Biologics_Improvers_Rheumatology
advertisement

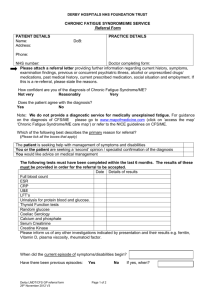
Title: Patients receiving Anti-TNF Therapies Experience Clinically Important Improvements in Rheumatoid Arthritis (RA) Related Fatigue – Results from the British Society of Rheumatology Biologics Register for RA. Authors: KL Druce1; GT Jones1; GJ Macfarlane1;N Basu1 1 Epidemiology Group, The Institute of Applied Health Sciences, University of Aberdeen Address for corresponding author and reprint requests: Ms Katie L Druce Epidemiology Group, The Institute of Applied Health Sciences, University of Aberdeen 1.007 Polwarth Building, Foresterhill, Aberdeen, AB25 2ZD Email: k.druce@abdn.ac.uk Short title: RA-Fatigue improves with Anti-TNF therapies Keywords: Fatigue; Rheumatoid Arthritis; Anti-TNF 1 Objectives: Pro-inflammatory cytokines, such as TNFα, are important in the pathogenesis of fatigue in conditions such as rheumatoid arthritis (RA). This study aimed to determine whether fatigue improved in a cohort of RA patients, with clinically relevant fatigue, commencing anti-TNFα therapy and, if so, to identify predictors of improvement. Methods: Participants recruited to a long-term observational cohort study (the British Society for Rheumatology Biologics Register for RA, BSRBR-RA) provided information on fatigue (SF36 Vitality). The prevalence of high baseline fatigue (SF36 Vitality ≤12.5) was calculated and improvements, considered as a) absolute values and b) improvement from severe to non-severe fatigue (SF36 Vitality >12.5), examined six months subsequently. A comprehensive set of putative predictors of fatigue improvement were evaluated using multivariable logistic regression. Results: In 6835 participants, the prevalence of high baseline fatigue was 38.8%. Of those with severe fatigue, 70% reported clinically relevant improvements and 66% moved to the non-severe fatigue category (i.e. “improvers”). The mean change for improvers was three times the minimum clinically important difference for improvement (33.0 units). Independent baseline predictors of improvement were: female sex (odds ratio 1.3, 95%CI 1.1-1.7), not being unemployed due to illhealth (1.5,1.2-1.7), low disability (1.2,1.001-1.5), seropositivity (1.2,0.98-1.4), not using steroids (1.2,1.03-1.5), no history of hypertension (1.4,1.1-1.6) or depression (1.3,1.1-1.5) and good mental health (SF 36 mental health >35; 1.4,1.2-1.7). Conclusions: Fatigued RA patients reported substantial improvements in their fatigue after commencing anti-TNFα therapy. Further, a number of clinical and psycho-social baseline factors identified those most likely to improve, supporting future stratified approaches to RA-fatigue management. 2 Introduction Up to 80% of Rheumatoid Arthritis (RA) patients experience significant fatigue[1] which they consider to be equally, if not more, important as pain [2, 3]. Indeed the symptom is recognised as a principal determinant of poor quality of life (QOL) and work disability among patients [4-6]. Unfortunately, there are no accepted therapies for this burdensome symptom. The aetiology of RA related fatigue likely comprises multiple processes [7]. Biologically, pro-inflammatory cytokines, known to be pivotal to the development and progression of RA [8, 9], have also been shown to impact upon fatigue [10-13]. TNFα is one such cytokine which has also been found to induce fatigue in animal models [13, 14] and to occur in excess in conditions such as Chronic Fatigue Syndrome (CFS) [14, 15]. Although anti-TNFα therapies are effective at reducing inflammation in RA, the evidence of a link between TNFα production and fatigue suggests that these therapies could also provide some relief for those RA patients experiencing high levels of fatigue. Whilst improvements in fatigue have been noted in patients using traditional DMARDs, initial evidence suggests that the effect of anti-TNF therapies on fatigue is superior [1, 6, 16-19]. The results from existing RCTs show only a modest benefit of anti-TNF therapies on fatigue[18], however, to date, no studies which have reported antiTNFα-associated improvements in fatigue have focused on evaluating the response in the target population; those experiencing clinically relevant symptoms. Given the multi-factorial origin of fatigue, it is likely that the response of fatigue to treatment will vary between patients. However, to date, no study has examined whether certain patient characteristics are able to identify those most likely to improve. Further, most prior work pertains to randomised control trials (RCTs), rather than observational “real-life” studies such as cohort studies. We therefore sought to determine the improvement of fatigue in a large cohort of highly fatigued RA participants, commencing anti-TNFα therapy for their active disease. Furthermore, we aimed to determine predictors of fatigue improvement among these participants. 