Anatomy and Physiology - Unsri
advertisement

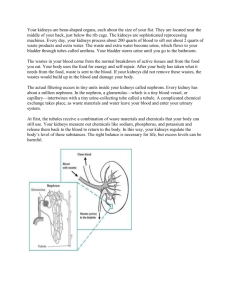
Anatomy and Physiology dear d34r123@yahoo.co.id KOMUNITAS BLOGGER UNIVERSITAS SRIWIJAYA Anatomy and Physiology The Human Renal System The human renal system is made up of two kidneys, two ureters, the urinary bladder, and the urethra. In addition to the production of urine the renal system has many other functions. One quarter to one fifth of cardiac output passes through the kidneys at all times. This means that the kidneys filter approximately 1.2 liters of blood every minute. It is therefore not surprising that even slight abnormalities of renal function quickly lead to electrolyte disturbances. If untreated death will occur. The Kidneys The kidneys are two bean shaped organs of the renal system located on the posterior wall of the abdomen one on each side of the vertebral column at the level of the twelfth rib. The left kidney is slightly higher than the right. Why do you think that the right kidney is lower than the left? (Q1). Human kidneys are richly supplied with blood vessels which give them their reddish brown color. The kidneys measure about 10cm in length and, 5cm in breadth and about 2.5 cm in thickness. The kidneys are protected by three highly specialized layers of protective tissues. The outer layer consists mainly of connective tissue which protects the kidneys from trauma and infection. This layer is often called the renal fascia or fibrous membrane. The technical name for this layer is the renal capsule. The next layer (second layer from the exterior) is called the fascia and it makes a fibrous capsule around the kidneys. This layer connects the kidneys to the abdominal wall. The inner most layer is made up of adipose tissue and is essentially a layer of fatty tissue which forms a protective cushions the kidney; and the renal capsule (fibrous sac) surrounds the kidney and protects it from trauma and infection. Blood and Nerve Supply The kidneys receive their oxygenated blood supply from the renal arteries which come off the abdominal portion of the aorta. Venous blood from the kidneys drains into the renal veins to join the abdominal portion of the inferior vena cava. The hilum of the kidneys is located toward the smaller curvature. The opening in the hilum allows for the entry and exit of blood vessels and nerves. The funnel shaped extension of the kidneys is called the renal pelvis and it connects the kidneys to the two ureters. This structure facilitates the collection of the urine from the kidneys and drainage to the urinary bladder. The ureters are tubes that are 25-30cm long and lined with smooth muscle. These tubes help carry urine to the bladder. The muscular tissue helps force urine downwards. They enter the bladder at an angle, so urine doesn’t flow up the wrong way. The functional parts of the kidneys are divided into two distinct regions. The outer region is reddish brown in color and is called the renal cortex. This is where the nephrons of the kidney are located. The inner layer of the kidney is more pinkish in color and is called the renal medulla. The renal cortex houses the functional units of the kidneys called nephrons. The inner area of the kidneys is supplied by a small blood vessel network called the vasa recta. The Nephron The nephron is a functional part of the kidneys. The Glomerulus is a collection of capillaries which are surrounded by the Bowman’s capsule. The afferent arteriole enters this capsule and the efferent arteriole leaves it. In the glomerulus the blood pressue is high and it pushes small structured molecules out (water, salts, glucose and urea). However larger molecules (Proteins and glycogen) stay within the capillary network. The particles which are pushed out with water (filtrate) enter the proximal convoluted tubule. This portion is convoluted and broad. The following portion is straight and narrow; hence it is called the straight collecting tubule, also referred to as the Loop of Henle. This portion is located in the Renal medulla. The collecting tubule upon re-entry into the renal cortex passes by the efferent arteriole. The macula densa is the final part of the ascending collecting tubule very closely. The filtrate is selectively reabsorbed in the distal broad convoluted and the proximal narrow straight tubules. Water and salts are reabsorbed in the Loop of Henle. Urine concentration occurs here. Proximal tubule is broad and convoluted. It is located in the renal cortex. Distal tubule is narrow and straight. It forms the Loop of Henle and is located in the renal medulla. When the filtrate arrives in the distal tubule water is reabsorbed. However, hydrogen ions, ammonia, histamines, and certain antibiotics are excreted into the distal tubule. This process is selective and involves the expansion of energy i.e. ATP