File - Respiratory Therapy Files
advertisement
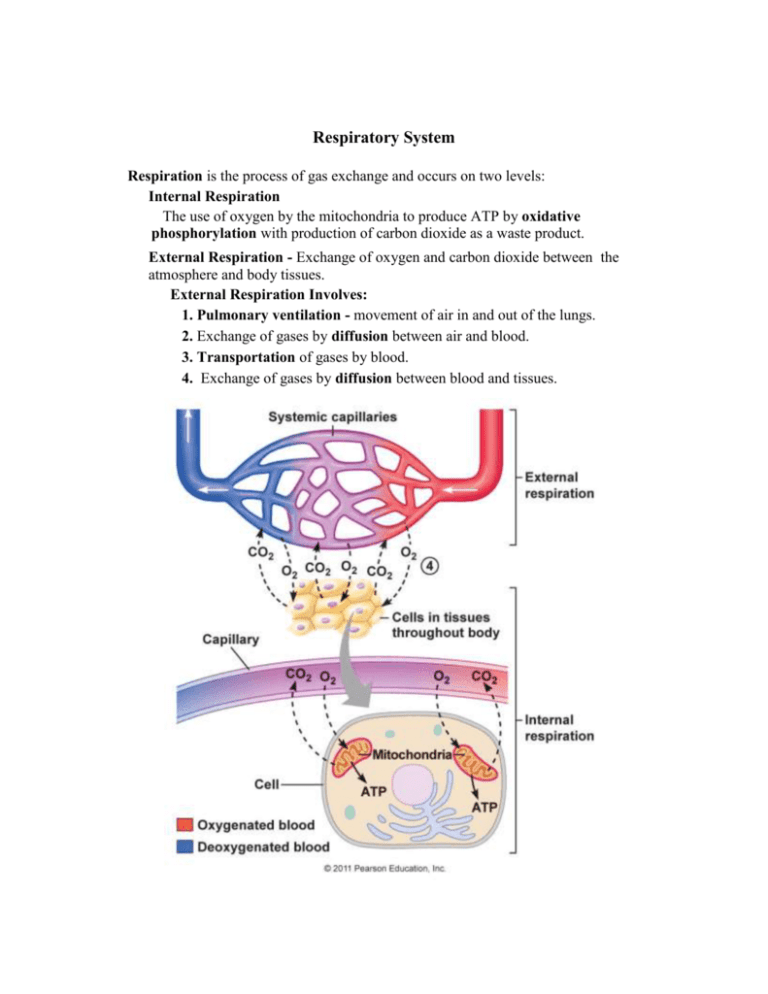
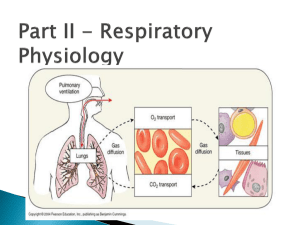
Respiratory System Respiration is the process of gas exchange and occurs on two levels: Internal Respiration The use of oxygen by the mitochondria to produce ATP by oxidative phosphorylation with production of carbon dioxide as a waste product. External Respiration - Exchange of oxygen and carbon dioxide between the atmosphere and body tissues. External Respiration Involves: 1. Pulmonary ventilation - movement of air in and out of the lungs. 2. Exchange of gases by diffusion between air and blood. 3. Transportation of gases by blood. 4. Exchange of gases by diffusion between blood and tissues. Forces for Pulmonary Ventilation Ventilation results from bulk flow of air as the result of pressure gradients created between alveoli and atmospheric pressure. Pulmonary Pressures There are four primary pressures associated with ventilation: Atmospheric Pressure The pressure of the outside air at sea level is 760 mm Hg. The remaining lung pressures are expressed relative to this pressure. Intra-Alveolar Pressure Varies with ventilation. During inspiration it is less than atmospheric pressure. During expiration it is greater than atmospheric pressure. At rest it is equal to atmospheric pressure. When it is equal to atmospheric pressure it is considered to be at 0 mm Hg. Intrapleural Pressure At rest it is - 4 mm Hg. It varies during ventilation but it is always less than intraalveolar pressure and is always negative (that is, less than atmospheric pressure) during normal breathing. This negative pressure results from the elastic forces exerted on the intrapleural space by the chest wall and the lungs. Both the chest wall and lungs are elastic. The chest wall is compressed and the elastic forces are pulling it outward. The lung walls are stretched and the elastic forces are pulling them inward. Hence, the elastic forces are trying to open the intrapleural space. The tension resisting these elastic forces is the surface tension of the pleural fluid. To maintain this negative intrapleural pressure the pleurae need to be airtight. If the integrity of the airtight space is compromised by trauma (gunshot or knife wound) or disease (pneumonia or emphysema) air enters this space and the condition is called pneumothorax. In pneumothorax, the lung collapses and the thoracic wall expands. - Transpulmonary Pressure Transpulmonary pressure is the difference between the intrapleural pressure and the intra-alveolar pressure. This force operates across the walls of the lungs and causes the lungs to expand. Mechanics of Breathing Between breaths, when the lungs are at rest, the volume of air in the lungs is called the functional residual capacity (FRC). No air is moving into or out of the lungs during this time. Air flow results from the muscles of respiration creating pressure gradients by changing the volume of the lungs. The relationship between pressure and volume is expressed by Boyle's law. This law states that the pressure of gas in any container is inversely related to the volume of the container. In other words, when volume increases, pressure decreases and when volume decreases, pressure increases. Air flows into the lungs by bulk flow. The rate of flow is equal to the pressure gradient created by the difference between atmospheric pressure and intra-alveolar pressure over the resistance encountered by air as it flows through the air passageways. Determinants of Intra-alveolar Pressure The changes in intra-alveolar pressure creates the pressure gradient that causes air to flow into and out of the lungs. Two factors determine intra-alveolar pressure: 1. the quantity (moles) of air molecules in the alveoli; 2. the volume of the alveoli. The pressure changes are shown in the figure above. During inspiration, alveolar volume increases and intra-alveolar pressure falls causing air molecules to enter down the pressure