May 2014 Small Animal Benchmark
advertisement
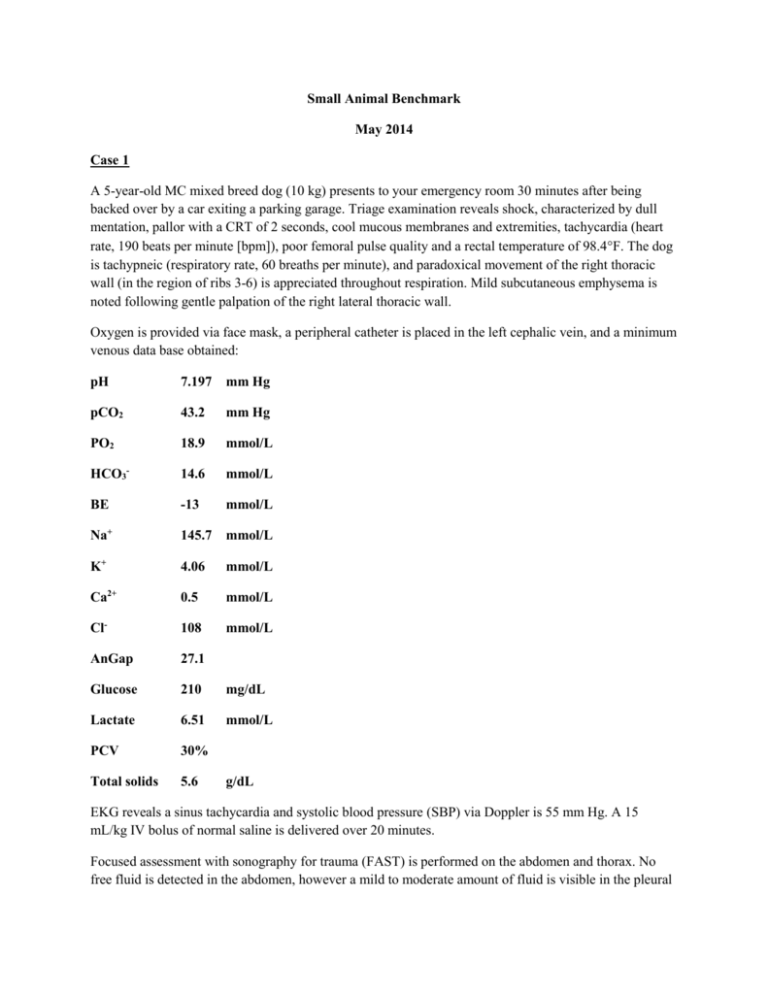
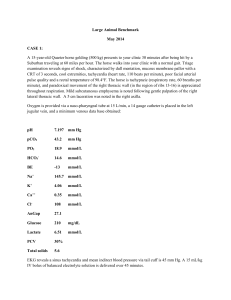
Small Animal Benchmark May 2014 Case 1 A 5-year-old MC mixed breed dog (10 kg) presents to your emergency room 30 minutes after being backed over by a car exiting a parking garage. Triage examination reveals shock, characterized by dull mentation, pallor with a CRT of 2 seconds, cool mucous membranes and extremities, tachycardia (heart rate, 190 beats per minute [bpm]), poor femoral pulse quality and a rectal temperature of 98.4F. The dog is tachypneic (respiratory rate, 60 breaths per minute), and paradoxical movement of the right thoracic wall (in the region of ribs 3-6) is appreciated throughout respiration. Mild subcutaneous emphysema is noted following gentle palpation of the right lateral thoracic wall. Oxygen is provided via face mask, a peripheral catheter is placed in the left cephalic vein, and a minimum venous data base obtained: pH 7.197 mm Hg pCO2 43.2 mm Hg PO2 18.9 mmol/L HCO3- 14.6 mmol/L BE -13 mmol/L Na+ 145.7 mmol/L K+ 4.06 mmol/L Ca2+ 0.5 mmol/L Cl- 108 mmol/L AnGap 27.1 Glucose 210 mg/dL Lactate 6.51 mmol/L PCV 30% Total solids 5.6 g/dL EKG reveals a sinus tachycardia and systolic blood pressure (SBP) via Doppler is 55 mm Hg. A 15 mL/kg IV bolus of normal saline is delivered over 20 minutes. Focused assessment with sonography for trauma (FAST) is performed on the abdomen and thorax. No free fluid is detected in the abdomen, however a mild to moderate amount of fluid is visible in the pleural cavity. No pneumothorax or pericardial effusion is noted. There are no other note-worthy neurologic, orthopedic or soft tissue injuries on your examination of this patient. Thoracic radiographs are obtained and are depicted below: Interpret the thoracic radiographs. Assign this dog an animal trauma triage (ATT) score. Provide an evidence-based description of the utility of this scoring system in outcome prediction in veterinary trauma patients. List 10 predictors of nonsurvival in dogs suffering from blunt trauma. Discuss the relevance of this trauma patient’s ionized hypocalcemia (iHCa). What is this patient’s shock index? Briefly discuss the utility of this parameter in assessment of dogs presenting to the emergency room. Define flail chest. What are the postulated mechanisms responsible for respiratory distress in patients diagnosed with flail chest? Outline your initial management strategy specifically for this patient’s flail chest. If conservative management fails, and surgical stabilization of the flail segment is indicated, briefly describe the technique you would choose for this patient. Heart rate remains elevated at 160 bpm despite adequate level of analgesia and normoxia (SpO2 of 94%, [FiO2 .4]). Systolic blood pressure after initial isotonic crystalloid bolus is 70 mm Hg. Follow-up PCV and TS are 20% and 3.5 g/dL, respectively. Repeat abdominal and thorax FAST examinations reveal static pleural effusion but now moderate peritoneal effusion is visible. Diagnostic abdominocentesis is performed and hemoperitoneum is confirmed (PCV of the fluid in the peritoneal cavity, 15%). You check a point-of-care prothrombin time (PT) and partial thromboplastin time (PTT). Both are out of range. Outline three hypotheses for the pathophysiology of acute traumatic coagulopathy (ATC). List six key factors that have been shown to influence ATC. Of these six, which two have been globally accepted as the main initiators of ATC? Briefly describe the