File
advertisement

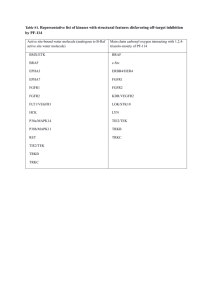
Samia B. April 9, 2013 Ponatinib in Refractory Philadelphia Chromosome–Positive Leukemias Leukemia is a cancer that originates in the bone marrow, ultimately causing proliferation of precursors of white blood cells. Because bone marrow stem cells divides into two distinct precursors, myeloid and lymphoid cells, before differentiating into blood cells, leukemia is classified into types based on the type of cell affected along with chronic (slow onset) or acute (rapid onset) of disease. Certain leukemias are attributed to cytogenetic abnormalities, namely the Philadelphia chromosome, where a mutation occurs on the bcr gene of chromosome 22 as a result of translocation of the abl gene from chromosome 9, resulting in a bcr-abl. This mutation is commonly associated with chronic myeloid leukemia and some cases of acute lymphoid leukemia and causes resistance to therapies inhibiting tyrosine kinase, the type of protein the bcrabl fusion presents as.1 The only three therapies approved for targeting the BCR-ABL protein are imatinib, nilotinib and dasatinib. Because of increased resistence and the limited number of therapies available, 20-30% of patients fail therapy on imatinib; of those 37-65% can fail on nilotinib and dasatinib . Only until recently, there was no approved treatment if the latter two therapies failed until a novel oral multi-kinase inhibitor by the generic name Ponatinib demonstrated possible efficacy following the failure of these two treatment options.2 Ponatinib is a oral multikinase inhibitor that is active against both normal and the mutant abl gene as well as several tyrosine kinases such as VEGFR, PDGFR, FGFR, EPH, Src family kinases, KIT, RET, FLT-3 and TIE-2.3 Ponatinib is also unique in that it allows the drug to remain active in the presence of a T351 mutation, which accounts for 20% of drug resistence to tyrosine kinase inhibitors due to blocked access of the drug to the ATP-binding site. This is due to a triple-bond linkage that bypasses steric hindrance that otherwise makes tyrosine-kinase inhibitors unable to access the ATP-binding site. Like the other tyrosine kinase inhibitors, Ponatinib is administered orally, generally at a dose of 45 mg/day unless the patient is taking a CYP3A4, for which the dose must be reduced to 30 mg/day due to possible interactions. Adverse effects include rash, pain, myelosuppression, and cardiac and hepatic toxicity. CBC (with differential), LFTs, serum lipase and serum uric acid should be monitored when using this drug. There is no drastic change in the dosing schedule or side effects profile of Ponatinib compared to Imatinib, Nilotinib, and Dasatinib. 2,4 The consideration of Ponatinib as a novel tyrosine kinase first became known around 2009, when point mutations in imatinib and subsequently, second-line therapies like nilotinib and dasatinb, were observed. Special emphasis was placed on the T315I mutation because it demonstrated resistance to all three regimens and created a basis for new drug development. By using crystallographic analaysis, it was revealed what chemical bonds hinder access to T315I mutations in already existing tyrosine kinase inhibitors, thus proposing a unique architecture for a novel tyrosine kinase inhibitor. This pre-clinical study assessed response in cells from patients who expressed the bcr-abl mutation as well as a preliminary measure of efficacy by testing the drug on rats. The results showed that potential Ponatinib (designated as AP24534 at the time) has potential in controlling resistance in CML, therefore providing a reference for clinical trials needed to evaluate use and effectiveness.4 From June 2008 to Octomber 2010, patients were enrolled for a phase I trial of Ponatinib that discussed the potential role of Ponatinib in refractory Philedelphia chromosome positive leukemias, based on pre-clinical experiments that demonstrated Ponatinib being effective against native and mutant forms of bcr-abl. Inclusion criteria defined patients 18 years old or above having hematologic cancer (except lymphoma) that either relapsed or was resistant to currently available therapies as well as an ECOG score of 2 demonstrating that with their diagnosis they were fully active as opposed to disabled. Patients had to had adequate renal, hepatic and cardiac function. The primary objective of the trial was to see the maximum tolerated dose or the daily recommended dose. Secondary endpoints included safety, pharmacokinetic, pharmacodynamic and pharmacogenomic markers and anti-leukemia activity In observing the effect of increasing the dose, patients were assigned