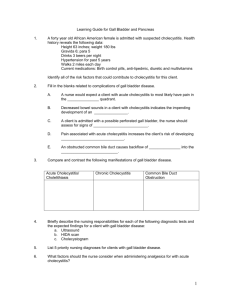
engtests gastro125
advertisement

1. Xylose absorption tests is good screening test for A. Fat absorption B. Pernicious anaemia C. Carbohydrate absorption * D. Amino acid absorption E. Protein absorption 2. Abnormal schilling test which persists after intrinsic factor is given suggests A. Blind loop syndrome * B. Pernicious anaemia C. Defective marrow D. Total gastrectomy E. Sectoral gastrectomy 3. Specific test for malabsorption A. D-xylose test * B. Schilling test C. Fecal fatestimation D. Hydrogen breath test E. X-xylose test 4. Whipples disease is associated with A. Cerebellar ataxia B. All * C. Dementia D. Supranuclear ophthalmoplegia E. It is not associated with anything 5. Patient with congenital lactose deficiency will experience distension, flatulence and diarhoea after ingestion ofA. Glucose 6. 7. 8. 9. B. Sucrose C. Milk * D. Eggs E. Cheese Diarrhoea, flatulence and abdominal cramps aftersucrose ingestion is probably due toA. Disacaharidase deficiency * B. Insulinoma C. Diabetes mellitus D. Glucose-6 phosphate dehydrogenase deficiency E. Violation of glucose tolerance Rare complication of ulcerative colitis – A. Pseudopolypi B. Carcinoma * C. Toxic dilatation D. Massive hemorrhage E. Perforation Perecentages of small intestine which can be removed without causing much digestive disabilitiesA. 10% B. 0% * C. 70% D. 90% E. 55% Coeliac disease is associated with HLA.... A. A-3 B. DR-3 C. D&8 D. DR-4 E. None * 10. Extra intestinal complication which is more common in Ulcerative Colitis than Crohns disease A. Uveitis B. Pyoderma gangrenosum * C. Cirrhosis D. Cholangiocarcinoma E. Pyoderma simplex 11. Which is not true about arthritis, which is associated with inflammatory bowel disease A. Migratory arthritis B. Knee joint most common C. Deformations are common* D. Correlates to severity of colitis E. Deformations are local 12. Fibrosis around Brunner's glands is characteristic of A. Intestinal lymphoma B. Radiation eneritis C. Amyloidosis D. Scleroderma * E. Gastroineritis 13. Treatment for psuedomembranous enterocolitis including all methods,except A. Retention enema of saline with faecal suspension B. Azulfidine C. ACTH D. Sodium colistimethate E. All * 14. All is true about short bowel syndrome except A. Intestinal transmit time is increased * B. Nutritional deficiency present C. Site atorrhea present D. None E. Decreased 15. Punctuated yellow exudate in colon, which was found during endoscopic examiantion are indicative ofA. Balantidium coli B. Ulcerative colitis C. Antibiotic colitis * D. Gluten induced enteropathy E. Hemocolitis 16. After extensive small bowel resection, increased incidence of renal stones is due to A. Increased absorption of Vit. D B. Increased CA absorption from rectum C. Increased acid loss duodenum D. Increased oxalate absorption * E. Decreased oxalate absorption 17. Loss of 90% of ileum & jejunum leads to all of following sings,except A. Anemia B. Osteomalacia C. Fluid loss D. All * E. General weakness 18. Jejunal biopsy is diagnostic in A. Celiac Sprue B. Tropical Sprue C. Whipple's disease * D. Radiation enteritis E. In all cases 19. Regarding incidence of Ca during ulcerative colitis which is true forA. Arise from pseudopolyps B. Increased incidence if age of ulcerative colitis is early * C. Always associated with exraintestinal manifestation D. decreased incidence with increase in age E. Decreased incidence if age of ulcerative colitis is early 20.According to ERCP, what are found to have associations with chronic pancreatitis? * Biliary obstruction and Pancreatic duct abnormalities Pancreatic duct abnormalities Biliary obstruction None of mentioned Tumor