Evaluation & Management - Coding Certification Tips
advertisement

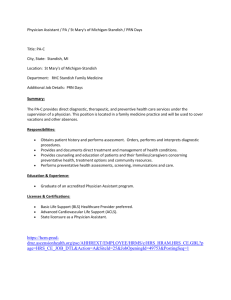
Evaluation and management 1. How does the CPT Professional Edition define a new patient? a. A new patient is one who has not received any professional services from the physician or another physician of the same specialty who belongs to the same group practice, within the past two years. b. A new patient is one who has not received any professional services from the physician or another physician of the same specialty who belongs to the same group practice, within the past three years. c. A new patient is one who has received professional services from the physician or another physician of the same specialty within the last two years for the same problem. d. A new patient is one who has received hospital services but has never been seen in the clinic by the reporting physician. 2. James, a 35-year-old new patient, received 45 minutes of counseling and risk factor reduction intervention services from Dr. Kelly. Dr. Kelly talked to James about how to avoid sports injuries. Currently, James does not have any symptoms or injuries and wants to maintain this status would you report this.This was the only service rendered. How service? a. 99213 b. 99203 c. 99385 d. 99403 3. Andrea, a 52-year-old patient, had a hysterectomy on Monday morning. That afternoon, after returning to her hospital room, she suffered a cardiac arrest. A cardiologist responded to the call and delivered one hour and 35 minutes of critical care. During this time the cardiologist ordered a single view chest x-ray and provided ventilation management. How should you report the cardiologist’s services? a. 99291, 99292 b. 99291, 99292, 71010, 94002 c. 71010, 94002, 99231 d. 99291, 99292, 99292-52 4. Brandon was seen in Dr. Shaw’s office after falling off his bunk bed. Brandon’s mother reported that Brandon and his sister were jumping on the beds when she heard a “thud.” Brandon complained of knee pain and had trouble walking. Dr. Shaw ordered a knee x-ray that was done at the imaging center across the street. The x-ray showed no fracture or dislocations. Dr. Shaw had seen Brandon for his school physical six months ago. Today, Dr. Shaw documented a detailed examination and decision-making of moderate complexity. He also instructed Brandon’s mother that if Brandon had any additional pain or trouble walking he should see an orthopedic specialist. How should Dr. Shaw report her services from today’s visit? a. 99204 b. 99394, 99214 c. 99214 d. 99203 5. Adam, a 48-year-old patient, presented to Dr. Crampon’s office with complaints of fever, malaise, chills, chest pain, and a severe cough. Dr. Crampon took a history, did an exam, and ordered a chest x- ray. After reviewing the x-ray, Dr. Crampon admitted Adam to the hospital for treatment of pneumonia. After his regular office hours, Dr. Crampon visited Adam in the hospital where he dictated a comprehensive history, comprehensive examination, and decision-making of moderate complexity. How would you report Dr. Crampon’s services? a. 99214 b. 99222 c. 99204, 99222-51 d. 99223, 99214-21 6. Why are the following codes not reported with continuing intensive care services (99478–99480): 36510, 36000, 43752, 51100, 94660, or 94375? a. These codes are deleted from the 2008 edition. b. These codes are included with continuing intensive care services. c. These codes are only add-on codes and should be reported with a modifier -51 d. These codes are Category III Codes and should never be reported with Category I codes. 7. Larry is being managed for his warfarin therapy on an outpatient basis. Dr. Nancy continues to review Larry’s INR tests, gives patient instructions, dosage adjustment as needed, and ordered additional tests. How would you report the initial 90 days of therapy including 8 INR measurements? a. 99363 b. 0074T c. 99214 d. This services is bundled with evaluation and management services 8. Dr. Jane admitted a 67-year-old woman to the coronary care unit for an acute myocardial infarction. The admission included a comprehensive history, comprehensive examination, and high complexity decision-making. Dr. Jane visited the patient on days two and three and documented (each day) an expanded problem focused examination and decision-making of moderate complexity. On day four, Dr. Jane moved the patient to the medical floor and documented a problem focused examination and straightforward decision-making. Day five, Dr. Jane discharged the patient to home. The discharge took over an hour. How would you report the services from day one to day five? a. 99213, 99232, 99231, 99239 x 2 b. 99221, 99222, 99223, 99238 c. 99231, 99232, 99355, 99217 d. 99223, 99232, 99232, 99231, 99239 9. Which code range would describe services for a critically ill patient who is 23 days old as a out patient? a. 