Community Grand Rounds*Re-Engineering Community and
advertisement

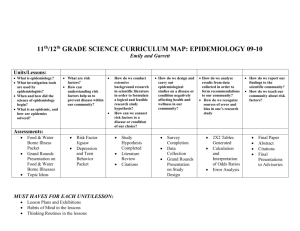
<T>Community Grand Rounds: Re-Engineering Community and Academic Partnerships in Health Education—A Partnership and Programmatic Evaluation <author> Kevin Heaton, MD1, George R. Smith, Jr. MPH2, Kimberly King, MPH3, Natalie Watson, MA2,4, Jen Brown, MPH5, Gina Curry, BSPH6, Brandon Johnson, JD7, Betty Nichols, MA8, Bernetta Pearson, RN9, Ernest Sanders, BA10, Norma Sanders, BS11, and Doriane Miller, MD2,4,12 <run head>Community Grand Rounds <run author>Heaton et al. <info>(1) University of Chicago, Pritzker School of Medicine; (2) University of Chicago Medicine, Center for Community Health and Vitality, Urban Health Initiative; (3) University of Chicago Medicine, Comprehensive Cancer Center, Office of Community Engagement and Cancer Disparities; (4) University of Chicago, Institute for Translational Medicine; (5) Northwestern University, Clinical and Translational Sciences Institute, Alliance for Research in Chicagoland Communities, Community-Engaged Research Center; (6) Northwestern University, Feinberg School of Medicine; (7) Washington Park Consortium; (8) South Chicago Community Leader; (9) Woodlawn Community Member; (10) Partnership for a Connected Illinois, Broadband Illinois; (11) Greater Auburn Gresham Development Corporation; (12) University of Chicago, Department of Medicine <abstract subhead>Abstract <abstract>Background: Community participation in population health improvement can assist university researchers in targeting intervention resources more effectively and efficiently, leading to more effective implementation of interventions, because of joint ownership of both process and product. Two academic health centers partnered with community based organizations to develop a bidirectional educational seminar series called “Community Grand Rounds” (CGR), which identified health concerns of Chicago’s South Side residents and provided information regarding university and community resources that addressed community health concerns. Objectives: We evaluated the community consultants’ perceptions of the quality and effectiveness of the planning and implementation of the seminars that resulted from the partnership. Methods: We conducted one-on-one interviews and focus groups with community consultants to assess their perceptions of the partnership using a tailored version of a previously developed individual and focus group interview instrument. Analysis of the interview text was conducted using grounded theory where themes were coded as they emerged. Conclusions: CGR is an effective mechanism for providing needed community health information in an easily accessible format. Additional work is needed to determine whether this format represents a sustainable community–university partnership. <abstract subhead>Keywords <abstract>Community-based participatory research, anthropology, power sharing, needs assessment, health promotion <info>Submitted 29 October 2012, revised 22 March 2013, accepted 16 June 2013 <N>Collaborative partnerships between community and academic health organizations have been shown to effectively improve population health, especially those partnerships that emphasize community needs and input.1-6 CGR grew out of a need to improve the interactions and communications between South Side residents and the University of Chicago Medicine. The primary service area of the University of Chicago Medicine encompasses 34 communities on the South Side of Chicago that are home to approximately 870,000, with a population that is 70% African American.7 Historically, there have been tense and sometimes unfavorable interactions and dialogue between local residents and the University of Chicago Medicine, resulting in decades of mistrust and negative perceptions on behalf of area residents. African Americans, whether residing on the South Side of Chicago or in other United States geographic areas, have had a long-standing distrust of medical providers, especially academic medical centers where research is developed and conducted.8-15 This mistrust can be attributed to a history of segregation, institutional racism, and unethical medical practices such as those employed in the Tuskegee Syphilis Study.16-20 In 2008, the Office of Community Affairs at the University of Chicago Medicine conducted an appreciative inquiry process, a strength-based problem-solving approach,21 with the intent of improving university relations with local residents. During the inquiry process, the Office of Community Affairs obtained information from community members and thought leaders on ways in which the University of Chicago Medicine could collaborate more effectively and efficiently in tangible ways to improve health and health outcomes. The inquiry was an informative experience, resulting in candid and helpful responses. Through the inquiry process, the Office of Community Affairs was able to formulate a definition of healthy community “as one that focused on the social, educational, and economic environment of its surroundings as well as access to high quality primary health care” (Elsmo L. Personal communication, 2009). Utilizing the principles of community-based participatory research, which has proved to be an effective research paradigm resulting in more effective participation from community partners,2229 the agenda for the Center for Community Health and Vitality and its first community-based information program, CGR, was shaped. Community members were interested in an approach that provided them with accessible educational activities and allowed for