Hypersensitivity I Usually, an immune response induces a
advertisement
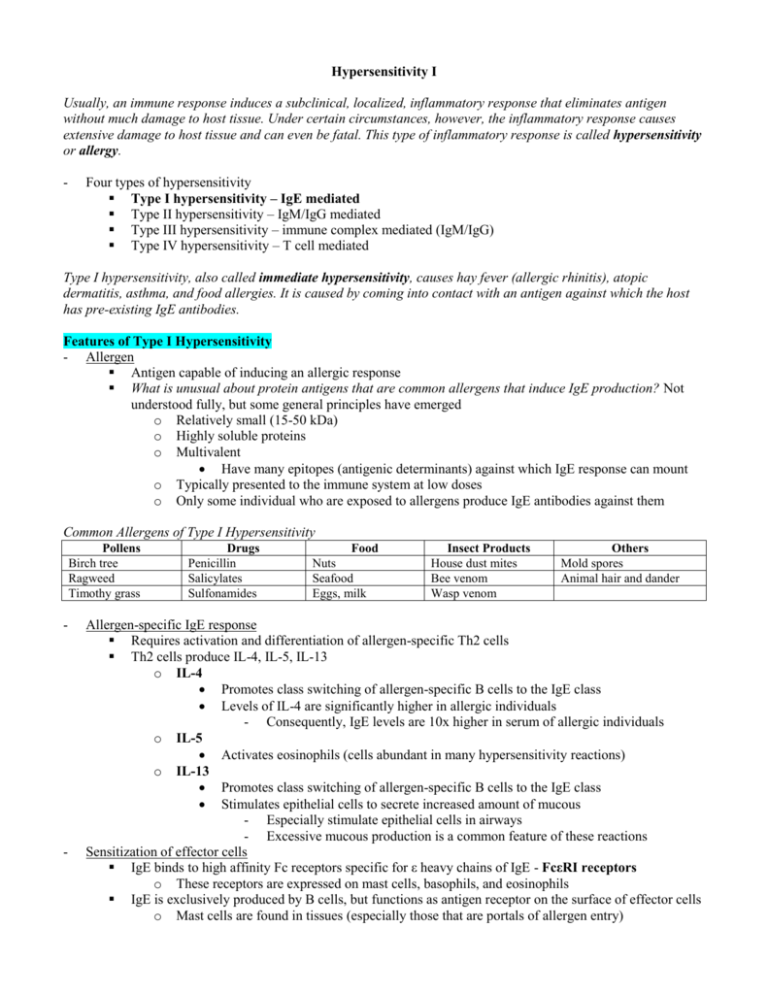
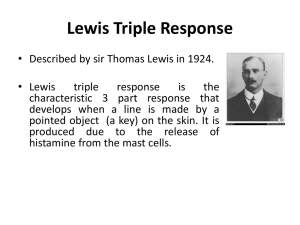
Hypersensitivity I Usually, an immune response induces a subclinical, localized, inflammatory response that eliminates antigen without much damage to host tissue. Under certain circumstances, however, the inflammatory response causes extensive damage to host tissue and can even be fatal. This type of inflammatory response is called hypersensitivity or allergy. - Four types of hypersensitivity Type I hypersensitivity – IgE mediated Type II hypersensitivity – IgM/IgG mediated Type III hypersensitivity – immune complex mediated (IgM/IgG) Type IV hypersensitivity – T cell mediated Type I hypersensitivity, also called immediate hypersensitivity, causes hay fever (allergic rhinitis), atopic dermatitis, asthma, and food allergies. It is caused by coming into contact with an antigen against which the host has pre-existing IgE antibodies. Features of Type I Hypersensitivity - Allergen Antigen capable of inducing an allergic response What is unusual about protein antigens that are common allergens that induce IgE production? Not understood fully, but some general principles have emerged o Relatively small (15-50 kDa) o Highly soluble proteins o Multivalent Have many epitopes (antigenic determinants) against which IgE response can mount o Typically presented to the immune system at low doses o Only some individual who are exposed to allergens produce IgE antibodies against them Common Allergens of Type I Hypersensitivity Pollens Birch tree Ragweed Timothy grass - - Drugs Penicillin Salicylates Sulfonamides Food Nuts Seafood Eggs, milk Insect Products House dust mites Bee venom Wasp venom Others Mold spores Animal hair and dander Allergen-specific IgE response Requires activation and differentiation of allergen-specific Th2 cells Th2 cells produce IL-4, IL-5, IL-13 o IL-4 Promotes class switching of allergen-specific B cells to the IgE class Levels of IL-4 are significantly higher in allergic individuals - Consequently, IgE levels are 10x higher in serum of allergic individuals o IL-5 Activates eosinophils (cells abundant in many hypersensitivity reactions) o IL-13 Promotes class switching of allergen-specific B cells to the IgE class Stimulates epithelial cells to secrete increased amount of mucous - Especially stimulate epithelial cells in airways - Excessive mucous production is a common feature of these reactions Sensitization of effector cells IgE binds to high affinity Fc receptors specific for ε heavy chains of IgE - FcεRI receptors o These receptors are expressed on mast cells, basophils, and eosinophils IgE is exclusively produced by B cells, but functions as antigen receptor on the surface of effector cells o Mast cells are found in tissues (especially those that are portals of allergen entry) o - - Mast cells Primary effector cells of type I hypersensitivity Have high affinity FcεRI receptors, to which much of the IgE of the body is bound o Half life of IgE in the bound state is several weeks o Half life of IgE in serum is 2-3 days Basophils and eosinophils also exhibit FcεRI receptors, to which IgE binds in type I hypersensitivity response - Skin Mucous membranes Connective tissue Basophils and eosinophils are present in blood Features of mast cells relevant to type I hypersensitivity o Large, mononuclear cells o Heavily granulated (more so than other effector cells) Granules contain potent mediators of immediate hypersensitivity reactions o Have a high density of FcεRI receptors (like basophils) 40,000-250,000 receptors per cell A single IgE molecule binds to each receptor Each IgE molecule can have its own antigen specificity Meaning that each cell represents a huge range of antigen specificity Cross-linking of FcεRI receptors and degranulation Effector cells are activated by cross linking of FcεRI receptors Occurs via binding of multivalent antigens with cell-bound IgE molecules In an individual allergic to a particular antigen, a large proportion of IgE molecules bound