Murmur Evaluation Curriculum
advertisement

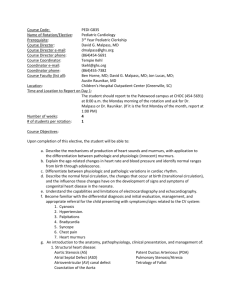
TeJosh Daily The Evaluation of Murmurs by Pediatric Residents Step 1: Problem Identification and General Needs Assessment Problem Identification In the United States, the incidence of moderate and severe forms of congenital heart disease(CHD) is 6 per 1,000 live births and incidence of all forms of CHD is 75 per 1,000 live births if trivial lesions such as small muscular ventricular septal defects are included (1). The diagnosis of CHD is often made by pediatric cardiologist following referral by general pediatricians, and the evaluation of a new murmur is the most common reason for referral to the pediatric cardiologist (2,3). It is estimated that up to 80% of children have heart murmurs, but only 0.35% have confirmed organic heart disease (3-5). Therefore, pediatricians must be competent at cardiac auscultation to screen these patients appropriately and costeffectively, while not overlooking those with serious structural defects. If pediatricians do not recognize pathologic murmurs, then heart disease remains undiagnosed and untreated which results in both morbidity and mortality. If pediatricians make inaccurate diagnosis and frequently refer innocent murmurs to specialists, then a significant financial burden is placed on the health care system, and the family suffers from undue patient and parental anxiety and psychological labeling when incorrectly labeling a child with an innocent murmur as having heart disease (6). Bergman studied this phenomenon of inappropriate referrals of innocent murmurs and concluded that the degree of disability from labeling healthy children with “cardiac disease” by pediatricians was greater than that caused by actual heart disease (7). Current Approach Currently, pediatricians complete four years of medical school followed by three years of pediatric residency prior to practicing independently. The primary training regarding the auscultation of murmurs is expected to occur during pediatric residency. Pediatric residents may spend time on a pediatric Cardiology rotation, but it is currently not required by the Accreditation Council for Graduate Medical Education (ACGME). The skill of auscultating murmurs is expected to be developed during the residency through the process of providing clinical care with supervision and participating in didactic educational activities which are primarily lectures. Unfortunately, the current approach to learning auscultation skills is inadequate, and the diagnostic accuracy of clinical assessment of heart murmurs by both pediatric residents and office based pediatricians is poor (8-11). In one study, one fifth of pathologic murmurs were missed by pediatric residents and most murmurs that were indicated as pathologic were actually innocent (11). Additionally, echocardiograms ordered by pediatricians without the consultation of a pediatric cardiologist have a very low likelihood of identifying cardiac disease (12) highlighting the gap in auscultation ability of pediatricians. In contrast, pediatric cardiologists can differentiate innocent from pathologic murmurs based on clinical exam with high specificity and sensitivity (2,13,14). However, given the prevalence of murmurs among children, the evaluation of each child who has a murmur by a pediatric cardiologist would not be cost-effective. Residency programs often try to address this gap in auscultation ability by encouraging or requiring pediatric residents to rotate in outpatient pediatric Cardiology clinic, but participation in an outpatient Cardiology clinic alone does not further improve auscultation skills(11). Ideal Approach An ideal curriculum would help pediatric residents learn to effectively evaluate murmurs in children and to accurately determine when to consult a pediatric cardiologist. The 6 cardinal signs of murmur pathology described by McCrindle et al (3) could serve as a framework so that the truly important ausculatory findings are stressed in the limited amount of time allowed for Cardiology teaching during residency. The 6 cardinal signs of murmur pathology are pansystolic murmur, murmur intensity ≥ grade 3, maximal intensity of murmur at left upper sternal border, harsh quality of a murmur, presence of an early/ midsystolic click, and presence of an abnormal S2 (3). Effective published curriculum should be reviewed and emulated where appropriate. The results from the literature are somewhat heterogeneous. Classroom based teaching, lead by a cardiologist who presents each case with audio recordings of murmurs and leads the discussion, has been shown to be effective at improving skills in auscultation (15). Additionally, a patient-centered teaching conference has been shown to be an effective method for improving cardiac ausculatory skills and diagnostic proficiency (16). Some data suggests that self-directed cardiac auscultation programs are more effective than traditional didactic approaches. Specifically, the auscultation skills of