PART ONE: Bioaerosol production when using - Bio-Link
advertisement

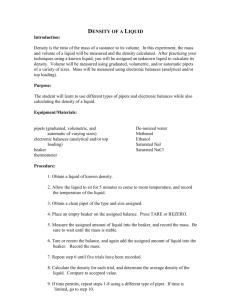
Laboratory: Bioaerosol Production in the Laboratory Purpose In this lab you will prepare to work with microbial and animal cell culture by examining how and when bioaerosols are produced. You will Demonstrate how aerosols are created See how aerosols can scatter over a flat surface Design an experiment to demonstrate how aerosols are produced Background Bioaerosols are mechanically produced droplets of liquid suspended in air that contain infectious particles. When working with biohazards, it is relatively easy to protect yourself from the biohazardous agent when it is clearly visible, such as when working with a culture plate or liquid culture of a microbe. Bioaerosols present more serious problems because the liquid droplets that comprise the bioaerosol are often too small to be seen with the naked eye. Bioaerosols increase the likelihood of contracting a laboratory-acquired infection in a number of ways. Obviously, workers in the laboratory can inhale small liquid droplets suspended in air. To minimize the risk of inhalation, workers may, depending upon the microbe or virus being used, choose to wear masks, breathing apparatus, or work in a biological safety cabinet. Of course, another method of controlling the risk associated with bioaerosols is to minimize the likelihood that bioaerosols are produced in the first place. Once procedures that produce bioaerosols have been identified, scientists may be able to devise alternate procedures that will reduce bioaerosol production. One purpose of this laboratory activity is to identify common laboratory procedures that may generate bioaerosols. This risk associated with bioaerosol production is not restricted to inhalation, however. Although bioaerosols remain airborne for some time, the infectious particles do, eventually, settle. This introduces the risk of ungloved hands picking up these particles and introducing them into the body via the eyes, nose or throat of the laboratory worker as well. Again, minimizing bioaerosol production or working in a biological safety cabinet will reduce this risk. Additionally, routine disinfection of work surfaces will decrease the likelihood of workers picking up settled infectious particles. Wearing gloves, goggles or safety glasses, and lab coats will also decrease the chance that infectious particles will settle on the worker or his street clothes and be carried outside of the controlled environment of the laboratory. So how are bioaerosols produced? There are numerous ways in which this sprays may be generated in the laboratory. Pipets are one of the basic tools of school and research laboratories. They are used for volumetric measurement of fluids and for transfer of these fluids from one container to another. Bioaerosols, the most common hazard associated with pipetting, are created when liquid drops from a pipet to a work surface, when cultures are mixed by alternate suction and expulsion, when an inoculum is forcefully ejected onto a culture dish or when the last drop is blown out of the pipet tip. It has been demonstrated by high-speed photography that an aerosol of approximately 15,000 droplets, most under ten micrometers in diameter, is produced when the last drop of fluid in the tip of a pipet is blown out with moderate force. 1 Laboratory activity Overview: In this laboratory you will be attempting to visualize how bioaerosols are produced and how they can be transmitted throughout the laboratory. Because infectious particles are too small to be seen by the naked eye, a safe fluorescent dye is used to simulate a biohazardous liquid. Precautions: students will wear laboratory coats, gloves and eye protection throughout this exercise. This lab will consist of the following parts: Examination of bioaerosol production by micropipetting Examination of bioaerosol production when using serological pipets Development of an experiment to visualize bioaerosol production in other common laboratory procedures Experimental protocol PART ONE: Bioaerosol production when using micropipettors 1. Cover lab benches with protective paper. 2. Put down a sheet of light colored absorbent paper. 3. Practice pipetting the saturated dyes from the stock bottle to a microcentrifuge tube, test tube and beaker. 4. Using a handheld UV lamp, (BE SURE TO WEAR UV-RESISTANT SAFETY GLASSES AT ALL TIMES WHEN ANYONE IN THE LABORATORY IS USING THE HANDHELD UV LAMPS!!) look for spill or sprays, indicating aerosol production. The dyes will fluoresce under the UV lamp making very small spills or sprays visible. 5. Check hands, lab coats, and your work area for further contamination. PART TWO: Bioaerosol production when using serological pipets 1. Drop an empty but wet pipet (one that was used to pipet water) from a height 12 inches above the lab bench surface. (You want a little residual liquid left in the pipet for this activity). 2. Circle the water droplets you can see on the lab bench paper. 3. Drop an empty but wet pipet, one that was used to pipet the fluorescent dye, 12 inches above the lab bench surface. 4. Circle the dye droplets with a different colored pen or pencil. 5. Compare the number and sizes of droplets produced by the water aerosol and the dye aerosol. 6. Use the handheld UV lamp to search for droplets not visible to the naked eye. PART THREE: Designing an experiment to create bioaerosols 1. Make a list of other ways of creating aerosols in lab. 2. Compare your list with at least two other groups. 3. Choose a different method per group and carry out your experiment. Record how easily the fluorescent dye is spread by your group. 2 Results: 1. Record your observations of bioaerosol production in Parts One, Two and Three in your laboratory notebook. 2. Compare your results for Part Three with those of other groups. Can you draw any conclusions about which common laboratory procedures are more or less likely to produce bioaerosols? Discussion questions 1. What did you learn in this activity concerning the ease with which bioaerosols can be created in the laboratory? 2. What do the results of this laboratory suggest about the need for proper cleanup following handling of biohazardous liquids? In what ways can you envision workers (both laboratory and non-laboratory) contracting laboratory-acquired infections? 3. Can you suggest ways to minimize bioaerosol production in any of the laboratory procedures investigated in Part Three of this activity? Can you suggest any alternate procedures that would reduce bioaerosol production? 4. In what ways can you reduce the risks associated with pipetting biohazardous liquids in the laboratory? 3