B. Exit and Transmission
advertisement

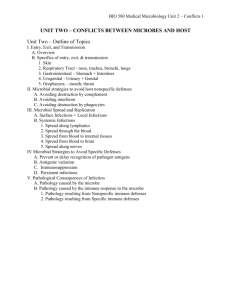
BIO 580 Medical Microbiology Unit 2 – Conflicts 1 UNIT TWO – CONFLICTS BETWEEN MICROBES AND HOST Unit Two – Outline of Topics I. Entry, Exit, and Transmission A. Overview B. Specifics of entry, exit, & transmission 1. Skin 2. Respiratory Tract - nose, trachea, bronchi, lungs 3. Gastrointestinal – Stomach + Intestines 4. Urogenital - Urinary + Genital 5. Oropharynx – mouth; throat II. Microbial strategies to avoid host nonspecific defenses A. Avoiding destruction by complement B. Avoiding interferon C. Avoiding destruction by phagocytes III. Microbial Spread and Replication A. Surface Infections = Local Infections B. Systemic Infections 1. Spread along lymphatics 2. Spread through the blood 3. Spread from blood to internal tissues 4. Spread from blood to brain 5. Spread along nerves IV Microbial Strategies to Avoid Specific Defenses A. Prevent or delay recognition of pathogen antigens B. Antigenic variation C. Immunosuppression D. Persistent infections V. Pathological Consequences of Infection A. Pathology caused by the microbe B. Pathology caused by the immune response to the microbe 1. Pathology resulting from Nonspecific immune defenses 2. Pathology resulting from Specific immune defenses BIO 580 Medical Microbiology Unit 2 – Conflicts 2 UNIT TWO –Terminology that will be encountered during lecture but not defined Using a medical dictionary, define: “acutely ill” Nuchal rigidity – Chronic granulomatous disease (CGD) – Febrile – Petechiae Polyarthritis – Myalgia – Dyspnea – Diaphoresis Erythrocyte sedimentation rate (ESR) – And what is a normal ESR for children? – Sequela – Arthralgia Anorexia Somnolesence Rigor Incubation period – Pyogenic Pyrogenic – BIO 580 Medical Microbiology Unit 2 – Conflicts 3 UNIT 2 – CONFLICTS BETWEEN MICROBES AND HOST Response to Infection – Biologic response gradient I. ENTRY, EXIT, AND TRANSMISSION Objectives: 1. know the first line host defenses of each of the 5 systems 2. explain how microbes enter each of the 5 systems 3. what is one of the most important mechanisms for establishment at each site of entry? 4. describe how microbes exit each system A. OVERVIEW Some microbes live on body surfaces Ex. normal skin microbiota like Staphylococcus epidermidis, diphtheroids. Also some pathogens - Vibrio cholera, Campylobacter jejuni 1. Entry into host a. Active penetration - invasive Ex 1. S. epidermidis is not invasive but S. aureus is Ex 2. Shigella invades epithelial cells of colon - Salmonella invades small intestinal epithelial cells. b. Insertion - by biting insect Exs. Organism Plasmodium Rickettsia typhi Yersinia pestis Yellow fever virus Disease malaria typhus plague yellow fever Insect vector mosquito rat flea rat flea mosquito c. Break (bite, puncture, burn) Exs. Pasteurella multocida, rabies virus, Clostridium tetani. d. Impairment - of surface or systemic defenses Ex. disorders of phagocytic cells ↑infections BIO 580 Medical Microbiology Unit 2 – Conflicts 4 Attachment to target cell - aided by specific receptors After attaching: 1. remain on outside of cell & multiply on the surface of the cell – Ex. Vibrio 2. enter cell & multiply w/in it – Exs. Shigella, Salmonella, viruses B. Exit and Transmission 1. Exit body a. shed - secretions - resp. droplets, saliva, semen, feces b. sucked out of blood - insects 2. Successful transmission to new host depends on: a. number of microbes shed - the more the better b. stability in the environ. - cysts, spores, naked viruses c. number of individuals required to infect a new host - varies - Shigella 1-10, Salmonella 106 The most common infections are spread Via: 1. respiratory route (Exs. colds, influenza) 2. fecal-oral route (Ex. diarrheal diseases like Giardia) 3. sexual transmission (4. needles have provided a new mech – Exs. HIV, Ebola, hepatitis B) BIO 580 Medical Microbiology Unit 2 – Conflicts 5 B. SPECIFICS OF ENTRY, EXIT, AND TRANSMISSION 1. Skin Rev. of defenses of the skin Some pathogens can live on non-living layer of skin - Ex. fungi called Dermatophytes a. Entry across skin barrier 1. break - wound/bite/burn 2. biting insect 3. hair follicles Ex. S. aureus - lipase, some strains toxin called exfoliatin - separates layers of dermis b. Exit & Transmission from skin Direct contact between infected hosts viruses: Exs. human papilloma virus (genital warts), herpes, chicken pox bacteria: Exs. pathogenic staphylococci & streptococci, Treponema pallidum dermatophytes: athletes foot, ringworm protozoa: Leishmania BIO 580 Medical Microbiology Unit 2 – Conflicts 6 2. Respiratory Tract - nose, trachea, bronchi, lungs a. Entry to RT Transmission – person to person via respiratory droplets or fomites/fingers Fate of droplet depends on the size of droplet particle: Particle diameter > 10 micrometers 5-10 micrometers < 5 micrometers Where lands URT: nose, throat Bronchioles Alveolar region Defenses against entry 1. nasal hairs (vibrissae) 2. mucus (containing lysozyme, lactoferrin, maybe antigen specific sIgA) 3. ciliary action 4. cooler temperature (33°C vs 37°C) Pathogens avoid these defenses 1. attach tightly - Exs. Bordetella pertussis, Neisseria meningitidis, Influenza virus, cold viruses 2. take advantage of dame to muco-ciliary clearance – Streptococcus pneumoniae 3. produce toxin to interfere with ciliary activity - Exs. Bordetella pertussis, Haemophilus influenzae, Pseudomonas aeruginosa, Mycoplasma pneumoniae 4. inhaled directly into lungs main defense of lungs - complement, alveolar macrophages, maybe antigen specific sIgA and IgG Mycobacterium tuberculosis b. Exit & Transmission from RT Cause increase in secretions inflammation vas. permeability fluid *sneezing coughing talking easily spread because of crowding dry air impairs mucociliary action (also smoke, alcohol) from one person’s respiratory tract directly into another's BIO 580 Medical Microbiology Unit 2 – Conflicts 7 3. Gastrointestinal – Stomach + Intestines a. Entry to GI Transmission – fecal-oral route (includes fecal – water/food – oral) Defenses of GI 1. acid of stomach 2. dense normal microbiota 3. peristalsis, mucus + sIgA + phagocytes 4. proteolytic enz, bile 5. gut associated lymphoid tissue (GALT) Pathogens avoid these defenses 1. motility - Exs. V. cholera, Salmonella, some E. coli 2. mucinase - Ex. V. cholera 3. attachment a. via specific receptors Exs. V. cholerae, rotavirus; Shigella vs. Salmonella b. mechanical Exs. Giardia lamblia trophozoites, hookworms 4. Survive in presence of acid, proteolytic enzymes, bile Exs. Streptococcus faecalis, Salmonella b. Exit and Transmission from GI feces Exs. cysts (Giardia, Cryptosporidium), naked viruses (rotavirus, poliovirus) BIO 580 Medical Microbiology Unit 2 – Conflicts 8 4. Urogenital - Urinary + Genital a. Entry to bladder and/or urethra Transmission – via self-inoculation Urine in the bladder is normally sterile Defenses of bladder and lower UT 1. voiding urine 2. WBC + sIgA Invaded from the exterior- via the urethra = ascending infection Pathogens avoid these defenses 1. specialized attachment mechs - fimbriae - Exs. E. coli Neisseria gonorrhoeae, Chlamydia trachomatis Spread from urethra bladder - is difficult in males - urethra is 20 cm long UTI in females are common - 14X greater - 20% get symptomatic UTI - urethra is very short 5cm Defenses of female reproductive organs 1. downward flow of mucus + lysozyme 2. ciliated epithelial cells 3. normal microbiota - lactobacilli, 108/ml in adult female - pH 5 b. Exit and Transmission from Urogenital transmission via contaminated urine NOT common Exceptions - leptospira, Lassa virus (rodent urine) *direct mucosal contact - STI enhances transmission: discharge - gonorrhea, chlamydia sores -syphilis, herpes simplex BIO 580 Medical Microbiology Unit 2 – Conflicts 9 5. Oropharynx - mouth; throat a. Entry to oropharynx Transmission via iingestion, hand-mouth, mouth-mouth Defenses of oropharynx 1. Cleansing mechs - flushing action of saliva 2. sIgA 3. Lysozyme 4. Normal microbiota 5. WBC Pathogens avoid defenses 1. Attachment - fimbriae b. Exit and Transmission from oropharynx 1. Saliva - Ex. streptococci some infection of salivary glands - Exs. EBV (mono) mumps, herpes SUMMARIZE COMMON THEMES: What aids in establishment at a site of entry? What factors encourage transmission of microbes to new hosts? BIO 580 Medical Microbiology Unit 2 – Conflicts 10 II. MICROBIAL STRATEGIES TO AVOID HOST NONSPECIFIC DEFENSES