is used up. It is called tubular excretion. Question 2. How is this process different from osmosis and diffusion? For more details about nephrons please read the set text. The following Website also contains useful information and practice exercises. The Urinary Bladder The urinary bladder is located midline in the abdominal pelvis. It is a pyramid shaped muscular organ. The main function of the bladder is to collect and store urine. The stored urine will be excreted through the urethra when the controlling sphincters are relaxed after receiving signals from the brain. In men the urethra is much longer, is surrounded by the prostate gland and the enlargement of this gland can cause problems with the excretion of urine. The normal bladder can hold up to 500 mls of urine. In patients with urinary retention the bladder may be larger. The bladder has three openings, two ureteral openings to receive urine from the kidneys and one urethral opening to drain the urine. These openings form the trigone of the bladder. This area is smooth and triangular shaped. The trigone is sensitive to expansion (stretch) which occurs as the bladder fills with urine. When stretched to a certain degree, the urinary bladder signals the brain to empty its contents. When there are problems with the control or sphincter muscles the patient many experience urinary incontinence. As the bladder fills more the signals become more intense. The smooth muscle of the bladder is called the detrusor muscle. The urethral sphincter at the base of the bladder consists of ring like muscles which facilitate its opening and closing. When the bladder is full stretch receptors in the bladder send signals to the brain. When the brain receives these signals (indicating that the bladder is full) the sphincter relaxes and urination occurs. For urination to occur the detrusor muscle must contract and the urethral sphincter muscle must relax at the same time. The detrusor muscle is unique in the sense that it is capable of distension to accept large quantities or urine without increasing the internal pressure. This allows much larger volumes of fluids to be collected in the bladder (700 to 1000ml) without causing back pressure and damage to the kidneys. The urinary bladder is supplied with arteries to supply oxygenated blood vessels. The common arteries which supply the bladder are the vesical, the obturator, uterine, gluteal and vaginal arteries. A venous network drains the blood to the abdominal iliac vein. The voluntary muscles of the bladder are under the control of the Central Nervous system. The controls are located in the brain (voluntary) and in the spinal cord (involuntary). The Urethra The urethra is a tube like organ which drains urine from the bladder to the exterior. It is lined with endothelium and surrounded by involuntary muscles. In females it is about 5 to 6 cm long. Generally it is 6mm wide in healthy patients. In males it is 15 to 22 cm long. It begins at the base of the bladder and extends to the tip of the penis. Since the female urethra is shorter and located close to the vagina it is subjected to frequent urinary tract infections. The internal pudendal and vaginal arteries supply arterial blood to the urethra in females. In males the blood supply is slightly different. The inferior vesical and middle rectal arteries supply the bulk or arterial blood. The veinous return follow these blood vessels. Nerve innervation: he pudendal nerve. Functions of the Renal System The renal system has many functions. The following are the best known. Each is discussed under a separate subtitle because the functions are varied and complex: 1. Excretion of urea, a by product of protein metabolism 2. Regulations of the amount of water which stays in the body 3. Kidneys maintain the pH balance of the human body 4. Produce EPO hormone which has a role in the production of Red blood cells and s like 5. Produce the enzyme rennin. This enzyme has a role in the maintenance of blood pressure. a. Urine production and b. water regulation: These are important functions of the different parts of the nephrons. They filter blood of its small molecules and ions and make urine. During this process it reclaims useful minerals and sugars. In one day (24hrs) the kidneys reclaim 1,300 g of NaCl, 400 g of NaHCO3 and 180 g of glucose and 180 liters of water. These are the constituents which entered the tubules during the filtration process. c. Maintain pH value of human body: The human body is designed to function optimally at a pH value of 7.35 to 7.45. Death will occur if pH drops below 6.8 or rises above 7.8. It is for this reason that pH values are checked frequently during acute illnesses. pH is maintained by buffers dissolved in the blood. However, the kidneys and the lungs play a vital role in removing the H+ ion from the