biological therapies for obsessive compulsive disorder
advertisement

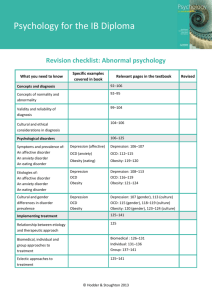
BIOLOGICAL THERAPIES FOR OBSESSIVE COMPULSIVE DISORDER To read up on biological therapies for obsessive compulsive disorder, refer to pages 536–539 of Eysenck’s A2 Level Psychology. Ask yourself If a biochemical imbalance is the cause of obsessive compulsive disorder (OCD) what would be the treatment? What are the main strengths of drug therapy? What are the main weaknesses of drug therapy? What you need to know DRUG THERAPY The effects of drug therapy on obsessive compulsive disorder Evaluation of drug therapy Drug therapy The serotonin reuptake inhibitors (SRIs) were initially the most effective drug therapy for OCD, in particular clomipramine, which has greater effects on the neurotransmitter serotonin than do the other SRIs. The selective serotonin reuptake inhibitors (SSRIs), including fluvoxamine, fluoxetine (Prozac), sertraline, and paroxetine, have also been found to be effective. It is now know that patients with OCD do not, as previously thought, have low serotonin levels (Rachman, 2004, see A2 Level Psychology page 536). It is possible that various brain structures in obsessive compulsives show increased sensitivity to serotonin. However, we do not really know why SRIs and the SSRIs are both effective in treating OCD. EVALUATION OF DRUG THERAPY Effectiveness Drugs work but not immediately. Dougherty et al. (2002, see A2 Level Psychology page 537) found that SSRIs, rather than improving symptoms, sometimes make them worse early in treatment but are effective after about 6 weeks. This can be explained by the fact that initially the SSRIs increase serotonin, but by 6 weeks they actually cause serotonin to decrease. This links OCD to high levels of serotonin, because the drugs work when they are reducing serotonin. SRIs and SSRIs are most effective. Eddy et al. (2004, see A2 Level Psychology page 537) found the SSRIs and SRIs were more effective than tricyclics and anti-anxiety drugs. The most effective drug of all was the SRI, clomipramine. A combination of drugs. A combined approach may be optimal because the use of atypical anti-psychotics in those who hadn’t responded to SRIs was found to be more effective than SRIs on their own. This links to the fact that some OCD patients may have too high a level of dopamine, as the antipsychotics reduce this. There is increasing evidence that dopaminergic and serotonergic pathways are both involved in the development and maintenance of obsessive compulsive disorder, and the dopamine and serotonin systems interact with each other in complex ways. Drop-out rate. The unpleasant side effects (dry mouth, drowsiness, sedation, and sweating) of clomipramine mean that compliance is an issue because patients are reluctant to take the drugs. This leads to a higher dropout rate than with patients taking the SSRIs. Treats symptoms not causes. Drug therapy treats symptoms, not the underlying causes, and so does not cure OCD. Relapse rates. The relapse rates show the effects of drug therapy are not long-lasting. For example, Simpson et al. (2004, see A2 Level Psychology pages 537–538) found during the 12 weeks following the end of treatment, 45% of the patients treated with clomipramine relapsed back into the disorder compared to only 12% of those who had received the behavioural treatment exposure and response prevention. Placebo effect. The placebo effect occurs when patients given an inactive substance or placebo (e.g. a salt tablet) show significant reductions in their symptoms. It is difficult to know how much any improvement is due to the drug and how much to the placebo effect, i.e. the patient improves because they expect the drug to work. A multi-dimensional approach to treatment. Drug therapy is most commonly used on its own; combining drug therapy with psychological forms of therapy may be more effective. Appropriateness Effectiveness. The effectiveness of drug therapy means that it is appropriate: for many patients it is effective in reducing anxiety levels and many of the symptoms of OCD. Valid basis for therapy. Drug therapy is appropriate in view of the increasing evidence that OCD is associated with complex abnormalities of serotonin and dopamine function. Individual differences. Clomipramine is not appropriate for all patients because it can pose dangers when it is taken by patients who have heart problems or who are at risk of attempting suicide. Slow acting. Drug treatment is slow acting because it can take approximately 6 weeks to work and, at least initially, can make the symptoms worse. Side effects. All the drugs used in the treatment of OCD possess unwanted side effects. For example, the SSRIs can cause insomnia, reduced sex drive, and nausea; SRIs can cause dry mouth, drowsiness, sedation, and sweating, which question the appropriateness of the treatment. Drop-out rate. The fact the drop-out rate is higher than for psychological therapies questions appropriateness. Lack understanding of their effect. We do not fully understand why serotonin reuptake inhibitors and selective serotonin reuptake inhibitors are successful in reducing obsessional and compulsive symptoms. So what does this mean? Drug therapy has the advantage of being reasonably effective in the treatment of OCD, at least in the short term. However, the length of any improvement is a key issue; research suggests the improvement lasts only as long as patients stay on the drugs, and being on drugs is not an optimal solution! Furthermore, all biological treatments raise issues of appropriateness such as side effects, and the fact that they treat the symptoms not the causes, which leads to a high relapse rate. This last criticism is a key weakness as this makes biological treatments palliative because they manage the disorder rather than cure it. Hence we need to consider whether psychological treatments offer more hope of a cure. Nevertheless, some patients may need drug therapy to calm them down to a state in which they can benefit from psychological therapy. So a multi-dimensional approach to treatment may be optimal as research suggests that the drug therapy helps patients to cope with the anxiety of the behavioural therapy exposure and response prevention and consequently patients are less likely to drop out. The psychological therapy has a much lower relapse rate than drugs so the combination of the two is more effective than either therapy on its own. Over to you (a) Outline one or more biological therapy(ies) for one anxiety disorder. (9 marks) (b) Evaluate the therapy(ies) described in (a). (16 marks)