99291–99292 b. 99293–99294 c. 99295–99296 d. None of the above 10. Mr. Johnson, a 38-year-old established patient is being seen for management of his hypertension, diabetes, and weight control. On his last visit, he was told he had a diabetic foot ulcer and needed to be hospitalized for this condition. He decided to get a second opinion and went to see Dr. Myers. This was the first time Dr. Myers had seen Mr. Johnson. Dr. Myers documented a comprehensive history, comprehensive examination, and decision-making of high complexity. He concurred with hospitalization for the foot ulcer and sent a report back to Mr. Johnson’s primary care doctor. How would you report Dr. Myers visit? a. 99245 b. 99205 c. 99215 d. 99255 11. How does the CPT Professional Edition define an emergency department? a. An organized hospital-based facility for the provision of unscheduled episodic services to patients who present for immediate medical attention. The facility must be available 24 hours a day. b. An organized hospital-based facility for the provision of scheduled episodic services to patients who present for immediate medical attention. The facility must be available 24 hours a day. c. An organized hospital-based facility for the care and treatment of chronically ill patients who present for services. The facility must be available on weekends and holidays. d. An organized outpatient-based facility for the care and treatment of unscheduled patient who present for immediate medical attention. The facility must be available 24 hours a day. 12. Lucus, a three-year-old new patient is seen for a well-child examination. The doctor documents an age appropriate history, examination, anticipatory guidelines, risk factor reduction intervention, and indicates Lucus’ immunizations are up to date. How would you report this service? a. 99392 b. 99213-25, 99385 c. 99203 d. 99382 13. 80-year-old patient is returning to the gynecologist’s office for pessory cleaning. Patient offers no complaints. The nurse removes and cleans the pessory, vagina is swabbed with betadine, and pessory replaced. For F/U in 4 months. What CPT® and ICD-9 should be used for this service? A. 99201, V45.59 B. 99211,V52.8 C. 99202, 996.65 D. 99212,V53.99 14. Patient was in the ER complaining of constipation with nausea and vomiting when taking Zovirax for his herpes zoster and Percocet for pain. His primary care physician came to the ER and admitted him to the hospital for intravenous therapy and management of this problem. His physician documented a detailed history, comprehensive examination and a medical decision making of moderate complexity. Which E/M service is reported? A. 99285 B. 99284 C. 99221 D. 99222 15. 20-day-old infant was seen in the ER by the neonatologist admitting the baby to NICU for cyanosis and rapid breathing. The neonatologist performed intubation, ventilation management and a complete echocardiogram in the NICU and provided a report for the echocardiography which did indicate congenital heart disease. Select the correct code(s) for the physician service. A. 99468-25, 93303-26 B. 99471-25, 31500, 94002, 93303 C. 99460-25, 31500, 94002, 93303 D. 99291-25, 93303 16. A 40 year-old patient is coming to see her primary care physician for hypertension. Her physician performs an expanded problem focused exam and low medical decision making. After the exam the patient discusses with her physician that the OBGYN office had just told her that her Pap smear came back with an abnormal reading and is worried since her aunt had passed away with cervical cancer. The physician spends an extra 45 minutes face-to-face time discussing with her the awareness, other screening procedures and treatment if it turns out to be cervical cancer. What code(s) should be used for this visit? A. 99215 B. 99213, 99354 C. 99213 D. 99213, 99403 17. A patient was admitted yesterday to the hospital for possible gallstones. The following day the physician who admitted the patient performed a detailed history, a detailed exam and a medical decision making of low complexity. The physician tells her the test results have come back positive for gallstones and is recommending having a cholecystectomy. What code should be reported for this evaluation and management service? A. 99253 B. 99221 C. 99233 D. 99234 18. A patient came in to the ER with wheezing and a rapid heart rate. The ER physician documents a comprehensive history, comprehensive exam and medical decision of moderate complexity. The patient has been given three nebulizer treatments. The ER physician has decided to place him in observation care for the acute asthma exacerbation. The ER physician will continue examining the patient and will order additional treatments until the wheezing subsides. Select the appropriate code(s) for this visit. A. 99284, 99219 B. 99219 C. 99284 D. 99235 19. Patient