Supplementary Background: Sarcoidosis is a multi
advertisement

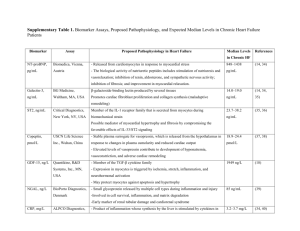
Supplementary Background: Sarcoidosis is a multi-system disorder of unknown etiology which is characterized by the formation of non-caseating granulomas in multiple organs (1). Cardiac sarcoidosis, which affects at least one quarter of patients (2), portends a worse prognosis and accounts for the majority of deaths from this disease. Treatment with corticosteroids may slow the progression of heart failure (3-5) while implantable cardiac defibrillators (ICD) may improve survival (6). Nevertheless, such therapies have considerable side effects and are costly and thus require accurate diagnosis of patients who have cardiac involvement and have an increased risk of adverse events. Supplementary Methods: Study Population For patients that had multiple exams, only the initial PET exam was included in the study. Patients with coronary artery disease (CAD) -- defined as stenosis >50% based on invasive angiography, percutaneous coronary intervention (PCI), or coronary artery bypass grafting (CABG) surgery, regardless of whether these procedures occurred before or after the PET study – were excluded. PET Perfusion / Metabolism Protocol Myocardial perfusion and metabolism images were independently interpreted by two experienced cardiologists blinded to all patient information as well as extra-cardiac findings. Patients were studied using a whole body PET-CT scanner Discovery RX LightSpeed 64, GE Healthcare, Milwaukee, WI). Non-gated CT imaging was used for the purpose of attenuation correction. Resting myocardial perfusion was assessed following the intravenous administration of ~50 mCi of 82Rubidium. Following perfusion imaging, 10-12 mCi of 18F-fluorodeoxyglucose (FDG) was injected intravenously. After a 90-minute uptake period, dedicated cardiac PET/CT images were performed in the same manner. Finally, limited whole body FDG images were also obtained from the base of the skull to the mid thigh. Non-contrast helical CT imaging was performed over the same range without breath-hold for attenuation correction of PET images and for localization of FDG uptake. Left ventricular ejection fraction (EF) was calculated from the rest gated myocardial perfusion images using commercially available software (Corridor 4DM, INVIA, Ann Arbor, MI). The estimated average radiation dose per study was ~15 mSv. All patients were instructed to follow a high fat, high protein, low carbohydrate diet followed by a fast of at least 3 hours in order to shift normal myocardial metabolism to primary fatty acid utilization and, thus, suppress the uptake of FDG by normal myocardium. Patients were specifically instructed to avoid any sugar or sugar containing foods. Image Analysis Cardiac images. Myocardial perfusion and metabolism images were independently interpreted by two experienced cardiologists blinded to all patient information as well as extra-cardiac findings. Consensus was achieved by a joint interpretation with a third expert reader who was also blinded to all clinical data. In order to quantify the severity of FDG uptake by the myocardium, the maximum standardized uptake value (SUVmax) for the myocardium was recorded for each patient with focal FDG uptake, adjusted for decay corrected injected activity and patient weight. In addition, the right ventricular free wall SUVmax was also recorded for each patient that was found to have focal FDG uptake by the right ventricular myocardium. Whole body images. Whole body FDG PET/CT images were reviewed by an experienced nuclear medicine physician who was blinded to the interpretation of the cardiac PET results and to the clinical history. Patients were classified as having active extra-cardiac disease if FDG- avid disease was present in the mediastinum and/or lungs or in other organs with suspected sarcoid involvement. Endomyocardial Biopsy Among the subset of patients who underwent endomyocardial biopsy as part of their clinical care, the findings on cardiac PET exam were compared to the biopsy results. Biopsy of the right ventricular septum was performed through the right internal jugular or femoral vein, with 4-5 specimens typically taken per patient. The specimens were fixed in 10% neutral buffered formalin, processed and embedded in paraffin. Step sections were taken through the paraffin block to produce three hematoxylin and eosin stained slides with 3-4 levels on each slide. Biopsies containing non-necrotizing granulomas were considered positive for sarcoidosis once other potential etiologies for granulomas were ruled out. Polarized light examination was undertaken to rule out foreign material as a source of the granulomas, and methenamine silver (MSS) and acid fast (AFB) stains were performed to rule out infection. Ascertainment of Outcomes Cause of death was obtained by reviewing death certificates and, when applicable, electronic medical records. Cardiac death included any death which was attributed to heart failure and/or cardiac arrhythmias, as there were no myocardial infarctions identified for any patients. In addition, for each patient that experienced a VT event, all available clinical data was reviewed by two cardiologists in order to assign the most probable clinical diagnosis / cause for event (see supplement Table below). Statistical analysis Patient demographics and baseline characteristics were summarized as means ± standard deviation for continuous variables and frequencies for dichotomous and ordinal variables. Statistical significance was assessed using t-tests or Wilcoxon tests for normal and non-normal continuous data, respectively, and with Fischer exact or chi-square tests for categorical variables. Two sided p values <0.05 were considered significant. All statistical analyses were performed using STATA software, version 11.0 (Stata Corp., College Station, Texas). Cox proportional hazard regressions were used to assess the impact of PET exam results on the primary outcome. For each model used, the validity of the proportional hazards assumption was tested. Multivariable models included all variables which had a significant univariate association with the primary