engagement with both academic and community professionals. This interest led to the development of CGR. After a 6month planning process, the first CGR took place in October 2010. CGR was designed as a collaborative partnership in which community and academic partners would work together to determine the topics, delivery vehicle, and location of each educational seminar (Table 1). The community partners, also known as Community Consultants, are active leaders in their communities with strong connections to their communities’ business and social networks. Supported by researchers showing the benefits of paying community partners as consultants and motivated by respect and high regard for the expertise of community partners, CGR generated paid consultant opportunities for community members.30 <T>Table 1 <N> Community Consultants were recruited from the leadership of the seven South Side sites of the Local Initiatives Support Corporation/Chicago New Communities Program (NCP), representing 11 distinct communities. Begun in 2003, NCP is a long-term initiative to support comprehensive community development in 16 Chicago neighborhoods. NCP agencies are committed to spending at least 10 years implementing their quality-of-life plans. Through local and citywide partnerships, NCP communities address employment, housing, recreation, commercial and retail development, child care, education, neighborhood aesthetics, and personal security. Unlike traditional academic health center grand rounds, which are held in hospital auditoriums, these seminars were held at community venues. Community Consultants worked collaboratively to recruit participants through the utilization of social media, email, word of mouth, and printed marketing materials. Each consultant was responsible for recruiting participants from their represented South Side community. Participants were targeted based on the topic of the CGR. For example, Chicago Hyde Park Village, a group of aging community residents, was consulted when the focus of the CGR was on older adults. Likewise, Chicago Youth Programs, an organization that provides educational and mentoring services, was significant in assisting with youth recruitment. Attendees of the CGR included representatives of various community-based organizations, academic institutions, community residents, and health professionals. Attendees were offered light refreshments before a 60-minute presentation on a health-related topic that concluded with a 30-minute, open, question-and-answer period from the audience. Presenters were chosen based on their expertise in a specific CGR topic area. Community Consultants provided recommendations for potential presenters. Before the CGR, presenters were provided with a brief description of the seminar. After the presentation and question-and-answer session, representatives from community and academic entities were available at tables with flyers and descriptive posters to share information about various health services they provide. Community Consultants controlled the CGR development process with assistance from a Center for Community Health and Vitality staff member. During biweekly conference calls, consultants selected the health-related problems that were of paramount importance to their communities as topics for CGR events. Some examples of discussion topics include mental health resources for youth impacted by violence, asthma, diabetes and obesity prevention, and ethical issues regarding African Americans in research (Table 2). All participants received audience feedback forms asking them to assign a value to the CGR experience, rate their prior knowledge of the subject matter, rate the quality of the speakers, and rate their desire to have the events in a community venue. In addition, participants were provided with GOURD (Gift of Useable Research Data) generated from the community asset mapping work of the South Side Health and Vitality Studies, a research unit within Center for Community Health and Vitality. The GOURD consisted of geographical maps of place-based information about health resources and was specific to the CGR topic. For example, during the adolescent depression CGR the GOURD contained contact information for mental health resources. <T>Table 2 <A>Evaluation <N>Deciding on the correct community partners was integral to the program’s success. It was important to select partners who had established relationships with neighboring organizations and who worked collectively with community residents. NCP had done this while developing quality-of-life plans for their represented communities. Consistent with the principles of community-based participatory research, we conducted a formative evaluation of our partnership’s adherence to the key tenets of community–academic partnerships.31-33 Participatory researchers commonly use focus groups to document and evaluate the experiences of community and academic partners. The downside of focus groups that we hoped to counteract with in-depth individual interviews is that, in groups, dominant personalities can suppress others’ views and individual feelings or dissent from majority opinion can be lost.34 We used the semistructured interview guide and focus group guide developed by the Detroit Community-Academic Urban Research Center as templates in developing tailored survey instruments of our own (Appendixes A and B include the interview guides).35 We evaluated consultants’ perceptions of the quality and effectiveness of the partnership itself and of the educational seminars resulting from the partnership. In addition, the major domains that we sought to