Complement, interferon, phagocytosis Objectives: 1. Understand that successful pathogens have evolved strategies to avoid nonspecific defenses 2. Explain how these pathogen avoidance strategies work. 3. Understand the significance in particular of anti-phagocytic strategies. A. AVOIDING DESTRUCTION RESULTING FROM ACTIVATION OF COMPLEMENT Several exs. of strategies to prevent formation of MAC 1. capsules prevent activation of alternate pathway Ex. S. pneumoniae, Klebsiella 2. coating w/ IgA prevents activation of classical complement Ex. Campylobacter 3. prevent stabilization of C3 convertase and resulting cascade Ex. Pathogenic streptococci & Campylobacter 4. degrade C3b & C5b before cell binding Ex. N. meningitidis, Y. pestis 5. bud off membrane bound C3b & C5b so MAC doesn’t form 6. long chains of polysaccharides prevent MAC formation Ex. strains of Salmonella B. AVOIDING INHIBITION BY INTERFERON poor inducers of interferons – hepatitis B block action of interferons – hepatitis B, HIV, EBV BIO 580 Medical Microbiology Unit 2 – Conflicts 11 C. AVOIDING DESTRUCTION BY PHAGOCYTES – very important pathogen strategies!! 1. Inhibit chemotaxis or mobilization of phagocytes a. toxins that suppress chemotaxis Ex. Streptococcus, Clostridium perfringens 2. prevent/delay contact with phagocyte a. capsules Ex. esp. pathogenic streptococci, Haemophilus influenzae, Klebsiella pneumoniae, many others b. fimbriae Ex. pathogenic neisseria c. M protein Ex. S. pyogenes d. FcR Ex. Staphylococcus aureus Protein A & S. pyogenes Protein G, herpes group viruses induce FcR on surface of infected cell 3. Escape from phagosome into cytoplasm Ex. Shigella, Listeria monocytogenes, Mycobacterium leprae, Trypanosoma cruzi 4. Prevent fusion of lysosome with phagocytic vacuole Ex. M. tuberculosis, Salmonella typhimurium, Toxoplasma gondii 5. Resist killing and digestion in phagolysosome Ex. L. monocytogenes, Yersinia pestis, S. typhimurium, reoviruses are actually stimulated to uncoat by lysosomal enz. 6. Resist oxygen-dependent killing Ex. M. tuberculosis prevents respiratory burst, M. leprae scavenges ROI Ex. catalase – staphylococci, L. monocytogenes 7. Kill the phagocyte Ex. hemolysins of pathogenic streptococci and staphylococci, L. monocytogenes Ex. Lethal factor of Bacillus anthracis BIO 580 Medical Microbiology Unit 2 – Conflicts 12 CONCEPT CHECK 5 Neisseria meningitidis (one causative agent of bacterial meningitis) is carried, apparently harmlessly, in the respiratory tracts of approximately 20% of the population (estimates vary). 1) Explain how, in general, respiratory tract pathogens are acquired, 2) List the defenses (defenses against entry and then nonspecific interior defenses) of the respiratory tract that would be relevant to bacterial infections, and 3) Discuss the strategies that specifically N. meningitidis has evolved that allows it to avoid the nonspecific defenses of the upper RT. BIO 580 Medical Microbiology Unit 2 – Conflicts 13 III. REPLICATION AND SPREAD OF MICROBES IN THE HOST Objectives: 1. Know some of the general differences between local infections and systemic infections 2. Understand the various mechanisms by which microbes can spread from the site of entry to other systems in the body There are 2 basic categories of infections - surface infections and systemic infections. A. SURFACE INFECTIONS = Local Infections Many microbes multiply at the site of entry and don't invade deeper into tissue or spread to other systems in the body. Surface or local infections spread easily on mucosal surfaces (intestinal, respiratory). Surface infections often result in large scale production and movement of body fluids. This large scale movement of fluid can spread an infection very quickly (large areas of the body surface can be involved within a few days). General Characteristics of Surface Infections: 1. Short incubation times - less than 1 week. 2. Microbes are replicate very rapidly 3. Nonspecific defenses are key to control - the early nonspecific defense mechanisms; complement activation, interferon, phagocytosis, and NK cells are key to controlling the infection - no time to wait for specific defenses to activate. Ex. Common cold, Gastroenteritis, Gonorrhea B. SYSTEMIC INFECTIONS Some microbes enter the lymph fluid or blood and then spread through the body involving more than one system. General Characteristics of Systemic Infections: 1. Longer incubation times, greater than 1 week. (Ebola virus, 12-21 days incubation; incubation for HIV is years.) 