appendix - JACC: Heart Failure
advertisement
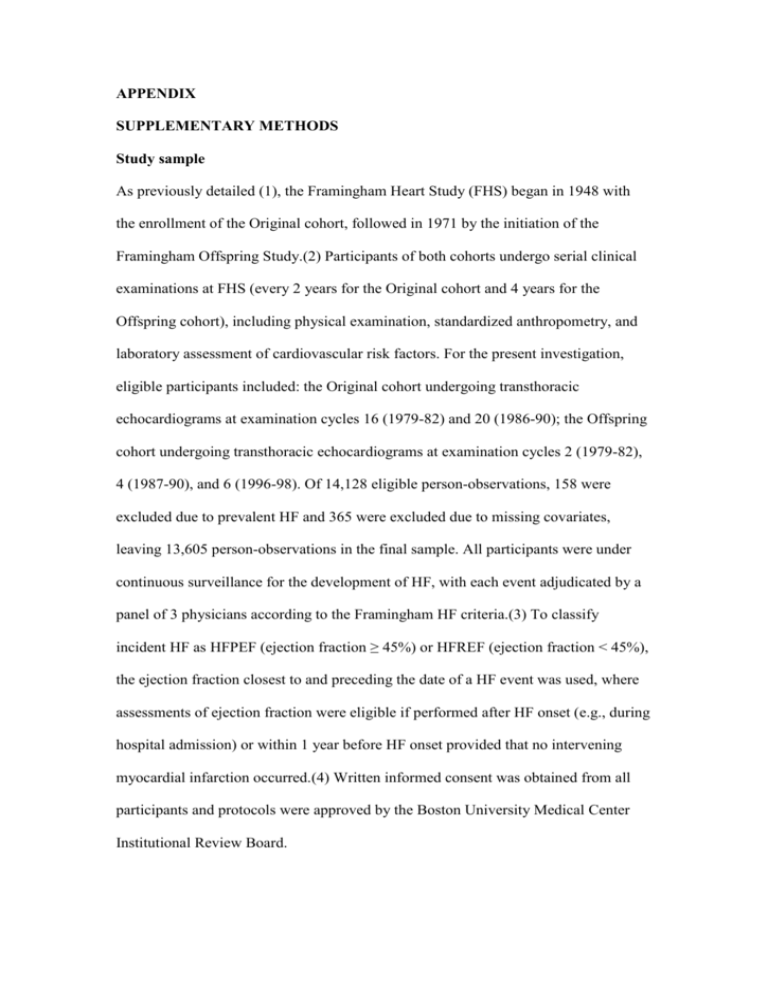
APPENDIX SUPPLEMENTARY METHODS Study sample As previously detailed (1), the Framingham Heart Study (FHS) began in 1948 with the enrollment of the Original cohort, followed in 1971 by the initiation of the Framingham Offspring Study.(2) Participants of both cohorts undergo serial clinical examinations at FHS (every 2 years for the Original cohort and 4 years for the Offspring cohort), including physical examination, standardized anthropometry, and laboratory assessment of cardiovascular risk factors. For the present investigation, eligible participants included: the Original cohort undergoing transthoracic echocardiograms at examination cycles 16 (1979-82) and 20 (1986-90); the Offspring cohort undergoing transthoracic echocardiograms at examination cycles 2 (1979-82), 4 (1987-90), and 6 (1996-98). Of 14,128 eligible person-observations, 158 were excluded due to prevalent HF and 365 were excluded due to missing covariates, leaving 13,605 person-observations in the final sample. All participants were under continuous surveillance for the development of HF, with each event adjudicated by a panel of 3 physicians according to the Framingham HF criteria.(3) To classify incident HF as HFPEF (ejection fraction ≥ 45%) or HFREF (ejection fraction < 45%), the ejection fraction closest to and preceding the date of a HF event was used, where assessments of ejection fraction were eligible if performed after HF onset (e.g., during hospital admission) or within 1 year before HF onset provided that no intervening myocardial infarction occurred.(4) Written informed consent was obtained from all participants and protocols were approved by the Boston University Medical Center Institutional Review Board. Statistical analyses To investigate the association of baseline AoD with incident HF, AoD at baseline examination (Original cohort examinations 16 and 20; Offspring examinations 2,4, and 6) was measured and sex-pooled standardized AoD was used in analyses. To examine the association between change in AoD and incident HF, the change in AoD between any 8-year examination cycles (from Original cohort examinations 16 to 20, Offspring examinations 2 to 4, and Offspring examinations 4 to 6) was calculated. We used pooled repeated observations in multivariable Cox regression analyses to relate baseline AoD, or change in AoD (in separate models), to the 8-year incidence of HF (up to Original cohort examinations 20 and 24; Offspring exams 4, 6, and 8 respectively).(5) Models were adjusted for risk factors for HF (age, sex, body mass index, systolic and diastolic blood pressure, hypertension treatment, diabetes mellitus, smoking, prior myocardial infarction, clinical valvular heart disease), as well as for baseline AoD in models using change in AoD. All models were checked to confirm that the assumption of proportionality of hazards was satisfied, and splines were assessed to confirm a linear association between AoD and HF incidence. We tested for effect modification by sex. In addition, we accounted for repeated observations in the same individual using the sandwich variance estimator.(6) In secondary analyses, we adjusted for arterial stiffness (indexed by the ratio of pulse pressure to stroke volume [PP/SV]), left ventricular (LV) structural characteristics (relative wall thickness, LV mass), and tested for effect modification by the presence versus absence of LV hypertrophy (defined empirically as LV mass ≥ sex-specific median). To evaluate if an association between baseline or change in AoD varied with the type of incident HF (HFPEF versus HFREF), (4) We used data augmentation in competing risks model to relate baseline AoD and change in AoD with 8-year incidence of HFPEF versus HFREF.(7) Data augmentation is an algorithm that uses auxiliary variables or latent variables to construct iterative optimization of complex posterior distributions. In supplementary analyses, we used height instead of body mass index to adjust for the effect of body size on AoD in our multivariable models. Supplementary Table 1. Relationship between Log AoD and incident HF Adjusted for age, sex, Log height, PP, hypertension treatment, diabetes mellitus and prior myocardial Log AOD P HR (95%CI) per 1-SD value 1.20 0.0002 (1.09 – 1.32) infarction Additional adjustment for arterial stiffness (Log PP/SV) Additional adjustment for LV mass 1.15 0.033 (1.01 – 1.30) 1.02 0.76 (0.90 – 1.16) Additional adjustment for relative wall thickness 1.16 0.016 (1.03– 1.32) AoD, aortic root diameter; HR, hazards ratio; PP, pulse pressure; SV, stroke volume REFERENCES 1. Dawber TR, Meadors GF, Moore FE, Jr. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health. 1951 Mar;41(3):279-81. 2. Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979 Sep;110(3):281-90. 3. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971 Dec 23;285(26):1441-6. 4. Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the framingham heart study of the national heart, lung, and blood institute. Circulation. 2009 Jun 23;119(24):3070-7. 5. Cox DR. Regression Models and Life Tables. Journal of the Royal Statistical Society, Series B. 1972;20:187-220. 6. Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. Journal of the American Statistical Association. 1989;84(408):1074-8. 7. Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995 Jun;51(2):524-32.