3 Patients and Methods Data from 13122 participants, recruited between October 2000 and November 2008, were obtained from the British Society for Rheumatology Biologics Register for RA (BSRBR-RA). Data collection methods have been described elsewhere [20], but briefly it is a large prospective register of RA (Physician diagnosed or ACR criteria [21]) subjects commencing anti-TNF therapy with Infliximab, Etanercept or Adalimumab, from across the UK. Data collection remains ongoing for a number of biological drugs. A comprehensive set of demographic, clinical and psycho-social variables were measured at commencement of therapy and every six months subsequently. Ethical approval was granted to the BSRBR-RA by the North West Multi-centre Research Ethics Committee (MREC 00/8/53). Data captured comprised demographic, psycho-social and clinical variables. Using a self-report questionnaire, age, sex, ethnicity, and work status were captured at baseline. At baseline and six months, participants also provided information on: Short form 36 (SF 36) Vitality – Fatigue was measured using the Short form 36 (SF 36) Vitality scale, which has been validated for use in RA populations [22, 23]. In line with recommended strategies [24, 25], missing SF 36 Vitality items were replaced with the mean of completed domain items, provided 50% of items were reported. In this analysis, 358 participants required item replacement for baseline or follow up fatigue (5.2%). Full domain scoring was also completed as per the recommendations. Scores were transformed into a 0-100 scale, where a higher score indicates a better health state. Change in fatigue was calculated between baseline and follow up. Suggested minimum clinically important differences (MCID) in SF 36 domains range from 5 to 10 units [26, 27], for this study a conservative MCID of change ≥10 fatigue units was adopted. As no published definitions of severe fatigue were available, severe fatigue was defined as ≤5th percentile from a general population sample. The general population data was obtained from 1604 4 participants randomly selected from health board records, as part of a large scale general population postal survey conducted in the Grampian Region of Scotland[28]. The sample, which were age and sex matched to those in the current study, reported data on a variety of health measures, including the SF 36 Vitality 0-100 scale. Severe fatigue was consequently defined as a score of less than or equal to 12.5 units on the SF 36 Vitality 0-100 scale. SF 36 – The SF 36 provided additional health status information pertaining to the pain, role physical, role emotional, physical functioning, social functioning, general health and mental health experienced over a recall period of one month. Missing SF 36 items imputation, scoring and 0-100 scale transformation, were conducted as for the vitality scale [24, 25]. Studies show the SF 36 has good internal consistency, construct validity and sensitivity in RA populations [22, 23]. For this study the pain, role physical, role emotional and mental health domains were used. High SF 36 scores were defined using the same general population study from which the severe fatigue value was derived. Definitions of high SF 36 domains, included in the logistic regression analysis, were therefore scores ≤ 5th percentile of the general population data; high pain ≤22, high role physical ≤25, high role emotional ≤33.3 and high mental health ≤35. Health Assessment Questionnaire Disability Index (HAQ-DI) - This measure of disability encompasses eight categories of functioning – dressing, rising, eating, walking, hygiene, grip, reach and usual activities. Participants rated their ability to complete given tasks and scores are calculated on a scale of 0 (no disability) to 3 (completely disabled). The HAQ was developed and validated with RA patients [29, 30]. All other variables were reported by clinicians using a questionnaire which comprised: 5 Clinical status - data was obtained on the length of disease duration, disease activity score (DAS28; baseline and follow up), the presence of erosions, history of early morning stiffness lasting longer than one hour, rheumatoid factor status, and body mass index (BMI). Medication – In addition to the type of anti-TNFα therapy, information on the current use of disease modifying anti-rheumatic drugs (DMARDs), steroids, non-steroidal anti-inflammatory drugs (NSAIDs), beta-blockers, thyroxine, antidepressants