Yeasting 11-9
advertisement

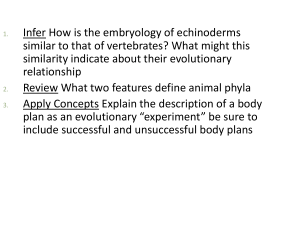
Yeasting Nov. 11, 2009; Development of Trilaminar Disc Implantation- in growth of trophoblast into endometrium. Endometrium alters and is known as deciduas; maternal BVs empty into intervillous space, which were originally lacunae; these coalesced and became larger, leaving synctitiotrophoblast suspended/hanging from fetal aspect of developing placenta to the maternal aspect of developing placenta. Cytotrophoblasts grow into these areas of synctiotrophoblasts, extraembryonic mesoderm grows in a BVs develop within this (embryonic fetal cardiovascular system) (see figure 4.17 & 4.16—longitudinal section through a villus) anchoring villi- when synctitiotrophoblasts are reinforced, anchor from fetal aspect to maternal; side branches develop from this as free villi—these do not bridge entire distance btw fetal aspect and maternal aspect (does not attach to maternal aspect); bridging villi hold things together Fig. 4.15 primary villi (cytotrophoblast growing into synctitiotrophoblastic elements) , secondary villi— when extraembryonic mesoderm grew in, tertiary villi (embryonic/fetal BVs developing in villi) We can tell that above picture of chorionic villus is a free villus bc we see fetal aspect but not the maternal surface; there are many BVs in here which is important for increasing the surface area for transmission diffusion from maternal blood to fetal blood and vise versa. Early on in pregnancy—(first half); placental barrier consists of fetal endothelial cells, extraembryonic mesoderm, cytotrophoblasts, synctitiotrophoblast. Diffusing back and forth- diffuse long distance and through several different cell layers (this occurs at early pregnancy); early on this is ok bc embryo is small and doesn’t need as much nutrients or waste products ridding; Early pregnancy is indicated by completed cytotrophoblastic layer Mid pregnancy—cytotrophoblasts drop away and run out; fetal BVs move to the sides of the villi and come in contact with syncytiotrophoblast through respective basal laminae (diffusion barrier has been reduced, very thin layer for diffusion to pass through); this is good bc the fetus is getting large at this point so we need more oxygen and nutrients to pass through readily and fetus needs to get rid of waste prdocucts (back diffusion) to get into maternal blood (this occurs before circulation happens) Components of maternal blood—has nutrients (good) and toxins (bad ) which can easily diffuse through the membrane; embryo/fetus gives up fetal waste which diffuses from high conc in fetal blood into low conc of maternal blood (fetal waste products then go with maternal blood and are eliminated either through maternal lungs as CO2 or nitrogenous wastes eliminated through the maternal kidneys) Immunoglobulins from mom to fetus can make it through and do not react to fetus, but give fetus some passive immunity so that when fetus is born it has some immunity to what mom has been exposed to. More harmful immunoglobulins and bacteria normally do not make it through membrane to fetus (so fetus is sequestered/hidden from maternal immune system) Tears in placenta- (occasionally this occurs) fetal blood is released in intervillus space; (fetal cells then circulate and are no longer hidden; fetus cells in mom’s body) mom might have immune response if have diff types of blood (different RH factors btw mom and child); maternal antibodies move across the placental membrane and begin to destroy fetus’ red cells. Other cells that migrate from fetal circulation into maternal circulation: ex. Fetal cells from male child can migrate to mom’s thyroid; male cells are found within thyroid bc thyroid is a vascular area and cells like it mom may have thyroid problems due to the immune response to these migrated cells. Trophoblast grows larger and larger, expands and grows into uterine lumen into Decidua capsilaris eventually it outgrows it’s blood supply; villi growing toward uterine cavity will decrease in size and degenerate as they lose a blood supply (thus these original villi are lost and smooth chorion remain) 2 portions of chorion (outer membrane)1) Villus portion= placenta 2) Smooth chorion (outer layer of extraembryonic membrane; this has lost it’s original villi) VIlli develop where there is a rich oxygen supply; where there is less O2, villi do not develop; start out with thin placenta, as villi get larger and more villi are formed, this takes up space; as this occurs, villi push further into underlying deciduas—syncio and cytotrophoblasts are pushed farther into deciduas. And areas without high growth are left in btw—cotelydons develop (these develop because of rich O2 supply by maternal vessels cause villus growth; in areas where there is not a lot of blood supply, partial septa develop in btw these go up toward the chorionic plate); fuzziness in coteyldon is due to the villi that have broken in; fetal BVs lie within the villus Tertiary villus has fetal BVs Early pregnancy indicated by complete trophoblastic layer; cyto and syncitio Red cells can only come in contact with here (in above pic) are either maternal endothelial cells or syncitiotrophoblasts; syncitiotrophoblasts and cytotrophoblasts will grow down around the ends of the open vessels to form a cap to prevent leakage. Maternal blood comes in, shoots all the way through the chorionic plate through the villi and then perculates back down across villi and then out through maternal veins Fig 4.18 stem villi extended from chorionic plate; figure 3.2 Maternal aspect of placenta—see cotyledons; break cotelydon open and see numerous fetal BVs lying within the villus; fetal aspect—see villi; chorionic tissues can develop well without the presence of a fetus (this is not a good thing if there is not a fetus there) Proof that all of this really does occur! When conceptus is invading in, it invades into glands which are good nutrient sources for developing fetus; maternal BVs are just under here and it will eventually invade into those too; initially there are villi that develop all around the conceptus; later on some of those villi will be lost; outer portion of extraembryonic membrane becomes known as the chorion this part will become stretched as conceptus enlarges which will decrease profusion; decidual capsilaris degenerates and chorion loses it villi which had originally developed. Villus chorion will become the placenta; placenta is always examined at the time of birth to make sure that the maternal aspect is intact and all the maternal placenta tissue has moved out of maternal body; this is important because chorionic tissues can develop well without fetus; if placental elements are retained, these may continue to develop and function and this is not a good thing. What occurs inside trophoblast: Extraembryonic coelom= chorionic cavity (cavity outside the embryonic proper; has fluid inside of it); hanging in chorionic cavity is the: 1) embryonic disc, 2) the amnion and the cavity that the amnion surrounds which is fluid filled; and the 3) umbilical vesicle (empty bubble, aka yolk sac; there is a primary and secondary/definitive yolk sac; there is actually no yolk in humans hence the name has been changed) also hangs within chorionic cavity, develops on other side of embryonic disc from the amnion. (see pic on page 1) Connecting stalk- largely extraembryonic mesoderm and some intraembryonic mesoderm (mesenchyme); connects intercell mass to the chorion Allantois diverticulum of yolk sac; vessels that supply this become umbilical vessels; when “shrink wrapped” by amnion it is known as umbilical chord See figure 2.10 and 3.1 Inner cell mass/embryoblast develops into 2 layers: 1) epiblast 2) hypoblast (hence we have a 2 layer disc) this is occurring during the 2nd week of development. Within the epiblast, a small cavity develops which becomes the amnionic cavity. Original epiblastic cells start separating bc of formation of epiblastic cavity into an epiblast proper (remains in same location) and amnioblasts (have moved out). Hypoblastic cells- on inferior aspect of epiblast; these stick into the original blastocyst cavity and with time the amnionic cavity enlarges, hypoblastic cells have proliferated and are growing down into inside of trophoblastic cells, forming an exoceolomic membrane (another layer now covers the original blastocele; 2 layers now exist—exocoelomic membrane of hypoblastic origin and trophoblastic cells). Hypoblastic cells migrate down on inside or trophoblasts and proliferate externally and this population of cells forms cellular layer of tissue known as extraembryonic mesoderm (has a lot of extracellular space, cells are stellate and have processes; fills space btw trophoblast and extracoelomic membrane and space btw trophoblasts and amnioblasts) grows into villi as they form to form secondary stage of villus formation (see figure 3.4); extraembryonic mesoderm completely surrounds the embryo proper/bilaminar discs and the 2 vesicles (amnion and primary yolk sac) forming within this. Everything in extraembryonic mesoderm will divide, except…the one place where extraembryonic mesoderm does not divide will become the connecting stalk. At same time as extraembryonic mesoderm spits, another generation of cells grow out of embryonic disc, making a new lining for the