2. Microbes replicate more slowly 3. Specific defenses (activated Tc, antibodies) are key to control - because of longer incubation times, there is time for specific defenses to activate and play a role in controlling infection. EX. Measles, Typhoid fever, Tuberculosis BIO 580 Medical Microbiology Unit 2 – Conflicts 14 1. What keeps surface infections from spreading deeper? a. Temperature - Ex. Rhinovirus- upper respiratory tract is 33°C, lower respiratory tract is 37°C. Rhinovirus don’t replicate well at 37ºC. b. Mechanism of exiting the infected cell - Ex. Influenza virus spreads through free surface of epithelial cells but not through the basal surface. 2. Why do some microbes take the risk of spread through the blood and lymph where they will encounter the full force of the immune system? Because they need to replicate at a body site distant from their point of entry into the body Ex. Mumps virus- enters via inhalation but multiplies in salivary glands. Ex. Hepatitis A virus enters the GI via ingestion, but it replicates in the liver. How would it get from the intestines to the liver? It needs to travel through the blood. Systemic Infections often follow a stepwise invasion of different tissues of the body. 1. Spread along the Lymphatics Many bacteria that spread along the lymphatic route induce significant signs of inflammation. For example, a minor skin wound followed by red streaking and tender swollen local lymph nodes are classical signs of inflamed lymphatic vessels. The bacteria secrete toxins or cause other forms of tissue damage that early on in the course of infection set off alarm bells to cause acute inflammation and alert the nonspecific interior defenses. In general, bacterial spread is accompanied by inflammation - bacterial spread is noisy. In contrast to bacteria, many viruses can invade along the lymphatics without inducing inflammation, they are silent. Viruses cause little tissue damage early in the course of infection so inflammatory responses are absent or delayed. EBV-(infectious mono) - may be present for weeks before any inflammatory responses are activated. And some viruses can infect cells for long periods of time before they damage them. BIO 580 Medical Microbiology Unit 2 – Conflicts 15 2. Spread through the Blood A microbial infection might be arrested at any point during lymphatic spread. But microbes that can evade phagocytosis or multiply within the lymph nodes will ultimately reach the blood stream, because movement from one system into the other is easy (see part (a) of picture below). Small numbers of bacteria can enter the blood without causing damage. Transient bacteremias, bacteria in the blood, are common. What happens to microbes moving through the blood is related to: 1. whether they are free in the plasma where they are exposed to phagocytes and antibodies, or 2. whether they are intracellular in circulating cells, like erythrocytes, monocytes, lymphocytes, where they can escape immune detection – this is a more successful strategy. Exs: EBV and Listeria are intracellular in monocytes or lymphocytes, malaria in erythrocytes, Salmonella and Leishmania in macrophages. Microbes may leave the circulation and enter other body sites as the blood flows through these tissues/organs. BIO 580 Medical Microbiology Unit 2 – Conflicts 16 3. Spread from Blood to Internal Tissues Sometimes free bacteria that enter the blood have the opportunity to colonize internal sites that are less well protected before being eliminated by phagocytes. Ex. (add notes) 4. Spread from Blood into Brain There is a barrier between the blood and the cerebral spinal fluid and between the blood and brain that is impervious to most microbes (this barrier is called the Blood-Brain Barrier (BBB But there are some microbes that can cross the blood-brain barrier and gain access to the CSF or brain. Often these microbes induce inflammation that makes the BBB more permeable. Infections of the