and analgesics upon entry to the register was obtained. Co-morbidities – clinician reported histories of hypertension, stroke, chronic obstructive pulmonary disorder (COPD), depression and renal disease were also gathered. For this study, participants were eligible if they were commencing anti-TNFα for the first time and, after following mean-value imputation methods for missing data, had measures of fatigue, SF 36 vitality, at baseline and at six month follow up. Comparison cohort The BSRBR-RA also provided data for 3774 participants recruited to a DMARD comparison cohort. Subjects with confirmed RA (Physician diagnosed or ACR criteria [21]) who were not commencing anti-TNFα therapy were recruited and followed the same protocol as the anti-TNF cohort. To be eligible for this analysis the DMARD comparison cohort, participants were required to have measures of fatigue (SF 36 vitality) at baseline and at six month follow up. The data of those DMARD participants with high baseline fatigue was compared against changes in fatigue observed in the anti-TNF cohort. The available variables for the DMARD cohort mirrored those above, however for 6 the purposes of comparison it was age, sex, DAS28, disease duration, HAQ and baseline and followup fatigue which were of interest for this analysis. Analysis The prevalence of severe fatigue was examined and among only those with severe fatigue (SF 36 Vitality 0-100 ≤12.5), changes in fatigue at 6 months were examined. Changes were considered in two ways a) as absolute values of change and b) as improvement from severe fatigue status to nonsevere fatigue status (SF 36 Vitality 0-100 >12.5) and in two groups a) all those with severe fatigue and b) those who improved to a non-severe fatigue status at 6 months. The prevalence of severe fatigue was then examined in the DMARD comparison group. Among those with severe fatigue, the changes in fatigue reported between baseline and six months were determined as an absolute value of change and presented as a percentage of the changes reported by anti-TNF commencers. All baseline variables were offered to univariate logistic regressions. Given the large number of putative associations, a relaxed p-value - p≤0.2 – was selected to determine variables which may be associated with improvement in fatigue after adjustment by other predictors and therefore be eligible to be offered to a forward stepwise logistic regression model. Variables returned as significant univariate predictors were re-coded to ensure all variables were associated with an increased likelihood of fatigue improvement. Variables were eligible for inclusion in the stepwise multivariable model p≤0.1 and were excluded at p>0.15 The model was evaluated by allocating points to each participant based upon the number of positively associated variables present (1 point per variable). Participants were then categorised according to total number of variables present and proportion of participants improved and mean reductions in fatigue reported for each category. 7 The SF 36 functioning scales were excluded from analysis due to perceived overlap with HAQ-DI and the SF 36 general health domain was excluded because it was felt to be too broad a construct. All analysis was conducted using Stata 12.1 (College Station, Tx). RESULTS 6835 participants were eligible for the study, baseline characteristics are shown in Table 1. In brief, participants tended to be white females, with an average age of 57 and disease duration of just over 13 years. As expected, DAS and disability were high (mean 6.57 (S.D 0.98) and 2.03 (0.56), respectively). Finally, overall health state was poor, evidenced by low scores on SF 36 domains, including pain (21.1 (15.8), fatigue (24.8 (19.7) and general health (30.6 (18.4)). TABLE 1 to be inserted here Severe fatigue was reported by 38.8% of the sample, and, as severe fatigue was defined using the 5th percentile of general population data, it was therefore almost 8 times more commonly reported than in the general population study. Of those with severe baseline fatigue (characteristics shown in Table 1), approximately 70% reported a clinically relevant improvement of at least 10 units, with the average change in fatigue reported as an improvement of 22.5 units (SD 20.5). Furthermore, 66.5% of those with severe fatigue improved to a non-severe fatigue state at follow up. The mean change in fatigue reported by improvers was 33.0 (SD 16.8); three times greater than the MCID for improvement. Comparison cohort Of the participants recruited to the DMARD cohort, 2375 were eligible for the comparison group. Participants were slightly older than anti-TNF commencers (mean 