upper portion of the primary yolk sac. What was a large space is now changing into 2 smaller spaces (hour-glass shaped, somewhat); endodermal cells coming out of the embryo proper push hypoblasts aside; one space will ultimately be lined with endoderm and other small space will be pinched off (2ndary yolk sac becomes related to embryonic disc and remnant sac will be lost). What was primary yolk sac is now dividing into secondary yolk sac and remnant. Thus, a cavity is created inside chorion (chorionic cavity) in which bilaminar embryo surrounded by amnionic cavity and yolk sac are susepended into; Trophoblastic structures (chorion ) is growing rapidly at this point and claiming space. Later on it will reduce it’s growth rate, then amnion and embryo will grow to fill this cavity. BVs develop within extraembryonic mesoderm related to chorion and within the connecting stalk and embryo proper. 3 major sets of vessels: 1) placental vessels 2) umbilical vessels (within what will become umbilical cord, derived from allantoids) 3) intraembryonic vessels. As embryo grows , it changes from a disc to a modified cylindar. Amnion enlarges; amnion is initially attached to the edge of the amnionic disc; edge of amnion disc becomes the circumference of umbilical chord (naval). Embryo pulls the amnion around as it changes from a disc to a modified cylinder; it’s still attached to edge of disc which is the circumference of the umbilicus. This will put the cylindrical embryo into the amnionic cavity; amnion will then grow rapidly, it will “shrink wrap” around the connective stalk bc this is also at the umbilicus. The 2ndary yolk sac sticks out through the umbilicus. As amnion increases in size it grows from the umbilicus down along the connective stalk wrapping together the connective stalk tissue and its contained BVs and a portion of the definitive yolk sac (2ndary yolk sac) creating the umbilical cord!! As amnion increases in size and amnionic cavity increases in size, chorionic cavity decreases in size. Amnionic cavity creates the fluid filled space that the little one develops in. Ultimately the chorionic cavity and amnionic cavity fuse and the chorionic cavity (extraembryonic coelom) is eliminated; outer surface of the amnion (extraembryonic mesoderm) fuses with the inner aspect of the chorion (extraembryonic mesoderm) and they come together IF YOU WILL. Decidua parietalis gets stretched and is eliminated so that smooth chorion ultimately comes in contact with the decidua parietalis and fuses. When placenta and other extraembryonic membranes are delivered at the time of partuition, placenta comes out and a layer of deciduas. Chorion and amnion fused together and come out and a layer of decidua related to this amnionic-chorionic membrane. Allantois-(along with chorion and amnion, another extraembryonic membrane) outgrowth of yolk sac; grows into the connective stalk; in animals who develop in shells (reptiles and birds), the allantois is a reservoir for waste products; in humans this will become part of the urinary bladder. BVs that supply the allantois become the vessels that develop within the connective stalk (become the umbilical vessels) connect intraembryonic circulation to placental circulation. When there is enough amnionic fluid- This can be sampled to tell the health of the little one (look at cell composition; cells from the amnionic fluid can be used for genetic testing (trophoblastic cells can also be use for this from biopsies of placenta or abdominal wall or even through the vagina/cervical canal to biops tissues there); placental tissue (extraembryonic tissue) have the same genetic makeup as the little one. Ultra sound is used to know that you are not sticking the little one. Implantation Problemsif there is a hold up (delay) in the conceptus, it implants in the uterine tube. When ZP dissolves(at about 5 days after fertilization) the conceptus will implant there (wherever it is, normally this is the uterine cavity, but if delayed it is the uterine tube). Uterine tube does not have the ability to expand like the uterine cavity (uterine tube is well vascularized). Uterine tube till rupture (vasculature will be torn open; fatal to little one; life threatening to mom); can also implant in isthmas portion of uterine tube (slightly further along)- uterus cannot expand as well here either so will rupture here also. Conceptus can also implant on other tissues such as the stomach; lt implants on BVs here. (fetus can be born from this and other extrauterine tissues; problem arises at time of birth/partuition; can get little one out through c-section but getting the placenta out is the problem; it should not