evaluate with our interview instruments include shared leadership, open two-way communication, levels of trust, clear goals, co-learning, capacity building, power sharing, equitable participation, and balance of knowledge generation and action. Interview text was analyzed for repeating ideas and themes using a grounded theory approach.36 <A>Individual Interview and Focus Group Process <N>Interviews were conducted by a trained medical student who was not a member of the partnership. Four of the nine individual interviews were also attended by an academic partner who assisted with data collection and interpretation, as well as meeting coordination. Community and university partners scheduled individual interviews to accommodate each other’s schedules, and interviews took place over several months in the fall of 2011. Scheduling individual interviews and a single focus group with all partners present was difficult and took months. The decision to conduct only a single focus group interview was because of the limited free time of Community Consultants. The single focus group took place in a conference room at the facility of one of the community partner’s organizations. Eight of the nine community partners were present for the focus group (the single missing partner had a scheduling conflict). The same medical student who conducted the individual interviews also conducted the focus group. A university partner was present to help coordinate and to take notes, but did not pose any questions or actively participate in the discussion. Interviews were conducted and audio-taped between October 2011 and January 2012. Following Israel’s method for key informant interviews, the two interviewers compared notes and discussed the interviews and their own understanding of responses.37-39 Transcripts from the interviews were analyzed using grounded theory for themes and were shared with all partners for clarification and to facilitate reflective discussion and improvement of group dynamics. A formal coding protocol was not used, but each interview was scanned for repeating ideas and phrases, measuring the frequency of occurrence to determine collective themes. Confidentiality was ensured by de-identifying transcribed interviews through the assignment of anonymous identification codes to each interviewed partner. The interview protocol was reviewed and approved by the University of Chicago Institutional Review Board as exempt. <A>Individual Interview and Focus Group Results <N>Community Consultants unanimously praised the partnership’s adherence to the principles of collaborative and equitable “group process” in the planning of the CGR seminar events. Much of the praise expressed by community partners in individual and focus group interviews pertained to the university partners’ adherence to the principles of community-based participatory research, for example, collaborative process, equitable group decision making, twoway communication, and transparency. <quote> They didn’t say, ‘Well we think you should talk about diabetes, or we think you should, you know,’ and each community had an opportunity to put down a top 3, top 5 things for ourselves. [Focus group participant] <N> Community Consultants also cited the university partners’ insight into community life and culture and their respect for the community. Multiple partners also expressed enthusiastic satisfaction with the paid “contract model” used to solidify the terms of the partnership and to specify the precise expectations of partners. <quote> [The academic partner] gets it. I think that while she’s on that research university hospitals track she understands community. [Individual interviewee] <A>Partners’ Expectations and Opinions <N>Most Community Consultants embarked on the partnership with modest but hopeful expectations. All hoped to benefit their communities by allying with the university, forming new relationships, raising awareness of health and quality-of-life issues, bringing new knowledge to the fight to improve the health and life of citizens, or bringing new funding streams or resources to their community. For most consultants, the CGR program met their expectations. For some, it exceeded their expectations. The collaborative process and the community events were very well-received by Community Consultants and residents. Consultants felt that they had co-created CGR, having decided on topics relevant to their community, venues, and programming. Consultants were impressed by the creativity of the seminars. The most cited example was the dramatic play written by a university partner at the request of the Community Consultants. The accessibility of educational content to community residents and the flexibility of medical center partners were manifested by their willingness to tailor the programming to the needs of each unique community. Consultants’ enthusiasm was, however, tempered by their concern over the sustainability and impact of one-night interventions attended by at most 100 to 200 community members. Multiple consultants felt the one-night event was insufficient to effect lasting change and expressed a wish to repeat seminars in their communities to reinforce the message. Community Consultants affirmed that the educational seminars had facilitated bidirectional communication between their community and the university medical center, but raised two critical issues concerning reliable measurement of the effect of CGR: 1) What outcomes signify success? and 2) How are we quantifying the effect of these seminars on the community residents? In this way, community partners provided visionary leadership