purported difference put forth by some authors between ATC and traumainduced coagulopathy (TIC): You suspect that your patient has ATC. How could you demonstrate a hyperfibrinolytic state in this patient? Which of the following was recently demonstrated in a study evaluating the coagulation status of 40 dogs within 12 hours of severe acute trauma? a. Decreased activated Protein C was the strongest predictor of nonsurvival in this patient population. b. Acute traumatic coagulopathy was documented in 45% of dogs at the time of hospital admission. c. Prolonged aPTT positively correlated with illness severity score, lactate and negative base excess. d. Measurement of thromboelastography was not useful in predicting need for transfusion or outcome. Treatment of hyperfibrinolysis may be pursued via provision of an antifibrinolytic drug. Briefly discuss mechanism/s of action, metabolism and potential adverse effects of tranexamic acid. You ask your senior resident for their opinion on using an antifibrinolytic agent in your patient. This person references a paper on the 2014 ACVECC Additional Journal Article List that was published in The Lancet in 2010. Briefly outline the major findings of the CRASH-2 trial. What evidence exists in the veterinary literature regarding the use of antifibrinolytic drugs to control/arrest hemorrhage? Tranexamic and aminocaproic acid are unavailable to you for immediate use. Your patient has a coagulopathy and clinical signs you deem referable to his anemia. Outline and justify your transfusion plan for this patient. Include in your answer blood products selected and product dosages and ratios. Case 2 A 6-year old FS Golden Retriever is being prepared for laparotomy for splenectomy following incidental detection of a splenic mass during abdominal ultrasound. Preoperative blood work and thoracic radiographs are within normal limits. Physical examination reveals a palpable mid-abdominal mass and a 2/6 left apical holosystolic murmur. The owners decline an echocardiogram. The dog is assigned an ASA (American Society of Anesthesiologists) status of 2; anesthetic induction is uneventful. With the patient under general anesthesia, an arterial catheter is placed in the right metatarsal artery to facilitate monitoring of hemodynamics and respiration. Briefly describe your technique for assembling, zeroing and leveling the electronic direct arterial pressure monitoring system. Diagram and identify the major components of an idealized central arterial pressure waveform. Superimpose on your diagram the expected changes as the pressure wave moves toward the periphery. Define pulse pressure. What is the most common cause of a low (narrow) pulse pressure? List 3 specific causes of a high (wide) pulse pressure. How is mean arterial pressure (MAP) calculated using the systolic arterial blood pressure (SAP) and diastolic arterial blood pressure (DAP)? How is this accuracy of this calculation affected by patient heart rate? Identify and briefly describe the test being performed below: List 1 cause each for an underdamped and an overdamped fluid-filled monitoring system. Your anesthesia technician informs you that the dog’s MAP has decreased to 40 mm Hg. A fluid challenge of 10 mL/kg of normal saline is administered over 15 minutes with no change in MAP. The anesthesiologist enters the surgical prep area and suggests that pulse pressure variation be determined in this patient. Describe the theory behind and potential clinical utility of pulse pressure variation (PPV) in