is here to follow up on her atrial fibrillation. Her primary care physician is not in the office. She will be seen by the partner physician that is also in the same practice. No new problems. Blood pressure is 110/64. Pulse is regular at 72. Temp is 98.6F Chest is clear. Cardiac normal sinus rhythm. Medical making decision is straightforward. Diagnosis: Atrial fibrillation, currently stable. What CPT® code is reported for this service? A. 99201 B. 99202 C. 99212 D. 99213 20. Documentation of a new patient in a doctor’s office setting supports the History in four elements for an extended history of present illness (HPI), three elements for an extended review of systems (ROS) and three elements for a complete Past, Family, Social History (PFSH) . There is an extended examination of six body areas and organ systems. The medical making decision making is of high complexity. Which E/M service supports this documentation? A. 99205 B. 99204 C. 99203 D. 99202 21.Two-year-old is brought to the ER by EMS for near drowning. EMS had gotten a pulse. The ER physician performs endotracheal intubation, blood gas, and a central venous catheter placement. The ER physician documents a total time of 30 minutes on this critical infant in which the physician already subtracted the time for the other billable services. Select the E/M service and procedures to report for the ER physician? A. 99291-25, 36555, 31500 B. 99291, 36556, 31500, 82803 C. 99285-25, 36556, 31500, 82803 D. 99475, 36556 22. 2-year-old is coming in with his mom to see the pediatrician for fever, sore throat, and pulling of the ears. The physician performs a brief history along with a problem pertinent review of systems. A limited exam was performed on the ears, nose and throat and respiratory systems. A strep culture was taken and came back positive. A diagnosis was also made of the infant having acute otitis media with effusion. The medical decision making was of moderate complexity with the giving of a prescription. What CPT® and ICD-9-CM codes should be reported? A. 99212, 462, 382.9 B. 99213, 034.0, 381.4 C. 99212, 034.0, 381.00 D. 99213, 034.0, 381.00 23. 42-year-old woman is being discharged today, 2/5/XX. She was admitted to the hospital 2/2/XX for acute diverticulitis. Refer to dictated notes for a detailed description of the history, exam, and assessment and treatment protocol. Patient was also seen in consultation by Dr Z. She was placed on intravenous antibiotics and has made slow steady progress. Today has no abdominal pain. Labs are normal and CT of the abdomen and pelvis showed changes consistent with diverticulitis in the left side of colon. She was given follow up instructions of her medications, what diet to have and to follow up with PCP in 10 to 14 days or return if pain resumes. Total time spent with patient 40 minutes. What CPT® code(s) should be reported? A. 99233, 99239 B. 99217 C. 99252, 99238 D. 99239 24. 63-year-old man is coming in for a second opinion for his sleep apnea. He has had it for the past five months. Sleep is disrupted by frequent awakenings and getting worse due to anxiety and snoring. He feels tired all the time, has some joint stiffness and night sweats; all other systems were negative. He is going through a divorce which is causing him anxiety and had a hernia repair two month ago. Doctor performs a comprehensive exam and orders labs and a sleep study test. Prescription was given to help with the anxiety. What CPT® code should be reported? A. 99203 B. 99204 C. 99244 D. 99214 25. A 55-year-old established patient is coming in for a pre-op visit; he is getting a liver transplant due to cirrhosis. The physician performs an expanded problem focused history, detailed examination, and moderate MDM. Patient agrees with his physician’s recommendations and the transplantation will take place as scheduled. After the evaluation, the patient expresses a number of concerns and questions for the prospective liver transplant. Physician spends an additional 30 minutes, excluding the time spent in doing the E/M service, in counseling and answering questions regarding the surgery and discussing possible outcomes. What CPT® codes should be reported? A. 99213, 99354 B. 99214, 99358 C. 99213, 99358 D. 99214, 99354 26. Physician performs a medical review and documentation on an 83-year-old patient still hospitalized for confusion for the last two days. She is alert and oriented x 3 today. Reviewing her labs from yesterday, her BNP was elevated suspecting her confusion is due to congestive heart failure. An echocardiogram is ordered and treatment will be for congestive heart failure. Patient is not safe to return home. What CPT® code should be reported? A. 99231 B. 99221 C. 99218 D. 99232 27. A plastic surgeon is called to the ED at the request of the emergency department physician to evaluate a patient that arrived