CNS are especially dangerous as the BBB also keeps out most host immune cells and drugs. – Exs. Neisseria meningitidis, Haemophilus influenzae- cause increased permeability of BBB and cross over into the brain. BIO 580 Medical Microbiology Unit 2 – Conflicts 17 5. Spread along Nerves Some microbes can spread along nerve networks. There are few if any host defenses to control, especially viral, spread once the nerves are infected. Exs herpes simplex is never eliminated varicella-zoster is never eliminated Rabies is never eliminated and is 100% fatal Covered in more detail in Unit 3, Diseases of the NS. BIO 580 Medical Microbiology Unit 2 – Conflicts 18 CONCEPT CHECK 6 Neisseria meningitidis enters the host via the nasopharynx, but invasive strains cause the disease bacterial meningitis when they infect the meninges of the brain. Discuss how N. meningitidis moves step-wise through the body from the nasopharynx to the meninges of the brain. BIO 580 Medical Microbiology Unit 2 – Conflicts 19 IV MICROBIAL STRATEGIES TO AVOID SPECIFIC DEFENSES Objectives: 1. Understand the significance of pathogen avoidance strategies in relation to replication and spread, pathology, and transmission. 2. Explain the potential consequences to the host of microbial mimicry. 3. Discuss the significance of antigenic variation. 4. Explain, in detail, the 3 mechanisms that produce antigenic variation A. PATHOGEN PREVENTS OR DELAYS RECOGNITION OF ITS ANTIGENS 1. Pathogen colonizes “privileged” sites a. external sites – skin & intestinal lumen b. internal sites - CNS, joints, testis, and placenta c. pathogen-created sites – cysts – Ex. Echinococcus d. integrate in to cell’s DNA – Ex. retroviruses 2. Pathogen is intracellular a. does not display antigens on cell surface – Ex. herpes b. puts proteins on an internal membranes – Ex. coronavirus c. prevents MHC + antigen traffic to cell surface – ex. adenovirus 3. Pathogen’s antigens are very similar to host antigens = mimicry – immune response may be weak or absent – Ex. scrapie (PrPS is similar to PrPC) Does NOT always prevent immune detection and pathological consequences. Example – Association between Streptococcus pyogenes and rheumatic heart disease (take good notes here) BIO 580 Medical Microbiology Unit 2 – Conflicts 20 4. Pathogen covers surface with host molecules (camouflage) a. antibody molecules absorbed via FcR – bacteria and viruses b. fibrin – coagulase-positive staphylococci c. host blood group glycoproteins + MHC molecules + antibodies – parasitic worms 5. Pathogen induces a lack of responsiveness to its antigens a. infection of the fetus – Ex. CMV, rubella b. produce large quantities of antigen or antigen-antibody complexes and desensitize immune response– Ex. fungal and protozoan infections c. exploit gaps in immune response B. ANTIGENIC VARIATION - change surface Ag presented to host immune Occurs in the antigens that are recognized by the immune response More common in long-lived hosts More common in infections that have short incubation times and pathogen is transmitted before a secondary response would come to full force. 1. Antigenic variation may occur in a given individual during an infection. Ex - Trypanosoma, Neisseria, Influenza virus 2. Antigenic variation may occur as the pathogen circulates through the community of hosts Ex – Poliovirus, Influenza virus 3 main mechanisms that produce antigenic variation: 1. mutation 2. recombination 3. gene switching BIO 580 Medical Microbiology Unit 2 – Conflicts 21 mutation – single base substitutions subtle changes in surface antigens = antigenic drift. 1. Exs. rhinovirus, enterovirus, poliovirus, HIV **Ex. Influenza virus –hemagglutinin and neuraminidase surface proteins Neuraminidase Hemagglutinin entry into cell RNA genome – 8 segments Single base mutations in RNA produce slight changes in H that gradually accumulate year to year = antigenic drift Seasonal flu epidemics BIO 580 Medical Microbiology Unit 2 – Conflicts 22 2. recombination of genes major changes in surface proteins = antigenic shift. **Ex. influenza A viruses – segments of RNA from human and animal strains recombine (also known as reassortment) Human strain Animal strain Co-infecting a single host target cell From the