of pancreas 21. Adversely affect survival include all of the following except * anemia less than 70 g/l age greater than 55 years, leukocytosis greater than 16,000/µm, LDH greater than 400 IU, AST greater than 250 IU/L. 22.All are true about pseudopancreatic cyst except Presents as an abdominal mass Serum amylase is increased Common after acute pancreatitis Common after acute cholecystitis * Most common site is in head of pancreas 23. All are true regarding Zollinger Ellison syndrome, except: severe peptic ulceration Hypergastrinemia Diarrhoea increased levels of the hormone gastrin * Decreased ratio of BAO to MAO 24.All of following may be in acute pancreatitis except: Hyperbilirubinemia Serum alkaline phosphatase is elevated Serum aspartate aminotransferase is elevated Elevated serum lactic dehydrogenase * Serum albumin is increased 25. All of the following have been used in management of Acute Pancreatitis except * Interleukin-10 Quamatel Somatostatin Peritoneal dialysis None of the listed 26.All of the following statements about Pseudopancreatic cysts are true except: Cystojejunostomy is treatment of choice Serum amylase levels are increased Presents as an epigastric mass Most common site is in body and tail of pancreas * Percutaneous aspiration is treatment of choice 27. All the following are causes of Acute Pancreatitis except: Alcohol Gall stones Hypercalcemia Hyperlipidemia * Hemochromatosis 28.An elderly man presents with severe epigastric pain radiating to the right hypochondrium. The pain has been worsening over the past day and a half and goes through to his back and shoulders. The patient feels sick and has vomited several times. He is jaundiced. Hepatitis A Hepatitis B Hepatitis C * Gallstones Pancreatitis 29.An elderly woman presents with painless jaundice and weight loss. On physical examination you find the gallbladder to be enlarged. Choose the single most likely diagnosis Gallstones Crohn's disease Duodenal ulcer Duodenitis * Carcinoma head of pancreas 30. An elderly woman presents with painless jaundice and weight loss. On physical examination you find the gallbladder to be enlarged. She enjoys smoking and drinking. Choose the single most likely investigation from the list of options above * Carcinoma head of pancreas Reflux oesophagitis Acute pancreatitis Chronic pancreatitis Duodenal ulcer 31. Antimitochondrial antibody test is characteristic sign of * Primary biliary cirrhosis Sclerosing cholangitis Anaerobic liver abscess Hepatoma Hepatitis C 32. Antimitochondrial antibody test is characteristic sign of * Primary biliary cirrhosis Sclerosing cholangitis Anaerobic liver abscess Hepatoma Hemochromatosis 33. Antimitochondrial antibody test is characteristic sign of * Primary biliary cirrhosis Sclerosing cholangitis Anaerobic liver abscess Hepatitis D Hemochromatosis 34. At present, gall stones are considered certainly as a cause of: Chronic pancreatitis * Acute pancreatitis Both chronic and acute pancreatitis None of above Tumour of pancreas 35. Carcinoma of the gallbladder is a result of: Hepatic disease * Presence of cholelithiasis with chronic chole¬cystitis Cholecystography Ultrasound examination of the gallbladder Constipation 36. Causes of Acute Pancreatitis are all of the following except: Alcohol ingestion Biliary tract disease (gallstones) Postoperative state (after abdominal or nonabdominal operation) * Gastritis Trauma 37. Causes of Hyperamylasemia and Hyperamylasuria are all of the following except: Acute Pancreatitis Chronic Pancreatitis Pancreatic pseudocyst Renal insufficiency * Respiratory insufficiency 38. Causes of Hyperamylasemia and Hyperamylasuria are all of the following except: Biliary tract disease: cholecystitis, choledocholithiasis Perforated or penetrating peptic ulcer * Acute leukaemia Acute Pancreatitis Chronic Pancreatitis 39. Drug of choice in Zollinger Ellison syndrome is B-blocker Ranitidine Antacids Atropin * Omeprazole 40.For Primary biliary cirrhosis select the circulating antibodies with which it is most closely associated: * antibodies to mitochondria antibodies to native DNA; antibodies to smooth muscle cells; antibodies to acetylcholine receptors; antibodies to parietal cells. 