pediatric residents have been shown to improve after the use of a self-directed cardiac auscultation teaching program (11), and the auscultation skills of family practitioners have been shown to improve with the use of interactive CD-ROM (17). It has also been suggested that instead of focusing on the correct diagnosis, the focus of assessing auscultation skills should be on patient outcomes (10,18). In other words, identifying whether the murmur is due to aortic stenosis or mitral regurgitation is not as important as distinguishing whether a murmur is pathologic or benign since a pediatrician doesn’t have to determine the final diagnosis, just whether to refer to pediatric Cardiology or not. Classroom based teaching employing learner participation and review of murmurs should be coupled with a self-directed cardiac auscultation program to both provide a framework for evaluating murmurs and allow pediatric residents the opportunity to hear many different murmurs, make an assessment, and then immediately compare their assessment to the correct one. Additionally pediatric residents should all have the opportunity to rotate in an outpatient pediatric Cardiology clinic. The combination of classroom based teaching, self-directed auscultation programs, and rotation in a Cardiology clinic should serve as the framework for a murmur evaluation curriculum. Step 2: Targeted Needs Assessment Targeted Learners The targeted learners for this curriculum are categorical pediatric residents at Cincinnati Children’s Hospital Medical Center (CCHMC). This group was selected for several reasons. Approximately 40% of pediatric residents in the United States intend to become general pediatricians(19). In the United States, general pediatricians are primarily responsible for the initial evaluation of murmurs in children. A much smaller percentage of medical students choose general pediatrics as a career so targeting medical students would not be as impactful. While targeting general pediatricians may be impactful, it would be very difficult to design a curriculum that would have a high level of participation from this group. In contrast, a murmur evaluation curriculum could be incorporated into the pediatric residency curriculum and be assimilated into lectures, clinical rotations, and online modules completed during night shifts. Targeted Environment At CCHMC, pediatric residents have intense exposure to a variety of clinical rotations throughout their three years. They attend conferences regularly, have a weekly general pediatric clinic, experience intensive rotations on specific subspecialty services including Cardiology, and complete on-line educational modules during night shifts. Given the structure of the residency program and the educational benefit of exposure to the topic multiple times over the entirety of the three years, a longitudinal experience would be ideal. Needs Assessment Pediatric residents are enmeshed in a complex medical system with tension created by an explosion in new medical knowledge and technology, a substantial increase in the acuity and complexity of illnesses in hospitalized children, an emphasis on quality and safety of medical care, and restricted duty hours (20). In the midst of all these changes, the length of pediatric residency (3 years) has remained the same which makes learning what is necessary to become competent pediatricians difficult. Learning to accurately assess murmurs in children is simply one skill among many that must be learned in a limited period of time. For this reason and likely others, the auscultation skills of pediatric residents is poor(11). Currently the evaluation of murmurs is not taught at CCHMC in a rigorous way. One lecture is given yearly during a noon conference which is only attended by the pediatric residents on rotations that allow them to attend (less than half of the pediatric residents attend on a given day). Approximately half of the pediatric residents spend time on a Cardiology rotation during their 3 years (this may be decreasing further in the next couple of years). Residents on the inpatient Cardiology rotation receive one lecture on the evaluation of murmurs and otherwise spend most of their time taking care of children with cardiac disease on the inpatient service. Some teaching may be provided at the bedside regarding physical exam skills, but this varies by attending cardiologist. Eager residents may have the opportunity to spend some time in an outpatient clinic which affords them the opportunity to evaluate children referred for murmurs. Additionally, residents have the opportunity to choose a 2 or 4 week outpatient Cardiology elective, but most do not make this selection. No study of auscultation ability has been performed among residents at CCHMC, but given the similarity of the CCHMC residency program to other pediatric residency programs in terms of structure, it is reasonable to expect CCHMC pediatric residents have similar gaps in auscultation ability. It is also not known what perspectives