PT Evaluation
advertisement

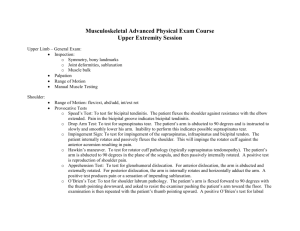
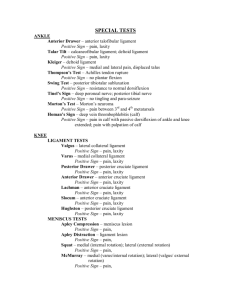
A Practical Guide to PT EXAM 1. Review of the Chart: As soon as you know you have a new eval the first thing you should do if possible is to look at the Pt.’s chart. Questions to ask yourself: Is the Pt. male or female, how old are they? Is the Pt. a referral, what is the doctor’s diagnosis? Is the Pt. post-surgical; if so are you familiar with the procedure? How long ago was the surgery? Do you know the surgeon, and their protocol for handling their post-op Pt.’s? 2. Pt.’s arrival: Greet the Pt. by name in the waiting room. Have your tools ready (goniometer, reflex hammer etc.etc.) Observation begins now (watch them walk towards you, begin using gait descriptors, walking posture, are they limping? using an AD? Holding their arm close to their side? Note all these things). Introduce yourself, make sure to explain your role as a PT student/ Intern (helpful hint: people for some reason like intern better than student). Begin building your relationship (ask how much trouble they had getting in, how they feel at the moment), begin gauging their personality. 3. Pt interview: Where will you take the patient? Are there private exam rooms available? if not create as much privacy as possible, pull curtains, try to minimize noise and distractions. 1. How is the Patient dressed, if it is winter they may have on a lot of layers, are gowns available, did they bring a change of clothes? 2. Try not to sit the patient on a plinth if possible, seat them in a comfortable chair with armrests, so they have support and can relax, face them to create eye contact and make sure they know they have your attention. 3. Although it may seem obvious to delve into the patients current complaint first, it may actually lead you off the trail, focus on PMH ( Hypertension, Cardiac Problems, Diabetes, Hypercholesteremia) PSH ( Bypass Surgery, Heart Transplants, Fractures) Medications ( if they have pain meds are they using them, did they take them before they came?) Occupation (Employed, On Disability, Retired), Social History (Apartment/ House w/ elevator/stairs, w/ Family/Alone, AD use at home and in the community). 4. Current Complaint: Now you cleared out all those things you can focus on the Current Complaint: Why did they see the doctor? If the problem is chronic or of long duration what exacerbated or triggered them to seek help? Was the onset insidious or traumatic, any visible symptoms (bruising, swelling), are they in pain currently (VAS 0-10); what is their average pain, when is their pain wore or better? What activities are they having trouble with? Try to make these quantitative if possible to help in goal setting. For the UE (are they having trouble lifting ( how many pounds), reaching overhead, writing, opening doors) For the LE (walking ( how far, how many blocks, or feet, standing( for how many minutes before they get pain or have to sit down), stairs ( how many do they climb, when do they get pain up or down). Interview Rule #1: You control the interview, if at any point you get the feeling you lost control get it back, steer the patient without being rude. 1) Physical Exam ** Before beginning the physical exam make sure to explain to the patient that certain test positions, motions, or special testing may provoke their pain, this may seem like common sense but it indicates to them that you care for their wellbeing and stops any nasty surprises. When evaluating a pt. try not to ask does this cause you pain? Instead ask is this your pain? Is this the pain that caused you to go see the doctor? If yes, where do you feel it, how does it feel? If not, what does this pain feel like, how is it different from your usual pain? Is it a stretch, discomfort, sharp, dull, aching, burning, give them time to provide their own descriptors before volunteering your own. Heart rate and BP check: if you have worries, now is the time to get this out of the way. Things that can be tested in the chair: Sensation: EO/EC, evaluate Light touch/ Comparison testing. For LE, if possible ask the Pt. to take off their shoes (get a towel for them to rest them on) evaluate their feet (look for edema, wounds, necrosis especially in Diabetic Patients). 