to mast cells (and other effector cells) are specific for that antigen o Thus, exposure to antigen will cross link enough IgE molecules to illicit mast cell activation In non-allergic individuals, mast cell-associated IgE molecules are specific for many different antigens, all of which induce very low levels of IgE production. Therefore, no single antigen will cross link enough IgE molecules to cause significant mast cell activation Activation of mast cells via cross linking of IgE molecules on its surface induces degranulation o Very rapid process o Secretory granules fuse with the plasma membrane and release preformed contents (primary mediators) into the extracellular environment - Mediators Clinical manifestation of type I hypersensitivity are attributable to the biological effects of mediators Primary mediators o Pre-made, stored in granules o Biological effects are observed within minutes of mast cell activation Secondary mediators o May be synthesized after target-cell activation o May be released via enzymatic breakdown of cell membrane phospholipids during degranulation Like mast cells, basophils and eosinophils also bind allergens by cross-linking with IgE. When recruited to inflammatory sites, they are degranulated via the same mechanism as mast cells. Basophil primary and secondary mediators have the same effects as mast cell mediators. In contrast, the granule proteins of eosinophils are toxic to parasites. Important mediators of type I hypersensitivity Mediator Primary mediators Histamine, seratonin (vasoactive amines)* Eosinophilic chemotactic factor (ECF-A) Proteases Secondary mediators Leukotrienes Prostaglandins Cytokines (TNFα, IL-4 are most important) Effect Increased vascular permeability, contraction of respiratory and intestinal smooth muscle, relaxation of blood vessels Eosinophil chemotaxis Mucous secretion, degradation of blood-vessel basement membrane, generation of complement split products Increased vascular permeability, contraction of pulmonary smooth muscle Vasodilation, contraction of pulmonary smooth muscle, platelet aggregation TNFα causes inflammation; IL-4 perpetuates Th2 response * Histamine is most important, but in rodents, serotonin may be of equal or greater importance - Histamine Shares structural feature of an amine group Considered a vasoactive amine because of its action on blood vessels Acts by binding to histamine receptors on many different cell types Actions are short-lived because it is rapidly catabolized Binding to endothelial cells causes cell contraction leading to leakage of plasma into tissues Stimulates endothelial cells to synthesize vascular smooth muscle relaxants o Prostacyclin – causes vasodilation Actions cause “wheal and flare” reaction of immediate hypersensitivity Causes contraction of intestinal and bronchial smooth muscle o Contributes to increased peristalsis associated with ingested allergens o Contributes to increased bronchospasms associated with asthma Antihistamines are histamine receptor antagonists that inhibit the effects of histamine. Bronchoconstriction in asthma is more prolonged than the effects of histamine, suggesting that other mast cell-derived mediators are important in causing asthma. Thus, antihistamines are not effective remedies in asthma. - - Prostaglandins Bind to receptors on smooth muscles Act as vasodilators (relaxes smooth muscle) Aspirin and non-steroidal anti-inflammatory drugs can block the synthesis of prostaglandins Leukotrienes Aspirin and non-steroidal anti-inflammatory drugs induce increased production of prostaglandins Effects are more pronounced and longer-lasting than that of histamine Active at nanomole concentrations - - o Can be 1000x more potent as bronchoconstrictors than histamine o More potent stimulators of vascular permeability and mucous secretion than histamine Blocking the binding of leukotrienes to their receptors leads to inhibition of their physiologic actions Cytokines Mast cells produce many cytokines that contribute to inflammation Most important cytokines are TNFα and IL-4 o TNFα induced inflammation