animal strain Recombination leads to a sudden and total change in surface protein = antigenic shift Pandemic BIO 580 Medical Microbiology Unit 2 – Conflicts 23 3. gene switching - most dramatic change in antigen Exs. Trypanosoma - 1000 different genes coding for surface glycoprotein - sequence of totally unrelated infections. Neisseria gonorrhoeae – genes coding for pilin and outer membrane proteins. Time BIO 580 Medical Microbiology Unit 2 – Conflicts 24 D. IMMUNOSUPPRESSION 1. Infection of the immune cells blocking of immune cell function. Exs. T cells - HIV, measles virus B cells – EBV Macrophages – HIV, CMV, Leishmania 2. Upset coordination of immune regulation a. polyclonal activation of T or B cells production of lots of cytokines - upset the balance. Ex – staphylococci b. inhibit T cell proliferation. Ex - glycoproteins on the surface of the envelope of HIV. c. inhibit IL-2 production d. induce Tregs 3. interfere with local immune defenses. a. IgA protease. Ex - Neisseria, Streptococcus pneumoniae, Haemophilus influenzae (remember as Nice STriP of Ham) E. PERSISTENT INFECTIONS - remain in the host in a persistent state for many years, or even for the life time of the host. 1. infectious form – hepatitis B in blood 2. low or partial infectivity – adenovirus in tonsils 3. non-infectious form – herpes virus in dorsal root ganglion Significance of persistence: 1. can be reactivated, usually when host is immunocompromised. Ex – herpes viruses 2. associated with chronic disease of organs like liver. Ex – hepatitis viruses 3. associated with cancer. Exs. – hepatitis, human papilloma virus BIO 580 Medical Microbiology Unit 2 – Conflicts 25 CONCEPT CHECK 7 The virulence of many viruses is attributable, at least in part, to their ability to evade the body’s immune defense systems. Viruses exhibit diverse mechanisms for subverting the immune defenses. Discuss how the human immunodeficiency virus (HIV) evades the host’s specific immune defenses. DISCUSSION Discuss the mechanism of antigenic drift in Influenza viruses. Discuss the mechanism of antigenic shift in Influenza A viruses. BIO 580 Medical Microbiology Unit 2 – Conflicts 26 V. PATHOLOGICAL CONSEQUENCES OF INFECTION Objectives: 1. Know the various ways that microbes can directly affect the cells/tissues of a host 2. Contrast exotoxins and endotoxins 3. List the 4 modes of action of exotoxins and be able to discuss examples of each 4. Understand the physiological responses of the host to the presence of endotoxin in the body 5. Recognize the physiological responses to LPS as part of a clinical presentation of a disease 6. Discuss, in detail, how microbial infections result in fever 7. Compare and contrast two example lung infections; pneumonia and tuberculosis and the bacteria that cause them. A. PATHOLOGY CAUSED BY THE MICROBE 1. metabolic shutdown of infected cell – viruses 2. lysis of infected cell – viruses, intracellular bacteria, protozoa 3. fusion of infected cells – viruses 4. alter antigens that mark host cells, set them up as targets of body’s own defenses – viruses 5. activate acute inflammatory response – bacteria 6. toxin production – bacteria BIO 580 Medical Microbiology Unit 2 – Conflicts 27 2 categories of bacterial toxins – exotoxins (secreted) and endotoxins (cell-wall bound) a. Exotoxins = proteins secreted by Gram positive and Gram negative bacteria (usually extracellular bacteria) are encoded by genes located on plasmids or infecting bacteriophages are extremely potent Exotoxins (see table 17.2) may show one of 4 different modes of action: 1. Aid in survival or spread – very common - many examples of enzymatic toxins (-ase) a. Hyaluronidase – hydrolyzes hyaluronic acid present in connective tissue b. Collagenase – disintegrates collagen in connective tissue c. DNase – degrades DNA d. Streptokinase – converts plasminogen plasmin – lysis of fibrin clots e. Lipases – break lipids f. Coagulase - splits fibrinogen fibrin, creating clots 2. Damage or destroy cells – very common - membrane active cytotoxins - lyse RBC (= hemolysins), phagocytes& lymphocytes (= leukocidins) a. enzymes like lecithinase, phospholipase b. pore-forming molecules 3. Superantigens – toxins that over stimulate cytokine release by T cells. Ex. Staphylococcus aureus TSS strains. Over abundance of IL-2 nausea, vomiting, fever, rash, falling blood pressure, shock. TH secreted by pathogen APC Other exs. avian influenza in humans, SARS BIO 580 Medical Microbiology Unit 2 – Conflicts 28 4. Interfere with cell metabolism –very common (diphtheria, cholera, anthrax, etc) - share a common structural arrangement. 