2) Postural Assessment: Ask the Pt. to stand up, make sure to evaluate anterior, lateral and posterior views. Things to note: Forward head posture Rounded Shoulders Scapula winging Increased Thoracic Kyphosis Decreased or Increased Lumbar Lordosis Anterior /Posterior Pelvic Test: Get on and locate the iliac crests, the ASIS and PSIS (make sure they are level) Internal and External Rotation at the hips Genu Valgum/Varum or Recurvatum at the Knees Over Pronation (Flat Foot) (Too many toes laterally), High Arches, Calcaneal Eversion/Inversion at the ankles. Shoulder Exam: Minimize position changes for patient comfort. Tests in Standing: Painful Arc Test: 60-120 degrees (Shoulder impingement) With the Pt. with UE complaints of numbness and tingling/parasthesias, you must rule out Cervical Radiculopathy, TOS in your exam. Sit the Pt. on the Plinth, if the table is adjustable do so for your own comfort depending on the Pt.’s height, if not use other things like steps or stools to put yourself in comfortable positions. Tests to perform in sitting: Cervical ROM: flex, ex, SB, ROT: Do any positions produce pain or reproduce symptoms. Special testing: Spurling’s Test for Cervical Compression, Distraction: any increase or decrease in symptoms? Palpation ( Note tender points, tight musculature (Upper traps), muscle spasm, trigger points) Gross UE ROM. Goniometric Measurements: Flexion, Abd, IR/ER. Take both AROM/PROM, is the problem strength or capsular restriction, is there pain, note end-feels. MMT: Do a gross check of the UE; don’t forget IR/ER strength at the shoulder. Special testing (In Sitting): TOS: Positive Testing is an absence of pulse/ or reproductions of symptoms. 1) 2) 3) 4) 5) 6) Adson’s Vascular Test Allen’s Test Wright’s Test Halstead Maneuver Costoclavicular test Roo’s Test Shoulder Special Tests 1) Obrien’s Test: Inside Pain: Slap Lesion, Outside Pain: AC Pathology. 2) Crank test: Labral pathology 3) Neer’s Test: Posterior Overpressure( Bursa), Medial Over Pressure (Supraspinatus Impingement) 4) Hawkins-Kennedy: Subacromial Impingement 5) Jobe’s Full can/Empty can test: RTC pathology 6) Drop Arm Test: Full Thickness Tear 7) Gerber’s Lift off Test: RTC pathology( subscapularis) 8) Bell Press Test: RTC pathology ( subscapularis) 9) Speed’s Test: Pain w/ biceps tendonitis, Labral Instability w/ SLAP lesion. Special tests in Supine: 1) Anterior/ Posterior Drawer Tests: Capsular insufficiency 2) Anterior Apprehension and Relocation testing: Capsular Insufficiency 3) Compression/ Rotation test: Labral Pathology (Slap Lesion) 4) ULTT: Radial, Median ½, Ulnar Nerve. In Prone: 1) Evaluate Thoracic Spine: Spring testing (If thoracic spine has decreased mobility, this can lead to problems in reaching overhead). 2) MMT: Scapula Stabilizers: Assess Rhomboids, Mid/Lower Traps, and Latissmus for muscular imbalances. *Special Tests: Pick which special tests are relevant to the patient, in post surgical patients, resistive testing may be contraindicated. Low Back/Hip Pain: Minimize position changes for comfort. With the Pt. with LE complaints of numbness and tingling/parasthesias, you must rule out Lumbar Spine in your exam. Tests in Standing: Lumbar flex, ex, SB, Rot (ask the Pt. if their pain is reproduced/relieved which each motion and if the experience any LE sensations, note any deficiencies or limitations and abnormal movement patterns) Repeated Motions: flex, ext, (any increase/decrease in symptoms) Get your hands on the Pt: Standing Flexion Test: (Are the PSIS moving equally?) Gillet’s Test: illiosacral Joint dysfunction. In Sitting: Gross LE ROM LE MMT Reflexes In Supine: For Hip: Hip Flexion, ABD, IR, ER ROM SI Gapping Test: Anterior SI Ligament Stress Test Compression test: Posterior SI Ligament Stress Test (Also Sidelying) Faber’s Test: hip pathology, pubis symphysis, SI joint dysfunction, illopsoas muscle spasm. Gaenslen’s Test: hip pathology, SI joint dysfunction, pubic symphysis instability, L4 nerve root lesion. Posterior Thigh Thrust: SI Pathology Piriformis Test: Piriformis Syndrome Hamstring Length Testing: 90/90 test (Objective) Thomas Test: Rectus Femoris/Hip Flexor Tightness In Sidelying: Ober’s Test for ITB tightness (It has been theorized that weak gluteus medius and tight ITBs can contribute to Low Back Pain. Abductor strength In Prone: Palpation: Look for Tender Point, trigger points and Muscle Spasm. Lumbar Spring Testing (Identify Hyper-mobile and Hypo-mobile points, Scoliotic postures). Ask the Pt. to go into extension: Does it increase or decrease their pain? Assess Sacral Bases/ILA’s are they level, any pain or tenderness? Special Testing 1) Yoeman’s Test: SI Pathology, Lumbar Spine, Hip Joint, Illopsoas. 2) Ely’s Test: Femoral Nerve Tension, Rectus Femoris tightness Knee Pain: Minimize position changes for Pt. comfort In sitting: Gross LE ROM LE MMT Reflexes Observe patella tracking as the Pt. moves from knee flexion to extension. In Supine: With the Pt’s knee in extension to slack the Quadriceps tendon, assess Patella mobility, Look at medial and lateral movement, (Lateral Apprehension Test) Look at Patella tilts, assess for pain, Clarke’s Test for possible chrondromalacia patella. Sweep testing for intracapsular swelling. Assess Quadriceps Tendon Mobility, ITB, look for tissue restrictions lateral and medially. Knee ROM: Measure Flexion and Extension Special tests in Supine 1. Anterior Drawer/ Lachman’s test: ACL sprain/tear 2. Posterior Drawer/ Godfrey’s Test: PCL sprain/tear 3. Valgus Stress Test: Pain, Laxity @ full extension (medial capsule, MCL, cruciates) @ 25 degrees knee flex. (MCL sprain). 4. Varus Stress Test: Pain, Laxity @ full extension (lateral capsule, LCL, cruciates) @ 25 degrees knee flex. (LCL sprain). 5. Slocum drawer Tests: Anterior medial Instability (ER), Anterior lateral instability (IR) 6. Hughston’s Drawer Test: Posterior medial Instability (IR), Posterior lateral instability (ER) 7. McMurray’s Test: 3 passes (Neutral, IR, ER) Valgus force w/ flexion and Varus force w/ extension. For Meniscal Tears. 8. Thomas test: Rectus Femoris Tightness/ Hip Flexor Tightness 9. Hamstring Length Testing: 90/90 test (Objective) In Side Lying Ober’s test: ITB tightness Abductor strength: Glut med weakness can cause over compensation of ITB which leads to tissue tightness. In Prone: Hamstring and Gastroc Tendon Mobility @ the knee: Look for muscular restrictions and tendon tightness. Gastroc/Soleus: Achilles tendon tightness: Hypo-mobility at the ankle can cause knee pain. Apley’s Test: Compression w/ IR/ER followed by Distraction w/ IR/ER: Meniscal tear/Collateral/Cruciate ligament tear. Ankle Pain: Minimize Position changes for Pt/ comfort. In Sitting: Gross LE ROM LE MMT: Don’t forget Ankle Eversion/ inversion Reflexes Measure DF/PF/INV/EV ROM AROM/PROM Special tests in Sitting 1. Syndesmosis Squeeze Test: High Ankle Sprain 2. External Rotation Test: high Ankle Sprain In Supine Assess edema formation Assess accessory motions Assess Mid Foot Mobility, Talus Mobility, Great Toe Mobility Special Testing: 1. Valgus Stress test: Deltoid Ligament Integrity 2. Varus Stress Tess: ATF. CF. PTF tears 3. Anterior Drawer: ATF ligament sprain 4. Talar Tilts: Inversion w/: PF (ATF ligament), Neutral (CF ligament), and DF (PTF ligament). Eversion: Deltoid Ligament. 5. Plantar fascia: restrictions, tender points. In Prone: Gastroc Soleus: Achilles tendon mobility, tissue restrictions. Thompson Test: Achilles tendon rupture