human experimentation for science o Led to international body coming up with regulations o BUT those government doctors couldn’t see any parallel between the nazi doctors and what they themselves were doing o Retarded sort of nonsense – so much emphasis on the right to vote, and all that, but no regard for them as experimental subjects o Powerful example of paternalistic example of medicine or research o Bureaucratic inertia – moving the study one step further than another (COG. DISS) o 1972: Syphillis victims not treated for FORTY YEARS o 28 deaths in the Tuskegee study H4. “Discussions in Bioethics” (“A Critical Choice”) [Clemons VHS 4663] Film considers: o Cost of high-risk organ transplants o Allocation of scarce medical resources A child is in need of a liver transplant o Has only 40% chance of surviving with the transplant o 100% chance of dying without the transplant How should society’s scarce medical dollars be spent? o Give the child that 40% chance, or o Use the money for Other patients who have a higher chance of survival Research for cures for illnesses like cancer, which would benefit a lot more people H4. “Discussions in Bioethics” (“A Critical Choice”) [Clemons VHS 4663] This short film is set in Canada where a hospital administrator must decide how to allocate the funds that is given to his hospital. He has to choose between a dying daughter of a single mother who needs a transplant or to spend the much needed resources on one of the wards of the hospital. The child has a 40% chance of surviving with the transplant. Her doctor and advocate contacted a hospital in Michigan and the hospital wants reassurance that if the mother can't pay the expenses the hospital will cover for it. The gist of the story is this: the administration must decide how to allocate the scarce funds that he is provided with. He could choose to give the child a liver transplant (which she may or may not end up surviving) or he could spend the funds on his hospital which could (in the future) save many lives. The story ends with a cliffhanger and it cannot be predicted which one the administrator chose. H4. “Discussions in Bioethics” (“A Critical Choice”) [Clemons VHS 4663] o A child has in-stage liver disease, and it is predicted that the child will have a week to live at the most if she does not have a liver transplant. However, where the child is hospitalized, they do not do the procedure, so the hospital must send the child to America for treatment. As the child’s mother (no father) is constantly in and out of welfare, the mother demands that the hospital guarantees all the money for the child’s expensive treatment. However, the hospital is low on funds and the director of the hospital is very reluctant to send the child to get treatment. His financial advisor also reminds him that if they provide money for the child’s treatment, they must cut money from other budgets, such as from the money to purchase a machine for infant screening. On the other hand, one of the doctors supporting the child’s health asks, “How do you do a cost estimate on a child’s life?” The video does not tell us what decision is made. Relates to Justice and Access to Healthcare Should the hospital sent the one child to America for treatment or purchase the screening machine? o If the hospital sends the child for treatment, the child will most likely survive by getting the liver transplant. (communitarian and libertarian) However, there are also problems with this resolution. After the operation, the child will still need further treatments, and they must make sure that she doesn’t succumb to infections and diseases, but the mother still will not be able to provide this support. o If the hospital denies the child treatment, they can use the funds to purchase the screening machine, which will benefit more people in the long run. (utilitarian and also communitarian) However, for the hospital to have enough money to purchase this technology, they would be leaving the child to die. H5. “A Heart for Jo?” [Clemons VHS 9335] -Jo has Down syndrome and needs a heart and lung transplant. -She is given a lower priority than a “normal” child in England’s hospital because the hospital believes that she won’t have as good a survival rate. -Family and friends believe she’s normal -It is too late to mend the hole in Jo’s heart, and it has affected her lungs. -The transplant team in England say that children with Down syndrome has more chances of infections because of a weaker immune system. -A cardiologist says it shouldn’t matter, only need to be more careful after the transplant. -Herefield does a lot of heart transplants, and the director said that if they have one organ and two patients, they choose the one with fewer problems; she calls it the “greater good” not discrimination. Mother says how can she say that one child is better than another, and if haven’t done any transplants for patients with Down syndrome, how can they say it isn’t as good? -Doctors say that people with Down syndrome won’t be able to comply to the doctor’s order of medications. But a girl in the U.S. knew why she wanted a transplant and knew what medications she needed to take. -Jo ends up not getting a heart/lung transplant and dies at age 25. A requirement for the waiting list was that the patient’s prognosis is no longer than 1 year, which wasn’t the case for Jo. H5. “A Heart for Jo?” [Clemons VHS 9335] a. Jo was in need of a heart transplant but was deemed ineligible in Great Britain because she has downs syndrome i. She has a hole in her heart which diseased her lungs b. They believe it is too late too operate because her lungs would collapse c. But down syndrome creates bodily environment that is friendly to transplants d. Doctors reject her for patients who have less problems i. Transplant organs are scarce ii. Children without down syndrome are much likely to do better e. Went to USA to meet with Sandra and Kay (a down syndrome patient who had a successful heart transplant performed in the US i. Sandra was angered by their lack of autonomy ii. Will to live is not good enough reason for transplant iii. Laws prohibit discrimination based on disability so they ended up winning H5. “A Heart for Jo?” [Clemons VHS 9335] Jo is a mentally handicapped woman living in the UK in need of a heart transplant. After seeking help in the UK and finding heavy resistance from several different transplant teams, she heard of a story of a woman in a similar situation in America. This woman is also mentally handicapped and a heart transplant was approved for her in the states. Jo’s mother sought counsel with this woman’s lawyer, and gained new hope for her battle in the UK; the lawyer insisted that Jo had the same rights as non-handicapped patients. The transplant teams all stressed similar themes: the scarcity of organs for transplantation and the need to give a normal person precedence over Jo. The movie ended with Jo’s mother returning to the UK to see Jo with renewed hope, the conclusion was unresolved. H5. “A Heart for Jo?” [Clemons VHS 9335] This film surrounds a young patient, Jo, with Down’s Syndrome, who is in need of a heart and lung transplant. She has “learning difficulties,” but other than the fact that she has Down’s, Jo is a perfectly normal child. The basis of the entire film surrounds the idea that in the eyes of Jo’s family and friends, she is just like any other normal child. The question in her family’s eyes remains: why do other so called “normal” kids have more opportunity to have this opportunity, when they see Jo as normal. Jo’s mother visits several doctors: mainly being one who says the transplant is not a good idea, and another that gives some hope to Jo’s family. The doctor who opposed the transplantations for Jo had two main arguments in addition to the fact that Jo has “other” problems. 1. It is possible that Jo would not comply with “rules”/cope clinically with her after care 2. Those with Down’s syndrome have a lowered immune system to begin with The mother felt that Jo was “devalued” by this doctor; in the eyes of the mother, Jo is just as normal and deserving as any child without a learning disability. The physician that provided some hope for Jo, especially in the fact that after a transplant the immune system is suppressed and Jo will already have a lower immune system. He saw this as a huge benefit. In the end Jo’s mother met with Sandra, an American woman with Down’s Sydrome who got the heart and lung transplant after being rejected twice. They had to fight, with legal action, to get the procedue done, and the idea of being refused was referred to as “a death sentence.” Other issues to consider: consent of those with Down’s Sydrome, is refusing someone based on “other problems”or mental retardation devaluing these human lives?