be left in (bc it has such a big blood supply!) In uterus, blood supply to placenta is pinched off during uterine contraction so with partuition uterus gets smaller and BVs passing through here to the placenta are pinched off and there is partuition hemmorage @12 days post fertilization; synctitiotrophoblasts gets nutrients from endometrial glands and then into maternal BVs (small ones first); see fig 3.4; Conceptus releases early pregnancy factors as it moves through uterine tube. Synctitiotrophoblast releases gonadotrophins (“feeding gonads”), (hCG), which comes from the chorion gets into maternal circulation and circulates throughout the body; this stimulates the CL (which would normally diminish at this time) to continue to be maintained and enlarge; thus progesterone is still produced which maintains endometrium/decidua. This occurs for about 3 months. After this point, synctitiotrophoblasts produce enough placental estrogen and progesterone and other hormones to maintain pregrancy. If syncytiotrophoblasts do not produce hCG at this time (during first 3 months), sloughing will occur which allows normal menstruation to occur and little one is lost TRILAMINAR DISC: Day 13—(fig 3.7)- there is a bilaminar disc; fluid filled cavities surround it; before circulation has been established. Cut edge of amnion apprears to edge of disc, which is somewhat oval in shape; there is a proliferation of cells within the embryoblast; Around Day 18 a streak/mound eventually forms (“primitive streak”) (see figure 4.2); will become the caudal end of the embryo (away from the head); Cells will migrate away from the primitive streak and drop down deeper into the epiblastic layer and migrate in btw here and hypoblast creating a new layer of cells (mesoderm). During migration, point where they take off deepens and is called the “primitive goove” (as they migrate away this depression is created). The cranial end will become a pit-like area (deepening) of the primitive groove known as the “primitive node”; there is not a uniform widening (as embryo disc gets wider, it adds predominately to the caudal end, rather than the cranial end); tissue migrates away but mainly adds to caudal end (locally). Above is day 16 embyro; to the right is the cranial portion of the embryonic disc 3 areas where regular mesoderm does not go: 1) buccopharyngeal membrane (=oropharyngeal membrane); 2) cloacal membrane; 3) notochord (in midline btw oropharyngeal membrane and primitive node) (has same origin of mesoderm but has special properties therefore not considered mesoderm, notochord is controller) Oropharyngeal membrane (buccopharyngeal membrane)- (relating to mouth and pharynx; beginning of digestive tract) temporary membrane which forms the area of fusion of ectoderm and endoderm (non mesoderm in btw; thirs layer of cells does not migrate into this area), lies at cranial end Cloacal membrane- at the tail end (cloaca) of the membrane (sewer end of digestive tract); no mesoderm goes in btw here also Prechordal plate (=prochordal cells)- group of early migrating epiblastic cells that localize immediately caudal to the oropharyngeal membrane; organizing center for the head area Prenotochordal cells- epiblastic cells that drop down into what will become the mesodermal area (btw epiblast and hypoblast) and take up residency there Notochordal process- (prechordal cells are added to, to become this); usually depicted as a hollow rod (cylinder) of cells; was originally solid cells and tube developed within it (notochordal canal). Mesenchymal cells that have ingressed through the streak and aquire mesodermal cell fate which then go onto migrate cranially from the primitive node and pit forming this median cellular chord Notochordal plate-(notochordal process opens up and flattens out to form this) ventral aspect of notochordal process opens up inferiorly blends with adjacent endoderm, flattens out and now becomes this. Arises once notochordal process elongates and the primitive pit extends from this to form notochordal canal (cellular tube which extends cranially from primitive node to prechordal plate); floor of notochordal process fuses with underlying embryonic mesoderm; these fused layers undergo degeneration and notochordal canal can communicate with umbilical vesicle; floor of notochordal canal disappears remains of notochordal process forms a flattened grooved notochordal plate Neurenteric canal- ventral aspect of notochordal process breaks up and becomes open to the yolk sac; sides of cylinder are now continuous with endoderm on top of yolk sac; this is a temporary opening/communication between yolk sac cavity and amnionic cavity; if this