to cohorts of at least three people and were each given escalating doses until drug toxicity occurred. Treatment was continued until either the disease progressed, an adverse effect occurred or if the patient withdrew. Toxicity was assessed based on adverse effects noted in the first cycle of therapy that lasted for greater than three days, despite supportive care, the development of febrile neutropenia unrelated to diagnosis or the effect of the lack of proper adherence to the medication. Pharmacokinetics and pharmacodynamics were evaluated via blood samples. Antileukemia activity was assessed by observing complete blood counts and white-cell differential counts three times a week for the first three weeks, then once a week afterward. Bone marrow aspirations were performed 28 days before the study and at least every 3 months following initiation and then continuation of therapy for morphologic and cytogenic assessments.2 A total of 81 patients were enrolled in the study. Of these patients, 65 had Ph-positive leukemia: 60 with CML and 5 with Ph-positive ALL. In assessing the primary endpoint, the maximum tolerated dose/recommended dose, 7 dose levels at 2mg, 4mg, 8mg, 15mg, 30mg, 45mg and 60mg were investigated. At 45 mg, a grade 3, dose-limiting rash was reported; at 60 mg, other dose-limiting toxicities were reported. After taking into consideration reports of pancreatitis and myelosuppression while observing pharmacokinetic and pharmacodynamic profile in regards to appropriate peak and trough concentrations and adequate drug response, it was established that 45 mg should be the maximum dose set for Ponatinib.2 In staying consistent with pre-clinical findings, anti-leukemia activity was assessed as one of the secondary endpoints of the study. Anti-leukemia activity was based on whether a hematological or a cytogenetic response was shown. A hematological response is one that demonstrates normalization of white blood cell count while a cytogenetic response is one that demonstrates response of treatment in the marrow rather than the blood5. Out of the 65 patients who were Ph positive, 43 of those had chronic-phase CML. Of these 43, 98% complete hematological response, 72% had major cytogenetic response, and 63% had a complete cytogenetic response. Of 12 patients who had chronic-phase CML with the T315I mutation, 100% had a complete hematological response and 92% had a major cytogenetic response. For the 13 patients who had CML without the T315I or any other significant mutation, 100% had major hematological response had complete hematological response and 62% had major cytogenetic response. Of the 22 patients who either had blast-phase CML or Ph-positive ALL, 36% had a major hematological response and 32% had a major cytogenetic response. These results showed that Ponatinib demonstrates significant clinical activity in patients who had Phpositive leukemias who were known to be resistant to most, if not all, of the available treatments used prior to enrolling in the study.2 In September of 2010, Ariad pharmaceuticals conducted a phase II trial, PONATINIB for Chronic Myeloid Leukemia (CML) Evaluation and Ph+ Acute Lymphoblastic Leukemia (ALL) (known as PACE), to further assess the clinical efficacy based on the phase I trial. Inclusion criteria for the study was a diagnosis of CML in either chronic phase, acute phase, or blast phase of either myeloid or lymphoid phenotype or either Ph+ positive ALL, development of resistence to dasatinib or nilotinib or the T315I mutation following treatment with imatinib, be at least 18 years of age, have an ECOG performance status of 2 or less, have a normal pancreatic status and QT interval, had adequate renal function and a minimum life expectancy of three months. Exclusion criteria was defined as having prior tyrosine kinase inhibitor therapy 7 days prior to starting treatment with Ponatinib, undergoing a stem cell transplant 60 days prior to treatment with Ponatinib, having evidence of Graft vs. Host disease, concurrent treatment with immunosuppressive agents, having active CNS disease, having significant or active cardiovascular disease, having a significant bleeding disorder unrelated to the leukemia, having a history of pancreatitis or alcohol abuse, having uncontrolled and elevated triglycerides, having underwent major surgery 14 days prior to starting Ponatinib or having an ongoing or active infection. Approximately 440 participants were enrolled in the study. Primary outcomes were defined as having a major hematologic response as well as a cytogenetic response. Secondary outcomes included clinical response, molecular response, clinical outcomes