Thyroid Disease
advertisement

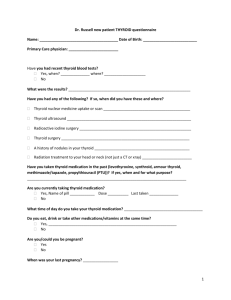
Thyroid Disease FY1 Sejal Nirban Thyroid Gland Predominantly secretes T4 and small amounts of T3 Most T3 is produced by peripheral conversion of T4 Iodine is an essential requirement for thyroid hormone synthesis 99% of T4 and T3 circulate bound to plasma proteins (Thyroid Binding Globulin) Free hormones are available to control the metabolic rate of many tissues Thyroid function is measured using Serum TSH and free T4 and T3 Hyperthyroidism Affects 1/50 females and 1/250 males Due to an excess of T3 and T4 causing thyrotoxicosis An acute exacerbation of symptoms is called a thyrotoxic crisis- usually brought on by infection Diagnosis is made by measuring TSH, free T3 and free T4 Raised TSH suggests the fault is in the pituitary or hypothalamus whereas low TSH is due to a thyroid problem Symptoms Weight loss Increased appetite Heat intolerance Palpitations Fatigue Sweating Diarrhoea Oligomenorrhoea Psychiatric symptoms Irritability Emotional lability Psychosis Signs General Hair thinning Goitre Lid lag, lid retraction Pre-tibial myxoedema Eye signs Palmar erythema CVS Tachycardia AF Neuro Fine tremor Causes: 1. Graves Disease- most common cause. IgG antibodies bind to TSH receptor stimulating thyroid hormone production 2. Toxic Multinodular Goitre 3. Solitary adenoma 4. De Quervains Thyroiditis- acute inflammation of thyroid gland (fever, malaise and neck pain) 5. Postpartum thyroiditis Management: 1. Anti-thyroid drugs: Carbimazole (UK) Methimazole (USA)- both block thyroid hormone biosynthesis and also have immunosuppressive affects. Clinical benefit is not seen for 10-20 days. Carbimazole can cause agranulocytisis- seek urgent blood count if patient develops unexplained fever or sore throat 2. Beta blockers: Propanolol used for symptomatic control 3. Radioactive Iodine: contraindicated in pregnancy and breast feeding. Accumulates in the gland and results in local irridation 4. Surgery: thyroidectomy can only be performed in euthyroid patients. Complications of surgery include bleeding, hypocalcaemia and hypothyroidism. Thyroid Storm Life threatening condition- severe thyrotoxicosis Precipitated by infection, stress and surgery Treated with large doses of carbimazole, propranolol, potassium iodide and hydrocortisone Graves’ Disease Goitre Eye signs- oedema, proptosis, lid retraction, lid lag, and opthalmoplegia- worse in smokers. Thyrotoxicosis Cause: T lymphocytes react with antigens shared by the orbit and thyroid leads to retro orbital inflammation. Swelling and oedema of extra-ocular muscles leading to limitation of movement and proptosis. Increased pressure on the optic nerve may cause optic atrophy. Treatment is low dose of carbimazole, surgery or radioiodine and stop smoking advice Hypothyroidism Affects 1/100 females and 1/500 males. Incidence increases with age. T3 and T4 levels are low with a raised TSH If TSH is low then there is likely to be a hypothalamic or pituitary lesion Symptoms Weight gain Fatigue, lethargy Cold intolerance Constipation Menorrhagia Hoarse voice Myalgia Carpal tunnel syndrome Psychiatric symptoms Depression Dementia Signs General Dry skin and hair Goitre Non-pitting oedema Facial features – purple lips, malar flush, periorbital oedema, lateral eyebrow loss CVS Bradycardia Neuro Cerebellar ataxia Slow relaxing reflexes Peripheral neuropathy Causes 1. 2. 3. 4. 5. Iodine deficiency Autoimmune thyroiditis- Hashimoto’s thyroiditis Iatrogenic- thyroidectomy, radioactive iodine Drug induced- carbimazole, lithium, Amiodarone Congenital hypothyroidism- thyroid aplasia Management: Lifelong Levothyroxine. Aim to normalise TSH Myxoedema coma Severe hypothyroidism with swelling of subcutaneous tissues- typically around eyes and back of hands ‘’bunch of banana hands’’ Unresponsive, decreased respiratory rate, low bp, low glucose, low temperature Pregnancy and Thyroid Increased concentration of TBG Total T4 and T3 increase Free T4 and T3 remain within normal range TSH does not change Two pregnancy-related hormones—human chorionic gonadotropin (hCG) and estrogen—cause increased thyroid hormone levels in the blood. Made by the placenta, hCG is similar to TSH and mildly stimulates the thyroid to produce more thyroid hormone. Increased estrogen produces higher levels of thyroid-binding globulin. Transient autoimmune thyroiditis can occur postpartum resulting in hypo or hyperthyroidism Hyperthyroid management: Propylthiouracil. Carbimazole is associated with congenital defects including aplasia cutis of the neonate. Hypothyroid management: Levothyroxine is safe to give in pregnancy Thyroid Malignancy Most present as asymptomatic thyroid nodules Types: 1. 2. 3. 4. 5. Papillary- 70%. Good prognosis Follicular- 20%. Good prognosis Anaplastic <5%. Aggressive, poor prognosis Lymphoma 2%. Poor prognosis Medullary 5%. Often familial. Poor prognosis Investigation: FNAC distinguishes between benign and malignant nodules Treatment: Radioactive iodine, thyroidectomy with wide local lymph node excision. External radiotherapy and palliative care for anaplastic and lymphomas.