Resident Expectations - Clinical Departments
advertisement
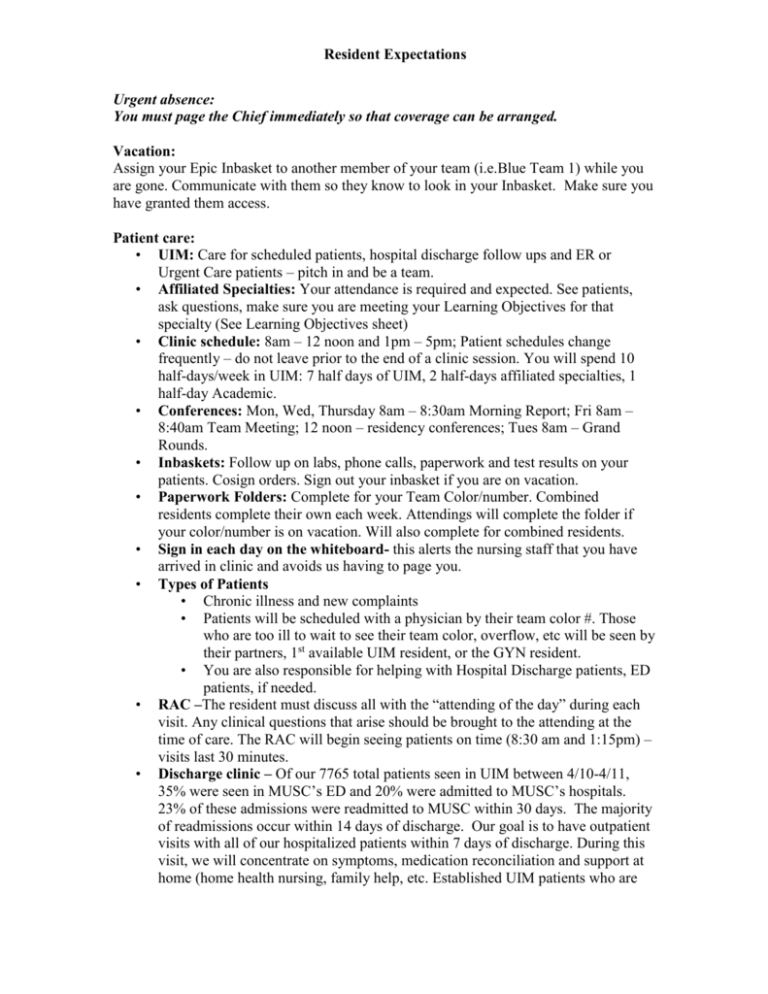
Resident Expectations Urgent absence: You must page the Chief immediately so that coverage can be arranged. Vacation: Assign your Epic Inbasket to another member of your team (i.e.Blue Team 1) while you are gone. Communicate with them so they know to look in your Inbasket. Make sure you have granted them access. Patient care: • UIM: Care for scheduled patients, hospital discharge follow ups and ER or Urgent Care patients – pitch in and be a team. • Affiliated Specialties: Your attendance is required and expected. See patients, ask questions, make sure you are meeting your Learning Objectives for that specialty (See Learning Objectives sheet) • Clinic schedule: 8am – 12 noon and 1pm – 5pm; Patient schedules change frequently – do not leave prior to the end of a clinic session. You will spend 10 half-days/week in UIM: 7 half days of UIM, 2 half-days affiliated specialties, 1 half-day Academic. • Conferences: Mon, Wed, Thursday 8am – 8:30am Morning Report; Fri 8am – 8:40am Team Meeting; 12 noon – residency conferences; Tues 8am – Grand Rounds. • Inbaskets: Follow up on labs, phone calls, paperwork and test results on your patients. Cosign orders. Sign out your inbasket if you are on vacation. • Paperwork Folders: Complete for your Team Color/number. Combined residents complete their own each week. Attendings will complete the folder if your color/number is on vacation. Will also complete for combined residents. • Sign in each day on the whiteboard- this alerts the nursing staff that you have arrived in clinic and avoids us having to page you. • Types of Patients • Chronic illness and new complaints • Patients will be scheduled with a physician by their team color #. Those who are too ill to wait to see their team color, overflow, etc will be seen by their partners, 1st available UIM resident, or the GYN resident. • You are also responsible for helping with Hospital Discharge patients, ED patients, if needed. • RAC –The resident must discuss all with the “attending of the day” during each visit. Any clinical questions that arise should be brought to the attending at the time of care. The RAC will begin seeing patients on time (8:30 am and 1:15pm) – visits last 30 minutes. • Discharge clinic – Of our 7765 total patients seen in UIM between 4/10-4/11, 35% were seen in MUSC’s ED and 20% were admitted to MUSC’s hospitals. 23% of these admissions were readmitted to MUSC within 30 days. The majority of readmissions occur within 14 days of discharge. Our goal is to have outpatient visits with all of our hospitalized patients within 7 days of discharge. During this visit, we will concentrate on symptoms, medication reconciliation and support at home (home health nursing, family help, etc. Established UIM patients who are Resident Expectations • • • • • discharged will be seen in their panel resident’s clinic if an appointment is available within 7 days. Sickle Cell Clinic – In an effort to improve continuity of care and reduce ED visits and hospitalizations, we have a Sickle Cell Medical Home for approximately 50 patients of our patients at high risk for admission. We aim to provide comprehensive care for these patients including open access appointments for any complaint. Regular continuity clinic sessions will be held Mon, Wed and Fri afternoons. Patients wishing to be seen at other times will be added onto the urgent SS schedules every morning. We will be giving IV fluids and pain medications to these patients as needed in accordance with an acute care plan developed by the Sickle Cell team. Residents will not be directly involved with this care. PCMH – Our practice has been designated by the NCQA as a Level 3 Patient Centered Medical Home. This model of care focuses on the following principles: a personal physician, physician directed medical practice, whole person orientation, coordinated/integrated care, care that is safe and high-quality, enhanced patient access, and appropriate payment. Continuity and