and a rich source of ideas for improving and extending the influence of the CGR project. <quote> I think the overall sense of how successful the programs are is down the road. Because I think what we’re trying to do is bring about a change in behavior through an educational process, and I think the measurement perhaps for that is when we see decreases in diabetes and decreases in those particular health disparities that are so unique and common to us. [Focus group participant] <A>Perceptions of CGR Seminar Effectiveness <N>Community Consultants felt that the format and content of the seminars were effectively tailored to the unique needs of each community. They were happily surprised by the ability of university researchers to convey complex subject matter clearly and respectfully. Consultants also felt that community members were able to speak back to university researchers, whether through “question-and-answer” sessions or as co-members of expert panels sitting on the stage. Many community partners expressed enthusiasm for the creativity and local knowledge demonstrated in the CGR. Consultants were also pleased by the flexibility of program planning to accommodate the community residents, which they believed increased attendance and dissemination. <quote> I was worried my community would feel talked down to or like guinea pigs… [but] the staff were adept at translating intellectual medical into laymen’s [terms] without offending. They were able to convey the information very clearly and in deintellectualized ways that helped me and my community and the info was delivered in a way me and my community could understand. [Individual interviewee] I’ve been very pleased by the different types of events, and the flexibility….one of the key things that stuck out to me is that it wasn’t just a bunch of events with talking heads… There were sections for question and answer and for the experts to share their expertise but there were opportunities for the people to relate to …whether it was a play or poetry...that was really nice to be able to relate on a different level so people could really click into the topic. [Individual interviewee] <N> Consultants were asked what they “learned from their partnership and how it expanded their knowledge.” Consultants said that they learned about vital health information, their own communities’ needs, how to engage people on public health issues, the inner workings of large academic hospitals, the organizational credibility to be gained from associating with a renowned research institution, and new conceptual frameworks through which to view their own work as community advocates. When asked what “tangible benefits the partnership and educational seminars had brought to their community,” most consultants cited knowledge and increased awareness of health and social issues. For the consultants, their affiliation with the university through the partnership made knowledge more accessible, conferred “credibility” on their organization, “improved reputation and legitimacy and sophistication around health issues,” and increased their organization’s capacity to meaningfully increase health awareness for their constituents. Community Consultants came to “trust” the university partners and the information conveyed by university speakers at CGR, but this did not translate to the overall medical center. This was highlighted by the following statement: “There is a tremendous amount of trust” between the academic partners and my organization, “but the jury is still out about the U of C overall.” Six of nine community consultants expressed a similar sense of trust in academic partners involved with CGR, while either reserving judgment about or expressing persistent distrust of the overall medical center; two partners expressed increased trust in the university overall. This theme of trust in academic partners but wariness of the overall institution arose in the focus group as well. When asked, “what comes to mind now [after having worked in the CGR partnership] when you think about” the medical center, one partner articulated this theme: <quote> I would separate the people I work with from the institution… I feel good about the doctors we’ve worked with and their intentions and the work they’ve done and efforts they’ve put forth. I do feel strongly that… what do they call it, “community-based participatory research,” I think you can hold up their work as a “grade A best practice.” I would not translate that to the institution. <N>Knowing that the overall medical center to some extent influenced funding, this wariness of the overall medical center affected their expectation of the sustainability and meaning of the partnership. <A>Barriers <N>Community consultants were asked what they thought were barriers to the CGR partnership in its first year. Multiple consultants felt that the community events were not publicized far enough in advance to entice as many audience members as the project intended. Consultants cited the following as barriers to success: The distance between their own community and the community in which the event was held, transportation, the constraint of hosting events in the few after work hours when people were tired and hungry (food was provided at all events at the recommendation of Community Consultants), and the limitation of one event per geographical area inhibited lasting change and deeper levels of education and dialogue between community and university. Some community members thought that a single educational seminar event was enough to introduce community members to health information and health resources, but