with multiple facial fractures after being in an automobile accident for her opinion on the need for reconstructive surgery. The plastic surgeon arrives at the ED, obtains a history of present illness including an extended history of present illness; a system review, including constitutional, musculoskeletal, integumentary, neurologic, and EENMT; and the patient’s social history and past medical history. The plastic surgeon then performs a physical exam including respiratory, cardiovascular, and an extended examination of the skin and bony structures of the patient’s face. The plastic surgeon performs moderate medical decision making, including deciding the patient needs major surgery to repair the injuries. The plastic surgeon schedules the patient for surgery the next day and documents her full note with findings in the ED chart. A. 99284-57 B. 99244 C. 99243-57 D. 99221 28. At the request of the mother’s obstetrician, the physician was called to attend the birth of an infant being delivered at 29 weeks gestation. During delivery, the neonate was pale and bradycardic. Suctioning and bag ventilation on this 1000 gram neonate was performed with 100 percent oxygen. Brachycardia worsened; endotracheal intubation was performed and insertion of an umbilical line for fluid resuscitation. Later this critically ill neonate was moved from the delivery room and admitted to the NICU with severe respiratory distress and continued hypotension. What are the appropriate procedure codes? A. 99465, 99468 B. 99465, 99464, 99468-25, 31500, 36510-51 C. 99468, 99464 D. 99465, 99468-25, 31500-59, 36510-59 29. 38-year-old female initial visit, just moved from out of state, has neck and back pain for the last year and is getting worse. Pain is exacerbated when she drives, bends, or changes positions, and moderately alleviated with ibuprofen. Positive for aches and weakness in her muscles and tingling and numbness of the arms and hands, as well as headaches. All other systems are reviewed and are negative. She has had a partial hysterectomy and is divorced. Her mother has a history of breast cancer. The physician performs an exam on the following systems: constitutional, eyes, ENT, respiratory, cardiovascular, gastrointestinal, musculoskeletal, and neurologic. X-rays of the cervical and lumbar spine were taken. Will be sending her to get a MRI and to start physical therapy. Prescription was given for muscle relaxer. Select the appropriate CPT® code for this visit? A. 99203 B. 99204 C. 99214 D. 99244 30. A four-year-old patient presents with pain in the left forearm following a fall from a chair. The injury occurred one hour ago. Her mom applied ice to the injury but it does not appear to help. The ED physician performs a four system ROS. The patient lives at home with both parents and attends pre-K classes. The patient has no known drug allergies. The ED physician performs an extended six system exam. An X-ray is ordered, which shows a fracture of the distal end of the radius as read by the radiologist. The ED physician performs moderate conscious sedation with ketamine for 30 minutes. The fracture is reduced and cast applied by an orthopedic surgeon following consultation with the ED physician. The child was monitored with pulse oxymetry, cardiac monitor and frequent physician evaluation. The patient was discharged with a sling and requested to follow up with the orthopedic surgeon. Code the services performed by the ED physician. A. 99284, 99143 B. 99284-25, 99148 C. 99283-25, 99143 D. 99283 31. Dr. X performs a follow-up consultation on certain tests that were not available in a nursing facility for a 75- year-old-male that was having chest pain. Today the patient is feeling better after a GI cocktail with Maalox and Xylocaine. The EKG showed an arrhythmia and the chest X-ray came back normal. Dr. X performs a problem focused history. He listens to the patient’s heart and lungs. Dr. X makes the recommendation of repeat cardiac enzymes and EKG and to have a GI evaluation. The PCP accepts the recommendations and implements the plan of care. What CPT® code should be reported for Dr. X? A. 99241 B. 99232 C. 99308 D. 99251 32. Physician was called to the floor to evaluate a 94-year-old that had sudden weakness, hypotension, and diaphoresis. Physician found the patient in mild distress and dyspenic. Her BP 101/60, pulse 85. Her heart was positive for a systolic murmur. EKG came back with ST elevation V2-V6. Labs were still pending. She was admitted to CCU for Acute Antero-lateral MI and hypotension. Physician spent total critical care time of 48 minutes. Select the appropriate CPT® code for this visit: A. 99253 B. 99233 C. 99291 D. 99236 ANSWERS 1. “b” A new patient is described as not receiving any professional serves in the past three years. You can find this answer in the Evaluation and Management Services Guidelines and on the Decision Tree for New vs. Established Patients (same guidelines) in the CPT Professional Edition. 