body. Metabolic Acidosis occurs when the kidneys fail to remove the H+ ions. Respiratory acidosis occurs when the lungs fail to remove the excess of CO2 from circulation. Question 3: Why does exercise generate H+? Question 4: How can H+ generated in muscle cells during exercise affect the pH of the blood throughout the body? d. Hormone production: Kidneys produce two hormones known as erythropoietin (EPO), and calcitriol. They also produce the enzyme known as rennin. Erythropoietin (EPO): Is a hormone which is produced by the kidneys. It is needed in the bone marrow for the formation of red blood cells. Chemically EPO is a glycoprotein with a molecular weight of 34,000. A glycoprotein is a protein with an attached sugar molecule. Highly specialized cells of the kidney which are sensitive to low oxygen levels in the blood produce EPO. The EPO subsequently stimulates the bone marrow to produce RBCs to increase O2 carrying capacity. This also leads to greater production of hb. Hb is the molecule which facilitates the transport of oxygen by the cardiovascular system. The EPO gene is located on chromosome 7, band 7q21. Some EPO is also produced in the liver. Normal levels of EPO are 0 to 19mU/ml (milliunits per milliliter). Elevated levels of EPO indicate polycythemia. Lower levels are seen in chronic renal failure. EPO is often prescribed to Renal Failure Patients. Kidneys have a role in the manufacture of vitamin D (Calcitriol) * Calcitriol is 1,25[OH]2 = Vitamin D3, the active form of vitamin D. * Vitamin D3 (Cholecalciferol): Is synthesized in skin when it is exposed to sunlight. * Vitamin D2 (Ergocalciferol) is a synthetic vitamid D derivative * Both vitamin D2 and D3 are hydroxylated in the kidneys into Calcitriol. Vitamin D regulates Calcium and Phosphorus levels in blood by promoting their absorption from the food in the intestines and promoting re absorption of Calcium in the kidneys. Deficiency Disorders: Insufficient calcitriol prevents normal deposition of calcium in bone. In childhood, this produces the deformed bones characteristic of rickets. In adults, it produces weakened bones causing osteomalacia. The commonest causes for vitamin D deficiency are inadequate dietary intake and insufficient exposure to the sun. A rare inherited mutant gene also interferes with the production of the enzyme which converts 25[OH] vitamin D3 into calcitriol. Some inherited rickets are also caused by two defective genes for the calcitriol receptor. e. Renin : Is an enzyme which is in the juxtaglomerular cells of the juxaglomerualr apparatus of the renal system. This occurs when: a. the circulating blood volume is low or b. or serum NaCl concentrarion is low. Overproduction causes hypertension and underproduction causes hypotension. Sympathetic stimulation of Beta 1 and Alpha 1 adrenergic receptors on the JGA cells also bring about the production of renin. Normal concentration is 1.0 to 2.5 mg/ml. * Answer to Question 1 : This positional difference is due to the presence of the liver in the right side. The liver pushes the right kidney down. * Answer to question 2: Osmosis and Diffusion are passive processes. There is no expenditure of energy because the movement of water and particles occurs to balance out the gradient which existed. Once a state of equilibrium is reached there will be no net movement of water or any other particles. * Answer to Question 3: During exercise muscles use the energy stored in glucose. The oxygen is obtained from the oxyhaemoglobin, As the result of this interaction CO2 and H+ ions are produced. * Answer to Question 4: How can H+ generated in muscle cells during exercise affect the pH of the blood throughout the body? Kidneys ultimately remove H+ ions from the body. During exercise H+ ions are produced. If they are not removed Metabolic Acidosis will occur. The lungs are able to get rid of the H+ ions more quickly so they are more effective in getting rid of the H+ ions. Kidney Disease (Data are for the U.S.) Morbidity * Number of noninstitutionalized adults with diagnosed kidney disease: 3.7 million * Percent of noninstitutionalized adults with diagnosed kidney disease: 1.7% Source: Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2008, tables 7, 8 Mortality * Number of deaths from nephritis, nephrotic syndrome, and nephrosis: 45,344 * Deaths per 100,000 population: 15.1 * Cause of death rank: 9 Source: Deaths: Final Data for 2006, table B More Data * Search Tables for Kidney in Health Data Interactive Related Links * National Health Interview Survey * Mortality data * National Center for Chronic Disease Prevention and Health Promotion * National Institute of Diabetes and Digestive and Kidney Diseases Reference: http://www.cdc.gov/nchs/fastats/kidbladd.htm http://healthmad.com/healthcare-industry/kidney-anatomy-and-physiology/ DOWNLOAD