and safety. Of the approximately 440 patients, 267 had chronic-phase CML. 56% of these patients had a major cytogenic response whereas 46% achieved a complete cytogenetic response. Of the 64 of these patients who had the T513I mutation, 70% achieved a major cytogenic response while 66% achieved a complete cytogenetic response. Those patients who did not have the mutation demonstrated a 51% major cytogenetic response. The most common side-effects demonstrated in the phase II trial were rash, abdominal pain, headache, dry skin and constipation in mild to moderate severity. The data of the study was released in December 2012 at the Annual Meeting of the American Society of Hematology, where it was revealed that the 12-month trial reinforced that Ponatinib demonstrates great anti-leukemic activity in patients who are otherwise resistant to available therapies.6 Approximately a week following the the Annual Meeting of the American Society of Hematology, the FDA officially approved Ponatinib under the trade name Iclusig for the treatment of chronic myeloid leukemia (CML) and Philidelphia chromosome positive acute lymphoid leukemia (ALL). 7 Inclusig was approved three months earlier than when it was scheduled to complete the drug application review because it proved to be safe and effective, with no alternative therapy available for substitution. The safety and efficacy of Inclusig were based heavily on data from the PACE trial. As of current, Ariad has initiated a Phase III trial, known as the Evaluation of Ponatinib versus Imatinib in Chronic Myeloid Leukemia (EPIC trial), which is designed to provide clinical data demonstrating the basis to use Ponatinib in treatment naïve CML patients8. The trial will be a randomized, two-arm multi-center trial. Inclusion criteria defines patients to be at least 18-years of age and diagnosed with CML 6 months prior to enrollment. The expectation is for 500 patients to be randomized at a 1:1 ratio of ponatinib and imatinib to achieve the primary outcome of a major molecular response. Secondary endpoints may include a major molecular response at 5 years, a molecular response at 3 months to see the reduction of bcr-abl trancripts to 10%, complete cytogenetic response rate at the end of 12 months, progression-free survival and overall survival based on follow-up up till 8 years from initiation. Patient enrollment for EPIC is open until the end of 2013. Based on these trials, especially PACE, that gathered a large enough population size for the event, Ponatinib has demonstrated substantial effectiveness in treatment of resistant and mutated CML cancers as well as the rare Philedelphia Chromosome Positive ALL. Its early approval provides a means of treatment for patients who had little to no options left in terms of other tyrosine-kinase inhibitors. With the EPIC trial underway, Ponatinib may be readily available to treatment naïve patients on CML as a better alternative to Imatinib due to greater potential for resistence and mutations in with the use of the drug. Nevertheless, because it is a new drug, much of the data understanding its current clinical use has yet to be established—the current available information is sponsored by Ariad pharmaceuticals itself, so the true benefit of the drug may not be realized until it has been in the market for many more years. References 1. "What You Need to Know About Leukemia."Http://www.cancer.gov/cancertopics/wyntk/leukemia. National Cancer Institute, n.d. Web. 2. Cortes, J. E., Kantarjian, H., Shah, N. P., Bixby, D., Mauro, M. J., Flinn, I., & Talpaz, M. (2012). Ponatinib in Refractory Philadelphia Chromosome–Positive Leukemias. New England Journal of Medicine, 367(22), 2075-2088. *Primary Source 3. Gold Standard, Inc. Ponatinib. Clinical Pharmacology [database online]. Available at: http://www.clinicalpharmacology.com. Accessed: April, 9, 2013. 4. O'Hare, T., Shakespeare, W. C., Zhu, X., Eide, C. A., Rivera, V. M., Wang, F., & Clackson, T. (2009). AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer cell, 16(5), 401-412. 5. "Respose." Http://www.nationalcmlsociety.org/living-cml/response. The National CML Society, n.d. Web. 6. "ARIAD Announces 12-Month Data from Pivotal PACE Trial of Ponatinib in Heavily Pretreated Chronic-Phase CML Patients." Ariad, n.d. Web. <http://phx.corporateir.net/phoenix.zhtml?c=118422&p=irol-newsArticle&ID=1765565&highlight=>. 7. "News & Events." FDA Approves Iclusig to Treat Two Rare Types of Leukemia. N.p., n.d. Web. . <http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm332252.htm>. 8. "EPIC Clinical Trial." - ARIAD. N.p., n.d. Web. <http://www.ariad.com/wt/tertiarypage/epic>.