outcome. In order to avoid model over-fitting and due to co-linearity, the presence of focal RV FDG uptake and abnormal PET perfusion or metabolism imaging were introduced into separate models. All multivariable models were also repeated after excluding patients with known coronary artery disease. Supplementary Results: Study Population Notably, only 9 (8%) patients had known cardiac sarcoidosis prior to the PET examination, and 38 (34%) patients met JMHW criteria for cardiac sarcoidosis. ICDs had been implanted in 48 (41%) of patients prior to the PET exam. Repeat Testing to Assess Response to Therapy Among the 116 patients in our study, repeat PET/CT testing was performed in 25 individuals in order to assess the response to immunosuppressive therapies. Of them, 16 (64%) demonstrated reduction in FDG uptake. Association of SUV with Adverse Events There was no significant difference in measured SUVmax between patients that experienced the combined endpoint of death or ventricular tachycardia versus those that did not. (SUVmax 8.4 vs. 7.9, p = 0.72) Furthermore, there was no significant difference in measured SUVmax between patients that had focal RV involvement versus those that did not. (SUVmax 8.5 vs. 8.2, p = 0.89) Association of PET Findings with Adverse Events: Sub Group Analysis When comparing the 54 patients with any abnormal FDG findings (regardless of perfusion results) to those with normal FDG scans, there was a highly significant association of abnormal myocardial inflammation with events (log rank p = 0.004). Similarly, among the 51 patients with abnormal perfusion defects (regardless of FDG findings), there was a significant, although weaker, association of abnormal myocardial perfusion with future events (log rank p = 0.037). Evaluation of coronary artery disease in patients with perfusion defect and increased metabolism In order to verify the absence of CAD among the 34 patients that had both perfusion and metabolism abnormalities the following tests were performed: 21 patients had an invasive angiography which did not identify any obstructive disease, and 7 patients who did not undergo invasive angiography had a cardiac magnetic resonance imaging (CMR) which did not identify any myocardial infarcts. Of the remaining 6 patients, 4 had positive endomyocardial biopsy for CS, 1 had no ischemia on stress perfusion imaging and 1 patient – who was 43 years old and had no risk factors for CAD -- had high enough index of suspicion for CS (known pulmonary sarcoidosis and positive cardiac PET) that coronary angiography was not felt to be clinically needed. Among the 34 patients that had both perfusion and metabolism abnormalities, 13 had CMR and all had abnormal late gadolinium enhancement. Only 1 of the 13 CMR studies showed late enhancement which involved the subendocardium (a pattern which could represent a myocardial infarction), however this patient had no disease on coronary angiography, and has improved following treatment with steroids for presumed cardiac sarcoidosis (no biopsy was performed). There were 3 patients that had no LGE by CMR who had focal FDG uptake with normal rest myocardium perfusion. In one such patient, the FDG uptake involved the lateral wall and was thought to be a non-specific finding, while the two other patients had focal FDG uptake that was thought to possibly represent cardiac sarcoidosis, although neither one of these patients had any cardiac events upon follow-up. REFRENCES 1. Iannuzzi MC, Fontana JR. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA 2011;305:391-9. 2. Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation 1978;58:1204-11. 3. Cooper LT, Baughman KL, Feldman AM et al. The role of endomyocardial biopsy in the management of cardiovascular disease. European Heart Journal 2007;28:3076-3093. 4. Yazaki Y, Isobe M, Hiroe M et al. Prognostic determinants of long-term survival in Japanese patients with cardiac sarcoidosis treated with prednisone. Am J Cardiol 2001;88:100610. 5. Grutters JC, van den Bosch JM. Corticosteroid treatment in sarcoidosis. Eur Respir J 2006;28:627-36. 6. Paz HL, McCormick DJ, Kutalek SP, Patchefsky A. The automated implantable cardiac defibrillator. Prophylaxis in cardiac sarcoidosis. Chest 1994;106:1603-7. Supplementary Table and Figure Table: Clinical diagnosis among patients that experienced death or ventricular tachycardia. Clinical Diagnosis / Etiology for cardiac event Normal PET Death as primary event with no prior VT (n = 4) Cardiac arrest 20 to severe pulmonary hypertension; severe RV dysfunction. History of ocular sarcoid. NICM (EF 15%), aortic stenosis; despite extra cardiac sarcoidosis, etiology of NICM thought NOT to be related to CS. Sepsis in patient with metastatic colon cancer and cardiac sarcoidosis PEA arrest following prostate biopsy in patient with cardiac sarcoidosis 2 1 Ventricular Tachycardia (n = 27) LV dysfunction presumed 20 to CS Nonischemic cardiomyopathy, unknown etiology Nonischemic lamin-associated cardiomyopathy VT of unknown etiology VT of unknown etiology, possible CS Idiopathic VT 4 1 3 Death with previous VT as primary event (n = 4) LV dysfunction s/p LVAD presumed secondary to CS; Clostridium difficile infection at time of death NICM, heart block, sepsis and multi-organ failure NICM, Refractory VT, EMBx negative for CS, Possible CS although cause of death uncertain NICM, Presumed cardiac sarcoidosis, EMBx negative for CS although positive extra-cardiac biopsy and CMR and PET both c/w CS 1 1 Abnormal Perfusion or Metabolism 2 Abnormal Perfusion and Metabolism 0 1 1 1 9 3 2 1 1 1 1 14 10 1 1 2 2 1 1 1 1 CS = cardiac sarcoidosis; VT = ventricular tachycardia; NICM = non-ischemic c cardiomyopathy; EMBx = endomyocardial biopsy; PEA = pulseless electrical activity. Supplementary Figure 1. Survival free of cardiac death or VT stratified by cardiac PET exam results. Secondary survival analysis was performed to assess the endpoint of cardiac death or sustained VT. During this analysis, 2 patients that had non-cardiac death were removed. Supplementary Figure 2 Guidelines for Diagnosis of Cardiac Sarcoidosis Guidelines for diagnosis of cardiac sarcoidosis from the Japanese Ministry of Health and Welfare.