41. Gall bladder stone formation in caused by all except: * Leucocytosis Hyperalimentation Primary biliary cirrhosis Clofibrate therapy None of mentioned 42.In acute pancreatitis, the pancreas: * is characteristically enlarged has scattered calcification has ductal decompression is replaced no changes 43. In which one of the following situations would therapy with oral chenodeoxycholic acid be most effective in dissolving gallstone(s)? A 27-year-old Asian woman with thalassemia A 49-year-old woman with two 2-cm stones A 60-year-old man with gallstones visible on chest x-ray * A 45-year-old woman with a history of gallstone pancreatitis and a residual 1-cm radiolucent gallstone 44.A 55-year-old man with a history of biliary colic, several small gallstones seen on ultrasonography, and a poorly opacified gallbladder after oral cholecystography Increased amylase may be seen in all of the following except: Pancreatic pseudocyst Perforated peptic ulcer Cancer of the pancreas Acute pancreatitis * Appendicitis 45. Ingestion of arsenic causes * Non cirrhotic portal fibrosis Hepatic adenoma Hepatic carcinoma Hepatic cirrhosis Pancreatic carcinoma 46.It is supposed that gall stones can result in chronic pancreatitis because they may induce: * Inflammation and stenosis or obstruction of ampulla of Vater Fever Abdominal pain None of mentioned Peptic ulcer 47. likely explanation for these findings? Bile duct tumor Choledocholithiasis Congenital polycystic liver Primary biliary cirrhosis * Primary sclerosing cholangitis 48.Marker of Cholestatic syndrome in hepatitis is * ^Alkaline phosphatase All of above vfibrinogen ^AST ^ALT 49.Markers of Cholestatic syndrome in hepatitis are all of the following except * ^ALT ^cholesterol ^Bilirubin ^Alkaline phosphatase ^GGT 50.Markers of Cholestatic syndrome in hepatitis is * All mentioned ^cholesterol ^Bilirubin ^Alkaline phosphatase ^GGT 51. Markers of Cholestatic syndrome in liver diseases are * ^Bilirubin, ^Alkaline phosphatase, ^GGT, ^cholesterol ^AST, ^ALT, ^GGT, ^Bilirubin vAlbumine, vprothrombin, vcholesterol, vfibrinogen ^ESR, ^ᵞ-globulins, ^timol test ^Le, ^C-react. protein None of mentioned 52. Metabolic changes associated with excessive vomitting includes the following: Metabolic acidosis Hyperchloremia Decreases bicarbonates Hypercalciemia * Hypokalemia 53. Most Common Cause of death in early acute Pancreatitis is * Respiratory Failure Cardiac failure Renal Failure Uncontrolled Coagulopathy None of the listed 54. Most common complication of acute pancreatitis is: Phlegmon Pancreatic abscess Pleural effusion Appendicitis * Pseudocyst 55. Most common site of cholangiocarcinoma is * Hepatic duct bifurcation Intrahepatic Lower End of CBD (Common Bile Duct) Lower 1/3rd of CBD (Common Bile Duct) None of mentioned 56. Most lesions of pancreas on CT are characterized by all of the following except: * the presence of ductal decompression enlargement of the pancreatic outline, distortion of the pancreatic contoura a fluid filling that has a different attenuation coefficient than normal pancreas none of the listed 57. Nealon's classification is used for Acute pancreatitis chronic pancreatitis * pseudocyst