anesthetized patients. This patient’s PPV is 21%. What does this indicate? Increasing preload in this patient via an additional fluid bolus (5 mL/kg of Hespan) results in restoration of normotension (MAP, 85 mm Hg). This improvement in perfusion is likely due to augmentation of the patient’s cardiac output. What cardiovascular factors contribute to a patient’s cardiac output? Describe the difference between cardiac output and cardiac index. What is the normal range for the cardiac index in a dog? List 5 techniques specifically used for measurement of cardiac output (CO)? Provide one limitation for each methodology listed. With a pulmonary artery catheter (PAC), name and briefly describe the 2 methods that can be used to measure CO. Once the cardiac output is measured, Oxygen Delivery (DO2) and Oxygen Consumption (VO2) can be calculated. What are the formulas for calculating these two oxygen-derived variables? While the patient is being shaved for surgery there is an acute rise in heart rate (180 bpm, sinus rhythm) and recurrence of hypotension (MAP, 35 mm Hg). These hemodynamic changes are accompanied by acute pallor of the mucous membranes, and there is concern the patient’s splenic mass has ruptured. If cardiac output was being measured in this patient, would you expect the CO to increase, decrease or stay the same in this situation? Define systemic vascular resistance (SVR) and provide a formula for its calculation following determination of patient CO. In this patient would you expect the systemic vascular resistance (SVR) to increase, decrease or stay the same? What are the locations of the arterial and cardiopulmonary baroreceptors? Using a diagram, show how does the baroreceptor reflex work to maintain normal blood pressure? You elect to use hypotensive resuscitation in this patient while you await the arrival of your supervising soft tissue surgeon. Describe the principle and advantages of this resuscitation strategy, and indicate why it can be used safely in this patient. Once in the OR, due to active bleeding, a 5 clamp technique is used to provide rapid hemostasis. In the diagram below indicate where these 5 clamps should be placed. Provide evidence FOR or AGAINST performing concurrent gastropexy during this surgery to prevent this dog having a GDV in the future. Following surgical control of hemorrhage, a pRBC transfusion (10 mL/kg), and 2 boluses each of normal saline (20 mL/kg total volume) and Hespan (10 mL/kg total volume), your patient’s hemodynamic status normalizes. Review of the anesthesia record following the dog’s recovery from surgery reveals that the technician had initially opted for an intraoperative fluid rate of 15 mL/kg/hour. You explain to this technician that “perioperative fluid delivery rates should be individualized and goal-directed”. List 10 detrimental effects of liberal perioperative fluid administration and fluid overload in human (and likely veterinary) surgical patients. Differentiate between type 1 and type 2 fluid shifts out of the intravascular space toward the interstitium in the perioperative period. Briefly describe the revised Starling equation and glycocalyx model of transvascular fluid exchange as this pertains to perioperative fluid prescriptions. List at least 3 inflammatory mediators that have been implicated to result in compromise of the endothelial glycocalyx layer (EGL). There have been several proposed and experimental therapies that target the glycocalyx for protection and/or restoration. List 3 of these options.