pediatric residents at CCHMC currently have regarding the training they receive and their confidence in their ability to evaluate murmurs. Other important information to gather are perceived barriers to learning how to evaluate murmurs, desire for more training regarding the evaluation of murmurs, desired content, willingness to complete on-line modules, and perspective of the usefulness of rotations in the outpatient Cardiology clinic. Questionnaire To answer the questions posed above, a questionnaire should be developed and distributed to pediatric residents at CCHMC. First initial qualitative data should be gathered through in-person informal discussions with pediatric residents. Based in part on the initial informal discussions, an on-line survey will be created. The sample population will consist of all pediatric residents at CCHMC. The survey design will be cross-sectional. The questionnaire will be developed and administered through Qualtrics (21) which will allow administration through email. The questionnaire will be designed to be completed in less than 5 minutes. The pediatric residents will be notified of the survey, its purpose, what their responses will be used for, that the responses will be confidential, and the time needed to complete the questionnaire. Prior to the administration of the questionnaire, a pilot study will be performed with a small selection of pediatric residents to assure clarity and understandability of the questionnaire. A survey methodologist at CCHMC will be employed in the development of the survey and the Question Appraisal System will be utilized to assure the quality of the questions (22). The following questions are examples of the questions that will likely be included in the survey. 1. Are you currently a 1st, 2nd, or 3rd year pediatric resident? 2. How many lectures have you attended in which the auscultation of murmurs in children was taught? 3. Have you rotated on the inpatient Cardiology service? If you answer no, then please skip to question #5. 4. During your rotation on the inpatient Cardiology service, how would you describe your satisfaction with the education you received regarding the evaluation of murmurs in children? not at all satisfied, slightly satisfied, moderately satisfied, very satisfied, extremely satisfied 5. Have you rotated on the outpatient Cardiology clinic? If you answer no, then please skip to question #7. yes or no 6. During your rotation in the outpatient Cardiology clinic, how would you describe your satisfaction with the education you received regarding the evaluation of murmurs in children? not at all satisfied, slightly satisfied, moderately satisfied, very satisfied, extremely satisfied 7. During your residency so far, how would you describe your satisfaction with the education you received regarding the evaluation of murmurs in children? not at all satisfied, slightly satisfied, moderately satisfied, very satisfied, extremely satisfied 8. How would you describe your ability to accurately assess whether a murmur in a child is benign or pathologic? Poor, fair, good, very good, excellent 9. What are some of the barriers that limit pediatric residents from learning important auscultation skills? 10. Describe your support for the incorporation of an on-line module reviewing heart murmurs into the night shift curriculum? strongly oppose, somewhat oppose, neutral, somewhat favor, strongly favor 11. What changes do you think should be made with regard to the education provided to pediatric residents on the evaluation of murmurs in children? Step 3: Goals and Objectives Goals The overarching goal of the curriculum is for all pediatric residents at Cincinnati Children’s Hospital Medical Center to develop the knowledge, attitudes, and skills required to effectively evaluate and develop appropriate management plans for murmurs in children. Objectives Cognitive Objectives: Individual Level: By the end of residency, each pediatric resident will: have achieved cognitive proficiency in the diagnosis and management of murmurs as measured by acceptable scores on the pediatric in-service examination administered during their last year of training. be able to identify the six cardinal signs of murmur pathology(3) as measured on an online quiz administered at the end of residency. be able to accurately determine whether children with murmurs should be referred to Cardiology as measured by a score of greater than 80% correct on an online quiz administered at the end of residency. Aggregate Level: At the end of each year, greater than 80% of graduating pediatric residents will: have achieved cognitive proficiency in the diagnosis and management of murmurs as measured by acceptable scores on the pediatric in-service examination administered during their last year of training. be able to identify the six cardinal signs of murmur pathology(3) as measured on an online quiz administered at the end of residency. be able to accurately determine whether children with murmurs should be referred to