60.7, SD 11.8), with a shorter disease duration (9.9, 10.5) lower disease activity (5.02, 1.30) and less disability (1.45, 0.76). They reported less fatigue, on average (36.9, 20.3) and a smaller proportion reported severe fatigue at baseline (16.9%, n=403). For DMARD participants with severebaseline fatigue, the average 8 improvement in fatigue between baseline and the six-month follow up was 13.3 units; reflecting 59% of the improvement reported by anti-TNF participants with severe fatigue, and 40% of the improvement reported by anti-TNF ‘Improvers’. As a result and 60% of the improvement reported by anti-TNF ‘Improvers’ was above the value likely accounted for by regression to the mean. Predicting those who will improve in fatigue after commencing anti-TNFα therapies Variables offered to the stepwise logistic regression, after using univariate analysis to determine individual significance (i.e. those associated at p≤0.2) , were mental health, role emotional, role physical, HAQ, sex, BMI, work status, histories of depression, hypertension, COPD and renal disease, the use of DMARDs, steroids, anti-depressants and beta blockers and Rheumatoid Factor status (RF+). No difference in improvement was observed between the use of Infliximab (INF), Adalimumab (ADA), or Etanercept (ETA) (INF vs ADA p=0.37; INF vs ETA p=0.41; ADA vs ETA p=0.92; all univariate analysis shown in Supplementary Table 1.). Eight variables were identified as independent predictors of fatigue improvement; good mental health (SF 36 Mental health>25), no history of hypertension, or of depression, no use of steroids, a work status other than “not working due to illness or disability”, low disability (HAQ <2), female sex and being RF+ve (Table 2). TABLE 2 to be inserted here For the purposes of model evaluation, participants were grouped in scores of 0-2, 3-5, or 6-8 positively associated variables present (e.g. no history of depression and female sex). Improvement was high in all groups; however participants who were positive for ≥6 variables reported the largest absolute improvement in fatigue. Furthermore, 75% of those positive for ≥6 variables, reported improvement in fatigue (Figure 2). Image 1.tif to be inserted here Figure 1 – Proportion of participants who improve and mean improvement in fatigue for those with 0-2, 3-5 and 6-8 variables present. 9 DISCUSSION Severe fatigue was reported 8 times more commonly in RA patients initiating anti-TNF therapy population than within the general population. Yet, more than two thirds of those patients experienced important improvements in fatigue, which, on average, were in excess of 3 times the MCID following therapy. In addition, a number of independent baseline predictors of improvement were identified, including a) a good disease status, as reflected by a low HAQ, non-use of steroids and avoidance of unemployment due to ill health b) absence of past depression and good current mental health and c) female sex. A number of potential limitations should be considered when interpreting these results. First, the use of cohort data is often associated with concerns of bias of the sample following loss to follow up; however, no clinically meaningful differences for core variables such as age, sex, fatigue and disease activity (data not shown) were observed between those who were included and those lost to follow up. Second, the use of SF 36 Vitality is associated with debate as to whether fatigue and vitality sit on a continuum [31] and it is noted that this measure cannot account for the impact of fatigue on daily life. However, the scale, validated in RA populations, provides a global fatigue score, for which good internal consistency, sensitivity and construct validity have been found [22, 31]. Although availability and inclusion of an alternative measure of fatigue would have validated these results, we provide data using a scale which, crucially, is sensitive to change following biologic agents [22] and which, given its widespread use, allows our results to comparable to other disease groups and also to the general population. In addition, to be eligible to commence biologics and to enroll in the BSRBR-RA Biologics cohort,our sample had a specific disease profile of high disease activity and had RA refractory to traditional DMARD treatments. As a result, the study is not generalizable to the entire RA population, yet, the lack of association between fatigue improvement and baseline measures of disease status suggests 10 that the identified predictors may potentially be applicable to patients with less active disease and severe fatigue. Our selection of participants with the highest level of baseline fatigue