2 subunit types – A & B A subunit is responsible for toxicity B subunit binds to specific receptors Example 1 - Diphtheria Action of diphtheria toxin – prevents protein synthesis & so cell dies. Enough cells die, organ systems fail cardiovascular collapse. Example 2 - Tetanus Tetanus produces an enzyme called tetanospasmin – can get to the brain by 2 routes: 1. toxin blood brain = sudden death 2. toxin along nerve trunks peripheral nerves spinal column brain = slower death Action of tetanospasmin - blocks neurotransmitter release of inhibitory neurons – excitatory transmitter is continuously stimulating rigid, spastic paralysis Example 3 – Cholera - will be discussed in Unit 3 (Gastrointestinal) BIO 580 Medical Microbiology Unit 2 – Conflicts 29 B. PATHOLOGY CAUSED BY THE IMMUNE RESPONSE TO THE MICROBE 1. Pathology resulting from Nonspecific immune defenses a. Physical impairment of function of organ system Ex. S. pneumoniae infection of lungs induces acute inflammation (take good notes here) b. Response to endotoxin = lipopolysaccharide (LPS) not secreted, but released when bacterium dies toxic only in high doses, mg/kg body weight LPS triggers a series of physiological responses (Fig. 17.4) in the body that are due to: 1. mast cell degranulation secondary to IgE large amts of C3a & C5a 2. clotting of blood (via Hageman factor) 3. release of cytokines (esp. TNF, IL1, -IFN) Physiological responses to endotoxin are numerous, can be mild to very severe and fatal: 1. macrophages release cytokines that stimulate prod. of prostaglandins fever, weakness, aches 2. ↓in circulating neutrophils as they aggregate & stick to vessel walls where they release their toxic granules causing damage to endothelial cells. 3. clotting of blood in peripheral vasculature = disseminated intravascular coagulation (DIC) – rare - internal hemorrhaging (meningococcemia, Ebola, Dengue) 4. Bradykinin - vasodilation, ↑ vascular permeability 5. hypotension (severe drop in blood volume) vascular collapse - called endotoxic shock = septic shock 6. Multiple Organ System Failure (MOSF) a. lungs - acute respiratory distress syndrome (ARDS) b. kidneys - kidney failure c. brain - mental delirium d. liver - liver failure BIO 580 Medical Microbiology Unit 2 – Conflicts 30 c. Response to some cytokines = Fever Fever is a pathological consequence of cytokine production (IL-1 and TNF) fever = pyrexia Oral Normal Fever What part of the brain regulates body temperature? Mechanisms that result in fever 1. Stimulating an increase in body temperature – how body “knows” that temperature should be increased – happens at the chemical/cellular level Exogenous signals (signal originating from outside the body) Microbial pyrogens include (best known): 1. Gram negative LPS = endotoxin 2. teichoic acid - GP 3. units of peptidoglycan - GN and GP 4. TSST1 produced by S. aureus 5. erythrogenic toxin prod by Group A strep (S. pyogenes) 6. others yet unknown Endogenous signals (signals originating from inside the body, produced locally or systemically) = cytokines (TNF, IL-1) Drawing BIO 580 Medical Microbiology Unit 2 – Conflicts 31 Actually raising body temperature – happens at a physiological level Heat conservation mechanisms: behavioral changes piloerection - traps an air layer, retains body heat rather than letting it escape vasoconstriction - blood is diverted away from body surface where it normally would be cooled to the body’s interior where it is warmed up. Heat generation mechanisms: shivering – rhythmic contraction of muscles generates heat Resolution of fever – cooling mechanisms activated so body temperature returns to normal: behavioral changes vasodilation - increases flow of blood to the body surface where it is cooled sweating - evaporation from the surface Symptoms that accompany this cytokine production (in addition to fever): back pain