Prognostic Value of Myocardial Perfusion Imaging In Patients
advertisement
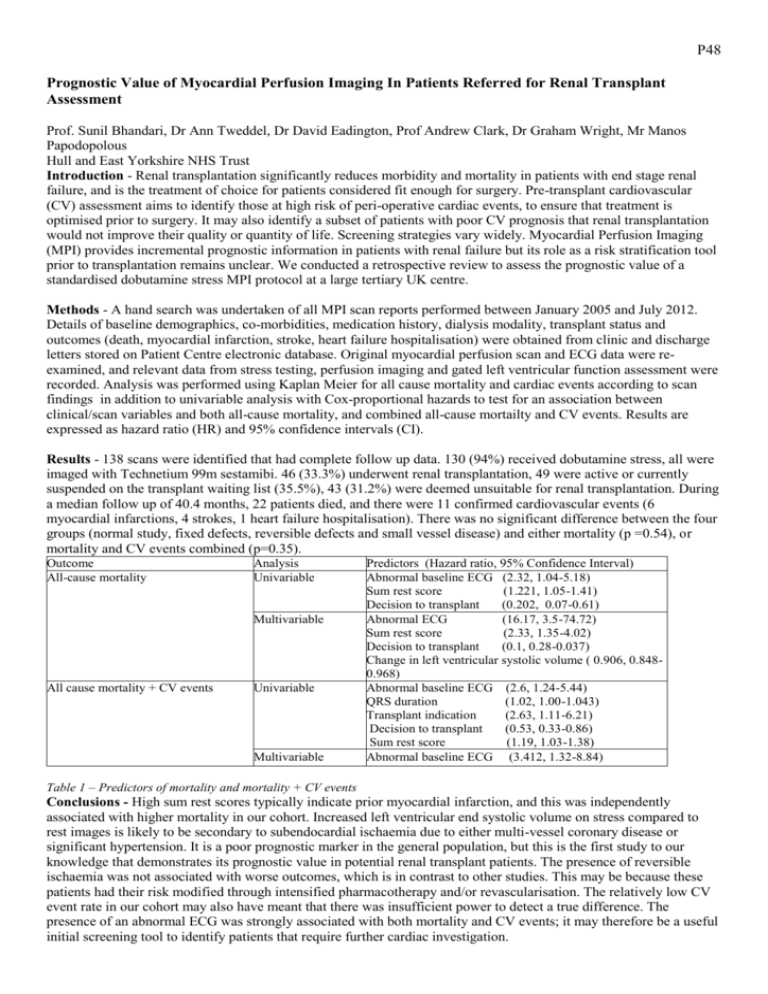
P48 Prognostic Value of Myocardial Perfusion Imaging In Patients Referred for Renal Transplant Assessment Prof. Sunil Bhandari, Dr Ann Tweddel, Dr David Eadington, Prof Andrew Clark, Dr Graham Wright, Mr Manos Papodopolous Hull and East Yorkshire NHS Trust Introduction - Renal transplantation significantly reduces morbidity and mortality in patients with end stage renal failure, and is the treatment of choice for patients considered fit enough for surgery. Pre-transplant cardiovascular (CV) assessment aims to identify those at high risk of peri-operative cardiac events, to ensure that treatment is optimised prior to surgery. It may also identify a subset of patients with poor CV prognosis that renal transplantation would not improve their quality or quantity of life. Screening strategies vary widely. Myocardial Perfusion Imaging (MPI) provides incremental prognostic information in patients with renal failure but its role as a risk stratification tool prior to transplantation remains unclear. We conducted a retrospective review to assess the prognostic value of a standardised dobutamine stress MPI protocol at a large tertiary UK centre. Methods - A hand search was undertaken of all MPI scan reports performed between January 2005 and July 2012. Details of baseline demographics, co-morbidities, medication history, dialysis modality, transplant status and outcomes (death, myocardial infarction, stroke, heart failure hospitalisation) were obtained from clinic and discharge letters stored on Patient Centre electronic database. Original myocardial perfusion scan and ECG data were reexamined, and relevant data from stress testing, perfusion imaging and gated left ventricular function assessment were recorded. Analysis was performed using Kaplan Meier for all cause mortality and cardiac events according to scan findings in addition to univariable analysis with Cox-proportional hazards to test for an association between clinical/scan variables and both all-cause mortality, and combined all-cause mortailty and CV events. Results are expressed as hazard ratio (HR) and 95% confidence intervals (CI). Results - 138 scans were identified that had complete follow up data. 130 (94%) received dobutamine stress, all were imaged with Technetium 99m sestamibi. 46 (33.3%) underwent renal transplantation, 49 were active or currently suspended on the transplant waiting list (35.5%), 43 (31.2%) were deemed unsuitable for renal transplantation. During a median follow up of 40.4 months, 22 patients died, and there were 11 confirmed cardiovascular events (6 myocardial infarctions, 4 strokes, 1 heart failure hospitalisation). There was no significant difference between the four groups (normal study, fixed defects, reversible defects and small vessel disease) and either mortality (p =0.54), or mortality and CV events combined (p=0.35). Outcome All-cause mortality Analysis Univariable Multivariable All cause mortality + CV events Univariable Multivariable Predictors (Hazard ratio, 95% Confidence Interval) Abnormal baseline ECG (2.32, 1.04-5.18) Sum rest score (1.221, 1.05-1.41) Decision to transplant (0.202, 0.07-0.61) Abnormal ECG (16.17, 3.5-74.72) Sum rest score (2.33, 1.35-4.02) Decision to transplant (0.1, 0.28-0.037) Change in left ventricular systolic volume ( 0.906, 0.8480.968) Abnormal baseline ECG (2.6, 1.24-5.44) QRS duration (1.02, 1.00-1.043) Transplant indication (2.63, 1.11-6.21) Decision to transplant (0.53, 0.33-0.86) Sum rest score (1.19, 1.03-1.38) Abnormal baseline ECG (3.412, 1.32-8.84) Table 1 – Predictors of mortality and mortality + CV events Conclusions - High sum rest scores typically indicate prior myocardial infarction, and this was independently associated with higher mortality in our cohort. Increased left ventricular end systolic volume on stress compared to rest images is likely to be secondary to subendocardial ischaemia due to either multi-vessel coronary disease or significant hypertension. It is a poor prognostic marker in the general population, but this is the first study to our knowledge that demonstrates its prognostic value in potential renal transplant patients. The presence of reversible ischaemia was not associated with worse outcomes, which is in contrast to other studies. This may be because these patients had their risk modified through intensified pharmacotherapy and/or revascularisation. The relatively low CV event rate in our cohort may also have meant that there was insufficient power to detect a true difference. The presence of an abnormal ECG was strongly associated with both mortality and CV events; it may therefore be a useful initial screening tool to identify patients that require further cardiac investigation.