for analysis raises concerns that improvements in fatigue may be influenced by regression to the mean (RTM) [32, 33], if the group selected for analysis are outliers (i.e. they report abnormal fatigue levels). In spite of those with severe fatigue not being outliers ( 38.8% of the sample) we examined the potential impact of RTM using the BSRBR-RA’s DMARD comparison cohort. As we observed that the improvements in fatigue reported by anti-TNF Improvers were approximately 2.5 times greater than the natural variation reported by the DMARD cohort, it was concluded that at worst only part of the substantial improvements reflects RTM. Furthermore, given that 80% of improvers were found to report non-severe fatigue after one year (data not shown), swe conclude the improvements to be long-term, rather than short lived placebo effect from commencing a new therapy. We propose that it would be of interest for future longitudinal research to provide mechanistic insight as to how fatigue develops and changes with reference to other disease status measures. Such insight would develop understanding of the symptom and would potentially inform treatment options. Within this study, we determined predictors of those who will most likely improve to a non-severe fatigue status at six months, however, a high proportion of participants with 0-2 variables present improved in fatigue. This highlights the multidimensional nature of fatigue and, in spite of consideration of a broad range of relevant co-variates, the probable existence of residual confounding, which arises from a number of variables known to be associated with fatigue, the (e.g. sleep problems and cognitive influences [34]), were not captured by the original study and therefore not available for this analysis. That said, a number of previously identified associations were highlighted in this analysis, including an association between fatigue and hypertension, likely the result of treatment by beta11 blockers[35], and being RF+ve. Within this study, classification of RA was often defined according to the physician diagnosis alone and so although previous studies have associated seronegativity with more severe fatigue [36, 37], we propose that the inclusion of seropositivity in the model may serve to identify those who truly have RA, rather than those who may have been misclassified. The importance of both history of depression and current mental health has been discussed previously [2, 13, 38]and the suggestion that a “residual scar” is left after a depressive episode, leaving patients vulnerable to further depression and disruptions of symptoms, is supported by our model[2, 38]. Similar theoretical frameworks may explain why the ability to maintain work and low levels of disability would be important predictors of fatigue improvements [39, 40]. In contrast to our results, it has been suggested that males experience more clinically significant effects from anti-TNF due to a lack of androgens in RA [41, 42]. However, previous literature, is conflicting and, as in this study, ( data not shown), has demonstrated that females consistently report more fatigue than their male counterparts [43-46] and as such greater improvement may simply be due to females having a greater capacity for change. Notably, in spite of a wealth of literature discussing the prominence of the pain-fatigue relationship [1, 3-5, 44, 46, 47], pain was not determined to be an individually significant predictor of fatigue improvement. However, recent literature has found that the pain-fatigue relationship is synchronous, or transitory [47, 48] and therefore baseline pain may have little influence on fatigue in longitudinal analysis such as ours. Although the results from existing studies are equivocal [36, 49, 50], anecdotally both patients and clinicians may consider disease activity to determine fatigue status [46, 51]. Given the lack of association between fatigue and measures of disease activity within this study, we believethe importance of measuring fatigue in RA patients as an independent 12 outcome is emphasised. It is proposed that a future trial specifically assessing the impact of anti-TNF therapy, regardless of disease activity, on fatigue would be informative. Furthermore, as fatigue has yet to be considered as a primary end point, previous trials have not focussed upon the most clinically relevant sub-population of RA patients. In consequence they have tended not to recruit those most in need of fatigue treatment (evidenced by our participants’ lower SF36 vitality, than participants in other published studies[1, 6, 16-19]) and have demonstrated a more modest response of fatigue to anti-TNFα therapy [18], than our study. However, since the mechanisms underlying fatigue are likely to be multi-factorial and vary between patients, such therapy will not be appropriate for all and so the predictors identified in this study may inform strict selection criteria for such a study. Conclusions Our study examined the impact of anti-TNF therapy on levels of RA related fatigue in those presenting with clinically relevant fatigue and is the first to identify predictors of response. We have demonstrated clinically important improvements in fatigue are common, in those with greatest need, after commencing anti-TNFα therapy. Because of the multi-factorial origins of fatigue, immunomodulation therapy is not suitable for all; we therefore proceeded to identify baseline predictors of improvement. We believe predictors identified may inform stratified approaches to RA related fatigue management by differentiating those who may benefit from immunomodulatory approaches from others who may also require alternative interventions. 13 Key messages Rheumatoid Arthritis patients commencing anti-TNF therapy commonly report substantial improvements in fatigue after six months. Patients most likely to report improvement in fatigue can be identified by baseline characteristics. Improvement in fatigue does not seem to be related to baseline disease activity. Acknowledgements: The authors would like to thank the University of Manchester for access to the BSRBR-RA data and the BSR staff and Steering Committee for assistance with manuscript preparation. Conflicts of interest: KD, GJT, GJM - no conflicts of interest to declare. NB - research support and/or advisory: Pfizer, MSD, GSK Funding statement: This work was supported by The Institute of Applied Health Sciences, who fund KDs PhD. The British Society for Rheumatology Biologics Register for RA (BSRBR-RA) is supported by a research grant from the British Society for Rheumatology to the University of Manchester, which is indirectly funded by Schering Plough, Wyeth Laboratories, Abbott Laboratories and Amgen. 14 References [1] Pollard LC, Choy EH, Gonzalez J, Khoshaba B, Scott DL. Fatigue in rheumatoid arthritis reflects pain, not disease activity. Rheumatology 2006;45(7):885-9. [2] Jump RL, Fifield J, Tennen H, Reisine S, Giuliano AJ. History of affective disorder and the experience of fatigue in rheumatoid arthritis. Arthritis Care Res 2004;51(2):239-45. [3] Hewlett S, Nicklin J, Treharne GJ. Fatigue in musculoskeletal conditions. Reports on the Rheumatic Diseases (Series 6). Topical Reviews 1. Arthritis Research Campaign 2008. [4] Suurmeijer TPBM, Waltz M, Moum T, et al. Quality of life profiles in the first years of rheumatoid arthritis: results from the EURIDISS longitudinal study. Arthritis Care Res 2001;45(2):111-21. [5] Rupp I, Boshuizen HC, Jacobi CE, Dinant HJ, van den Bos GAM. Impact of fatigue on healthrelated quality of life in rheumatoid arthritis. Arthritis Care Res 2004;51(4):578-85. [6] Moreland LW, Genovese MC, Sato R, Singh A. Effect of etanercept on fatigue in patients with recent or established rheumatoid arthritis. Arthritis Care Res 2006;55(2):287-93. [7] Aaronson LS, Teel CS, Cassmeyer V, et al. Defining and Measuring Fatigue. Journal of Nursing Scholarship 1999;31(1):45-50. [8] Arend WP. Physiology of cytokine pathways in rheumatoid arthritis. Arthritis Care Res 2001;45(1):101-6. [9] Patarca R. Cytokines and Chronic Fatigue Syndrome. Ann N Y Acad Sci 2001 Mar 1;933(1):185-200. [10] Epstein FH, Choy EH, Panayi GS. Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med 2001;344(12):907-16. 15 [11] McInnes IB, Schett G. Cytokines in the pathogenesis of rheumatoid arthritis. Nature Reviews Immunology 2007;7(6):429-42. [12] Aouizerat BE, Dodd M, Lee K, et al. Preliminary evidence of a genetic association between tumor necrosis factor alpha and the severity of sleep disturbance and morning fatigue. Biological research for nursing 2009;11(1):27-41. [13] Norheim KB, Jonsson G, Omdal R. Biological mechanisms of chronic fatigue. Rheumatology 2011;50(6):1009-18. [14] Sheng WS, Hu S, Lamkin A, Peterson PK, Chao CC. Susceptibility to Immunologically Mediated Fatigue in C57BL/6 versus Balb/c Mice. Clin Immunol Immunopathol 1996;81(2):161-7. [15] Patarca R, Klimas NG, Lugtendorf S, Antoni M, Fletcher MA. Dysregulated Expression of Tumor Necrosis Factor in Chronic Fatigue Syndrome: Interrelations with Cellular Sources and Patterns of Soluble Immune Mediator Expression. Clin Infect Dis 1994;18(Supplement 1):S147-S153. [16] Weinblatt ME, Keystone EC, Furst DE, et al. Adalimumab, a fully human anti-tumor necrosis factor-alpha monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis & Rheumatism 2003;48(1):3545. [17] Yount S, Sorensen MV, Cella D, Sengupta N, Grober J, Chartash EK. Adalimumab plus methotrexate or standard therapy is more effective than methotrexate or standard therapies alone in the treatment of fatigue in patients with active, inadequately treated rheumatoid arthritis. Clinical & Experimental Rheumatology 2007;25(6):838. 