o IL-4 perpetuates the Th2 response Genetic predisposition Genetic predisposition to develop type I hypersensitivity reactions is multigenic o An inheritable characteristic controlled by multiple genes Polymorphisms in IL-4, IL-13, or IL-14 cytokine genes o Associated with tendency to develop atopy, immediate hypersensitivity, and asthma Atopy is a clinical syndrome involving the hereditary predisposition of an individual to produce IgE antibodies in response to some environmental antigens and to develop strong type I hypersensitivity (allergic) responses. Atopy can manifest in different forms such as asthma, urticaria (hives), or chronic eczema Increased tendency to produce IgE against some, but not all, antigens may be linked to MHC II alleles o Atopic individuals inherit MHC II alleles that can bind and display dominant epitopes of certain allergens Phases of Type I Hypersensitivity - Sensitization phase IgE antibodies are produced in response to an antigenic stimulus IgE bind to specific receptors on mast cells and basophils - Activation phase Re-exposure to an antigen causes cross-linking of FcεRI that triggers mast cell and basophil degranulation (60-300 seconds) and the release of pharmacologically-active mediators - Effector phase Mediators act on targets and exhibit their biological effects Clinical Applications - Localized anaphylaxis or atopy Demonstrate early and late phase reactions o Wheal and flare reaction (early phase) Occurs within 30 minutes after administration of allergen Injection site becomes red - Local vasodilation - Engorgement with RBCs Soft swelling at site (“wheal”) - Results from plasma leakage from venules Characteristic red swelling around rim of wheal (“flare”) - Blood vessels at margin of wheal dilate and become engorged with RBCs o Late phase reaction Occurs within 2 to 6 hours after administration of allergen Accumulation of inflammatory leukocytes (neutrophils, eosinophils, basophils, CD4+ Th2 cells) Inflammation is maximal by 24 hours, then gradually subsides Reaction is rich in eosinophils Reaction cannot be inhibited by antihistamines Reaction can be eliminated by corticosteroids that inhibit cytokine synthesis Allergic rhinitis (hay fever) o Caused by airborne allergens that react with IgE-sensitized mast cells in nasal passages and conjunctiva o Mediators released from mast cells cause localized vasodilation and increased capillary permeability Leads to watery exudation of conjunctiva o Typical signs – intense lacrimation, sneezing, and coughing Dogs – prone to runny noses, sneezing, and excessive lacrimation Asthma o Activation of mast cells in lower airways Leads to bronchial constriction and increased secretion of fluid and mucus Results in difficulty breathing due to trapped air in lungs o Characterized by chronic inflammation Occurs in the absence of allergen due to airways becoming hyper-reactive to other factors - Cigarette smoke, viral or bacterial infection, exercise, or sudden exposure to cold can trigger asthma attack Chronic inflammation is due to increased presence of lymphocytes, eosinophils, neutrophils and other leukocytes o Basenji dogs and cats are particularly prone to sensitive airways and asthma Food allergies o Mast cell degranulation in the GI tract Leads to smooth muscle contraction, increased peristalsis, and vasodilation Causes vomiting and diarrhea o Dogs have food allergies Atopic dermatitis o Allergies to inhaled particles (dogs and cats) o Chronic dermatitis skin lesions can be found anywhere on the body Crusting, scaling, pyoderma Can lead to intense pruritus (bleeding underneath skin) o Cutaneous inflammatory infiltrate contains mast cells, dendritic cells, and low numbers of eosinophils, and neutrophils o Chronic inflammation is cytokine derived - o Reaction is treated by corticosteroids, not antihistamines Systemic anaphylaxis or anaphylactic shock Onset occurs within minutes of systemic absorption of an allergen Triggered by a wide range of antigens o Insect bites, drugs (i.e. penicillin, insulin, antitoxin), vaccines, seafood, nuts Widespread mast