not enough to effect meaningful change. <A>Accomplishments <N>Consultants felt that health topics discussed at the community seminars were well-chosen and clearly explained by researchers and that “real-time” partner feedback was listened to and used to modify the community programming. Consultants also cited the following as major accomplishments of the seminars: Outreach to distant South Side communities not typically in contact with the university, good attendance at events, bonding of community leaders from geographically distant areas around common problems, facilitation of better communication between the university and its surrounding communities, creative approaches to presentations based on community recommendations, and communicating an expanded definition of “health” including mental health and social determinants such as poverty, unemployment, and violence to the community. <A>Summary and Limitations <N>CGR serves as a venue for translating evidence-based approaches on health improvement into a community friendly format. CGR is in keeping with Strategic Goal #4 of the Clinical and Translational Science Awards as stated by the Clinical and Translational Science Awards Consortium: To Improve the Health of Communities and the Nation.40 In addition to providing important information about health improvement, through a facilitated discussion, university investigators learn about community health needs and priorities. Many academic–community partnerships are based on interventions for a targeted condition, with interventions planned only by the academic partner.41,42 Creating an environment where university investigators and community members can share information about health needs and priorities helps to build trust between community members and university investigators. By building trust through addressing health education needs based on community priorities, future investigators may find it easier to engage community in translational research activities. While evaluating the program, Community Consultants expressed an interest in measuring whether or not providing health education in the CGR format has a real and lasting impact on reducing health disparities in their community. Although consultants expressed an increased level of trust in the university faculty and staff responsible for planning CGR, there remained a level of wariness as to whether the educational seminar series represented a true and sustainable community–university partnership. A limitation to this evaluation was that some survey questions proved to be ambiguous to the community consultants. Another limitation of our evaluation is a lack of in-depth interview data on the consultant’s perceptions of the medical center and partnership before the initiation of CGR, which would have allowed us to make more reliable assertions about changes in specific perceptions over time. Instead, we asked partners to “look back” and retrospectively recall how they perceived the medical center before beginning the partnership. It is possible that the presence of an academic partner at the individual and focus group interviews inhibited partners from being completely candid or otherwise limited the validity of our evaluation. However, given the partners' explicit expressions of doubts and critiques of both the Grand Rounds and the academic partnership, we feel that it is unlikely that this concealed the true perceptions of our community partners. Further efforts need to be made to increase the level of involvement of university faculty members in CGR as well as their level of engagement with the community. Community Consultants have expressed pleasure in seeing university faculty members attending CGR events, but would like to see more. Also, most faculty members who have attended have been community-engaged researchers. Although the consultants viewed their attendance as an attribute, they expressed a desire to have a more diverse set of university faculty attendees. Although originally grant funded, CGR has demonstrated its value to University of Chicago’s executive leadership and is now internally funded. The future of CGR depends on its partnership expansion, presentation of topics of interest to the community, and proven value to the university as well as our community partners. Plans are underway to integrate medical students into the planning process as well as the development of a Youth Council to work on CGR planning and adolescent audience outreach and development. <A>Acknowledgments <N>The authors acknowledge Marshall H. Chin, MD, MPH, and Arshiya A. Baig, MD, MPH, both of the Department of Medicine at the University of Chicago, for their contributions to this manuscript. References 1. Minkler M, Wallerstein N. Improving health through community organization and community building. In Glanz K, Lewis BM, Rimer BK, editors. Health behavior and health education. 2nd ed. San Francisco: Jossey-Bass Publishers; 1997. pp. 241-69. 2. Buchanan DR. Building academic-community linkages for health promotion: A case study in Massachusetts. Am J Health Promot. 1996;10(4):262-9 3. Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annu Rev Public Health. 2000;21(1):369-402. 4. Jones L, Wells K. Strategies for academic and clinician engagement in community- participatory partnered research. JAMA. 2007;297(4):407-10. 5. Wolff M, Maurana CA. Building effective community-academic partnerships to improve health: a qualitative study of perspectives from communities. Acad Med. 2001;76(2):166-72. 6. Plowfield L, Wheeler E, Raymond J. Time, tact, talent, and trust: Essential ingredients of effective academic-community partnerships. Nurs Educ Perspect. 