16 [18] Chauffier K, Salliot C, Berenbaum F, Sellam J. Effect of biotherapies on fatigue in rheumatoid arthritis: a systematic review of the literature and meta-analysis. Rheumatology 2012;51(1):60-8. [19] Maini RN, Breedveld FC, Kalden JR, et al. Sustained improvement over two years in physical function, structural damage, and signs and symptoms among patients with rheumatoid arthritis treated with infliximab and methotrexate. Arthritis & Rheumatism 2004;50(4):105165. [20] Watson K, Symmons D, Griffiths I, Silman A. The British Society for rheumatology biologics register. Ann Rheum Dis 2005;64(suppl 4):iv42-iv43. [21] Arnett FC, Edworthy SM, Bloch DA, et al. The american rheumatism association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis & Rheumatism 1988;31(3):31524. [22] Hewlett S, Hehir M, Kirwan JR. Measuring fatigue in rheumatoid arthritis: A systematic review of scales in use. Arthritis Care Res 2007;57(3):429-39. [23] Ruta DA, Hurst NP, Kind P, Hunter M, Stubbings A. Measuring health status in British patients with rheumatoid arthritis: reliability, validity and responsiveness of the short form 36-item health survey (SF-36). Rheumatology 1998;37(4):425-36. [24] Ware JE, Jr., Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med Care 1992;30(6):473-83. [25] Wiles N, Symmons DPM, Harrison B, et al. Estimating the incidence of rheumatoid arthritis: trying to hit a moving target? Arthritis & Rheumatism 2001;42(7):1339-46. 17 [26] Kosinski M, Zhao SZ, Dedhiya S, Osterhaus JT, Ware JE. Determining minimally important changes in generic and disease-specific health-related quality of life questionnaires in clinical trials of rheumatoid arthritis. Arthritis & Rheumatism 2001;43(7):1478-87. [27] Strand V, Singh JA. Improved health-related quality of life with effective disease-modifying antirheumatic drugs: evidence from randomized controlled trials. Am J Manag Care 2007;13(supple 9):s237-s251. [28] Jones GT, Beasley M, Atzeni F, Fluess E, Sarzi-Puttini P, Macfarlane GJ. The prevalence of fibromialgia in the general population - a comparison of the ACR 1990, 2010 and modified 2010 classification criteria. Arthritis & Rheumatism 65 (10 Suppl): S358. 2013. [29] Kirwan JR, Reeback JS. Stanford Health Assessment Questionnaire modified to assess disability in British patients with rheumatoid arthritis. Rheumatology 1986;25(2):206-9. [30] Bruce B, Fries J. The Stanford Health Assessment Questionnaire: Dimensions and Practical Applications. Health and quality of life outcomes 2003;1(1):20. [31] Hewlett S, Dures E, Almeida C Measures of fatigue: Bristol Rheumatoid Arthritis Fatigue Multi-Dimensional Questionnaire (BRAF MDQ), Bristol Rheumatoid Arthritis Fatigue Numerical Rating Scales (BRAF NRS) for Severity, Effect, and Coping, Chalder Fatigue Questionnaire (CFQ), Checklist Individual Strength (CIS20R and CIS8R), Fatigue Severity Scale (FSS), Functional Assessment Chronic Illness Therapy (Fatigue) (FACIT-F), Multi-Dimensional Assessment of Fatigue (MAF), Multi-Dimensional Fatigue Inventory (MFI), Pediatric Quality Of Life (PedsQL) Multi-Dimensional Fatigue Scale, Profile of Fatigue (ProF), Short Form 36 Vitality Subscale (SF-36 VT), and Visual Analog Scales (VAS). Arthritis Care & Research 63; S263-S286. 18 [32] Linden A. Assessing regression to the mean effects in health care initiatives. BMC Med Res Methodol 2013;13(1):1-7. [33] Barnett AG, van der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol 2005;34(1):215-20. [34] Hewlett S, Chalder T, Choy E, et al. Fatigue in rheumatoid arthritis: time for a conceptual model. Rheumatology 2011;50(6):1004-6. [35] Erickson SR, Williams BC, Gruppen LD. Perceived symptoms and health-related quality of life reported by uncomplicated hypertensive patients compared to normal controls. J Hum Hypertens 2001;15(8):539-48. [36] van Hoogmoed D, Fransen J, Bleijenberg G, van Riel P. Physical and psychosocial correlates of severe fatigue in rheumatoid arthritis. Rheumatology 2010;49(7):1294-302 [37] Coury F, Rossat A, Tebib A, et al. Rheumatoid arthritis and fibromyalgia: a frequent unrelated association complicating disease management. The Journal of Rheumatology 2009;36(1):5862. [38] Fifield J, Tennen H, Reisine S, McQuillan J. Depression and the long-term risk of pain, fatigue, and disability in patients with rheumatoid arthritis. Arthritis & Rheumatism 1998;41(10):1851-7. [39] Hazes JM, Taylor P, Strand V, Purcaru O, Coteur G, Mease P. Physical function improvements and relief from fatigue and pain are associated with increased productivity at work and at home in rheumatoid arthritis patients treated with certolizumab pegol. Rheumatology 2010;49(10):1900-10. 