gradient created by the inspiration. The air flow stops when pressure is equal to atmospheric pressure (0 mm Hg). During expiration, alveolar volume decreases and intra-alveolar pressure increases causing air molecules to leave down a pressure gradient in the reverse direction until the pressure returns to 0 mm Hg. The movement of air into and out of the alveoli is due to the changes in the volume of the thoracic cavity produced by the muscles of ventilation. The diaphragm and the external intercostal muscles are the primary inspiratory muscles, whereas the internal intercostal and abdominal muscles are the primary expiratory muscles. Inspiration The expansion of the thoracic cavity during respiration causes intrapleural pressure to decrease. This increases the transpulmonary pressure that is due to the difference between the intra-alveolar pressure and the intrapleural pressure (Palv - Pip). This increase in transpulmonary pressure causes the lungs to expand. The increase in the volume of the alveoli that accompanies this expansion decreases intra-alveolar pressure. The pressure gradient between atmospheric pressure and intra-alveolar pressure (Patm - Palv) causes air to flow into the lungs. Air flow continues until intra-alveolar pressure equals atmospheric pressure. Expiration During normal breathing expiration is a passive process in which the muscles of inspiration relax and the elastic properties of the chest wall and lungs cause lung volume to decrease. This decrease in lung volume causes an increase in intra-alveolar pressure and creates the pressure gradient that causes an outflow of air. A more forceful expiration results from contraction of the muscles of expiration in a process called active expiration. Factors Affecting Pulmonary Ventilation Lung Compliance Compliance is a measure of the ease with which the lungs can be stretched. Lung compliance is equal to the change in volume over the transpulmonary pressure or DV D(Palveolar- Pintrapleural) The greater the lung compliance the less the work necessary to bring in a given volume of air. Lung compliance depends on the elasticity of the lungs and the surface tension of the liquid in the alveoli. Both factors tend to decrease the lung compliance. The impact of surface tension on lung compliance is lessened by pulmonary surfactant which is secreted by Type II alveolar cells. Compliance decreases if lung tissue thickens as in tuberculosis, and in the loss of surfactant as occurs in infant respiratory distress syndrome. Airway Resistance This refers to the resistance of the entire system of airways in the respiratory tract. The radius of the airways is the most important factor affecting resistance. During quiet breathing (eupnea) airway resistance in the conducting zone is low and only a pressure gradient of less than 2 mm Hg is required to maintain sufficient air flow. If airway resistance increases a much larger pressure gradient is needed to maintain a given airflow. Resistance to airflow is affected by: 1. Passive forces exerted on the airways. 2. Smooth muscles in bronchioles 3. Secretion of mucous into airways Passive forces are due to changes in the transpulmonary pressure that occurs during inspiration and expiration and tractive forces exerted on the airways by the surrounding tissue. During inspiration both forces act to decrease resistance while during expiration resistance increases. When the smooth muscle of the bronchioles contract (bronchoconstriction) the radius of the bronchioles decreases and the resistance increases. When the smooth muscles relax (bronchodilation) the radius increases and resistance decreases. Contraction and relaxation of smooth muscle is subject to both extrinsic (neural and hormonal signals) and intrinsic (local chemical mediators) control. Sympathetic stimulation causes relaxation of smooth muscle (bronchodilation) while parasympathetic stimulation causes contraction (bronchoconstriction). Epinephrine causes