2005;26(4):217-20. 7. Bureau of the Census. 2010 census data. Washington (DC): Author; 2011. 8. Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999;14:537–46. 9. Wasserman J, Flannery MA, Clair JM. Raising the ivory tower: The production of knowledge and distrust of medicine among African Americans. J Med Ethics. 2007;33(3):177-80. 10. Randall V. Dying while black. Dayton (OH): Seven Principles Press; 2006. 11. Randall V. Slavery, segregation and racism: Trusting the health care system ain't always easy! An African American perspective on bioethics. St. Louis University Public Law Review. 1996;15:191-235. 12. Moseley KL, Freed GL, Bullard CM, Goold SD. Measuring African-American parents' cultural mistrust while in a healthcare setting: A pilot study. J Natl Med Assoc. 2007;99(1):15– 21. 13. Hammond W, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling AfricanAmerican men. J Gen Intern Med. 2010;25(12):1300-8. 14. Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(2):358–65. 15. Hammond W. Psychosocial correlates of medical mistrust among African American men. Am J Community Psychol. 2010;45(1-2):87–106. 16. Freimuth VS, Quinn SC, Thomas SB, Cole G, Zook E, Duncan T. African Americans’ views on research and the Tuskegee syphilis study. Soc Sci Med. 2001;52(5):797-808. 17. Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87(11):1773-8. 18. Corbie-Smith G. The continuing legacy of the Tuskegee syphilis study: Considerations for clinical investigation. Am J Med Sci. 1999;317(1):5-8. 19. Byrd WM, Clayton L. An American health dilemma: The medical history of African Americans and the problem of race, Vol. 1. New York: Routledge; 2000. 20. Byrd WM, Clayton L. An American health dilemma: Race, medicine, and health care in the united states, 1900-2000. New York: Routledge; 2001. 21. Whitney DD, Trosten-Bloom A. The power of appreciative inquiry: A practical guide to positive change. San Francisco: Berrett-Koehler; 2010. 22. Leung MW, Yen IH, Minkler M. Community based participatory research: A promising approach for increasing epidemiology's relevance in the 21st century. Int J Epidemiol. 2004;33(3):499-506. 23. Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312-23. 24. Israel BA, Eng E, Schulz AJ, Parker EA. Methods in community-based participatory research for health. San Francisco: Jossey-Bass; 2005. 25. Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: The intersection of science and practice to improve health equity. Am J Public Health. 2010;100 Suppl 1:S40-S46. 26. Shoultz J, Oneha MF, Magnussen L, Hla MM, Brees-Saunders Z, Dela Cruz M, Douglas M. Finding solutions to challenges faced in community-based participatory research between academic and community organizations. J Interprof Care. 2006;20(2):133-44. 27. Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173-202. 28. Lantz P, Viruell-Fuentes E, Israel B, Softley D, Guzman R. Can communities and academics work together on public health research? Evaluation results from a community-based research partnership in Detroit. J Urban Health. 2001;78(3):495–507. 29. Christopher S, Watts V, McCormick AKHG, Young S. Building and maintaining trust in a community-based participatory research partnership. Am J Public Health. 2008;98(8):1398-406. 30. Flicker S. Who benefits from community-based participatory research? A case study of the positive youth project. Health Educ Behav. 2008;35(1):70-86. 31. Israel BA, Lichtenstein R, Lantz P, McGranaghan R, Allen A, Guzman J, et al. The Detroit community-academic urban research center: Development, implementation, and evaluation. J Public Health Manag Pract. 2001;7(5):1-19. 32. Lantz P, Viruell-Fuentes E, Israel BA, Softley D, Guzman R. Can communities and academics work together on public health research? Evaluation results from a community-based research partnership in Detroit. J Urban Health. 2001;78(3):495–507. 33. Johnson D, Johnson F. Joining together: Group theory and group skills. Boston: Allyn & Bacon; 2003. 34. Gubrium JF, Holstein JA. Handbook of interview research: Context and methods. Thousand Oaks (CA): Sage; 2002. 35. Israel BA, Eng E, Schulz AJ, Parker EA. Methods in community-based participatory research for health. San Francisco: Jossey-Bass; 2005. 36. Auerbach CF, Silverstein LB. Qualitative data: an introduction to coding and analysis. New York: New York University Press; 2003. 37. Shulz AJ, Israel BA, Lantz P. Instrument for evaluating dimensions of group dynamics within community-based participatory research partnerships. Eval Program Plann. 2003;26:249– 62. 38. Lantz P, Viruell-Fuentes E, Israel BA, Softley D, Guzman R. Can communities and academics work together on public health research? Evaluation results from a community-based research partnership in Detroit. J Urban Health. 2001;78(3):495–507. 39. Israel BA, Eng E, Schulz AJ, Parker EA. Methods in community-based participatory research for health. San Francisco: Jossey-Bass; 2005. 40. Clinical and Translational Science Awards Consortium. (n.d.). About the CTSA Consortium [cited 2013 Jun 13]. Available from: https://ctsacentral.org/about-us/ctsa. 41. Abdulrahim S, El Shareef M, Alameddine M, Afifi RA, Hammad S. The potentials and challenges of an academic–community partnership in a low-trust urban context. J Urban Health. 2010;87(6):1017-20. 42. Ross LF, Loup A, Nelson RM, Botkin JR, Kost R, Smith GR, et al. The challenges of collaboration for academic and community partners in a research partnership: Points to consider. Journal of Empirical Research on Human Research Ethics. 