Surgery Rotation Syllabus
advertisement

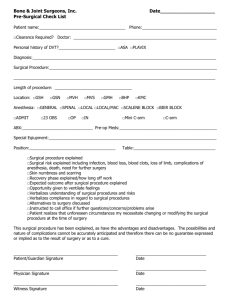
Department of Physician Assistant Studies Learning. Caring. Serving. Leading. PAS 638: Surgery 3 Semester Hours Course Director: Diane Duffy, MD Tracey Tonsor, PA-C Office FC 205 FC 207 Phone 336-278-6848 336-278-6852 E-mail dduffy2@elon.edu ttonsor@elon.edu Course Description: The Surgery clinical rotation is designed to give students experience in the care of patients undergoing elective or acute surgical procedures. The student will perform the pre-operative history and physical; assist, when able, in the operating room; be involved in immediate post-operative care and stabilization; and assist with post-operative follow up. Course Goals: The educational goals of the Surgery rotation include: 1. To apply the medical content and principles that define the care of surgical patients. 2. To provide opportunities for each student to develop the core PA competencies in a supervised surgical setting. 3. To expose each student to an experienced and competent medical provider role model for the care of surgical patients. Learning Outcomes: Upon completion of this course the clinical phase PA students will: 1. Obtain and document an appropriate surgical history and physical examination. 2. Demonstrate the ability to apply knowledge of surgical principles to develop a working diagnosis and treatment plan for common surgical problems, taking into account clinical epidemiology and probabilistic reasoning. 3. Demonstrate an understanding of the appropriate diagnostic tests used in the evaluation of the surgical patient and an ability to correctly interpret results from these studies. 4. Determine the appropriate use of medications, fluids, and anesthetics in the surgical patient. 5. Properly perform/assist and document surgical procedures under the supervision of the preceptor including wound closure. 6. Be able to communicate in a medically professional manner, both orally and in writing, with the patient, the family and health care professionals. 7. Demonstrate proficiency in creating and maintaining the medical record of the surgical patient. 8. Be able to recognize and jointly manage life-threatening emergencies. Revised 10/23/13 9. Participate in and complete discharge planning with the healthcare team and patient to include writing prescriptions, arranging for outpatient or home therapies, and setting up follow-up visits. 10. Assure smooth and thorough transfer of care back to referring or primary care health care provider. Teaching Methodologies: The content of this module will be presented through a variety of methods that include observation and participation at the clinical site, independent reading and participation in online activities developed to guide experiential learning. Accommodations: Students requiring academic accommodations must follow the “Academic Support” policy in the Elon University DPAS Student Handbook. Academic Honesty: All Elon PA students acknowledged their commitment to abide by the Elon Honor Code by signing the Honor Pledge during orientation. Students will sign an Honor Pledge (electronically or manually) each time an assignment is turned in or an examination is started to reaffirm their complete understanding of the Honor Code of Elon University and their affirmation that their work abides by that Code. Required Textbooks: All first-year required textbooks. Essential of General Surgery by Lawrence, 3rd Ed. Surgical Recall by Blackbourne, 2nd Ed. ISBN: 0-683-30102-0 (Optional) Other Resources: *Moodle: Please check the course site frequently for new announcements, updated schedules, assignments and other course communication. Practicing physician assistants, physicians, allied health care providers and laboratory teaching aids. Revised 10/23/13 Assessment Activities: Exams/quizzes (25%), Preceptor Evaluation (65%), Professionalism (10%). Grade Scale and Grade Points Percentage 89.50-100 85.50-89.49 79.50-85.49 75.50-79.49 69.50-75.49 Below 69.50 There is no rounding of grades. Letter Grade A B+ B C+ C U Grade points 4.0 3.3 3.0 2.3 2.0 0 Note: For further information regarding academic standing in the Department of Physician Assistant Studies, please see the Student Handbook. Grading Criteria: 1. Demonstrate acquisition of a strong basic science and medical science knowledge base as demonstrated on the written examination/quizzes. 2. Demonstrate satisfactory self-directed learning skills, clinical reasoning skills, commitment to patient-centered care and professionalism as evidenced by satisfactory performance on the preceptor evaluation. 3. Demonstrate a commitment to learning and professionalism by actively participating in all clinical activities and exceeding the professional behavior standards and minimum requirements for clinical rotations available in the Elon PA Student Handbook. Instructional Objectives: Upon completion of the clinical rotation clinical phase physician assistant students will be able to: 1. Clinical Skills a. Demonstrate the ability to obtain an accurate and appropriate surgical history documenting all information from available sources such as patient and family; recognizing and accounting for comorbid disease states; and taking into account any medications the patient is using. b. Perform and document appropriate physical examination for pre-operative screening and post-operative follow-up. c. Ensure proper pre-operative preparation of the patient. 