pancreas alcoholic pancreatitis None of above 58. Peptic ulcer should be differentiated with all of the following except Cholecystitis Gastritis Myocardial infarction Pancreatitis * Pneumonia 59. Peptic ulcer should be differentiated with all of the following except Stomach cancer Gastritis Gastroesophageal reflux disease Pancreatitis * Bronchial asthma 60.Peptic ulcer should not be differentiated with * Ulcerative colitis Cholecystitis Gastritis Miocardial infarction Pancreatitis 61. Pruritus, elevation of alkaline phosphatase and positive antimitochondrial antibody test are characteristic signs of * Primary biliary cirrhosis Sclerosing cholangitis Anaerobic liver abscess Hepatoma Hepatitis C 62.Put preliminary diagnosis. * Chronic cholecystitis, acute phase. Chronic cholecystitis, subacute phase. Chronic cholecystitis, phase of remission. Dyskinezia of bile ducts. Rotor’s syndrome. 63. Raised serum amylase levels are used to diagnose Acute cholecystitis Degenerative diseases Autoimmune disease Appendicitis * Acute pancreatitis 64. Cell present in large numbers in the fluid of Tuberculous peritonitis areA. Eosinophils B. Polymorphs C. Lymphocytes * D. Monocytes E. Neutrophils 65. Treatment of drug induced gastritis – peritont A. Mesoprostol B. H,receptorblock * C. Antacids D. Famotidine E. Ranitidine 66.Which of the following cations is presents gastric juice in a larger concentration than in blood plasmaA. Na+ B. K+ * C. Mg+ D. Ca+ E. Lithium 67. Progressive dysphagia is seen inA. Carcinoma esophagus * B. Globus hystericus C. Presbyesophagus D. Achalasia E. Gastric carcinoma 68.Carcinoma stomach is associated with blood group – A. A* B. B C. AB D. 0 E. None 69. Stress ulcers seen in burns are – A. Curling's ulcer * B. Cushing's ulcer C. Meleney's ulcer D. Rodent ulcer E. Intestinal ulcer 70.Most common cause of decrease in incidence of H.pylori in west is d/t A. Change in the style * B. Increased use of PP1 C. Chemotherapy D. Mutation in organism E. Bad food 71.Treatment of H. pylori is required in all of the following expect? A. Gastro esophageal reflex disease * B. Gastric ulcers C. Duodenal ulcers D. Gastric lymphoma E. Tumor of pancreas 72.True regarding GERD is all except A. Avoid coffee & Tea B. Transient lower esophageal relaxation C. Lower esophageal sphincter length and its pressure is important * D. Proton pump inhibitor is the treatment of choice E. Avoid meet and sugar 73.Eradication of helicobacter pylori has been proved to be beneficial in which of the following disorders of the stomach A. Low grade malt lymphoma * B. Prosive gastritis C. Carcinoma stomach D. Gastroesophageal disease E. Thyroid carcinoma 74..H. Pylori is known to cause all of the following exceptA. Gastric ulcer B. Duodenal ulcer C. Gastric lymphoma D. Fundal gastritis * E. Tumor of large intestine 75.True about mucosa associated lymphoma A. H. Pylori predisposes * B. Chemotherapy sensitive C. Multiple lymphomas D. Stromal polyp E. Diffuse poliposis of large intestine 76.All are true regarding Helicobacter pylori except A. Less prevalent in developing countries * B. Toxigenic strains usually causes ulcers C. Urea breath is positive D. Gram negative organism E. Gram positive organism 77.Diagnostic tests for H. Pylori include all of the following exceptA. Urea-breath test B. Rapid urease test C. Gastric biopsy & Warthin-starry stain D. SAFA test * E. pHmetry 78. Epidemiological studies of H. Pylori are done by using A. Urea-breath test B. Serological markers * C. Culture D. Gastric-biopsy urease test E. SAFA test 79.A patient with H. pylori infection is treated with drugs. The best method to detect presence of residual H. pylori infection in this