2. “d” Counseling and/or risk factor reduction intervention services are provided to patients with symptoms or established illness. 3. “a” The guidelines for critical care have a list of services that are included with critical care when performed by the physician providing the critical care and these services should not be reported separately. 4. “c” This is an established patient visit and meets two of the three key components for a 99214 level visit. 5. “b” The subcategory guidelines for Initial Hospital Care state, “When the patient is admitted to the hospital as an inpatient in the course of an encounter in another site of service (e.g., hospital, emergency department, observation status in a hospital, physician’s office, nursing facility) all evaluation and management services provided by that physician in conjunction with that admission are considered part of the initial hospital care when performed on the same date as the admission. Therefore, the services are reported with the initial hospital care code only. The office visit is a bundled service. 6. “b” These codes are included (bundled) and you can’t report them in addition to the Continuing Intensive Care Services. In the subcategory guidelines for these services it is noted, “…These codes include the same procedures that are outlined in the Pediatric Critical care services section and these services should not be separately reported.” 7. “a” This question deals with outpatient anticoagulant management. The code 99363 gives specific parameters for reporting. 8. “d” Day one admission or initial hospital care is 99223. Days two and three are subsequent hospital care services at 99232 and you should report them separately. Day four is subsequent hospital care at level 99231. Day five is the discharge service, which is based on time and code 99239 is reported for services of more than 30 minutes, regardless of the actual time. Report this code only once. 9. “a” Refer the page 21 in CPT manual. 10. “b” This is a new patient visit not a consultation. “A “consultation” initiated by a patient and/or family, and not requested by a physician or other appropriate source, …is not reported using the consultation codes but may be reporting using the office visit, home service, or domiciliary/rest home care codes.” Report a consultation code only when a request (written or verbal) is made by another physician or appropriate source, an opinion is rendered, and a written report is sent back to the “requestor.” In this case the patient initiated the visit. 11. “a” You can find this definition in the CPT Professional Edition under the subcategory guidelines for Emergency Department Services. 12. “d” Preventive medicine services are based on new vs. established patient and age. 13. B Scenario documents patient returning to the gynecologist guiding you to the codes for established patient office visit. This eliminates multiple choices A and C. For this scenario, the patient did not have any complaints that required the presence of a physician. There was no examination or medical making decision performed for the patient guiding you to code 99211. There must be an order for the patient to come in for the office visit. For the diagnosis code, the pessary was removed for cleaning with no documentation of a complication of the device nor is this device a contraceptive device; therefore, report V52.8 (Fitting, device, prosthetic, other specified) 14 . C According to CPT® guidelines: When the patient is admitted to the hospital as an inpatient in the course of an encounter in another site of service (example, hospital emergency department, observation status in a hospital, physician’s office, nursing facility) all evaluation and management services provided by that physician in conjunction with that admission are considered part of the initial hospital care when performed on the same date of service. Meaning for this scenario the patient’s physician had come to the ER and also admitted the patient on the same date of service, eliminating multiple choices A and B. The three key components are required for the Initial Hospital Care. Detailed History + Comprehensive Exam + Moderate MDM = 99221. 