19 [40] Mancuso CA, Paget SA, Charlson ME. Adaptations made by rheumatoid arthritis patients to continue working: a pilot study of workplace challenges and successful adaptations. Arthritis Care Res 2000;13(2):89-99. [41] Cutolo M, Sulli A, Capellino S, et al. Anti-TNF and Sex Hormones. Ann N Y Acad Sci 2006;1069(1):391-400. [42] Kristensen LE, Kapetanovic MC, Gülfe A, Söderlin M, Saxne T, Geborek P. Predictors of response to anti-TNF therapy according to ACR and EULAR criteria in patients with established RA: results from the South Swedish Arthritis Treatment Group Register. Rheumatology 2008;47(4):495-9. [43] Thyberg I, Dahlstrom O, Thyberg M. Factors related to fatigue in women and men with early rheumatoid arthritis: the Swedish TIRA study. Journal of Rehabilitation Medicine 2009;41(11):904-12. [44] Sokka T, Toloza S, Cutolo M, et al. Women, men, and rheumatoid arthritis: analyses of disease activity, disease characteristics, and treatments in the QUEST-RA study. Arthritis research & therapy 2009;11(1):R7. [45] Treharne GJ, Lyons AC, Hale ED, Goodchild CE, Booth DA, Kitas GD. Predictors of fatigue over 1 year among people with rheumatoid arthritis. Psychology, Health & Medicine 2008;13(4):494-504. [46] Mancuso CA, Rincon M, Sayles W, Paget SA. Psychosocial variables and fatigue: a longitudinal study comparing individuals with rheumatoid arthritis and healthy controls. The Journal of Rheumatology 2006;33(8):1496-502. 20 [47] van Dartel SAA, Repping-Wuts JWJ, van Hoogmoed D, Bleijenberg G, van Riel PLCM, Fransen J. Association Between Fatigue and Pain in Rheumatoid Arthritis: Does Pain Precede Fatigue or Does Fatigue Precede Pain? Arthritis Care Res 2013;65(6):862-9. [48] Nijrolder I, van der Windt DA, Twisk JW, van der Horst HE. Fatigue in primary care: Longitudinal associations with pain. Pain 2010;150(2):351-7. [49] Bergman M, Shahouri S, Shaver T, et al. Is Fatigue an Inflammatory Variable in Rheumatoid Arthritis (RA)? Analyses of Fatigue in RA, Osteoarthritis, and Fibromyalgia. The Journal of Rheumatology 2009;36(12):2788-94. [50] Stebbings S, Herbison P, Doyle TCH, Treharne GJ, Highton J. A comparison of fatigue correlates in rheumatoid arthritis and osteoarthritis: disparity in associations with disability, anxiety and sleep disturbance. Rheumatology 2010;49(2):361-7. [51] Hewlett S, Cockshott Z, Byron M, et al. Patients' perceptions of fatigue in rheumatoid arthritis: Overwhelming, uncontrollable, ignored. Arthritis Care Res 2005;53(5):697-702. 21 Table 1 – Baseline characteristics for participants All eligible Participants with participants severe fatigue (n=6835) (n=2652) Age (years) - mean (SD) 57 (11.7) 56 (11.4) % female (n) 76.5 (5228) 79.6 (2111) % white (n) 96.7 (6395) 97.3 (2492) % Not working due to illness and 30.5 (2020) 36.4 (935) % Rheumatoid factor positive (n) 64.1 (4381) 63.02 (1670) % Erosions (n) 62.9 (4290) 61.91 (1640) Disease duration (years) - mean (SD) 13.4 (9.8) 13.8 (10.0) Disease Activity (DAS 28) - mean (SD) 6.57 (0.98) 6.79 (0.93) Fatigue (SF36) – mean (SD) 24.8 (19.7) 5.8 (5.3) Pain (SF 36) - mean (SD) 21.1 (15.8) 14.0 (12.9) Role physical (SF 36) - mean (SD) 19.0 (22.5) 11.2 (15.4) Role emotional (SF 36) - mean (SD) 44.1 (36.2) 33.2 (33.8) Physical functioning (SF 36) - mean 19.8 (20.0) 13.1 (16.1) Social functioning (SF 36) - mean (SD) 36.3 (24.8) 23.1 (19.9) General health (SF 36) - mean (SD) 30.6 (18.4) 23.1 (15.9) Mental health (SF 36) - mean (SD) 55.1 (20.2) 45.1 (19.8) Disability (HAQ) - mean (SD) 2.03 (0.56) 2.23 (0.47) disability (n) (SD) 22 Table 2 – Odds ratio for variables significantly associated with improvement in fatigue in multivariable analysis (n=2414). Variable Mental health (SF 36) Disability (HAQ) Sex Work status Seropositivity Steroid use History of hypertension History of depression Odds-ratio (95% CI) Poor (≤ 35) 1.0 Good (>35) 1.4 (1.2-1.7) High (≥2) 1.0 Low (<2) 1.2 (1.001-1.5) Male 1.0 Female 1.3 (1.009-1.7) Not working due to illness or disability 1.0 All other work status 1.5 (1.2-1.7) Rheumatoid factor negative 1.0 Rheumatoid factor positive 1.2 (0.98-1.4) Using steroids 1.0 Not using steroids 1.2 (1.03-1.5) Yes 1.0 No 1.4 (1.1-1.6) Yes 1.0 No 1.3 (1.1-1.5) Figure legend Figure 1 – Proportion of participants who improve and mean improvement in fatigue for those with 0-2, 3-5 and 6-8 variables present. 23