Cardiology as measured by a score of greater than 80% correct on an online quiz administered at the end of residency. Affective Objectives: Individual Level: By the end of residency, each pediatric resident will: rank the effective evaluation of murmurs as important for pediatricians as evidenced by >or = 3 on a 4-point scale on an online quiz administered at the end of residency. Aggregate Level: At the end of each year, greater than 80% of graduating pediatric residents will rank the effective evaluation of murmurs as important for pediatricians as evidenced by >or = 3 on a 4-point scale on an online quiz administered at the end of residency. Psychomotor Objectives: Individual Level: By the end of residency, each pediatric resident will: have demonstrated to a Cardiology faculty at least once the proper techniques of auscultation including listening over the aortic valve, the pulmonary valve, the tricuspid valve, and the mitral valve in the supine, sitting, and standing position, palpation of femoral pulses, and palpation for hepatomegaly. Aggregate Level: At the end of each year, greater than 80% of graduating pediatric residents will: have demonstrated to a Cardiology faculty at least once the proper techniques of auscultation including listening over the aortic valve, the pulmonary valve, the tricuspid valve, and the mitral valve in the supine, sitting, and standing position, palpation of femoral pulses, and palpation for hepatomegaly. Process Objectives: Individual Level: By the end of residency, each pediatric resident will: have evaluated at least five patients in Cardiology clinic who have been referred for the evaluation of a murmur. have attended at least one interactive lecture given by a cardiologist on the evaluation of children with murmurs. have completed an online module on the evaluation of children with murmurs. Aggregate Level: At the end of each year, greater than 80% of graduating pediatric residents will: have evaluated at least five patients in Cardiology clinic who have been referred for the evaluation of a murmur. have attended at least one interactive lecture given by a cardiologist on the evaluation of children with murmurs. have completed an online module on the evaluation of children with murmurs. Step 4: Educational Strategies The educational strategies are based on the ideal approach as identified in Step 1: Problem Identification and General Needs Assessment. Educational methods are selected to be congruent with the educational goals and objectives. Given the structure of the pediatric residency program at CCHMC and the educational benefit of exposure to the topic multiple times over the entirety of the three years, a longitudinal experience is ideal. This longitudinal experience will include clinical experience in outpatient and inpatient pediatric cardiology, participation in an internet module during night float, and a series of lectures/discussions lead by a pediatric cardiologist. Clinical Experience Each pediatric resident will be required to participate in a week long rotation in the outpatient Cardiology clinic at CCHMC. Each day they will be paired with a different pediatric cardiologist preceptor. They will be expected to see all children with new referrals for heart murmurs in their preceptor’s clinic, to independently see and evaluate each patient, to present their assessment and plan to the attending cardiologist, and then to accompany the cardiologist as he/she evaluates each patient. Additionally, there will be a morning Cardiology clinic (“intern clinic) each Friday morning for interns on the inpatient Cardiology rotation. All interns who rotate on the inpatient Cardiology will participate in this clinic. Each Friday morning, the senior pediatric residents on the Cardiology rotation and the nurse practitioners will round on the patients admitted to the Cardiology service so that the interns will be excused to participate in this clinic. This clinic will consist entirely of new referrals including murmurs, chest pain, and syncope. Two patients will be scheduled each hour to allow ample time for teaching. In keeping with importance of patient outcomes instead of patient diagnosis, the focus of the teaching will be placed on differentiating benign from pathologic murmurs (10,18). Internet Modules During one rotation on night float each year, each pediatric resident will be expected to complete an online interactive module on the evaluation of children with murmurs (11,17). The module will consist of listening to murmurs, making a decision about whether the murmurs are benign or pathologic, and then receiving immediate feedback regarding the correct diagnosis. Additionally, the module will explain which of 6 cardinal signs of murmur pathology as described by McCrindle et al (3) are present in each pathologic murmur. Residents will complete this online module each year during a specific night float rotation, so that by the time they graduate they will have completed it 3 times. Lectures/ Discussions Each year two 50 