15. A According to CPT® subsection guidelines under Inpatient Neonatal and Pediatric Critical Care: If the same physician provides critical care services for a neonatal or pediatric patient in both the outpatient and inpatient setting on the same day, report only the appropriate Neonatal or Pediatric Critical Care codes 99468-99476 for all critical care services provided on that day. This eliminates multiple choice answers C and D. The baby is 20-days-old and you can not bill intubation (31500) and ventilation management with the neonatal and pediatric critical care codes, eliminating multiple choice B. 16. A According to E/M Guidelines “When counseling and/or coordination of care dominates (more than 50%) the physician/patient and/or family encounter (face-to-face in the office or other outpatient setting or floor/unit time in the hospital or nursing facility), then time may be considered the key or controlling factor to qualify for a particular level of E/M services.” The extent of the counseling /coordination of care must be documented. In this case, the office level visit was 99213 (Expanded problem focused exam and low medical decision making). The average time listed in the description of 99213 is 15 minutes. The report states that an additional 45 minutes was spent in counseling for a total time of 60 minutes of which, more than 50% was spent in counseling. The E/M visit is taken up to 99215 which has a time description of 40 minutes. Prolonged services can only be reported after 30 additional minutes. In this case 10 minutes remain; therefore, only report 99215. 17. C Patient was not initially admitted to the hospital. The scenario indicates the physician evaluating the patient on the following day of admission, eliminating multiple choice B. The patient is not in observation status in which she was admitted and discharged on the same date of service, eliminating multiple choice answer D. There is no request documented in the scenario for another physician to recommend care for the condition, eliminating multiple choice A. Subsequent hospital care codes require two of the three key components be met. In this case, we have detailed history and exam and low MDM which qualify for 99233. 18. B According to CPT® subsection guidelines under Initial Observation Care: When “observation status” is initiated in the course of an encounter in another site of service (example, hospital emergency department, physician’s office, nursing facility) all evaluation and management services provided by the supervising physician in conjunction with initiating “observation status” are considered part of the initial observation care when performed on the same date. Meaning you will not report an emergency service code since the patient was placed in observation care from the ER on the same date of service, eliminating multiple choice C. CPT® subsection guidelines add: Evaluation and management services on the same date provided in sites that are related to initiating “observation status” should not be reported separately. This eliminates multiple choice A. Patient was not admitted and discharged in observation status on the same date of service, eliminating multiple choice D. 19. C According to CPT® guidelines: An established patient is one who has received professional face-toface services from the physician or another physician of the same specialty who belongs to the same group practice, within the past three years. This eliminates multiple choices A and B. The documentation in the scenario provides a problem focused history (Brief HPI, No ROS, No Past, Family or Social History). The physical exam is an Expanded problem focused (Limited exam of three organ systems-Constitutional [vitals], Respiratory, and Cardiovascular). An established office visit requires at least 2 of 3 key components: Problem Focused History + Expanded Problem Focused Exam + Straightforward MDM = 99212 20. C All three key components (history, exam, and medical decision making) need to be met to qualify for a particular level of E/M service for an office visit of a new patient. According to the subsection guidelines in the CPT® manual under the heading: Instructions for Selecting a Level of E/M Service: Determine the Extent of History Obtained: (Scenario) -Extended HPI + Extended ROS + Complete PFSH = Detailed History; Determine the Extent of Examination Performed: -Extended Examination = Detailed Exam; [Detailed history + Detailed exam + Medical Decision Making of high complexity = 99203] Detailed history and exam brought the level down to code 99203. 21. A According to the CPT® subsection guidelines for Inpatient Neonatal and Pediatric Critical Care: To report critical care services provided in the outpatient setting (example, emergency department or office) for neonates and pediatric patients of any age, see the Critical Care codes 99291, 99292. This would eliminate multiple choice D. There is documentation in which the ER physician spent a total of 30 minutes on a critical patient, eliminating multiple choice C. Blood gas (82803) is a lab procedure that is not separately reported by the physician when billing for critical care. A list of services included in reporting critical care is found in the subsection guidelines under Critical Care Services. Modifier 25 needs to be appended to 99291 since it is an evaluation and management service in which billable procedures were performed on the same date of service. 