2010;5(1):19-31. <table number>Table 1. <table title>Community Grand Rounds Collaborators <table> Name Description Claretian Associates LISC/NCP community organization that serves South Chicago, a community on Chicago’s South Side Greater Auburn Gresham Development LISC/NCP community organization that serves Corporation Auburn Gresham, a community on Chicago’s South Side LISC/NCP National Organization that helps nonprofit community development organization build healthy and sustainable communities Network of Woodlawn LISC/NCP community organization that serves Woodlawn, a community on Chicago’s South Side Quad Communities Development Corporation LISC/NCP community organization that serves Douglas, Grand Boulevard, and Kenwood, communities on Chicago’s South Side Teamwork Englewood LISC/NCP community organization that serves Englewood and West Englewood, communities on Chicago’s South Side Washington Park Consortium LISC/NCP community organization that serves Washington Park, a community on Chicago’s South Side Near North Service Corporation Nonprofit, federally qualified health center that provided community-based primary care in Chicago Northwestern University Academic partner University of Chicago Academic partner <table note>LISC, Local Initiative Support Corporation; NCP, New Communities Program. <table number>Table 2. <table title>List of Community Grand Rounds Title It Shoulda Been Me Topic Posttraumatic stress disorder and adolescent depression Becoming a Piece of the Peace Conflict resolution, anger management, and gender issues Wish You Were Here The effects of domestic and interpersonal violence on the community and family unit Live Life Before You Give Sexually transmitted Life disease/infection prevention and teen pregnancy Eating, Praying, and Loving Obesity and diabetes Part 2: Keys to Your Good prevention Health Timeless Treasures Within the Symptoms, diagnosis, and Seasoned Circle treatment for asthma, sarcoidosis, bronchitis, and other respiratory illnesses Chicago Community Auburn Gresham Washington Park South Chicago Englewood Grand Boulevard Englewood <A>Appendix A: Focus Group Interview Protocol for Community Partners, 2011 <N>Doriane Miller, MD, Kimberly King, MPH, and Kevin Heaton, BA Introduction: Hello, my name is __________________ I’m going to be leading our focus group discussion today. This is ______________, who will be taking notes and helping me during our discussion. We will be here for about 90 minutes to 2 hours to talk about your experience as a community consultant/partner with the University of Chicago Medical Center and your experience with the development of the Community Grand Rounds seminar series. Your candid insights and opinions on the first year of the community-academic partnership and on the Community Grand Rounds program are extremely valuable, and will allow us to improve the partnership and Community Grand Rounds for next year, so please say what’s on your mind and what you think. Your answers will be de-identified and made anonymous to protect you and to allow you to speak freely. There is no right or wrong answer. <numbers>1. Please think back to over a year ago (or before you had formed a relationship with the University of Chicago). At that time, what came to mind when you thought of the University of Chicago Medical Center? [Probe: what did you associate with the University and Medical Center?] 2. What comes to mind now when you think of University of Chicago Medical Center? [Probe: Has (or how has) working with the center for Community Health and Vitality on Community Grand Rounds altered your perception of the medical center and the university? What do you associate now with the university and medical center?] 3. What has it been like to work with the University of Chicago Medical Center? [Probe: Was it a positive experience? Has it been good for your community? Has it been good for you personally? ] 4. Community Grand Rounds was designed to enable “two-way communication” between the University and communities. Do you think your community was able to communicate to the University through Community Grand Rounds? Do you think The University successfully communicated to your community through Community Grand Rounds? [Probe: can you think of any instances examples of exchanges of information, assistance, or support between your organization and the UCMC?] 5. What did you like about the partnership itself? Did you like the way it was run? What were good qualities of the partnership [probe: was there good, clear communication, was it respectful, did it feel collaborative, did you feel valued, was there trust, was power shared, was there equal participation from all partners]? Would you change anything? 6. What did you dislike about the partnership? Were there characteristics that were not good for you? 7. What did you expect Community Grand Rounds to accomplish in your community? 7a. Was it effective in accomplishing these goals? [Probe: if yes, what do you think made it successful? If not, what prevented CGRs from being successful?] 8. Knowing that your feedback will be a critical component of how the Community Grand Rounds program is re-formatted (and hopefully improved) for next year, what else would you like to share about the program that you think we should definitely know to be able to improve the program? <A>Appendix B: In-depth Semistructured Interview Protocol for Community Partners, 2011— Interview Questions <N>Doriane Miller, MD, Kimberly King, MPH, and Kevin Heaton, BA <B>Partner Perceptions <outline>(1) The roles partners perceive themselves to play in their own community. 