persists in some individuals it becomes a fistula between tissue around spinal cord and lumen of digestive tract. Notochord- when notochordal plate rises back up again to form a solid rod of cells (not a cylinder despite pic) it is known as the notochord; it is a very important controlling structure; organizes through induction and inhibition the tissue surround it to determine the fates of the cells surrounding this structure (helps develop a lot of axial structures). A cellular rod-like structure; extends from oropharyngeal membrane to primitive node; it will degenerate as the bodies of the vertebrae form; small portions persist forming the nucleus pulposus of each intervertebral disc. See fig 4.3, figure 4.12 Summary: epiblastic cells dropping down to the underlying hypoblastic layer; some cells take up residency here (become endoderm), others stay in area btw (become mesoderm) ; others will migrate through the primitive groove. 3 areas where mesoderm does not go: oropharyngeal membrane, cloacal membrane, notochord. There is a new layer of cells that replace hypoblastic cells= “intraembryonic endoderm”; these push hypoblastic cells aside; early on the migration of these cells is haphazard, then it becomes more organized and majority of migration takes place through primitive streak/primitive groove area. Epiblastic cells become known as ectoderm, mesodermal cells, and then endodermal cells! Mesoderm: 3 major areas of organization: 1) para-axial (closests to the notochord; “next to axis”) gives rise to somites 2) intermediate area- lateral to para-axial; gives rise to urinary and reproductive systems 3) lateral plate mesoderms-most lateral of the mesoderm areas; gives rise to body wall structures, CT, gut (digestive tract), internal organs Migration of cells is not willy nilly (see fig 4.11)- migrate into these 3 areas of mesoderm (can have deficits in some areas and not other areas) Lateral plate mesoderm this will cleft; forms areas of enlarged intracellular or extracellular spaces which eventually coalesce forming the body cavities (“intraembryonic coelom”). Before this para-axial and intermed develop. Para-axial-- Somites develop give rise to axial skeleton, skull, vertebral bodies, and muscles related to these areas, nervous system, also muscles of limb muscles and body wall (see fig 4-9) Lateral plate mesoderm forms a coelom that is intraembryonic; divided into 2 regions by coelom: 1) somatic mesoderm- overlying ectoderm which contributes to body wall and soma, skeletal muscle, bone, cartilage 2) visceral/splanchnic mesoderm- yolk sac; gives rise to CT or muscle related to central organs, glands Combining terms: Somatopleure= somatic mesoderm + ectoderm Splanchnopleure= visceral mesoderm + endoderm Notochord controls tissue development around it. Epiblastic cells dorsal to notochordal structure will be transformed/maintained and become neural tissue. Neural tissue forms a groove as it folds, groove deepens, ultimately comes together and neural tissue breaks free and becomes central portion of nervous system. Ectoderm comes together and is fused to form epidermis Neural crest tissue= Specialized tissue developing btw regular ectoderm and neural tissue; was at crest of neural fold; this will break free and is free to migrate and develop into whatever it wants to do (fig 5.3) Primitive streak/groove should turn off it’s proliferation- if not, a sacro-coccuygeal teratoma may arise **New individual is of epiblastic origin!! Bc this replaces hypoblast (moves them aside) to become endoderm, or forms mesoderm; hypoblast contributes to extraembryonic structures. Ectodermsurface ectoderm: epidermis; gives rise to epidermal structures (skin, nails, hair, glands) Endodermgives rise to epithelium of digestive tract and organs of digestive tract (lungs, liver, pancreas, urinary system, etc.) Mesodermfills in everything in btw! Neural crest (ectodermal origin) ganglia, sensory neurons, medulla of supernal glands, a lot of CT cells within head and neck; neural ectoderm becomes central portion of nervous system Folding process of the embryo: -Embryo starts as a disc (intraembryonic coelom within it), growth processes related to development of the nervous system are accentuated, occurring rapidly -disc eventually folds so that it folds over its margins; center area grows more rapidly than peripherally (so it will rise up and overflow) -a head and tail fold will develop and lateral body folds develop at the same time. -Becomes a modified cylinder. Portion of 2ndary yolk sac is taken up into cylinder becoming precursor of digestive tract beginning at the oropharyngeal membrane and ending at the cloacal membrane