person is A. Rapid urease test B. Urea breath test * C. Endoscopy and biopsy D. Serum anti H. pylori titre E. Serological markers 80. Which drug is not effective against H.pylori – A. Colloidal Bismuth B. Metronidazole C. Amoxicillin D. Erythromycin * E. Clotrimazoli 81. All are used in treatment of Helicobactor pylori, EXCEPTA. Colloid bismuth B. Cisapride * C. Clarithromycin D. Metronidazole E. Amoxicillin 82. All of the following drugs are commonly used in regimens against H. pylori except – A. Oxytetracycline * B. Amoxicillin C. Bismuth subcitrate D. Omeprazole E. Tetracyclini 83.All of the following are true regarding a patient with acid peptic disease except A. Misoprostol is the drug of choice in patients on NSA1DS B. DU is preventable by the use of single night time H, blockers * C. Omeprazole may help ulcers refractory to H2 blockers D. Mesoprostol is DOC in pregnant patients E. All above 84. Stress ulcers seen in burns are – A. Curling' ulcer * B. Cushing's ulcer C. Meleney's ulcer D. Rodent ulcer E. Intestinal ulcer 85.Early gastric cancer generally indicates A. Gastric adencarcinoma detected early B. Gastric adenocarcinoma confined to the mucosa C. Gastric adenocarcinoma confined to the mucosa & submucosa * D. Gastric adenocarcinoma less than 1 cm. In size E. Gastric adenocarcinoma less than 2 cm in size 86. Treatment of Heliobactor pylori are except – A. Clarithromycin B. Cisapride * C. Bismuth subsalicylate D. Metronidazole E. Tetracyclini 87.Histopathological findings in Whipple's disease include all of the following except - A. Marked increase in the number of macrophages in the mucosa. B. Marked increased in the number of intraepethelial lymphocytes * C. Dilatation of lymphatics in the mucosa D. Lipid deposition in the mucosa E. Protein deposition in the mucosa 88.Does not affect prognosis in acute pancreatitis A. Leucocytosis> 19000 B. Amylase > 8000IU * C. Albumin < 3.2 gm/dl D. Age > 60 yrs. E. Age <70 yrs. 89.Best diagnosis of pancreatic cancer (head) is by – A. Ultrasound B. ERCP * C. CAT scan D. PTC E. Angiography 90.Ectopic ACTH syndrome is seen most common 1> withA. Renal cell carcinoma B. Lymphoma C. Bronchogenic carcinoma * D. Pituitary adenoma E. Acute pancreatitis 91. Carcinoma pancrease attains largest size when it is sited inA. Head B. Ampulla C. Body & tail * D. Periampullary E. Tail 92. Increased C-peptide is seen in – A. Glucagoma B. Insulinoma * C. Gastrinoma D. Hepatoma E. Carcinoma 93. Investigation of choice for pancreatic islet cell tumour is A. CT scan B. MRI C. Nuclear scan * D. USG E. Capilaroscopy 94.Serum amylase level is raised in all except A. Acute pancreatitis B. Perforation of stomach C. Strangulated small intestine D. Acute appendicitis * E. Acute fase of myocardial infarction 95.Pentagastrin-fast achlorhydria in patient with gastric ulcer indicates A. Antral ulcer B. Malignant ulcer * C. Zollinger - Ellison syndrome D. Gastric lymphoma E. Intestinal ulcer 96.Surum smylase usually becomes elevated in acute pancreatitis after. hrs A. 1/-2 hrs. B. 4-6 hrs. C. 24-48 hrs. * D. 48-72 hrs. E. 72-96 hrs. 97. Zollinger Ellison syndrome is cused by – A. Non Beta cells * B. Beta cells C. Alpha cells D. Non Alpha E. Non Beta 1 cells 98. The medical treatment of Zollinger Ellison's syndormeisA. Cimetidine B. Ranitidine C. Famotidine D. Omeprazole * E. Pansoprasole 99.Best progonosis in acute pancreatitis is seen with pancreatitis A. Gall stones * B. Viral C. Post operative D. Alcoholic E. With dyscynesia 100. Diarrhoea in Zollinger Ellison syndrome is due toA. Pantagastrin B. Secretin C. Gastrin * D. Enterokinin E. Holecystokinin 101. Carcinoma of pancreas attains greatest size when it is located