7_Complement - V14-Study
advertisement

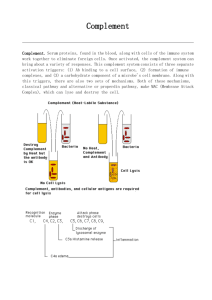
The Complement System Features of the Complement System - Comprises more than 30 circulating and membrane-expressed proteins - Is an important effector arm of both innate and acquired immune responses - Named from early observations of its activity Material of serum that “complemented” the ability of antibody to kill bacteria - Complement components play a major role in defense against infectious organisms Production of opsonins o Molecules that enhance the ability of macrophages and neutrophils to phagocytose material Production of anaphylatoxins o Peptides that induce local and systemic inflammatory responses Direct killing (lysis) of pathogens - Components are synthesized mostly in the liver and cells involved in the inflammatory response Circulatory concentration of all complement proteins is ~3mg/ml Some components are found at higher concentrations than others Complement Activation - The first step of complement activation is recognition of a pathogen - There are 3 different mechanisms by which the complement system recognizes microorganisms Each pathway results in the attachment of complement proteins to microbial surfaces Each pathway begins with an enzyme cascade Classical pathway o This pathway is a major effector pathway of the adaptive immune response Triggered by antibodies bound to antigens on a pathogen Antigen-antibody complexes (immune complexes) are the main pathway activators o Component proteins are designated C1 – C9 (order in which they were discovered) o First step of pathway is the binding of C1 to the Fc region of an antibody C1 is a macromolecular complex consisting of three proteins - C1q, C1r, C1s Each C1 must bind ≥ 2 Fc sites for a stable C1-antibody interaction to occur o Series of interactions between C1q, C1r, and C1s leads to generation of C1 protease C1 protease has two substrates (C4, C2) o C1 protease acts on C4 to yield two fragments C4a (smaller) C4b (larger) that binds covalently to the cell surface of a target o C1 protease also acts on C2 to form two products C2a C2b that remains attached to C4b on the pathogen’s cell surface (C4b2b) o C4b2b complex acts on complement component C3 to become C3 convertase o C3 convertase cleaves C3 to produce two fragments C3a (smaller) C3b (larger) o Some C3b binds to C4b2b to form a trimolecular complex (C4b2b3b) o C4b2b3b complex acts on complement component C5 to become C5 convertase Alternative pathway o This pathway is an effector arm of the innate immune response Activation of the alternative pathway occurs in the absence of specific antibody o Triggered directly by macromolecules on pathogen cell surfaces o Triggered by almost any foreign substance Lipopolysaccharide (LPS) from cell walls of gram-negative bacteria is widely studied o Component proteins can be unique (i.e. serum factors B, D, P) o Component proteins can be common to other pathways (i.e. C3) o Low-level C3 conversion (via slow spontaneous hydrolysis) makes complement activation possible without the participation of classical pathway components o C3 converts into two products C3a C3b o C3b binds to antigens on foreign pathogen surfaces o C3b then combines with serum protein Factor B to form C3bB o Serum protein factor D cleaves C3bB into C3bBb (alternative pathway C3 convertase) C3bBb interacts with Factor P to stabilize and extend the life of C3 convertase o C3 convertase generates C5 convertase (C3bBb3b complex) Lectin pathway o This pathway is an effector arm of the innate immune response Activation occurs in the absence of antibody o Activated by terminal mannose residues on the surface of pathogens Terminal mannose residues are not found on the surfaces of mammalian cells, so this pathway is thought to discriminate between self and non-self o Mannan-binding lectin (MBL) binds to mannose on the surface of pathogens Binding activates two associated proteases - Mannose-associated serine protease (MASP) 1 and 2 o Activated MASP 1 and 2 leads to C2 and C4 cleavage o C2b and C4b form C3 convertase (as in the classical pathway) o C3 convertase cleaves C3 into C3a and C3b - Leads to the formation of the C5 convertase (C4b2b3b) All complement activation pathways converge at the formation of the membrane attack complex (MAC) C5 convertase cleaves C5 to form two product o C5a, C5b C5b binds to microbial cell membranes and bind C6 (C5b6 complex) C5b6 complex combines spontaneously with C7 (C5b67) and inserts into the membrane C8 binds to the complex C5b67 and initiates the binding and polymerization of C9 Incorporation of many C9 molecules causes further membrane penetration that results in the formation of a larger transmembrane channel that disturbs the cell’s osmotic equilibrium Ions pass through the channel and water enters cell causing the cell to swell and lyse Regulation of Complement Activity - Complement activation generates activated fragments (especially cleavage products of C3, C4, C5) that induce potent inflammatory responses that remove infectious agents but can also damage the