2. Identify, perform, order and/or interpret appropriate, cost-effective, routine, diagnostic procedures, based on history and physical examination findings, and be able to assist the physician with other diagnostic procedures as directed. Revised 10/23/13 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. a. Identify the appropriate and available diagnostic tests for a particular problem based on the history and physical examination findings. b. Identify and discuss indications and contraindications of diagnostic tests c. Identify and describe the risks, costs, and patient inconvenience of diagnostic tests. d. Demonstrate the skills required to collect routine specimens including bacteriologic samples, venous and arterial blood, sputum, and urine. Discuss the appropriate use of medications in the surgical patient related to such issues as dosage, indications, contraindications, interactions, complications, metabolism and excretion in the following settings: a. Pain management b. Perioperative antibiotic usage c. Chemotherapy d. Inpatient considerations (e.g. sleep medications, anti-emetics, laxatives) Discuss anesthetics, their indications, modes of action, contraindications, complications and combinations in: a. General anesthesia b. Spinal and regional anesthesia c. Regional anesthesia/field blocks Know the composition of fluids that are frequently lost from the body, including urine, gastric secretions, diarrhea, third spaced fluids, and hemorrhage and be able to compensate for the loss of these fluids through the proper utilization of IV fluid, blood or blood product therapy. Understand the role interpreting serum electrolytes plays in determining the replacement fluid. Recognize the signs and clinical manifestations of hypovolemia and hypervolemia and institute corrective measures. Practice proper technique in the following settings a. Demonstrate knowledge of and ability to scrub and gown for surgery, position patient, maintain sterile technique, tie knots, suture/staple, apply dressings, transfer patient to and from O.R. table, hold retractors. b. Demonstrate ability to set up a sterile field outside the O.R. (for office procedures) Be competent in wound closure techniques a. Know the various techniques for dermal closure b. Discuss the different types of suture materials and their uses including silk, gut, chromic, nylon, Dacron and vicryl. Demonstrate I & D of an abscess. Identify and manage problems common to peri-operative management of the surgical patient such as DVT/PE prophylaxis, infection, mobility and ambulation, blood conservation and management. Present to the physician a brief synopsis of the patient’s illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen instituted. Communicate effectively with the patient and family regarding the disease process, risks, expected outcome, possible side effects, and post-operative care. Document the care of the surgical patient Revised 10/23/13 14. 15. 16. 17. 18. a. Write clear, concise and relevant progress notes delineating diagnostic, therapeutic and patient education plans b. Dictate or otherwise document the discharge summary c. Maintain a complete up-to-date problem list Recognize signs and symptoms of common emergencies and take appropriate action to sustain life a. Apply basic techniques of CPR b. Assist with or perform other techniques frequently indicated in life-threatening situations (e.g. endotracheal/nasogastric intubation; defibrillation/cardioversion; central line insertion, central venous pressure monitoring) c. Initiate hemostasis in a patient with hemorrhage d. Assess and treat hemorrhagic shock e. Be familiar with triage procedures in mass casualty situations. f. Assess patients with multiple trauma, skull and/or spinal injuries. Work with medical team and patient to formulate a complete discharge plan anticipating and arranging for discharge medication prescriptions, outpatient or home therapy services, home/self care instructions and scheduling follow-up. Anticipate specific needs of the patient being sensitive to the patient’s home environment, change in level of care needed based on post-surgical condition and ability to perform activities of daily living. Coordinate communication with the patient’s primary care and/or referring physician to allow for smooth transition of care. Describe the following common surgical problems, including risk assessment, pathophysiology, diagnosis, treatment, indications and contraindication for surgery and follow-up: Topics Pre-operative/Postoperative Cardiovascular Gastrointestinal (cont’d) Revised 10/23/13 Care Risk assessment: Cardiac disease: history of , MI, unstable angina, valvular disease, hypertension arrhythmias, heart failure Pulmonary disease: history of diabetes, adrenal insufficiency Hematologic disease: history clotting disorders, anticoagulant use Tobacco use/dependence Substance abuse Post-operative fever Wound infections Deep venous thrombosis Fluid/volume disorders Electrolyte disorders Acid/base disorders Hematologic System Easy bruising/bleeding Anemia Fatigue Chest pain; history of angina Syncope Dyspnea on exertion Claudication Aortic Aneurysm/dissection Arterial embolism/thrombosis Peripheral arterial disease Arterial/venous ulcer disease Varicose veins Gastrointestinal Abdominal pain Anorexia Heartburn/dyspepsia Nausea/vomiting Jaundice Hematemesis Diarrhea/constipation/ obstipation/change in bowel habits Melena/hematochezia Esophageal cancer Hiatal hernia Peptic ulcer disease Gastric cancer Pancreatic pseudocyst Pyloric stenosis Acute/chronic cholecystitis Pancreatic carcinoma Appendicitis Inflammatory bowel disease Small bowel carcinoma Toxic megacolon Colorectal carcinoma Diverticular disease Bowel obstruction (small, large, volvulus) Anal disease (fissures, abscess, fistula) Hemorrhoids Hernias (inguinal, femoral, incisional) Bariatric surgery Pulmonary Shortness of breath Hemoptysis Weight loss, fatigue Lung carcinoma Pleural effusion Pneumothorax Pneumonia (post-operative) Topics (cont’d) Genitourinary Edema Endocrinology Tremors Dermatology Rash Revised 10/23/13 Orthostatic hypotension Urinary retention Dysuria Fluid and electrolyte disorders Testicular carcinoma Wilm’s Tumor Bladder carcinoma Renal cell carcinoma Chronic renal failure (shunts/access) Renal vascular disease Nephrolithiasis Fatigue Palpitations Heat/cold intolerance Hyperparathyroidism Hyperthyroidism Thyroid nodules Adrenal carcinoma Pheochromocytoma Women’s Health Pain Skin Changes Nipple discharge Adenopathy Benign breast disease (fibroadenomas, fibrocystic breast disease) Breast carcinoma Redness/erythema Discharge Drug eruptions (postoperative) Urticaria (post-operative) Cellulitis Burns Pressure ulcers Basal cell carcinoma Squamous cell carcinoma Melanoma Neurology (Neurosurgery) Change in vision Change in speech Motor and/or sensory loss Vascular disorders (carotid disease) Subarachnoid hemorrhage Subdural hematoma Epidural hematoma Revised 10/23/13