minute lectures/discussions will be held during noon conference (one in the Spring and the other in the Fall). The lectures will consist of a 10-minute presentation focused on determining when to consult a pediatric cardiologist for a murmur in a child. The 6 cardinal signs of murmur pathology described by McCrindle et al (3) will serve as the framework for this presentation. The 6 cardinal signs of murmur pathology are pansystolic murmur, murmur intensity ≥ grade 3, maximal intensity of murmur at left upper sternal border, harsh quality of a murmur, presence of an early/ midsystolic click, and presence of an abnormal S2 (3). This information will be presented in lecture format utilizing a Powerpoint presentation during the first 10-15 minutes in keeping with the Primacyrecency effect in order to most effectively utilize Prime-time 1 (23). The remainder of the time will be spent reviewing audio recordings of murmurs followed by brief discussions of the features of the murmur lead by the cardiologist. The same lecture/discussion will be repeated twice yearly, so that by the end of residency each pediatric resident will potentially have heard it six times (but more likely 2-3 times). Step 5: Implementation Resources: Implementation of this curriculum will primarily require resources in the form of personnel. Faculty: Faculty participation and leadership are crucial for success of this curriculum. Since it is a longitudinal experience involving multiple educational strategies, the director of resident Cardiology education at CCHMC will take primary responsibility for leadership. He/she will be responsible for curriculum development and maintenance, oversight of didactic content, clinical operations, and coordination. He/she will need to identify and recruit faculty within the section of Cardiology to develop and facilitate the lectures/discussions, develop the online module, and precept residents in outpatient Cardiology clinic. Support of 0.1 full time employee (FTE) should be awarded to the director. Cardiology faculty including the director of resident cardiology education will provide the backbone of teaching in outpatient Cardiology clinic and during the lectures/discussions. A single faculty member with an interest and expertise in teaching will facilitate the twice yearly lecture/discussions. A small group of four Cardiology faculty who also have an interest and expertise in teaching will precept the weekly “intern clinic.” One of the preceptors should be the director of resident Cardiology education. All Cardiologists who participate in general outpatient Cardiology clinic will serve as preceptors for residents rotating on a Cardiology elective. Given the content of the curriculum (evaluating murmurs) and the expertise of the faculty members, no specialized training will be needed for faculty members. Support Staff: Support staff are critical to the smooth operation of this curriculum. A 0.25 FTE administrative assistant will serve as the coordinator for residents rotating on both the inpatient and outpatient Cardiology rotations. Patients: Children referred to Cardiology for the evaluation of murmurs will be needed. Given current patient Cardiology volumes and referral patterns at CCHMC, this should not be an issue. Facilities and Equipment: Our faculty space needs and equipment will not be costly. The resident lecture conference room will be utilized for the six lectures/discussions. The Cardiology clinic space will serve as the location for evaluating in outpatient Cardiology clinic. Online Learning: We will need to develop Internet modules that will be delivered with institutional content management software (Blackboard). A reservoir of audio recordings of specific murmurs that has already been collected by CCHMC faculty will be utilized by the faculty to create brief clinical vignettes with accompanying audio recordings of murmurs. The director of resident Cardiology education will be responsible for developing and maintaining these internet modules. Support: Internal funding support will come from the section of Pediatric Cardiology at CCHMC. Given the limited cost of this curriculum, no external funding is needed. Barriers: Curricular Time: Securing time for the clinical experiences, lectures/ discussions, and participation in internet modules during pediatric residency will be the most significant barrier. Residents at CCHMC already have daily noon conference lectures with multiple openings so incorporating two lectures per year will not be difficult. Residents are already required to complete specific educational activities while on night float, so incorporating the internet module into these activities, in which there is already an expectation for completion, should be met with minimal resistance. The primary barrier will likely be in providing time for the clinical experiences. As previously described inpatient Cardiology coverage for interns rotating on the Cardiology service will be arranged for a half day each week. Two-week outpatient