The recognition and Treatment of First
advertisement

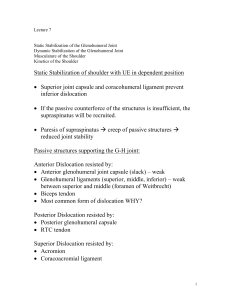
The recognition and Treatment of First-time Shoulder Dislocation in Active Individuals. (Wang, Arcero and Mazzocca, 2009). Glenohumeral instability affects approx 2% of the population and posterior instability occurs in only 2% to 5% of those with shoulder instability. It is doubled in younger athlete’s population. The active mechanism in GHS is primarily provided by the rotator cuff muscles. The type and severity of pathoanatomic lesions is influenced by the patient age, mechanism of injury and severity of trauma. Younger people tend to sustain labrel tears with dislocation; where as older patients with dislocation sustain rotator cuff tears. The inferior GHL (glenohumeral ligament) is the primary ligamentous restraint to anterior glenohumeral translation specifically with the arm in abduction and ER position. Detachment of the anterior labrum and capsule (bankart lesion) is considered one of the major pathoanatmoical features of traumatic anterior labrum, glenoid depth is decreased up to 50% and passive restraints is also lost. The incidence of bankart lesion after initial anterior shoulder dislocation has been reported to be 87%-100%. Lateral detachment of the IGHL from the humeral neck is another lesion that can occur from anterior shoulder dislocation ASD. This injury is referred to as humeral avulsion of the GHL. Traumatic glenoid humeral head fractures can occur with ASD. Two types of fractures involving anterior inferior glenoid: glenoid rim fracture and avulsion fracture. In the first time dislocation the athlete will be in obvious discomfort and experiencing intense pain, important to perform a prereduction and postreduction neurovascular exam. Most commonly 42% of people that are involved in the anterior dislocation, the axillary nerve will be reported to be injured, suprascapular nerve due to traction and the long thoracic nerve. They will resist any attempt to move the effected arm. Physical examination findings: asymmetry of the deltoid contour, palpable fullness below coracoids process towards the axilla that may occur on the affected side. Treatment: The decision for treatment in any patient after dislocation should be individualised. Decisions are made based on the age, activity level of the patient. Generally those that are involved in contact sports and ages 15 to 25 years acute repair may be a viable option based on the high risk of reacurrance, apprehension, impact on sports participation and quality of life, they favour arthroscopic instability repair for athletes in this age group. Patients who are age 25-40 have a much lower recurrence rate of dislocation in general and conservative treatment is generally the best RX. Older patients over 40, who sustain a Anterior dislocation have lower recurrence rates again but can residual disability from associated soft tissue injuries such as a rotator cuff tear, nerve injury or vascular injury. Traditional no-operative treatment has included a period of immobilisation with the arm in internal rotation for 6 weeks, this has not reduced the recurrence rate. Degenerative joint disease was found in both surgical and non-surgical cases. A short term clinical study revealed decreased recurrence rates in patients that were immobilised in ER. After 3 weeks of immobilisation they had a recurrence rate of 26% while those who were in IR had a 42% reccurance rate and 46% in patients that were younger than 30 years old. Athletes who sustain a first time dislocation at the end of the season or spring practice, one option is early mobilisation, rehabilitation and return to full activity. Another option is to immobilise for 3-4weeks, proceed with rehab, and return the athlete to sport after 6-8 weeks. In the young, contact athlete, modern operative stabilisation (open and arthoscopic) which reduces the recurance rate from the 80%-90% range-3-15% range. This is preferred with first time dislocation as the reccurane rate is decreased and it improves a better quality of life. The first 2 weeks after the injury occurs is the best time to operate, taking advantage of the good condition of the capsulolabral tissue. Focus of surgery is to repair the capsulolabral avulsion with suture anchors. Postoperative Treatment The first goal is to maintain anterior-inferior stability. The second is to restore adequate motion, specifically ER. 3rd goal is to succefully return back to sport or physical activity in a reasonable amount of time. Protocol includes immobilisation, pendulum exercises also. Active assisted ROM for ER and forward elevation are also started at this time. This is maintained for 6 weeks. Cold therapy is good to reduce pain post operatively. From 6-12 weeks AROM and active assisted are started with the goal of estabilishing full ROM, no strengthing exercises or repetitive exercise are started until after full range of motion has been estabilished. This protocol is based on the tendon to tendon bone healing. Strength training is begun once there is full, painless AROM at 12 weeks with sports specific exercises started at 16-20 weeks, finally contact sports are started between 20-24 weeks postoperatively. RESULTS: Arthoroscopic repair not only decreases the recurrence rate but increases the quality of life. Acute arthroscopic repair for the athlete in first-time anterior dislocation leads to improved outcomes. The decsion is made on patients age, timing during season, athletic level, contact vs. non contact sports. PS this article took me FOREVER TO READ!