Follow-Up – • You are responsible for all results coming back to Epic that you have ordered. If you are on vacation, it is your responsibility to get coverage for your inbasket by someone on your team color. Make sure you grant access to inbasket to all physicians on your team color # and case manager. To cover you will need to ‘attach’ to their “In-baskets after they have granted you “permission”. See epic tools for directions. • Follow up on all labs, test results for your patients. Communicate all results to the patient with either: letter sent via Epic, phone call you document in Epic, or My Chart release (See “More Epic Tips for details) • Go over your list of patients and let your Case Manager know if there is a clear error. If the patient has not seen anyone in our practice consistently and they are assigned to you, they are now your patient. We will use this list to give you personalized, individual feedback on clinical measures. • Your Case Manager has a paperwork folder for your Color + number team (i.e. Pink 1) – complete this every day and return. No paperwork should go to individual mailboxes (cubbies in the back room) • Please ensure every patient that you see has scheduled follow-up with their primary care physician. Add the appropriate physician’s name in the comment box under “Follow-up” in Epic so that the patient gets back with the appropriate physician. (See Epic Tips) Documentation: Your notes should be completed within 24hr of seeing the patient and preferably prior to leaving clinic the day you saw the patient. You should not delay seeing patients who have arrived in order to write your clinic notes. If you bring a patient back quickly for follow-up, communicate the reason for this in your note – be clear! Medications: You are expected to update the Medication list each visit and eprescribe all needed prescriptions at the time of the visit. Please give sufficient refills (up to 11 refills) or enough to f/u visit. If you do not your nurse will be Resident Expectations paging you. If a patient is on long term pain medications, please ensure that there is a physician/patient controlled substance agreement. Patients on Pain Agreements are required to be seen q 4 months by their primary care MD. Pharm D’s are available to assist with management of those patients on long term anticoagulation, provide diabetic education, smoking cessation counseling, and assist with medication management. Education: Update your Portfolio weekly during the month • Complete Self-assessment at the beginning of the month • Outline 3 learning goals per month • Outline 3 mini-CEX goals per month • Complete 7 on-line Hopkins modules per month • Present Morning Report using structured curriculum (per schedule) • Attend all conferences • Meet with your faculty 2 weeks into the block– sign off on your MidPoint evaluation checklist Academic ½ days: • Attend scheduled lectures and meetings • Complete patient care paperwork, labs, test results, letters, etc. for Team (i.e. Blue 1) • Work on QI project and publications/presentations related to clinic • Complete on-line ambulatory curriculum (Hopkins) and Board Review • Morning Report Prep • Update your portfolio weekly Clerical: • Continuity a resident issue – designate f/u resident on the AVS in comment section • Vacation – add team color to the vacation form; 1 from each color must be in clinic • AMION schedule for clinic done at least 2 months in advance Attending Duties • Beginning of the month – Residents will be oriented and set goals for the information below; record in portfolio • 2 weeks – Review the following with residents: • Learning Goals 3 (Self-assessment) • Mini-CEX goals 3 (Resident choice) • On-line curriculum progress 7 • Morning report progress 1 • Aging Q3 Acove progress • Feedback on performance: complete the MidPoint Evaluation form • Learning goals Resident Expectations • • • • Mini-CEX goals On-line curriculum goals Morning Report assignment End of the month – Whole team evaluates at week 3 – Meet with resident to do feedback if needed or desired