bronchodilation. Histamine which is released during an allergic reaction increases resistance by bronchoconstriction and increasing the secretion of mucus. Carbon dioxide affects the radius of bronchioles by causing bronchodilation when its concentration increases and bronchoconstriction when its concentration decreases. Asthma increases airway resistance by causing spastic contraction of smooth muscles of the bronchioles, increased mucus secretion and inflammation of bronchioles. Chronic obstructive pulmonary diseases (COPD's) also increase airway resistance. COPD's are due to chronic diseases such as emphysema and chronic bronchitis. Clinical Significance of Respiratory Volumes and Air Flows Spirometry is a technique of measuring volumes of inspired and expired air. The spirometer can be used to calculate three of 4 non-overlapping lung volumes: Tidal Volume The volume of air that moves into and out of the lungs in one unforced breath. The average volume is about 500 ml. Inspiratory Reserve Volume The maximum volume of air that can be inspired at the end of a normal inspiration. The average volume is about 3000 ml. Expiratory Reserve Volume The maximum volume of air that can be expired at the end of a normal expiration. The average volume is about 1000 ml. Residual Volume The volume of air remaining after a maximum expiration. The average volume is about 1200 ml. Tidal volume, inspiratory reserve volume, and expiratory reserve volume can be measured directly. Residual volume can be measured indirectly. Lung Capacities Lung capacities are sums of two or more lung volumes. These include: Inspiratory Capacity IC is the maximum volume of air that can be inspired at the end of a resting expiration. It is the sum of tidal volume and inspiratory reserve volume. It is approximately 3500 ml. Vital Capacity VC is the maximum amount of air that can be expired following a maximum inspiration. It the sum of tidal volume, inspiratory reserve volume and expiratory reserve volume. It is about 4500 ml. Functional Residual Capacity FRC is the volume of air remaining in the lungs at the end of a tidal expiration. It is the sum of expiratory reserve volume and residual volume. It is about 2200 ml. Total Lung Capacity TLC is the volume of air in the lungs at the end of a maximum inspiration. It is the sum of all the lung volumes including tidal volume, inspiratory reserve volume, expiratory reserve volume and residual volume. It is about 5700 ml. Pulmonary Function Tests Spirometry is used to test for respiratory disorders. The diseases that can be diagnosed fall into two categories: Obstructive Pulmonary Diseases Obstructive pulmonary diseases involve abnormal increases in airway resistance. In these diseases the lungs become over inflated and the functional residual capacity and lung volume often increase. Restrictive Pulmonary Diseases In these disorders something interferes with lung expansion. With these diseases there is a decrease in vital capacity and total lung capacity. Additional Tests Are: Forced Vital Capacity The patient makes a maximum inspiration and then exhales as forcefully and rapidly as possible. A low FVC is indicative of restrictive pulmonary disease. Forced Expiratory Volume A measure of the percentage of forced vital capacity that can be exhaled within a certain period of time. A FEV that is less than 80% is characteristic of obstructive pulmonary disease. Alveolar Ventilation Minute Ventilation Total air that flows in and out of respiratory system in a minute. It can be calculated by multiplying the tidal volume by the respiration rate or number of breaths per minute. Alveolar Ventilation This is a more important measure from a functional point of view because it is a measure of the volume of fresh air that reaches the alveoli each minute. It is calculated by subtracting from the minute volume the air that does not reach the alveoli because of the anatomical dead space (the combined volume of the nonexchanging airways).