in A. Head B. Body and tail * C. Ampullary region D. Ampula of vater E. Head and body 102. .Which one of the following types of pancreatitis has the best prognosis A. Gall stone pancreatitis * B. Alcoholic pancreatitis C. Idiopathic pancreatitis D. Traumatic pancreatitis E. Edeamatic pancreatitis 103. Raised serum amylase is not seen in A. Appendicitis * B. Pancreatitis C. Blocked salivary duct D. ectopic pregnancy ruptured E. Hepatitis 104. Which one of the following is best avoided in the treatment of acute pancreatitis A. Antibiotics B. Nasogastric suction C. Anti cholinergics * D. Morphine E. Infusional therapy 105. The following can be associated with acute pancreatitis EXCEPTA. Hyperparathyroidism B. Hyperthyroidism * C. Hypercalcemia D. Hypertriglceridemia E. Hypocalcemia 106. The most common hormone other than gastrin, contained in the gastric secreting islet cell tumour is A. ACTH * B. Glucagon C. Melanocyte stimulating hormone D. Growth hormone releasing factor E. Insulin 107. Most common tumor of pancreas isA. Insulinoma * B. Gastrinoma C. APUD'somas D. VIPoma E. Carcinoma 108. Complications of chronic pancreatitis include the following except A. Portal hypertension B. Obstructive jaundice C. Duodenal obstruction D. Renal artery aneurysm * E. Renal hypertension 109. Most important screening test for acute pancreatitis is- A. Serum amylase * B. Serum lipase C. CT(Abdomen) D. ERCP E. Elastase 110. Carcinoma pancrease attains largest size when it is sited in A. Head B. Ampulla C. Body & tail * D. Periampullary E. Whole gland 111. All are complications of ulcerative colitis exceptA. Haemorrhage B. Stricture C. Malignant change D. Polyposis E. Oesophageal varices * 112. Post diarrhoeal paralytic ileus occurs in – A. Hypokalemia B. Hypomagnesemia * C. Hypocalcemia D. All of the above E. None 113. Paralytic ileus is a feature of all exceptA. Retroperitoneal hematoma B. Hypokalemia C. Diabetes * D. Porphyria E. Hypertension 114. Characteristic features of ischaemic colitis at the onset of an attack include A. Steatorrhoea B. Normal barium enema C. Necessity of emergency surgery D. Signs of generalized peritonitis E. None * 115. Fatal gastroenteritis is caused by A. Typhoid * B. Amoebiasis C. Anthrax D. Giardiasis E. Stafylococcus 116. The normal fecal fat excretion is – A. Less than 5 gm/day * B. 8 gm/day C. 10 gm/day D. 15 gm/day E. 20 gm/day 117. Coeliac disease is associated with HLA.... A. A-3 B. DR-3 C. DE-8 D. DR-4 E. None * 118. Which is not true of arthritis associated with inflammatory bowel disease A. Migratory arthritis B. Knee joint most common C. Deformities are common * D. Correlates to severity of colitis E. Rheumatoid arthritis 119. Earliest pathological change is X-ray in Ulcerative ColitisA. Loss of haustration B. Aphthous ulcerations C. Mucosal granularity * D. Skip tensions E. There no changes 120. Celiac sprue causes malabsorption syndrome due toA. Coliform infection of small bowel B. Lactase deficiency C. Hypersensitivity to dietary gluten * D. Ischaemia of celiac artery E. Amilase defficiency 121. The schilling test is performed to determine the cause ofA. Lactose malabsorption B. Fatty acid malabsorption C. Amino acid malabsorption D. Cobalamin malabsorption * E. Gluten malabsorption 122. All are features of irritable bowel syndrome EXCEPTA. Vomiting * B. pain abdomen C. Diarrhoea D. E. 123. A. B. C. D. E. 124. A. B. C. D. E. Constipation Nausea Antigliadin antibodies are delectable in Tropical sprue Whipple's disease Celiac disease * Intestinal lymphoma Lactase malabsorption Best test for Small intestine malabsorption of carbohydrates is Lund meal test Shilling test D-Xylose test * Follacin test pH metry