1. Please describe your role in the community? (Probe: How long have you lived in your community? How long have you been in this role?) (2) The perception of partners of the health of the people in their community (“Assets and Needs”). 2. What are some of the best things about your community? Strengths? Positives? (Examples: Resources, people, social gatherings, agencies, support, physical places.) 3. What are some of the major problems or needs in your community? 4. What are some of the major health needs faced by your community? (3) Partners’ perceptions of UCMC before and after the first year of the partnership? 5. If you think back to before you began working as a partner with the University of Chicago on the Community Grand Rounds program, do you remember what your opinion was of the University and Medical Center? [Probes: What role did you actually see UCMC playing in your community or know of UCMC playing in your community? Did you think of UCMC as a friend, an obstacle, or as uninvolved in your community, or in some other way? Why did you want to work as a consultant for the UCMC?] 6. Has working with UCMC faculty and staff in this partnership altered your perception of the UCMC? [Probes: Was there any specific perception that changed? Were there specific incidents or characteristics of the partnership or a faculty or staff person that positively or negatively affected your perception of UCMC?] (4) Partners’ opinions of the effectiveness of the Community Grand Rounds seminars. (5) Partners’ expectations of the partnership and of partnership-borne programs like Community Grand Rounds. 7. The Community Grand Rounds program just finished its first year. When you first met with University of Chicago Medical Center (UCMC) staff last year in the initial meetings as a consultant (or partner), what did you hope (or expect) that the partnership and the Community Grand Rounds program would accomplish? [Probe: Would you say you had low or high expectations?] 8. Has the community-academic partnership between the UCMC and your community met your expectations for the first year? Has it exceeded these expectations? [Probes: If it has fallen short of your expectations, why do you think this happened? If exceeded expectations, why do you think this happened?] (6) Partners’ experience working with UCMC. 9. What has it been like to work with the UCMC? 9a. How does it compare with working with other organizations you have worked with? <B>Group Dynamics (7) Conflict resolution; (8) sense of shared goals; (9) shared leadership; (10) two-way communication; (11) trust, (12) sense of community and belonging; (13) co-learning; capacity building; (14) equitable participation; (15) power sharing; and (16) balance between knowledge generation and action. 10. Do you feel that there was two-way communication in the partnership? (Probes: Did you feel that you had the opportunity to voice your concerns and to share your expertise with university staff? Do you feel that your opinion was listened to and considered by other partners? Do you feel that university staff communicated effectively to you in partnership meetings? Do you feel that university staff were able to effectively communicate to your community at Community Grand Rounds seminars?) 11. Did you feel that the partnership was transparent? (Probes: Did you feel that important information was made available to you? Did you feel that you were given all the necessary information to participate in the decision making process?) 12. Could you please give me some examples of exchanges of information, assistance, or support between your organization and the UCMC? (What about between your organization and other organizations in the New Communities Program? [Probe: Specifically ask for examples that do not involve university staff or the university]). Do you think that this sharing or information, assistance, or support would have happened with the formation of the community-academic partnership between UCMC and New Communities Program? 13. What have you personally learned from your association with the UCMC? Has it expanded your knowledge at all, or helped to develop or refine any skills? Has it helped you professionally in any way? 14. How much trust do you feel there is between partners? [Probes: Do you trust that the UCMC (or other community partners) share(s) the goals of your community and has your community’s interests in mind? Do you trust UCMC and other community partners?]. 15. Over the past year, would you say that the amount of trust between partners has increased, decreased, stayed the same, or other? 16. Did you feel that you could talk openly and honestly at partnership meetings and conference calls? (17) The value and effectiveness of Community Grand Rounds for each consultant’s community. 17. Has the community grand rounds program provided any tangible benefit to your community thus far? 18. Has your affiliation with the UCMC provided any tangible benefit to your community thus far? 19. What does your organization hope to accomplish by its affiliation with the UCMC? (18) Perceived successes of the partnership/seminars, and suggested improvements to partnership/seminars. 20. What do you think were the major accomplishments of the Community Grand Rounds program in its first year? Please name two or more. 21. What do you think were the major barriers facing the Community Grand Rounds program in its first year? Please name two or more. 22. Do you have any recommendations for how to improve Community Grand Rounds for next year? (Probe: How can the partnership modify Community Grand Rounds for next year to overcome the barriers or shortcomings of the program’s first year?)