cell degranulation leads to the systemic release of vasoactive mediators (mainly histamine and leukotrienes) that has numerous effects o General vasodilatation and SM contraction o Sudden loss of blood pressure o Massive edema, diarrhea, vomiting o Severe bronchiole constriction o Death due to asphyxiation Food allergies o Mast cell degranulation in GI tract leads to increased permeability of mucous membranes, which allows entry of allergen into blood stream Allergen causes anaphylactic shock due to widespread mast cell degranulation Can also cause less severe system reactions (i.e. asthma, atopic urticaria of skin) - Hives may appear within minutes or up to two hours after eating, depending on where food is absorbed in digestive tract Milk allergy o Cattle are allergic to the α Casein protein within their own milk o Delays in milking increases intramammary pressure, which can sometimes forces milk proteins to enter the bloodstream In allergic cattle, this results in reactions that range from milk discomfort with urticarial lesions to acute anaphylaxis Diagnosis - Skin test reaction Wheal and flare reaction develops within 30 minutes of intradermal inoculation of allergen Late phase reaction develops 4 to 6 hours after testing and sometimes last 24 hours - Antibody-based tests Radioallergosorbent test o Highly sensitive technique that detects serum IgE levels specific for a specific allergen o Patient’s serum is added to allergen coupled to beads (or disks) o Amount of specific IgE bound is determined by adding 125I-labeled rabbit anti-dog IgE antibodies and measuring using radioactivity by gamma counter ELISA o Same as RAST, without use of radioactive substance Therapy - Environmental intervention – identify the offending allergen and avoid contact - Drugs Antihistamines o Receptor antagonists – compete with histamine for receptors on target cells Bind to receptors with a higher affinity than their histamine counterparts o Treat sneezing, itching, and runny noses Antileukotrienes o Receptor antagonists – compete with leukotrienes for receptors on target cells Effectively block leukotriene ability to bind to target cells Therefore, inhibit the physiological actions of leukotrienes o Used to treat asthma o Montelukast sodium – active ingredient in SINGULAIR Cromolyn sodium o Stabilizes mast cell membranes and prevents mast cell degranulation o Used to treat asthma (present in inhalers) Theophylline o Increases cAMP levels Results in relaxation of bronchial muscles and decreased mast cell granulation o Used to treat asthma Corticosteroids o Block the production of inflammatory cytokines o Used to treat asthma (present in inhalers) Epinephrine o Increases cAMP levels Results in relaxation of bronchial muscles and decreased mast cell granulation o Used to treat life-threatening systemic anaphylaxis MAb o Bind to the FcR1 receptor on the Fc region of mast cells o Prevents IgE from binding to mast cells o Omalizumab Immunologic intervention (hyposensitization) There is no drug that treats an allergy to a specific allergen. But once know what allergen the individual is allergic to, can use hyposensitizing/desensitizing vaccine Reduced to severity of type I reactions Patients are injected subcutaneously over an extended period of time with increasing doses of the antigen to which they sensitive Repeated introduction of allergen causes a shift towards IgG production as well as shift to Treg subset, which suppresses the Th2 response (the IgE response is eventually turned off) - Protective Role of IgE - Principal protective function of IgE-mediated immune reactions is the eradication of parasitic worms (i.e. helminths) - Antibodies bind to the surface of helminths and induce attachment of eosinophils via FcεRI receptors Binding of eosinophil FcεRI receptors to IgE leads to cross-linking of FcεRI receptors Consequently, eosinophils degranulate and release contents of their granules o Principally major basic protein (MBP) o MBP (not specific to worms) coats the surface of the worm and kills it o MBP is toxic to both worm and host tissue