Cardiology electives will be provided and will meet the ACGME requirements for subspecialty electives during pediatric residency. Significant support will need to be garnered from the pediatric residency leadership to make this two week elective a required rotation. Faculty Resources and Recruitment: As previously stated, only a few select Cardiology faculty will need to provide leadership and significant participation for the curriculum to succeed. Within a large Cardiology faculty (greater than 40 Pediatric Cardiologists) at an academic center recruiting four faculty members who are committed to teaching and willing to participate is not expected to be difficult. Introduction: The curriculum will be incorporated starting July 1, 1015. Given the nature of the curriculum and similarity to current resident Cardiology education, pilot testing will not be necessary. After the curriculum has been implemented, feedback from residents will be elicited by questionnaire from all residents completing rotations on inpatient and outpatient Cardiology services and all graduating residents. Step 6: Evaluation and Feedback: Evaluation will be kept simple. Data collection will be integrated into the curriculum schedule. The major goals of the evaluation are to provide formative information that the residents can use to achieve curricular objectives and that the faculty can use to monitor the quality of and improve the curriculum. Users: Pediatric residents, Cardiology faculty, and Residency program director and assistant directors. Uses: Formative information to help residents achieve learning objectives; Summative information for residents to assess their ability to assess murmurs at the conclusion of their residency, formative information for the director of resident Cardiology education and faculty to guide improvement of curriculum; summative information for the director of resident Cardiology education and residency program director and co-directors on resident performance and program effectiveness. Resources: The director of resident Cardiology education, Cardiology faculty, and administrative support as described in Step 5. No additional funding. Evaluation Questions: What percentage of residents score greater than 80% on an online quiz administered at the end of residency? What percentage of residents will identify the six cardinal signs of murmur pathology (3) as measured on an online quiz administered at the end of residency? What percentage of residents will rank the effective evaluation of murmurs as important for pediatricians as evidenced by >or = 3 on a 4-point scale on an online quiz administered at the end of residency? What percentage of residents will have achieved acceptable scores on the pediatric in-service examination administered during their last year of training? What percentage of residents will have demonstrated to a Cardiology faculty at least once the proper techniques of auscultation including listening over the aortic valve, the pulmonary valve, the tricuspid valve, and the mitral valve in the supine, sitting, and standing position, palpation of femoral pulses, and palpation for hepatomegaly? What percentage of residents will have evaluated at least five patients in Cardiology clinic who have been referred for the evaluation of a murmur? What percentage of residents will have attended at least one of the interactive lectures? What percentage of residents will have completed the online module on the evaluation of children with murmurs? What are the strengths of the curriculum? What are its weaknesses? How can it be improved? Evaluation design: Pre- and posttest design (O1…X…O2) will be used for the online quiz. The remainder of the learner and program evaluations will be posttest only (X…O). Evaluation Methods and Instruments: Learner Evaluations: Participation Passport: The clinical portion of this course is experiential in nature. A participation passport will help to ensure that each student evaluates at least five children with murmurs in Cardiology clinic and has demonstrated an adequate cardiac physical exam to a pediatric cardiologist. Internet Quiz: We plan a pre-quiz at the beginning of residency and a post-quiz at the end of residency. In addition to the assessment of knowledge by the quiz we will also assess attitude toward the importance of the accurate evaluation of murmurs by pediatricians with an additional Likert style question. Learners will also be asked how many of the murmur lectures that they attended. Pediatric In-service Exam: We plan to analyze the results for the Cardiology questions on obtained during the third year of residency. Program Evaluations: End of Residency: Standardized curriculum evaluation forms will be used for formative and summative program evaluation. These will be administered electronically with the on-line quiz. The form will elicit residents’ ratings of adequacy of the rotation, whether they would recommend the curriculum to others, and written comments on curriculum strengths, weaknesses, and