generalized myalgia arthralgia anorexia somnolence chills What are the potential benefits to the host of experiencing fever? BIO 580 Medical Microbiology Unit 2 – Conflicts 32 2. Pathology resulting from Specific immune defenses = Hypersensitivities a. Type I Hypersensitivity – IgE – Anaphylactic Ex. Typical allergic rxn What if happens on a large scale? - systemic mast cell degranulation acute fatal anaphylaxis (anaphylactic shock - constriction of smooth muscle, decrease in blood pressure, vascular collapse, pulmonary edema) Ex. worm infections, rupture of tapeworm cysts. b. Type II – IgG – Cytolytic or cytotoxic Ex - malaria - complement-mediated lysis of the RBC hemolytic anemia Also hepatitis B, yellow fever c. Type III - IgM and IgG- stick to blood vessels or tissues, activating C & neutrophils. Ex. glomerulonephritis - inflammation of nephrons in kidney Ex. systemic lupus erythematosus BIO 580 Medical Microbiology Unit 2 – Conflicts 33 d. Type IV – Delayed Type Hypersensitivity – mediated by T-cells & macrophages = Cellmediated immunity = CMI. Ex. measles Ex. Tuberculosis - An ancient disease of humans; chronically-infected macrophages & persistently stimulated TH Mycobacterium tuberculosis – obligate aerobe, obligate pathogen. Gram positive that stains acid-fast due to mycolic acid. Highly resistant to killing by macrophages. TB is contracted via the respiratory route by inhalation of infectious droplets transmitted by an infected individual – can remain in the air for hours – inhaled directly into lungs by-passing muco-ciliary defenses. Primary Infection – 7 steps 1. M. tuberculosis are inhaled into middle region of lungs 2. M. tb are engulfed by alveolar macrophages (resident in the lungs), but prevent phagolysosome fusion. 3. Multiply both within macrophages (destroying them) and extracellularly. 4. Lymphocytes and monocytes are attracted. Monocytes differentiate into macrophages that also phagocytize M. tb. 5. Infected macrophages are carried by lymphatics to regional nodes and also to apices of lungs. 6. First few weeks, no effective host defense against infection. Ab play no role in immune defense. M. tb are not opsonized & do not activate classical complement. ** BIO 580 Medical Microbiology Unit 2 – Conflicts 34 7. 2 possible outcomes from primary infection: 1. Control. By 3-8 wks, macs present to and activate TH. TH secrete IL-2 and TNF- and macs are activated to kill intracellular M. tb. Macs and TH control infection. The macs and T cells and fibroblasts surround infection and a tubercle (= granuloma) forms, becomes fibrotic, encapsulated, scars. M. tb are not all killed, can remain in tubercle for decades, provide continuous boost to CMI. OR 2. Clinical disease. CMI does not control infection and progressive primary disease results– children under 5, elderly, advanced AIDS. Bacteria continue to spread in lungs, macrophage secretion of IL-1 and TNF clinical symptoms of fever, weight loss, and profuse night sweats. Lesions fill lungs, interfere with lung function death. Endogenous Reactivation Usually within 2 years of a controlled, primary infection, but can occur anytime after primary infection. M. tb are still alive in tubercles. Control and absence of signs of disease results from precarious balance between presence of M. tb and activity of macrophages and TH. Reactivation of disease results from decline in immune competence. Lesions usually seen first in apex of lungs. Tubercles necrotic caseous coalesce into larger complexes centers liquefy discharge bacteria into bronchial tree resume multiplication and spread. Clinical disease (with symptoms as described above) Mycobacterium tuberculosis has no direct or toxin-mediated means of causing damage; in tuberculosis all pathology is caused by the damage induced by the response of macrophages and T lymphocytes. BIO 580 Medical Microbiology Unit 2 – Conflicts 35 COMPARE AND CONTRAST Processes that may result in pathology during viral infections versus processes that may result in pathology during infection by extracellular bacteria. (Ex. think of the two genital pathogens herpes virus versus Neisseria gonorrhoeae) Pneumonia to tuberculosis Primary progressive tuberculosis with reactivation tuberculosis