22. D An established patient office visit requires 2 of the 3 key components (history, exam and medical decision making) to qualify for a particular level of E/M service. The documentation in the scenario provides: Expanded Problem Focused History = Brief history (HPI) + Problem Pertinent review of systems (ROS) + No documentation of a Past, Family, and Social history (PFSH); Expanded Problem Focused Exam =Limited two organ systems (Ears, nose, mouth and throat and Respiratory); Medical Decision Making = Moderate complexity [Expanded Problem Focused History + Expanded Problem Focused Exam + MDM Moderate = 99213] The strep culture came back positive for strep. This is indexed in the ICD-9-CM under Infection/streptococcal/sore throat guiding you to code 034.0. The second diagnosis is indexed under Otitis/media/acute/with effusion guiding you to code 381.00. 23. D. According to CPT® guidelines: Final hospital care for discharge of a patient includes final examination of the patient, discussion of the hospital stay, instructions for continuing care, and preparation of discharge records.(Final day of a multiple day stay) This code includes all the E/M services provided on the day of discharge. No other E/M code is reported with discharge codes. The patient for this encounter was admitted on one date of service and got discharged a few days after. 24. B. The patient was not referred by another physician for a second opinion for his sleep apnea, so this is not a consultation visit. The patient decided to go on his own to get the opinion from another doctor. According to CPT® guidelines: If a "consultation" is requested by a patient and/or family and not requested by a physician (self-referral), an office visit code may be used to report this service The doctor is seeing the patient for the first time, making him a new patient. In the CPT® index, look up Evaluation and Management/Office or Outpatient. You are referred to 99201-99215. Review the codes to choose the appropriate level of service. 99204 is the correct code. Comprehensive History (Extended HPI, Complete ROS, and Complete PFSH) + Comprehensive Exam + Moderate MDM (New patient to examiner; 1 data point; moderate risk) = 99204. 25. D. For this encounter the established patient is coming into a doctor’s office to get an evaluation before he goes in for surgery. In the CPT® book, look up Evaluation and Management/Office and Other Outpatient. You are referred to 99201-99215. Review codes to choose the appropriate level of service. Two out of three key components are required. The provider performs a detailed exam and moderate MDM. 99214 is the correct code. After the evaluation the patient needs the physician to address questions and concerns he has regarding the liver transplant surgery. According to CPT® guidelines: 99354-99355 are used to report the total duration of face-to-face time spent by a physician beyond the usual service in either the inpatient or outpatient setting. The prolonged service includes the time he spent in face-to-face contact with the patient when he was not performing the history, physical examination, and medical decision making related to the level of E/M service he reported. In the CPT® index, look up Prolonged Services. You are referred 99354-99357, 99360. 99354 is the correct code since 30 minutes was spent face-to-face. 26. A. The patient is in the hospital for 3 days being seen by the physician for subsequent hospital care. In the CPT® index, look up Hospital Services/Inpatient Services/Subsequent Hospital Care. You are referred to 99231-99233. Review codes to choose appropriate level of service. 99231 is the correct code. Two out of three key components are needed for subsequent hospital care codes. The physician documented a problem focused exam (1 system) + Low MDM (Established problem to examiner; stable, 2 data points, low level of risk) =99231. 27. C. The E/M service is at the request of the ED physician to render an opinion on whether the patient needs surgery. A written report of the findings is documented in the ED chart. According to CPT® coding guidelines, the requirements for a consultation have been met. The service is provided in the ED, which is an outpatient setting. The plastic surgery performs a detailed history (extended HPI, extended ROS and pertinent PFSH), a detailed exam (extended 4 body area/organ system exam) and moderate MDM (New problem to examiner no additional workup planned and need for major surgery). For an outpatient consultation three of the three key components are required. 99243 is the appropriate code. During this encounter, the physician made the decision to perform a major surgery, which is scheduled for the next day. Modifier 57 is appended to the E/M service. 