The Role of Fibrinogen in Reducing Transfusion
advertisement

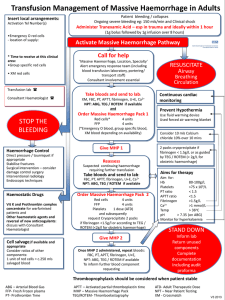
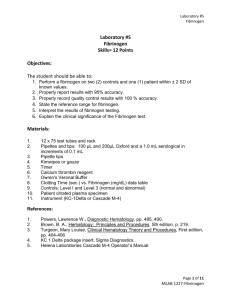
The Role of Fibrinogen in Reducing Transfusion C. David Mazer, MD, FRCPC Objectives: After attending this session, the participant will be better able to 1. discuss the pathophysiology of fibrinogen in the setting of massive bleeding and transfusion 2. explain the rationale for clinical trials involving administration of fibrinogen in these situations. Significant bleeding after cardiac surgery is common clinical problem. Allogeneic transfusion rates are variable but may approach 100% in some centers and for some procedures. Because of the risks, costs and adverse outcomes associated with transfusion (especially massive transfusion), there is an urgent need to evaluate the use of hemostatic agents and coagulation concentrates in this setting. Potential advantages could include low volume, pathogen inactivated, readily available and easily administered products which could be dose titrated. Fibrinogen is an essential component of the clotting system. The normal plasma concentration is between 1.5 and 4.0 g/L, although it can be higher in some clinical settings. It is a soluble, 340 kDa plasma glycoprotein which is cleaved to produce fibrin monomers, the basis of the clot. It also facilitates platelet aggregation, and is an acute phase reactant. Fibrinogen levels decrease in cardiac surgery patients because of bleeding, fibrinolysis, hemodilution, and consumption; low levels are associated with increased bleeding and transfusion. Fibrinogen is one of the first clotting factors to fall to critical levels in the surgical or trauma setting and low preoperative levels have also been found to be predictive of bleeding and transfusion. Recent guidelines recommend administration of fibrinogen in a bleeding patient when the concentration falls below 1.5–2.0 g/L. Plasma levels of fibrinogen can be assessed using spectroscopic (Clauss) techniques or by viscoelastic rotational thromboelastometry (eg ROTEM). There are 3 main sources of fibrinogen for perioperative use: Frozen plasma (FP), cryoprecipitate and fibrinogen concentrate. FP is obtained from centrifugation of donated blood and thus contains all proteins in human plasma in the same concentration as blood. Because of the complications associated with plasma administration, its use is increasingly being replaced with other products. Cryoprecipitate is made by thawing, centrifugation and separation of fresh frozen plasma. Each 15 ml unit of ‘cryo’ contains about 250-400 mg of fibrinogen. Fibrinogen concentrates are purified, heat-treated, lyophilized concentrates of human plasma fibrinogen which can be stored at room temperature. Different preparations are available in different jurisdictions. Fibrinogen concentrates are approved for treatment of fibrinogen deficiency in Europe and North America. Retrospective and prospective studies have documented the ability to raise fibrinogen levels with fibrinogen replacement. To increase fibrinogen concentration by ~1 gm/L in the typical patient would require about 3 gm of fibrinogen (or the equivalent of 1500-2000 ml FP, 8-10 units of cryoprecipitate or 100-300 ml of reconstituted fibrinogen concentrate). Recent randomized controlled trials have studied fibrinogen concentrate in patients undergoing cardiovascular surgery. In these studies, ROTEM guided fibrinogen concentrate administration in bleeding patients after aortic surgery significantly reduced the amount of allogeneic transfusion. A multicenter international RCT of Fibrinogen concentrate during complex cardiovascular surgery is currently in progress. While the relatively small amount of data so far is promising, recent systematic reviews and meta-analyses of the clinical trials to date highlight the need for more research to establish the optimal dosing, method, monitoring, efficacy, safety and cost-benefit of fibrinogen replacement for reducing transfusion in cardiac surgery. Selected References: Bolliger D, et al. Pathophysiology and treatment of coagulopathy in massive hemorrhage and hemodilution. Anesthesiology 2010;113:1205–19 Gielen C, et al The effects of pre- and postoperative fibrinogen levels on blood loss after cardiac surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2013 doi: 10.1093/icvts/ivt506 Karkouti K, et al. The relationship between fibrinogen levels after cardiopulmonary bypass and large volume red cell transfusion in cardiac surgery: an observational study. Anesth Analg. 2013 Jul;117(1):14-22. Karkouti K, et al. The influence of perioperative coagulation status on postoperative blood loss in complex cardiac surgery: a prospective observational study. Anesth Analg. 2010 Jun 1;110(6):1533-40 Karlsson M, et al. Prophylactic fibrinogen infusion reduces bleeding after coronary artery bypass surgery. A prospective randomised pilot study. Thromb Haemost 2009;102:137– 44 Kozek-Langenecker SA, et al Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2013;30(6):270-382 Levy JH, et al Fibrinogen and hemostasis: a primary hemostatic target for the management of acquired bleeding. Anesth Analg. 2012;114(2):261-74. Ozier Y, Hunt BJ. Against: Fibrinogen concentrate for management of bleeding: against indiscriminate use. J Thromb Haemost 2011;9:6–8 Rahe-Meyer N, et al. Fibrinogen concentrate reduces intraoperative bleeding when used as first-line hemostatic therapy during major aortic replacement surgery: results from a randomized, placebo-controlled trial. J Thorac Cardiovasc Surg. 2013 Mar;145(3 Suppl):S178-85. Rahe-Meyer N, et al Effects of fibrinogen concentrate as first-line therapy during major aortic replacement surgery: a randomized, placebo-controlled trial. Anesthesiology. 2013 Jan;118(1):40-50. Rossaint R, et al Management of bleeding following major trauma: an updated European guideline. Crit Care. 2010;14(2):R52 Solomon C, et al Time course of haemostatic effects of fibrinogen concentrate administration in aortic surgery. Br J Anaesth. 2013;110(6):947-56 Tanaka KA, et al Transfusion and hematologic variables after fibrinogen or platelet transfusion in valve replacement surgery: preliminary data of purified lyophilized human fibrinogen concentrate versus conventional transfusion. Transfusion. 2014;54(1):109-18. Yang L, et al. Postoperative fibrinogen level is associated with postoperative bleeding following cardiothoracic surgery and the effect of fibrinogen replacement therapy remains uncertain. J Thromb Haemost. 2013 Aug;11(8):1519-26. Weber CF, et al. Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology. 2012 Sep;117(3):531-47. Wikkelsø A, et al. Fibrinogen concentrate in bleeding patients. Cochrane Database Syst Rev. 2013 Aug 29;8:CD008864. doi: 10.1002/14651858.CD008864.pub2.