host - Uncontrolled complement activation can rapidly diminish complement components, leaving the host unable to remove infectious agents - Inappropriate complement activation does not normally occur due to regulatory mechanisms at most steps - Many molecules that regulate complement activation are expressed only on mammalian cell surfaces Not found on microbial cells Consequently, regulators of complement activity limit damage to the individual while allowing activated components to focus on removing microbial pathogens - Important regulators of the classical pathway C1 protease inhibitor (C1INH) inhibits the first step in the activation of the classical pathway o C1INH binds to C1r and C1s, causing them to dissociate from C1q Proteins inhibit C3 convertase assembly via displacement of C2b from the C4b2b complex and cleavage of C4b to inactive forms (C4d, C4c) o C4b-binding protein (C4BP) o Decay accelerating factor (DAF, CD55) o Cofactor protein (MCP, CD46) o Complement receptor 1 (CR1) CD59 prevents final assembly of the MAC at the C8 and C9 stages - Important regulators of the alternative pathway Factor H and Factor I regulate and inhibit C3 convertase assembly Biological Activities of Complement - Opsonization Macrophages and neutrophils express cell-surface receptors (CRI) that binds to C3b o Microorganisms coated with C3b can then be phagocytosed - Induction of local inflammation C3a, C4a and C5a fragments cause inflammation at a site of complement activation via 2 mechanisms o Fragments act as chemoattractants that direct phagocytic cell migration to the activation site o Fragments can cause degranulation of mast cells and basophils to release inflammatory mediators (histamine, other vasoactive substances) that increase capillary permeability If degranulation is too strong, anaphylactic shock occurs Thus, fragments are often referred to as anaphylatoxins - Pathogen lysis The membrane attack pathway causes hole formation in pathogen membranes (leads to pathogen lysis) - Viral neutralization MBL binds to a variety of viruses, leading to opsonization and lysis of the organism MBL can interfere with virus – membrane receptor interaction, preventing viral entry into the host cell - Clearance of immune-complexes Soluble immune complexes coated with C3b become bound to complement receptors (CRI) present on phagocytic cells and especially on circulating RBCs o RBCs carry complexes to the liver and spleen where they are removed by macrophages Complement Deficiencies - The complement system is particularly important in defense against pyogenic (pus-forming) bacteria Neisseria species (responsible for meningitis and some STDs) Staphlococcus aureus Streptococcus pneumoniae Haemophilus influenzae - The major pathways of defense include the production of IgG antibody that binds to bacteria, opsonization, compliment activation, phagocytosis, and intracellular killing If any one of these functions is diminished (i.e. from genetic deficiencies or acquired conditions), the individual becomes susceptible to pathogens - Because the compliment system is vital for removal of immune complexes from circulation, defective or deficient components can result in deposition of these complexes in tissues (results in autoimmune conditions) Deficiencies are rare (1 in 10,000 people) and not always associated with disease Complement Deficiency C1q, C1r, C2, C4 C3 C5 C1 INH Factor I Factor D Factor H Clinical Presentation Systemic Lupus Erythematosus (SLE) Recurrent infection Recurrent infection Hereditary Angioedema (HAE) Recurrent infection Recurrent infection Recurrent infection - Deficiencies in any of the classical pathway components (C1, C4, C2) are associated with the inability to clear immune complexes, resulting in increased susceptibility to autoimmune disease (e.g. SLE) A C3 deficiency is severe (even life-threatening) because C3 is central to all compliment pathways o C3-deficient individuals are susceptible to recurrent pyogenic infections and may also develop inflammatory disorders associated with circulating immune complexes Deficiency of the alternative pathway’s properdin (factors B or D) results in pyogenic infections Deficiency of MBL can be a major problem in early life, manifesting as severe recurrent infections Hereditary angionedema (HAE) Uncontrolled cleavage of C2 and C4 that results from a deficiency of C1INH, the regulatory control protein for classical pathway components C1r and C1s o C1INH inhibitory functions Inhibits complement activation Inhibits activity of enzymes in other serum cascades - Serum pathways that form kinins (e.g. bradykinin), potent vasodilators and inducers of vascular permeability and smooth muscle contraction Symptoms of HAE o Localized edemas in skin and mucosa due to dilatation and increased capillary permeability o Pain in the abdomen o Swelling of the larynx that can compromise breathing How can pathogens avoid being killed by these multiple complement activation pathways? Schistosomes – Extracellular parasitic blood worms that infect several wildlife species, livestock and people