suggestions for improvement. Feedback Session: At the conclusion of each resident’s outpatient Cardiology elective rotation, we will ask for verbal feedback regarding aspects of the rotation that could be improved. Passports: These will be collected at the conclusion of each resident’s outpatient Cardiology elective rotation to be used for quantitative assessment of student experiences. Ethical Concerns: End-of-curriculum evaluation forms will be completed by residents anonymously to promote uninhibited ratings and comments and to protect residents against any retaliation for unflattering ratings or comments. Data Collection: The end of curriculum quiz and evaluation forms will be administered online through email invitations during the last 3 months of residency. If residents do not complete the online quiz than two reminder emails will be sent. Notes from the feedback sessions and passports will be collected by the director of resident Cardiology education at the end of the outpatient Cardiology elective rotation. Data Analysis: Descriptive statistics will be performed on the pre-post quiz data for formative and summative evaluation. Reporting of Results: Collated evaluation results, with simple descriptive statistics, will be compiled and distributed yearly to the Cardiology faculty and residency program directors and co-directors. The description of the curriculum and associated results will be reported in manuscript form and submitted to a peer-reviewed journal for publication. References: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. Hoffman JI, Kaplan S. The incidence of congenital heart disease. Journal of the American College of Cardiology 2002;39:1890-1900. Smythe JF, Teixeira OH, Vlad P, Demers PP, Feldman W. Initial evaluation of heart murmurs: are laboratory tests necessary? Pediatrics 1990;86:497-500. McCrindle BW, Shaffer KM, Kan JS, Zahka KG, Rowe SA, Kidd L. Cardinal clinical signs in the differentiation of heart murmurs in children. Archives of pediatrics & adolescent medicine 1996;150:169-174. Fogel D. The innocent systolic murmur in children: a clinical study of its incidence and characteristics. American heart journal 1960;59:844-855. Freedom RM, Benson LN, Smallhorn JF. Neonatal heart disease: Springer-Verlag Berlin, Heidelberg, New York, 1992. McCrindle BW, Shaffer KM, Kan JS, Zahka KG, Rowe SA, Kidd L. An evaluation of parental concerns and misperceptions about heart murmurs. Clinical pediatrics 1995;34:25-31. Bergman AB, Stamm SJ. The morbidity of cardiac nondisease in schoolchildren. New England Journal of Medicine 1967;276:1008-1013. Haney I, Ipp M, Feldman W, McCrindle BW. Accuracy of clinical assessment of heart murmurs by office based (general practice) paediatricians. Archives of disease in childhood 1999;81:409-412. Gaskin PR, Owens SE, Talner NS, Sanders SP, Li JS. Clinical auscultation skills in pediatric residents. Pediatrics 2000;105:1184-1187. Kumar K, Thompson WR. Evaluation of cardiac auscultation skills in pediatric residents. Clinical pediatrics 2012:0009922812466584. Mahnke CB, Nowalk A, Hofkosh D, Zuberbuhler JR, Law YM. Comparison of two educational interventions on pediatric resident auscultation skills. Pediatrics 2004;113:1331-1335. Kwiatkowski D, Wang Y, Cnota J. The utility of outpatient echocardiography for evaluation of asymptomatic murmurs in children. Congenital heart disease 2012;7:283-288. Newburger JW, Rosenthal A, Williams RG, Fellows K, Miettinen OS. Noninvasive tests in the initial evaluation of heart murmurs in children. New England Journal of Medicine 1983;308:6164. Geva T, Hegesh J, Frand M. Reappraisal of the approach to the child with heart murmurs: is echocardiography mandatory? International journal of Cardiology 1988;19:107-113. Finley J, Sharratt G, Nanton M, Chen R, Roy D, Paterson G. Auscultation of the heart: a trial of classroom teaching versus computer-based independent learning. MEDICAL EDUCATIONOXFORD- 1998;32:357-361. March SK, Bedynek Jr JL, Chizner MA. Teaching cardiac auscultation: effectiveness of a patientcentered teaching conference on improving cardiac auscultatory skills. Mayo Clinic Proceedings: Elsevier, 2005:1443-1448. Roy D, Sargeant J, Gray J, Hoyt B, Allen M, Fleming M. Helping family physicians improve their cardiac auscultation skills with an interactive CD‐ROM. Journal of Continuing Education in the Health Professions 2002;22:152-159. Kopes-Kerr CP. Horton hears a Who but no murmurs—does it matter? Family practice 2002;19:422-425. Frintner MP, Cull WL. Pediatric training and career intentions, 2003–2009. Pediatrics 2012;129:522-528. Sectish TC, Zalneraitis EL, Carraccio C, Behrman RE. The state of pediatrics residency training: a period of transformation of graduate medical education. Pediatrics 2004;114:832-841. Snow J. The complete research suite: a step-by-step guide to using Qualtrics. Qualtrics, Provo 2011. Willis G. Question appraisal system QAS-99. Rockville, MD: Research Triangle Institute 1999. 23. Sousa DA. How the brain learns: Sage, 2011.