28. D. During this encounter, the physician performs resuscitation, endotracheal intubation, and inserts an umbilical line. According to CPT® coding guidelines, “procedures that are performed as a necessary part of the resuscitation are reported separately in addition to 99465”. Code 99464 cannot be reported with 99465. The critically ill neonate is admitted to critical care. According to CPT® coding guidelines, 99468 can be reported with 99465. The guidelines also state “other procedures performed as a necessary part of the resuscitation are also reported separately when performed as part of the preadmission delivery room care". In this scenario the intubation (31500) and the umbilical line (36510) were performed pre-admission for resuscitation so they are both reported. Modifier 59 is required because both services are bundled with 99468 when performed during after admission. Modifier 25 is reported to indicate a separate and significant E/M service. 29. B. In the CPT® book, look up Evaluation and Management/Office or Outpatient. You are referred to 99201-99215. Review the codes to choose the appropriate level of service. 99204 is the correct code. Patient is a “new patient” since this is an initial visit. Comprehensive HPI (Extended HPI, Complete ROS, and Complete PFSH) + Comprehensive Exam (eight system exam) + Moderate MDM (New problem to examiner with additional work up planned, 1 data point (radiology), moderate level of risk (prescription) = 99204. 30. B. In this case, the ED physician performed an E/M service and moderate conscious sedation so the orthopedic surgeon could provide fracture care. The services are performed in the ED setting, which is reported with codes 99281-99285. This category requires three of three key components for the E/M code. The physician performs a detailed history (extended HPI, extended ROS and complete PFSH), detailed exam (extended six system exam), and moderate MDM (New problem to the examiner, no additional workup planned, 1 data point, moderate risk). The documentation supports a 99284. Modifier 25 is appended to the E/M service because a significant and separately identifiable E/M service is performed during the same encounter as a procedure which is the moderate conscious sedation. When coding for MCS, you need to know the age of the patient, the amount of time and whether the physician providing MCS is the same physician performing the diagnostic or therapeutic procedure for which the patient requires MCS. In this case, the ED physician is providing the MCS. He is not performing the fracture care service. The proper code is within range 99148-99150. This eliminates answer options C and D. The patient is four-years-old and the MCS is provided for 30 minutes. The correct code is 99148. 31. C. Dr. X is performing a follow-up consultation in a nursing facility. According to CPT® guidelines, “Follow-up consultations that are performed in order to complete the initial consultation (eg, certain tests results previously not available are now ready) provided in the nursing facility setting, the subsequent nursing facility care codes (99307-99310) should be reported”. In the CPT® book, look up Nursing Facility Services/Subsequent Care. You are referred to 99307-99310. Review the codes to choose appropriate level of service. In this case the physician performed a problem focused history, expanded problem focused exam (limited exam of two systems) and low MDM (Established problem stable, 3 data points (labs, EKG, consult) and low risk). In this category two of the three key components are required, 99308 is the correct code. 32. C. According to CPT® guidelines, “Critical care is the care of the unstable critically ill or unstable critically injured patient who requires constant physician attendance (the physician need not be constantly at bedside per se but is engaged in physician work directly related to the individual patient's care). The critical care codes may be reported wherever critical care services are provided. It is important to recognize that the critical care codes are reported based upon the type of care rendered not the location of where the care is rendered. The critical care codes are used to report the total duration of time spent by a physician providing constant attention to an unstable critically ill or unstable critically injured patient even if the time spent by the physician providing critical care services on that date is not continuous.” For this encounter the physician was called to the floor to evaluate a critically ill patient. The keywords to look for are the statement “total critical care time,” to indicate a critical care service. In the CPT® book, look up Evaluation Management/Critical Care. You are referred to codes 99291-99292. Review codes to choose appropriate level of service. The physician documents 48 minutes of critical care time which is reported with 99291.